Abstract
Purpose
The goal of this study was to determine whether sleep moderates the associations between family-related stress and depressive symptoms and negative affect outcomes during adolescence. We combined traditional survey measures of stress and depressive symptoms with daily assessments of stress and negative affect to examine whether sleep differentially impacts the link between chronic and acute experiences of stress and affect.
Methods
Participants were 316 adolescents from ethnically diverse backgrounds. Primary care-givers and adolescents reported on stressful family events during the past 12 and 3 months, respectively. Adolescents also reported on their daily experiences of family demands for 15 days and wore actigraph watches for the assessment of sleep during the first eight nights.
Results
Regression analyses revealed that more stressful family events were related to more depressive symptoms. This relation was stronger among adolescents with lower sleep efficiency. The same pattern emerged for the relation between daily family demands and negative affect aggregated across the 15 days. Daily-level analyses indicated that daily negative affect was related to daily family demands when sleep efficiency was higher than usual, but only among European American adolescents.
Conclusions
These findings suggest that chronic experiences of lower sleep efficiency, but not sleep duration, may render adolescents more vulnerable to the negative effects of family stress on emotional adjustment. A more complex picture emerged for the role of prior night’s sleep in the day-to-day variation in negative affect reactivity to family stress.
Keywords: Stressful events, Daily stress, Depression, Mood, Adolescence
Depression is a common and debilitating mental health disorder that often emerges during adolescence. Up to 11.7% of adolescents meet criteria for clinical depression and nearly a third exhibit subclinical levels of depressive symptomatology [1,2]. Family-related stress is a major risk factor for developing depression and increases negative affect (NA), a core symptom of depression [3]. However, its effects on depression risk may vary as a function of individual difference factors. Sleep may be one important factor given its reciprocal relations with cognitive and emotional functioning implicated in stress processes and development of depression [4,5]. For instance, poor sleep (e.g., shorter sleep duration and lower sleep quality) disrupts emotion regulation, increasing NA and risk for depression [5,6]. The impact of poor sleep on emotional responses to stress may be especially profound during adolescence given that neural systems underlying cognitive and affective processes and circadian and homeostatic systems underlying sleep processes undergo significant changes during this time [7,8].
Several studies support the moderating role of sleep in the effects of stress. Specifically, perceived discrimination, peer victimization, and interparental conflict have been more strongly related to internalizing symptoms and aggression among adolescents with lower sleep quality and efficiency and shorter sleep duration relative to those with better sleep [9–11]. The present study builds on these studies by combining traditional survey approaches, on which previous studies have relied, with a daily diary approach. Daily measures of experiences minimize retrospection and can elucidate whether previous findings translate to adolescents’ everyday experiences in their natural context [12]. In addition, a daily diary approach enables examination of acute and chronic experiences, providing a more nuanced understanding of sleep’s modulation of the stress-affect connection. Acute experiences of stress, sleep, and NA are common in everyday life and can have immediate, same-day effects on one another [13,14]. They can also occur repeatedly over time, cumulatively leading to poor outcomes (e.g., [15]). Thus, a daily diary approach can shed light on whether links between family stress, sleep, and affect differ for chronic versus acute experiences in everyday life.
The purpose of the present study was to examine the moderating role of sleep in the link between family-related stress and depressive symptoms and NA among adolescents. With the aim of replicating prior studies, we examined this question using traditional survey measures of depressive symptoms and family-related stressful events, a robust predictor of depression [16]. Extending past studies, we examined the same question using daily assessments of NA and family demands, which increase during adolescence and have been shown to be impactful daily stressors among adolescents [17–19]. We addressed our research question at the individual and daily levels. Individual-level analyses focused on chronic experiences, testing whether the association between family demands and NA aggregated across days varied as a function of sleep averaged across days. Analyses at the daily level focused on acute experiences, testing whether the daily association between family demands and NA depended on prior night’s sleep.
We focused on actigraphy estimates of sleep duration and sleep efficiency, common and important sleep parameters used as an index of sleep quantity and quality, respectively [20,21]. Sleep duration reflects the total amount of sleep obtained, whereas sleep efficiency (percentage of sleep during the in-bed period) captures difficulties in falling asleep and maintaining sleep. Both short sleep duration and low sleep efficiency have each been linked to health-related outcomes [22,23]; however, they may also have differential effects [24,25]. Examining both can help identify which aspect of sleep may be a more impactful moderator of stress-related risk.
Methods
Participants
Participants were 316 adolescents (180 females) ages 15–20 years (Meanage = 16.4 years, standard deviation = .74). Twenty-nine percent of adolescents were of European descent, 42% Latino, 23% Asian, and 6% reported other backgrounds. Parent-reported median household income was $50,000 (range = $0–$825,000). Parents also reported their own and their spouse’s highest level of education completed, which was used to calculate mean parental education level across parents. Approximately 14% of participants’ parents did not obtain a high school diploma, 15% graduated high school, 42% completed vocational trade school or some college, 17% graduated college, and 11% completed at least some graduate or professional school.
Procedures
Participants were recruited from four Los Angeles high schools. In-class presentations were made and fliers and recruitment forms were distributed at schools and via mail to students’ homes. Families expressing interest were contacted, given more details about the study, and scheduled for an in-home visit, during which adolescents and their primary caregivers (usually mothers) completed questionnaires and assessments of biological markers (data not presented here).
Participants then completed a 15-day diary protocol. Each night before going to bed, participants completed a 4-page diary checklist on their social and emotional experiences. Participants indicated when each checklist was completed using security-coded, pre-programmed time stampers and stamping booklets. Approximately 94% of adolescents completed daily checklists for at least 14 days; 4% completed diary checklists for less than 7 days. Of the completed diaries, the vast majority (over 97%) were completed before noon on the following day and therefore judged to be compliant.
Adolescents also wore actigraph watches on their nondominant wrists and completed morning diaries of their previous night’s sleep for the first 8 days. They were instructed to push a button on the device to mark when they turned off the lights to sleep, got out of bed during the night, and got out of bed in the morning. The majority of participants (93%) wore the actigraph watches. Of these, 29% wore them for 8 days, 33% for 7 days, 23% for 6 days, 4% for 5 days, and 10% wore them for 4 or fewer days. To help ensure high rates of compliance, adolescents were sent reminder text messages of when to complete the diary checklists and wear their actigraph watches each day.
Adolescents were compensated $50 and two movie theater passes if their daily checklists were completed correctly and on time. Caregivers consented (with youth assent) to all study procedures, which were approved by the University Institutional Review Board.
Measures
Family-related stressful life events
Parents and adolescents completed event checklists adapted from widely used measures of stressful life events associated with negative outcomes [26,27]. Parents indicated whether they had experienced any of 13 events within the last 12 months (e.g., got laid off, relationship with your spouse changed for the worse, a family member died). Adolescents indicated whether they had experienced any of 14 events within the last 3 months (e.g., did not see mom for 1 month or longer, became seriously ill, grades in school went down). Affirmative responses were summed across parent and adolescent reports given that each measure assessed different events and that stressful experiences of one family member can spillover and affect family functioning as a whole [28].
Daily family demands
Two items on daily checklists assessed whether adolescents experienced family demands on any given day: [1] had a lot of work at home and [2] had a lot of demands made by your family. These items were adapted from previous daily diary studies of adults and have been linked to negative outcomes, including lower academic achievement, higher NA, and shorter sleep duration [18,19,29]. The average correlation between the two items each day across the 15-day study period was .23 (range: .08–.43). Scores were summed across the two items for each day and recoded as 0 or 1 to indicate whether adolescents experienced any family demands that day. This variable was used in daily-level analyses. For individual-level analyses, recoded scores were averaged across the 15-day study period, resulting in summary scores representing proportion of days that family demands occurred.
Depressive symptoms
The Center for Epidemiologic Studies-Depression Scale [30] was used to assess depressive symptomatology over the past month. Using a four-point scale (0 = rarely or none of the time, 3 = most or all the time), participants rated items such as “I felt sad,” and “I could not get going.” From the original 20-item scale, the item assessing sleep was excluded before analyses. The remaining 19 items were summed to create a composite score for each individual (α = .91).
Daily negative affect
Using a five-point scale (1 = not at all, 5 = extremely), adolescents reported how sad, hopeless, discouraged, frightened, nervous, on edge, scared, threatened, uneasy, worried, and unsafe they felt each day. Items were taken from the Profile of Mood States anxiety and depression subscales [31], and additional items were included to assess fear. Principal components analysis revealed that a single factor explained 83%–97% of the variance on each day of the 15-day daily diary period. Loadings of each item onto the single factor ranged from .83 to .99. For daily-level analyses, items were averaged each day (α = .83–.92). For individual-level analyses, daily average scores of NA were averaged across all 15 days (α = .92).
Sleep
Sleep was assessed for eight consecutive nights using Actigraph (Micro Motionlogger Sleep Watch, Ambulatory Monitoring, Inc.). Action4 software (Ambulatory Monitoring, Inc.) was used to score actigraphy data. The first and last event markers indicating when participants turned off the lights to sleep and when they got out of bed in the morning were used to determine the in-bed period. When event markers were absent, participants’ reports of when they turned off the lights and/or got out of bed in the morning from the morning diaries were used. Of all potential event markers, 4.6% were absent.
To compute sleep duration and efficiency, sleep onset and offset times were first determined using the Sadeh actigraph algorithm to score 1-minute epochs [32]. The first 3 or more consecutive minutes of sleep indicated sleep onset time and the last 5 or more consecutive minutes of sleep indicated sleep offset time [33]. These sleep onset and offset times were checked against the morning self-reports of the previous night’s sleep. Actigraphy-based and diary-reported sleep and wake times were highly correlated (sleep: r =.80, p < .001; wake: r =.76, p < .001). Total sleep duration was the total number of minutes scored as sleep during the in-bed period. Sleep efficiency was the percentage of actual sleep over total time in bed. Sleep indices were averaged across the eight nights for individual-level analyses.
Statistical analyses
Stata 14.2 was used to conduct all data analyses. We first examined descriptives and bivariate associations among study variables. Variables were also examined for missing data and outliers. Of the 316 participants, 289 had complete data on all relevant variables. Outlier screening revealed six individuals who had mean sleep efficiency (n = 3) or sleep duration (n = 3) that were below three standard deviations. These values were set to missing to minimize their influence on results. Multiple imputation was used to handle missing data in regression analyses. Imputation models contained all predictor, outcome, control, and auxiliary variables. Regression models were estimated in the 20 imputed data sets and we report model parameters pooled across data sets.
A series of hierarchical regressions were then conducted to test whether sleep moderated the association between family-related stress and depressive symptoms and NA at the individual level. Family stress, sleep, and sociodemographic variables (i.e., age, gender, ethnicity, and parental education) were entered in the first step. The interaction term between family stress and sleep was added in the second step. Daily variables were aggregated across the diary period (15 days for family demands and NA; 8 days for sleep indices), and continuous variables were mean centered. Separate models were examined for each measure of family stress and sleep. To facilitate interpretation of observed significant interactions, we conducted follow-up tests of simple slopes at half a standard deviation above and below the mean of sleep indices because no adolescent was above one standard deviation for sleep efficiency. Additional exploratory and regions of significance analyses were also conducted (see Appendix).
Next, multi-level modeling tested whether the daily association between family demands and NA depended on the previous night’s sleep. Level 1 modeled the daily variation in NA within individuals, and Level 2 modeled between-person differences. Family demands, previous night’s sleep, and their interaction were entered as predictors at the daily level, and potential confounding variables were entered as predictors of the intercept at the individual level. In addition to sociodemographic characteristics, prior day’s NA and total number of demands across the study period were included as covariates to ensure that results were not due to affective spillover or greater stressor exposure. Continuous daily-level predictors were person-centered and continuous covariates were grand-mean centered. Two separate models were tested for sleep duration and sleep efficiency. Any observed interactions were followed up with tests of simple slopes at half a standard deviation above and below the mean of sleep indices. Because sleep was assessed on the first 8 days, daily analyses were based on 8 days of daily diary data. All models were estimated using full information maximum likelihood estimation.
All analyses were repeated with sleep duration and efficiency and their interactions with family stress variables entered into the same model to determine unique effects of each sleep parameter. We also explored whether observed results varied by gender, ethnicity, and socioeconomic status (SES) by testing a series of three-way interactions (e.g., family stress × sleep × gender). Unless otherwise noted, gender, ethnic, and SES differences were not observed. Sensitivity analyses were also conducted (see Appendix).
Results
Descriptive data and bivariate correlations are displayed in Table 1. More stressful events and daily demands were related to greater depressive symptoms and daily NA. More depressive symptoms were related to higher NA, and higher sleep efficiency was related to greater sleep duration. Correlations between demographic variables and primary study variables show that older age was associated with shorter sleep duration, and higher parent education was associated with fewer stressful life events. See Appendix for details on gender and ethnic differences on primary study variables.
Table 1.
Descriptive statistics and bivariate correlations
| Variables | Mean (SD) | Range | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age (years) | 16.40 (.74) | 14.50–20.50 | – | −.13* | .01 | −.10 | −.07 | −.03 | .01 | −.15* | .10 |
| 2. Parent education | 7.19 (1.81) | 1.50–11.00 | – | −.14* | −.01 | −.02 | −.03 | .06 | .01 | .06 | |
| 3. Family stressful events | 3.71 (2.45) | .00–14.00 | – | .10 | .10 | .26** | .20** | .06 | −.03 | ||
| 4. Daily family demands (proportion of days) | .12 (.17) | .00–1.00 | – | .97*** | .23*** | .22*** | −.11† | −.05 | |||
| 5. Daily family demands (sum across days) | 1.94 (2.93) | .00–17.00 | – | .22*** | .25*** | −.13* | .03 | ||||
| 6. Depressive symptoms | 14.78 (10.10) | .00–47.00 | – | .44*** | .01 | .01 | |||||
| 7. Daily negative affect | 1.34 (.40) | 1.00–3.73 | – | −.02 | .03 | ||||||
| 8. Sleep duration (hours) | 7.46 (.99) | 2.20–10.05 | – | .40** | |||||||
| 9. Sleep efficiency (percent) | 93.33 (6.34) | 24.50–99.58 | – |
p < .05,
p < .01,
p < .001,
p = .06.
Categories for parent education were 1 = some elementary school, 2 = completed elementary school, 3 = some junior high school, 4 = completed junior high school, 5 = some high school, 6 = graduated high school, 7 = trade or vocational school, 8 = some college, 9 = graduated from college, 10 = some medical, law, or graduate school, and 11 = graduated from medical, law, or graduate school. Daily negative affect scores are on a five-point scale (1 = not at all, 5 = extremely).
SD = standard deviation.
Family stressful life events, sleep, and depressive symptoms
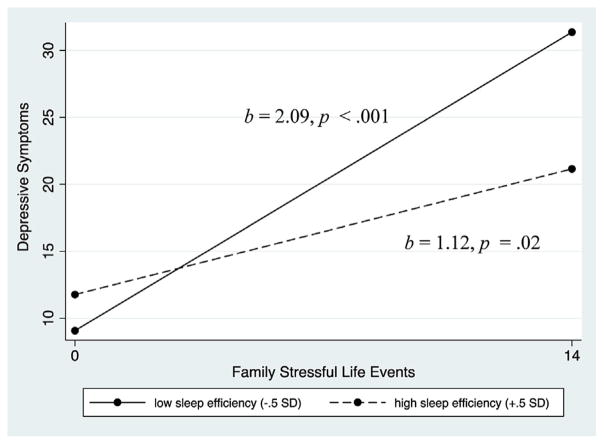
Regression analyses revealed that more stressful life events were related to greater depressive symptoms (p values < .001; Table 2, columns 1 and 3), which was qualified by sleep efficiency (p = .01; column 2). As depicted in Figure 1, more stressful life events were more strongly related to greater depressive symptoms among adolescents with lower sleep efficiency (b [SE] = 2.09 [.54], p < .001; SE, standard error) compared to those with higher sleep efficiency (b [SE] = 1.12 [.47], p = .02).
Table 2.
Regression analyses predicting depressive symptoms and daily NA as a function of family stress, sleep, and the interaction between family stress and sleep
| Stressful life events | Daily family demands | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Sleep efficiency | Sleep duration | Sleep efficiency | Sleep duration | |||||
|
|
|
|
|
|||||
| Step 1 | Step 2 | Step 1 | Step 2 | Step 1 | Step 2 | Step 1 | Step 2 | |
|
|
|
|
|
|
|
|
|
|
| b (SE) | b (SE) | b (SE) | b (SE) | b (SE) | b (SE) | b (SE) | b (SE) | |
| Intercept | 12.24 (1.24)*** | 11.62 (1.25)*** | 12.36 (1.24)*** | 12.23 (1.23)*** | 1.24 (.05)*** | 1.25 (.05)*** | 1.25 (.05)*** | 1.24 (.05)*** |
| Age | −.40 (.75) | −.42 (.75) | −.51 (.77) | −.69 (.77) | .02 (.03) | .01 (.03) | .01 (.03) | .01 (.03) |
| Gender | 3.35 (1.17)** | 3.65 (1.16)** | 3.32 (1.13)** | 3.40 (1.13)** | .15 (.05)** | .14 (.05)** | .14 (.04)** | .14 (.04)** |
| Latino | .62 (1.42) | 1.30 (1.43) | .60 (1.43) | .60 (1.43) | .03 (.06) | .02 (.05) | .03 (.06) | .04 (.06) |
| Asian | 1.53 (1.60) | 1.98 (1.59) | 1.41 (1.62) | 1.56 (1.61) | −.05 (.07) | −.04 (.06) | −.05 (.06) | −.05 (.06) |
| Other | −.61 (2.47) | −.29 (2.45) | −.64 (2.48) | −.50 (2.47) | .15 (.10) | .15 (.09) | .15 (.10) | .15 (.10) |
| Parent education | .21 (.33) | .32 (.33) | .17 (.33) | .12 (.33) | .02 (.01) | .01 (.01) | .01 (.01) | .01 (.01) |
| Stress | 1.09 (.23)*** | 1.06 (.23)*** | 1.10 (.23)*** | 1.11 (.23)*** | .56 (.13)*** | .59 (.13)*** | .55 (.13)*** | .52 (.13)*** |
| Sleep | −.11 (.15) | −.12 (.14) | −.01 (.01) | −.003 (.01) | −.01 (.01) | −.01 (.01) | .00 (.00) | .00 (.00) |
| Stress − Sleep | −.15 (.06)** | −.01 (.004)† | −.10 (.03)*** | −.003 (.002) | ||||
| Adjusted R2 | .08 | .11 | .08 | .09 | .07 | .10 | .07 | .07 |
p < .05,
p < .01,
p < .001,
p ≤ .07.
Gender coded as male = 0 and female = 1. Ethnicity was dummy coded with European Americans as the reference group.
SE = standard error.
Figure 1.
Greater family major life events were more strongly related to more depressive symptoms among adolescents with lower sleep efficiency compared to adolescents with higher sleep efficiency.
There was a trend toward an interaction between stressful life events and sleep duration (p = .07; column 4); however, when sleep efficiency, duration, and their interactions with stressful events were entered into the same model, only sleep efficiency remained a significant moderator (events × sleep duration: b [SE] =−.01 [.004], p = .14; events × sleep efficiency: b [SE] = −.13 [.06], p = .03).
Daily family demands, sleep, and negative affect
Individual level
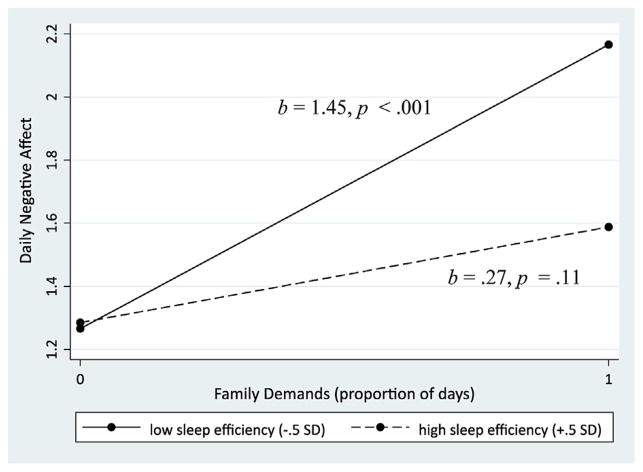
Next, regression analyses examined whether sleep moderated the relation between daily family demands and NA aggregated across the 15-day period. More family demands were related to greater NA (p values ≤ .001; Table 2, columns 5 and 7), which was moderated by sleep efficiency (p = .002; column 6). As shown in Figure 2, more daily demands were associated with higher levels of NA among adolescents with lower sleep efficiency (b [SE] = 1.45 [.31], p < .001) but not among those with higher sleep efficiency (b [SE] = .27 [.17], p = .11). Moderation of sleep duration on the family demands-NA relation was not observed (p = .28, Table 2, column 8). The interaction between family demands and sleep efficiency remained significant even when sleep duration and its interaction with family demands were included in the model (b [SE] =−.10 [.03], p = .002).
Figure 2.
More family demands were related to greater negative affect only among adolescents with lower sleep efficiency, but not in adolescents with higher sleep efficiency.
Daily level
We also examined whether sleep moderated the family demands-NA link at the daily level using multilevel modeling. NA was higher on days when adolescents had family demands compared with days when they had no family demands (b [SE] = .13 [.04], p < .001). This association depended on previous night’s sleep efficiency (b [SE] = .01 [.01], p = .03), but not sleep duration (b [SE] = .00 [.00], p = .66). Tests of simple slopes revealed that increases in NA on family demand days were higher when adolescents had higher sleep efficiency than they usually do (b [SE] = .39 [.14], p = .004) compared with when they had lower sleep efficiency than they usually do (b [SE] = .15 [.13], p = .24). Results were unaltered when sleep duration and its interaction with family demands were included in the model (b [SE] = .01 [.01], p = .03).
There was significant ethnic variation in sleep efficiency’s modulation of the link between daily family demands and NA (Table 3, column 2). Follow-up analyses within each ethnic group revealed a significant interaction between family demands and sleep efficiency only among European Americans (b [SE] = .05 [.01], p < .001) and not among the other ethnic groups (p values > .34). European American adolescents had higher levels of NA on family demand days compared with nonfamily demand days only when they had higher sleep efficiency than they typically do the night before (b [SE] = .39 [.13], p = .004). Demands were unrelated to NA when they achieved lower sleep efficiency than they usually do the night before (b [SE] = .15 [.13], p = .24).
Table 3.
Multilevel models predicting daily NA as a function of daily family demands, prior night’s sleep, sociodemographic characteristics, and their interactions
| Sleep duration | Sleep efficiency | |
|---|---|---|
|
|
|
|
| b (SE) | b (SE) | |
| Intercept | .89 (.05)*** | .89 (.05)*** |
| Age | .01 (.03) | .01 (.03) |
| Gender | .10 (.04)** | .10 (.04)** |
| Latino | .02 (.05) | .02 (.05) |
| Asian | −.03 (.05) | −.03 (.05) |
| Other | .09 (.08) | .09 (.08) |
| Parent education | .01 (.01) | .01 (.01) |
| Prior day NA | .25 (.02)*** | .25 (.02)*** |
| Total # of family demands | .02 (.01)* | .01 (.01)* |
| Demands day | .30 (.11)** | −.32 (.11)** |
| Sleep | .000 (.000) | −.004 (.004) |
| Demands day × Sleep | .001 (.001) | .04 (.01)*** |
| Demands day × Sleep × Gender | .001 (.001) | −.01 (.01) |
| Demands day × Sleep × Latino | −.001 (.001) | −.04 (.02)** |
| Demands day × Sleep × Asian | −.000 (.001) | −.04 (.02)* |
| Demands day × Sleep × Other | −.001 (.002) | −.07 (.04)† |
| Demands day × Sleep × Parent education | .000 (.000) | −.005 (.004) |
p < .05,
p < .01,
p < .001,
p = .07.
Gender coded as male = 0 and female = 1. Ethnicity was dummy coded with European Americans as the reference group. Lower order interaction terms omitted for simplicity.
NA = negative affect; SE = standard error.
Discussion
The present investigation found that sleep efficiency, but not sleep duration, consistently moderated the association between family-related stress and depressive symptoms and NA among adolescents, even when adjusting for the role of sleep duration. The links between family-related stressful life events and depressive symptoms and between daily family demands and NA across the daily diary period were stronger among adolescents with lower sleep efficiency. The daily contingency between family demands and NA was accentuated in the context of higher sleep efficiency, but only among European American adolescents. These findings highlight sleep efficiency above sleep duration as an important modulator of family stress–related risk.
Lower sleep efficiency potentiated the links between family-related stress and depressive symptoms and NA at the individual level, suggesting that low sleep efficiency day after day may be an important risk factor in the context of more chronic or repeated stress. One potential explanation for these findings is that lower sleep efficiency, as an index of fragmented sleep, interferes with restorative processes that occur during sleep, including neurobiological alterations that may help resolve strong emotions related to challenging situations and reset the brain’s sensitivity to emotional stimuli [34]. Alternatively, heightened vigilance and arousal may be the source of moderation rather than sleep efficiency per se. Intrusive thoughts, anxiety, and perceptions of threat can prolong sleep onset and interfere with sleep maintenance [35]. Thus, low sleep efficiency may reflect difficulty in decreasing vigilance and arousal [36], which in turn may amplify the effects of stress on NA and depressive symptoms. Experimental induction of sleep fragmentation is needed to help determine whether sleep maintenance or heightened vigilance renders adolescents more susceptible to the negative emotional effects of stress.
The modulating role of sleep efficiency was also observed at the daily level, but only among European American adolescents. Levels of NA were higher on family demand days when European American adolescents achieved higher sleep efficiency than they usually do. Ethnic differences in family dynamics may explain why this was specific to European American adolescents. Latino American and Asian-American youth have a stronger sense of family obligations and spend more time assisting their families compared with their European American peers [37]. Thus, European American adolescents may be more sensitive to family demands, whereas Latino American and Asian-American adolescents may find helping the family to be more rewarding [38]. Indeed, ancillary daily-level analyses revealed increases in NA responses to family demands were greatest among European American adolescents (European: b [SE] = .23 [.07], p = .002; Latino: b [SE] = .10 [.05], p = .05; and Asian: b [SE] = .11 [.07], p = .11). The amplification of NA responses to family demands was observed in the context of higher rather than lower sleep efficiency, which seems to contradict findings from individual-level analyses. However, acute bouts of sleep loss subsequently increase sleep efficiency during sleep recovery [39]. High sleep efficiency on a particular night, then, may reflect accumulated sleep debt, whereas low sleep efficiency across time may reflect chronic experiences of lower sleep quality. Experimental induction of sleep fragmentation and sleep restriction across a number of days can help elucidate whether daily-level findings are indeed due to incurred sleep debt.
Several features of the study should be considered when interpreting findings. Given the correlational nature of the study, directionality of effects and causal relations cannot be ascertained. Longitudinal investigations clarifying causal relations are critical given documented bidirectional relations among primary study variables. Pubertal status, which has been implicated in sleep [40], was not evaluated and future work should determine its role in the observed pattern of results. Generalizability of findings is limited, and it remains to be seen whether the findings apply to African-American adolescents or to those in rural areas. Findings also cannot be generalized to a clinical sample, as our sample was overall well-adjusted and slept fairly well. With this in mind, findings are particularly striking, and results may be more pronounced among clinical samples or at more extreme levels of sleep duration and efficiency.
The present study emphasizes sleep efficiency as a modulator of stress-related risk during adolescence. Despite public health campaigns and national sleep recommendations focusing on the total hours of sleep adolescents should be getting nightly, our findings suggest that indices of sleep maintenance, such as sleep efficiency, may be equally important for adolescent emotional development.
Supplementary Material
IMPLICATIONS AND CONTRIBUTION.
Difficulty falling and staying asleep may amplify depressive symptoms and negative emotions following family stress during adolescence. Efforts to identify at-risk adolescents and improve emotional adjustment related to family stress should consider the role of sleep.
Acknowledgments
Funding Sources
This research was supported by funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01-HD062547), UCLA California Center for Population Research, which is supported by the National Institute of Child Health and Human Development (R24-HD041022), the UCLA Older Americans Independence Center, which is supported by the National Institute of Aging (P30-AG028748 and P30-AG017265), and the Cousins Center for Psychoneuroimmunology at UCLA Semel Institute for Neuroscience.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Disclaimer: The content does not necessarily represent the official views of the National Institute of Child Health and Human Development, National Institute of Aging, or the National Institutes of Health.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.jadohealth.2017.04.011.
References
- 1.Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138:e20161878. doi: 10.1542/peds.2016-1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balazs J, Miklósi M, Keresztény Á, et al. Adolescent subthreshold-depression and anxiety: Psychopathology, functional impairment and increased suicide risk. J Child Psychol Psychiatry. 2013;54:670–7. doi: 10.1111/jcpp.12016. [DOI] [PubMed] [Google Scholar]
- 3.Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychol Bull. 2002;128:330–66. [PubMed] [Google Scholar]
- 4.Goel N, Rao H, Durmer JS, et al. Neurocognitive consequences of sleep deprivation. Semin Neurol. 2009;29:320–39. doi: 10.1055/s-0029-1237117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vandekerckhove M, Cluydts R. The emotional brain and sleep: An intimate relationship. Sleep Med Rev. 2010;14:219–26. doi: 10.1016/j.smrv.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Breslau N, Roth TL, Rosenthal L, et al. Sleep disturbance and psychiatric disorders: A longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39:411–8. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 7.Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007;8:602–12. doi: 10.1016/j.sleep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev. 2000;24:417–63. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- 9.Lemola S, Schwarz B, Siffert A. Interparental conflict and early adolescents’ aggression: Is irregular sleep a vulnerability factor? J Adolescence. 2012;35:97–105. doi: 10.1016/j.adolescence.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Tu KM, Erath SA, El-Sheikh M. Peer victimization and adolescent adjustment: The moderating role of sleep. J Abnorm Child Psychol. 2015;43:1447–57. doi: 10.1007/s10802-015-0035-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yip T. The effects of ethnic/racial discrimination and sleep quality on depressive symptoms and self-esteem trajectories among diverse adolescents. J Youth Adolesc. 2015;44:419–30. doi: 10.1007/s10964-014-0123-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bolger N, Davis A, Rafaeli E. Diary methods: Capturing life as it is lived. Annu Rev Psychol. 2003;54:579–616. doi: 10.1146/annurev.psych.54.101601.145030. [DOI] [PubMed] [Google Scholar]
- 13.Chung GH, Flook L, Fuligni AJ. Daily family conflict and emotional distress among adolescents from Latin American, Asian, and European backgrounds. Dev Psychol. 2009;45:1406–15. doi: 10.1037/a0014163. [DOI] [PubMed] [Google Scholar]
- 14.Doane LD, Thurston EC. Associations among sleep, daily experiences, and loneliness in adolescence: Evidence of moderating and bidirectional pathways. J Adolescence. 2014;37:145–54. doi: 10.1016/j.adolescence.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 15.Chiang JJ, Eisenberger NI, Seeman TE, et al. Negative and competitive social interactions are related to heightened proinflammatory cytokine activity. Proc Natl Acad Sci. 2012;109:1878–82. doi: 10.1073/pnas.1120972109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- 17.Telzer EH, Fuligni AJ. Daily family assistance and the psychological well-being of adolescents from Latin American, Asian, and European backgrounds. Dev Psychol. 2009;45:1177–89. doi: 10.1037/a0014728. [DOI] [PubMed] [Google Scholar]
- 18.Flook L, Fuligni AJ. Family and school spillover in adolescents’ daily lives. Child Dev. 2008;79:776–87. doi: 10.1111/j.1467-8624.2008.01157.x. [DOI] [PubMed] [Google Scholar]
- 19.Fuligni AJ, Hardway C. Daily variation in adolescents’ sleep, Activities, and psychological well-being. J Res Adolescence. 2006;16:353–78. [Google Scholar]
- 20.Doane LD, Gress-Smith JL, Breitenstein RS. Multi-method assessments of sleep over the transition to college and the associations with depression and anxiety symptoms. J Youth Adolescence. 2015;44:389–404. doi: 10.1007/s10964-014-0150-7. [DOI] [PubMed] [Google Scholar]
- 21.Ohayon M, Wickwire EM, Hirshkowitz M, et al. National sleep Foundation’s sleep quality recommendations: First report. Sleep Health. 2017;3:6–19. doi: 10.1016/j.sleh.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 22.Javaheri S, Storfer-Isser A, Rosen CL, et al. Sleep quality and elevated blood pressure in adolescents. Circulation. 2008;118:1034–40. doi: 10.1161/CIRCULATIONAHA.108.766410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mezick EJ, Hall M, Matthews KA. Sleep duration and ambulatory blood pressure in black and white adolescents. Hypertension. 2012;59:747–52. doi: 10.1161/HYPERTENSIONAHA.111.184770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raikkonen K, Matthews KA, Pesonen AK, et al. Poor sleep and altered hypothalamic-pituitary-adrenocortical and sympatho-adrenal-medullary system activity in children. J Clin Endocrinol Metab. 2010;95:2254–61. doi: 10.1210/jc.2009-0943. [DOI] [PubMed] [Google Scholar]
- 25.Prather AA, Janicki-Deverts D, Hall MH, et al. Behaviorally assessed sleep and susceptibility to the common cold. Sleep. 2015;38:1353–9. doi: 10.5665/sleep.4968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hammen C. Generation of stress in the course of unipolar depression. J Abnorm Psychol. 1991;100:555–61. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- 27.Conger RD, Wallace LE, Sun Y, et al. Economic pressure in African American families: A replication and extension of the family stress model. Dev Psychol. 2002;38:179. [PubMed] [Google Scholar]
- 28.Repetti RL, Wang SW, Saxbe D. Bringing it all back home how outside stressors shape families’ everyday lives. Curr Dir Psychol Sci. 2009;18:106–11. [Google Scholar]
- 29.Bolger N, DeLongis A, Kessler RC, et al. Effects of daily stress on negative mood. J Personal Soc Psychol. 1989;57:808–18. doi: 10.1037//0022-3514.57.5.808. [DOI] [PubMed] [Google Scholar]
- 30.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 31.McNair D, Lorr M, Droppleman L. Profile of mood states (POMS) San Diego, CA: Educational and Industrial Testing Services; 1971. [Google Scholar]
- 32.Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: An empirical test of methodological issues. Sleep. 1994;17:201–7. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
- 33.Acebo C, Sadeh A, Seifer R, et al. Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1-to 5-year-old children. Sleep. 2005;28:1568–77. doi: 10.1093/sleep/28.12.1568. [DOI] [PubMed] [Google Scholar]
- 34.Goldstein AN, Walker MP. The role of sleep in emotional brain function. Annu Rev Clin Psychol. 2014;10:679–708. doi: 10.1146/annurev-clinpsy-032813-153716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Riemann D, Spiegelhalder K, Feige B, et al. The hyperarousal model of insomnia: A review of the concept and its evidence. Sleep Med Rev. 2010;14:19–31. doi: 10.1016/j.smrv.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 36.Dahl RE. The regulation of sleep and arousal: Development and psychopathology. Dev Psychopathol. 1996;8:3–27. [Google Scholar]
- 37.Fuligni AJ, Tseng V, Lam M. Attitudes toward family obligations among American adolescents with Asian, Latin American, and European backgrounds. Child Dev. 1999;70:1030–44. [Google Scholar]
- 38.Telzer EH, Masten CL, Berkman ET, et al. Gaining while giving: An fMRI study of the rewards of family assistance among White and Latino youth. Social Neurosci. 2010;5:508–18. doi: 10.1080/17470911003687913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: What a difference an hour makes. Child Dev. 2003;74:444–55. doi: 10.1111/1467-8624.7402008. [DOI] [PubMed] [Google Scholar]
- 40.Knutson KL. The association between pubertal status and sleep duration and quality among a nationally representative sample of US adolescents. Am J Human Biol. 2005;17:418–24. doi: 10.1002/ajhb.20405. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.