Abstract
Background
In 2010 the Consortium on Safe Labor published labor curves. It was proposed that the rate of cesarean delivery (CD) could be lowered by avoiding the diagnosis of arrest of dilation before 6 cm. However, there is little information on the uptake of the guidelines and on changes in CD rates that may have occurred.
Objective
To test the hypotheses that: 1) among patients laboring at term, rates of arrest of dilation disorders have decreased leading to a decrease in the rate of CD; 2) in the second stage, pushing duration prior to diagnosis of arrest of descent has increased also leading to reduction in the rate of CD for this indication. As a secondary aim, we investigated changes in maternal and neonatal morbidity.
Study Design
This was a secondary analysis of a prospective cohort study of all patients presenting at ≥ 37 weeks’ gestation from 2010–2014 with a non-anomalous vertex singleton and no prior history of CD. Rates of CD, arrest of dilation, and changes in rates of maternal and neonatal morbidity were calculated in crude and adjusted models. Cervical dilation at diagnosis of arrest of dilation, time spent at the maximal dilation prior to diagnosis of arrest of dilation, and time in the second stage prior to diagnosis of arrest of descent were compared over the study period.
Results
There were 7845 eligible patients. The CD rate in 2010 was 15.8% and in 2014 17.7% (p-trend 0.51). In patients undergoing CD for arrest of dilation, the median cervical dilation at the time of CD was at 5.5 cm in 2010 and 6.0 cm in 2014 (p-trend 0.94). In these patients, there was an increase in the time spent at last dilation: 3.8h in 2010 to 5.2h in 2014 (p-trend 0.02). There was no change in the frequency of patients diagnosed with arrest of dilation at <6 cm: 51.4% in 2010 and 48.6% in 2014 (p-trend 0.56). However, in these patients, the median time spent at the last cervical dilation was 4.0h in 2010 and 6.7h in 2014 (p-trend 0.046). There were 206 CDs for arrest of descent. The median pushing time in these patients increased in multiparous patients from 1.1h in 2010 to 3.4h in 2014 (p-trend 0.009); in nulliparous patients these times were 2.7h in 2010 and 3.8h in 2014 (p-trend 0.09). There was a significant trend towards increasing adverse neonatal and maternal outcomes (p<0.001 for each). The aOR for adverse maternal outcome for 2014 compared to 2010 was 1.66 (95%CI 1.27, 2.17); however considering only transfusion, hemorrhage, or infection, there was no difference (p-trend 0.96). The aOR of adverse neonatal outcome in 2014 compared to 2010 was 1.80 (95%CI 1.36, 2.36).
Conclusion
Despite significant changes in labor management that have occurred over the initial years since publication of the new labor curves and associated guidelines, the primary CD rate was not reduced and there has been an increase in maternal and neonatal morbidity in our institution. A randomized controlled trial is needed.
Keywords: Cesarean delivery, labor management, arrest of dilation, arrest of descent, guidelines, neonatal morbidity, maternal morbidity
INTRODUCTION
In 2010 Zhang et al. and the Consortium on Safe Labor proposed a labor curve based on a contemporary cohort of parturients with normal neonatal outcomes.1 The main difference from the previous work of Friedman was that active labor begins at 6 cm dilation in both multiparous and nulliparous patients.1, 2 In an effort to stanch the increasing rate of cesarean delivery (CD), The American College of Obstetricians and Gynecologists (ACOG) and Society for Maternal-Fetal Medicine (SMFM) responded to the new labor curves with workshop recommendations in 2012 and an Obstetric Care Consensus statement on safe prevention of the primary CD in 2014.3, 4 It was proposed that the rate of CD could be lowered by avoiding the diagnosis of arrest of dilation before 6 cm.1 In the second stage, providers were to let multiparous patients push for at least 2 hours and nulliparous patients at least 3 hours.3
There has been controversy as to whether the new curves should be adopted.5–11 Furthermore, it is unclear to what degree the new labor curves have been implemented into clinical practice and what effect this may have had on CD rates.12 Change in clinical practice in medicine is slow.13–15 For instance, within obstetrics, the delay between discovery of the beneficial effects of antenatal corticosteroids and their adoption into routine practice has been well documented.16
We therefore aimed to investigate how and to what degree the new labor guidelines have been adopted within a single, tertiary care academic medical center where adoption of the new curve was encouraged through widespread education of residents and attending physicians from 2010 to the present. We tested the hypothesis that among low-risk patients laboring at term, rates of arrest of dilation disorders have decreased leading to a decrease in the rate of CD. We also hypothesized that in the second stage, pushing duration prior to diagnosis of arrest of descent has increased also leading to reduction in the rate of cesarean for this indication. As a secondary aim, we investigated changes in maternal and neonatal morbidity over the study period. Finally, we investigated providers’ attitudes and knowledge of the contemporary guidelines.
MATERIALS AND METHODS
Study Design and Population
This was a secondary analysis of a prospective cohort study of all patients laboring at or beyond 37 0/7 weeks at Washington University School of Medicine from 2010–2014. Low-risk patients admitted for either spontaneous or induced labor at ≥ 37 weeks’ gestation were included. Low-risk was defined as patients similar to those in the Consortium on Safe Labor cohort of parturients.1 We excluded women with a history of CD, multiple gestation, non-vertex presentation, fetal anomalies, or in utero fetal demise. Women presenting for scheduled CD were also excluded.
Data Collection
Clinical and demographic information was abstracted by formally trained obstetric research nurses. Intrapartum events including all cervical exams were obtained from the labor and delivery record. Race/ethnicity was assigned as African-American, Caucasian, Latina, or other based on patient report. Simplified Bishop Score was calculated prior to any cervical ripening by the admitting provider.17 Use of induction/augmentation agents including prostaglandins, Foley bulb, and oxytocin was recorded. The hospital uses a hybrid paper-electronic medical record which does not warn about possible labor disorders. It is possible to generate and review a graphic labor record/curve, but this is at the discretion of the provider.
Mode of delivery and indications for operative deliveries were abstracted from the delivery record. Information on comorbidities included hypertensive disorders as well as both pre-gestational and gestational diabetes. Gestational diabetes was defined as glucose ≥140 g/dL on a glucose tolerance test followed by at least 2 abnormal values on a 3-hour glucose test using the National Diabetes Data Group definitions.18 Since 2013, preeclampsia has been defined using the updated ACOG guidelines;19 prior to that it was defined based on blood pressure >140 mm Hg systolic or >90 mm Hg diastolic and proteinuria. The composite neonatal adverse outcome included death, hypoxic-ischemic encephalopathy, meconium aspiration syndrome, need for therapeutic hypothermia, intubation, oxygen therapy, ventilator support, suspected sepsis or any other condition requiring a stay in the Level IV or Level II nurseries. These diagnoses were made by the attending neonatologist. The National Institute of Child Health and Human Development criteria were used for diagnosis of hypoxic-ischemic encephalopathy.20 Meconium aspiration syndrome was diagnosed based on respiratory distress in the presence of meconium-stained amniotic fluid.21 Therapeutic hypothermia is employed in accordance with routine institutional guidelines.22 For the composite, only one morbidity was counted per neonate. We included suspected sepsis as a morbidity because it is associated with increased duration of membrane rupture and because even if the evaluation is negative, workup for sepsis is associated with increased neonatal evaluation and treatment.23, 24 Maternal morbidities included wound infection, fever, hemorrhage, transfusion, endometritis, or other severe morbidity as documented by the treating clinician.
The primary outcomes were rates of CD per year, indications for CD, and average cervical dilation at CD for arrest of dilation over the course of the study. Due to the very small amount of missing data, complete case analysis was used and imputation was not performed.
Statistical Analysis
Demographic and clinical characteristics were compared by year using chi-square or Fisher exact test for categorical variables. Continuous variables were assessed for normality with the Kolmogorov-Smirnov test and then ANOVA or Kruskal-Wallis tests were used as appropriate. Rates of CD were computed by year, and the Cochrane-Armitage test of trend was used to examine trend. As a sensitivity analysis, we also restricted these analyses to nulliparity as well as augmented/induced labor. Adjusted odds ratios (aOR) and 95% confidence intervals (CI) of CD by year were computed with logistic regression and potential confounders including maternal age, body mass index (BMI), race/ethnicity, nulliparity, labor type (spontaneous, augmented, or induced), use of prostaglandins, oxytocin, or Foley bulb, macrosomia (birthweight >4000g), and maternal diabetes or hypertensive disorders. Next, rates of indications for CD were determined and the Cochrane-Armitage test was used to test for trend.
To further examine specific labor management characteristics, the median and interquartile range (IQR) of cervical dilation in patients undergoing CD for arrest of dilation each year were calculated and the Cochrane-Armitage test used to test for trend. To examine if there was a change in the characteristics of labor progress over time, the time in hours spent at the last cervical dilation prior to CD for arrest of dilation was calculated. This was considered as the time between the first diagnosis of the maximum cervical dilation and the last time this exam occurred. The median and IQR of time in hours were calculated, and a generalized linear model used to test for trend.
We dichotomized CDs for arrest of dilation into cervical dilation at ≥6 cm or <6 cm, and examined changes in the rates of these deliveries with both crude analyses as well as analyses adjusted for the above-mentioned potential confounders. Since more than one potentially competing diagnosis was often recorded which could have been the overriding indication for CD (such as non-reassuring fetal status), we performed a sensitivity analysis restricted to those with a solitary diagnosis of arrest of dilation.
To examine second stage characteristics, we compared the median pushing time over the study period in patients diagnosed with arrest of descent, stratifying by parity. Finally, we examined crude rates and aORs of adverse maternal or neonatal outcomes by adjusting for the above-mentioned potential confounders. We also compared rates of 5-minute APGAR score <7.
To accompany our analyses of changes in labor management, we conducted a survey of obstetricians at our institution, including chief residents, Maternal-Fetal Medicine fellows, and generalist and Maternal-Fetal Medicine faculty. Participants were asked 5 questions regarding their understanding and practices of labor management since the release of the guidelines.
The study was approved by the Washington University in St. Louis Human Research Protection Office. The sample size was fixed due to the retrospective nature of the study. We included all women who met inclusion criteria, without an a priori sample size calculation. A p-value <0.05 was considered statistically significant. We did not adjust for multiple comparisons. Analyses were performed in SAS software (version 9.2; SAS Institute, Inc, Cary, NC).
RESULTS
Patient Characteristics
There were 7845 eligible patients, and patient characteristics are shown in Table 1. Maternal age increased slightly over the study period, and the rate of preeclampsia increased from 8% to 18% (p<0.001). The frequency of unfavorable cervical exam at admission and use of Foley bulb induction increased over time. Information on BMI was missing in 91 patients (1.15%), which was the covariate with the largest amount of missing information.
Table 1.
Baseline Characteristics
| Characteristic | 2010 n=1338 |
2011 n=1913 |
2012 n=1766 |
2013 n=1699 |
2014 n=1129 |
P |
|---|---|---|---|---|---|---|
| Maternal age, years | 25.2± 6.1 | 25.2± 6.0 | 25.6±5.8 | 25.7± 5.8 | 26.2± 6.0 | <0.001 |
| Gestational age at delivery, weeks | 39.3± 1.2 | 39.4± 1.2 | 39.3± 1.2 | 39.3± 1.2 | 39.3± 1.2 | 0.22 |
| Race/Ethnicity | <0.001 | |||||
| Black | 867 (64.8) | 1257 (65.7) | 1156 (65.5) | 1087 (64.0) | 717 (63.5) | |
| Caucasian | 291 (21.8) | 387 (20.2) | 394 (22.3) | 433 (25.5) | 282 (25.0) | |
| Latina | 103 (7.7) | 167 (8.7) | 119 (6.7) | 107 (6.3) | 53 (4.7) | |
| Other | 77 (5.8) | 102 (5.3) | 97 (5.5) | 72 (4.2) | 77 (6.8) | |
| Body mass index (kg/m2) | 32.0± 7.3 | 31.9± 7.1 | 32.1± 7.3 | 32.4± 7.4 | 32.3± 7.4 | 0.40 |
| Preeclampsia | 106 (7.9) | 166 (8.7) | 213 (12.1) | 200 (11.8) | 198 (17.5) | <0.001 |
| Gestational diabetes | 37 (2.8) | 59 (3.1) | 52 (2.9) | 58 (3.4) | 29 (2.6) | 0.73 |
| Pre-gestational diabetes | 13 (1.0) | 22 (1.2) | 19 (1.1) | 33 (1.9) | 21 (1.9) | 0.05 |
| Nulliparous | 627 (46.9) | 886 (46.3) | 775 (43.9) | 764 (45.0) | 529 (46.9) | 0.36 |
| Simplified Bishop Score ≤ 5 | 927 (69.3) | 1146 (60.0) | 1191 (67.5) | 1208 (72.2) | 856 (75.9) | <0.001 |
| Starting cervical dilation, cm | 3.0 (1.5, 4.5) | 3.5 (2.0, 5.0) | 3.0 (2.0, 4.5) | 3.0 (1.5, 4.0) | 3.0 (1.0, 4.0) | <0.001 |
| Regional anesthesia | 1192 (89.1) | 1713 (89.6) | 1579 (89.4) | 1541 (90.7) | 1037 (91.9) | 0.11 |
| Labor type | 0.002 | |||||
| Spontaneous | 395 (29.5) | 586 (30.6) | 501 (28.4) | 548 (32.3) | 338 (29.9) | |
| Augmented | 360 (26.9) | 549 (28.7) | 463 (26.2) | 433 (25.5) | 256 (22.7) | |
| Induced | 583 (43.6) | 778 (40.7) | 802 (45.4) | 718 (42.3) | 535 (47.4) | |
| Oxytocin use | 902 (67.4) | 1267 (66.2) | 1208 (68.4) | 1122 (66.0) | 771 (68.3) | 0.46 |
| Foley bulb use | 121 (9.0) | 187 (9.8) | 162 (9.2) | 194 (11.4) | 196 (17.4) | <0.001 |
| Prostaglandin use | 262 (19.6) | 372 (19.5) | 310 (17.6) | 321 (18.9) | 230 (20.4) | 0.37 |
| Birthweight, g | 3251±458 | 3246± 464 | 3240± 460 | 3250± 460 | 3236± 462 | 0.73 |
| Birthweight | ||||||
| >4000g | 65 (4.9) | 105 (5.5) | 98 (5.6) | 90 (5.3) | 67 (5.9) | 0.82 |
| Birthweight | ||||||
| <2500g | 79 (5.9) | 104 (5.4) | 89 (5.0) | 91 (5.4) | 64 (5.7) | 0.74 |
Data represented as mean ± standard deviation, n (%), or median (interquartile range)
Primary Outcomes
Figure 1 shows primary CD and arrest of dilation rates by year. There was no significant trend toward decreased arrest of dilation diagnoses (p-trend 0.39) or overall CD (p-trend 0.51). In analyses restricted to spontaneous/augmented labor, there were no differences in diagnoses of arrest of dilation (p-trend 0.58) or in CD rates (p-trend 0.40), which was also true in analyses restricted to nulliparous patients. Comparing each year to 2010, the adjusted analyses demonstrated no associations between year and CD (aOR for 2014: 0.97, 95%CI 0.77, 1.23). There were no significant changes in indications for CD across the study period (Table 2).
Figure 1. Cesarean Delivery and Arrest of Dilation Rates by Year.
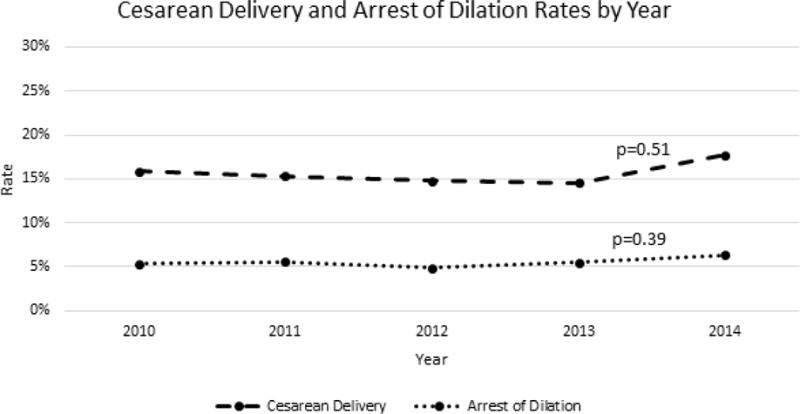
The rates of cesarean delivery and arrest of dilation did not change from 2010–2014.
Table 2.
Indications for Cesarean Delivery by Year
| Indication | 2010 (n=212) |
2011 (n=293) |
2012 (n=261) |
2013 (n=247) |
2014 (n=200) |
p-trend |
|---|---|---|---|---|---|---|
| Non-reassuring fetal status | 114 (53.8) | 176 (60.1) | 161 (61.7) | 140 (56.7) | 122 (61.0) | 0.36 |
| Arrest of dilatation | 72 (34.0) | 106 (36.2) | 86 (33.0) | 94 (38.1) | 72 (36.0) | 0.57 |
| Arrest of descent | 48 (22.6) | 48 (16.4) | 39 (14.9) | 37 (15.0) | 34 (17.0) | 0.12 |
| Other | 45 (21.2) | 39 (13.3) | 44 (16.9) | 42 (17.0) | 34 (17.0) | 0.68 |
Data represented as n(%)
Percentages add up to more than 100% as some patients had more than one indication for cesarean delivery.
Arrest of Dilation
There were 430 patients who underwent CD for arrest of dilation, and 70% of these (301 patients) were undergoing induction of labor (IOL). In patients undergoing CD for arrest of dilation, the median cervical dilation at the time of CD was unchanged at 5.5 cm in 2010 (IQR 4.8 cm, 7.5 cm) and 6.0 cm in 2014 (IQR 5.0 cm, 6.5 cm) (p-trend 0.94) (Table 3). In patients in spontaneous/augmented labor, the median cervical dilation at time of arrest of dilation diagnosis was 7.5 cm in 2010 (IQR 5.0 cm, 8.5 cm) and 6.0 cm in 2014 (IQR 5.8 cm, 7.0 cm) (p-trend 0.51). In IOL patients, the median cervical dilation at time of arrest of dilation was 5.0 cm in 2010 (IQR 5.0cm, 6.3cm) and 5.3 cm in 2014 (IQR 5.0 cm, 6.5 cm) (p-trend 0.94).
Table 3.
Characteristics of Patients with Arrest of Dilation (n=430)
| Year (n) | Time Spent at Final Cervical Dilation, hours | Cervical Dilation at Arrest Diagnosis, cm | Arrest of Descent Diagnosis with Dilation <6 cm, n |
|---|---|---|---|
| 2010 (72) | 3.8 (0.8, 6.0) | 5.5 (4.8, 7.5) | 37 (51.4) |
| 2011(106) | 2.6 (0.5, 4.9) | 6.0 (5.0, 7.5) | 45 (42.5) |
| 2012 (86) | 2.5 (0.9, 6.2) | 6.0 (5.0, 8.0) | 31 (36.1) |
| 2013(94) | 3.3 (1.7, 6.7) | 6.25 (5.0, 8.0) | 36 (38.3) |
| 2014 (72) | 5.2 (2.5, 8.0) | 6.0 (5.0, 6.5) | 35 (48.6) |
| p-trend | 0.022 | 0.94 | 0.56 |
Data represented as median (interquartile range) or n (%)
In patients diagnosed with arrest of dilation, there was a significant increase over the study period in the amount of time spent at last dilation, from 3.8h in 2010 to 5.2h in 2014 (p-trend 0.02) (Table 3). In patients undergoing IOL, the median time spent at the last cervical dilation prior to diagnosis of arrest of dilation was 4.0h in 2010 (IQR 1.0h, 6.5h) and 5.8h (IQR 2.8h, 8.1h) in 2014 (p-trend 0.047). There were 88 patients (20.5%) with arrest of dilation who had only one exam at the final cervical dilation.
There was no change in the frequency of patients diagnosed with arrest of dilation at <6 cm over the study period: 51.4% in 2010 and 48.6% in 2014 (p-trend 0.56), (Table 3). However, in these patients, the median time spent at the last cervical dilation was 4.0h (IQR 1.0h, 8.3h) in 2010 and 6.7h (IQR 1.2h, 9.6h) in 2014 (p-trend 0.046). In adjusted analyses there was no association between year of delivery and CD for arrest of dilation at <6 cm (aOR for 2014 vs. 2010 0.90, 95% CI 0.45, 1.80). The results were unchanged when restricted to cases in which the sole diagnosis was arrest of dilation (n=245).
Arrest of Descent
Over the study period there were 206 CDs performed for arrest of descent, 200 of which were in patients with epidurals. Arrest of descent was the indication for CD in 22.6% of CD in 2010 and 17.0% in 2014 (p-trend 0.12). In adjusted analyses the aOR for arrest of descent in 2014 compared to 2010 was 0.65 (95%CI 0.39, 1.11). The median pushing time in these patients increased in multiparous patients from 1.1h in 2010 (IQR 0.8, 2.2) to 3.4h in 2014 (IQR 2.0h, 4.4h), p-trend 0.009, although the numbers of multiparous patients with this diagnosis were small (n=44). In nulliparous patients (n=156), the median pushing time in patients diagnosed with arrest of descent was 2.7h in 2010 (IQR 2.0h, 3.8h) and 3.8h in 2014 (IQR 2.6h, 4.2h) which was not statistically significant (p-trend 0.09).
Secondary Outcomes
There was a significant trend towards increasing adverse neonatal and maternal outcomes over the study period (p<0.001 for each) (Table 4). The aOR for adverse maternal outcome for 2014 compared to 2010 was 1.66 (95%CI 1.27, 2.17), while the aOR of adverse neonatal outcome was 1.80 (95%CI 1.36, 2.36).
Table 4.
Maternal and Neonatal Outcomes
| Outcome | 2010 | 2011 | 2012 | 2013 | 2014 | p-trend |
|---|---|---|---|---|---|---|
| Adverse neonatal outcome | 107 (8.0) | 165 (8.3) | 154 (8.7) | 183 (10.8) | 153 (13.6) | <0.001 |
| Maternal complication | 113 (8.5) | 203 (10.6) | 208 (11.8) | 182 (10.7) | 153 (13.6) | <0.001 |
Data represented as n (%)
Rates of suspected neonatal sepsis significantly increased from 5.7% in 2010 to 10.8% in 2014 (p-trend <0.001), as did the rate of respiratory distress (from 3.7% in 2010 to 5.0% in 2014, p-trend 0.03). Although overall there was no significant association between a longer time spent at final cervical dilation in patients diagnosed with arrest of dilation and development of neonatal morbidity (p 0.48), the median time in patients without neonatal respiratory distress was 3.3h (IQR 1.0h, 6.2h) and in patients with neonatal respiratory distress was 5.5h (IQR 2.1h, 9.6h) (p 0.044). There was also no association between increased second stage length prior to CD for arrest of descent and neonatal morbidity (p 0.80). There was no change in percentage of neonates with 5-minute APGAR score <7 at 5 minutes of life over the study period (p-trend 0.25).
There was no association between amount of time spent pushing prior to arrest of descent diagnosis and maternal morbidity (p 0.86) or in the amount of time spent at last cervical dilation prior to arrest of dilation diagnosis (p 0.46). The majority of the increase in maternal morbidity was due to an increase in “other” morbidity in 2014 compared to other years. Considering only transfusion, hemorrhage, or infectious morbidity, there was no difference in rates of maternal morbidity over the course of the study period (p-trend 0.96).
Survey of Providers
All 16 providers who were asked to participate in the survey responded. There was unanimous agreement that “our understanding of normal labor has changed over the last 10 years.” All respondents agreed that changes included the timing of the active phase, length of the latent phase, and shape of the labor curve. Respondents indicated that active labor beings at 6 cm. When asked what they would do “if a patient has adequate contractions on oxytocin and is unchanged at 4 cm after 3 hours,” all respondents indicated they would continue current management as opposed to diagnosing arrest of dilation.
COMMENT
Principal Findings
We found that between 2010 and 2014 there was no change in the CD rate or arrest of dilation rate in low-risk patients at our institution. However, there was an increase in time at most advanced cervical dilation prior to diagnosis of arrest of dilation between 2010 and 2014. There was no increase in the median cervical dilation at arrest of dilation diagnosis. However, in patients being diagnosed with arrest of dilation at <6 cm, the time spent at the most advanced cervical dilation increased by a median 2.7 hours. There was an increased pushing time prior to diagnosis of arrest of descent in multiparous but not nulliparous patients. Rates of neonatal and maternal morbidities increased over the study period. Providers polled unanimously indicated agreement with the ACOG/SMFM guidelines.
Strengths and Limitations
A strength of our study is that data were collected prospectively by trained obstetrical research nurses as part of a large ongoing cohort study. Because we had information on each cervical exam we were able to accurately ascertain duration of time at maximal cervical dilation and cervical dilation at time of CD. Furthermore, the detailed data permitted us to evaluate and adjust for multiple potentially confounding factors.
As with any study, there are limitations to be considered. Baseline characteristics including IOL rates differed throughout the study period. Although we controlled for confounding, there is the possibility of residual confounding by unmeasured factors. Our sample size was fixed and our ability to detect small changes in the CD rate may have been limited. Additionally, the relatively small number of CDs for arrest of dilation and arrest of descent may have limited our power to detect changes over time. A post-hoc calculation shows that to detect a statistically significant change (with 80% power) in the CD rate from the observed 15.8% in 2010 to 17.7% in 2014, there would need to be 6048 patients in each year. Although post-hoc power analysis is not always advisable, this does indicate that our findings should be investigated in a larger Labor and Delivery unit or in a multicenter study.25 Notably, the majority of arrest of dilation cases occurred in patients undergoing IOL, and providers may have used “arrest of dilation” as a shorthand for “failed induction.” However, there were also no changes in the rates of arrest of dilation in the spontaneous/augmented laboring patients. Furthermore, “failed induction” was listed by providers as a separate and non-overlapping diagnosis in many cases. Our analysis covers the period from 2010–2014, which is the year the guidelines were formally released.3 Further analyses will be needed now that 3 years have passed to see what further impact the guidelines may have had.
Interpretation
Although there were significant changes in labor management over the study period, there was no change in CD rate in our study population. The CD rate in the United States has remained relatively constant since 2009, although the “low-risk” CD rate declined from 28% in 2009 to 25.8% in 2015.26 Our study is one of the first to examine the impact of the new labor guidelines at the hospital level. A similar study from Pennsylvania examined the adoption of the new labor guidelines in nulliparous patients; researchers found a decrease in cesarean rates from 26.9% to 18.8% and the frequency of CD for arrest of dilation dropped from 7.1% to 1.1% after implementation of the new guidelines.12 There are multiple possible explanations as to why we did not confirm these findings in our study. Perhaps most important is the difference in patient characteristics, notably obesity. While the average BMI in their study was 24.6 kg/m2 for the pre-intervention group, our mean BMI was 32.1 kg/m2. Multiple studies have shown that labor is longer in obese parturients, and thus the applicability of the new guidelines to this group may be questionable.27, 28 Secondly, we included multiparous patients as well as nulliparous patients, and the effects of these guidelines on patients of differing parity is unknown. Furthermore, their primary outcome was the CD rate among induced or augmented patients, while ours was the total CD rate. Our study also incorporated a far greater number of patients and took place over 5 years. Limiting the study period to a small number of patients immediately before and after the adoption of a labor management guideline may represent a different scenario than trying to capture labor management patterns in a large labor and delivery unit over time. Notably in their study Wilson-Leedy et al. found a decrease in maternal morbidity but a possible increase in neonatal morbidity.12 The effects of the new labor guidelines on morbidity remain to be determined.
There was an increase in the amount of time spent at the last cervical dilation prior to CD for arrest of dilation over the study period, without any associated change in median cervical dilation in patients diagnosed with arrest of dilation or in CD rates. This might indicate that although providers were more lenient in allowing labor to continue at the maximum dilation, this approach may not lead to a reduction in CD rates. The same was true of time spent pushing: an increase in time until arrest of descent diagnosis did not correspond to a decrease in CD rates.
Although there were major changes in labor management in our institution, there was still a high rate of CD for arrest of dilation at <6 cm throughout the study period. It is well-known that clinical practice often lags behind both changes in primary evidence as well as clinical guidelines.13–16 Reasons for failure to follow guidelines include knowledge gaps, disagreement with the guidelines, presence of external barriers, and the need to overcome inertia.13 Studies of dissemination and implementation science have demonstrated a number of effective approaches to encourage uptake of new guidelines into clinical practice.29 These include alert systems and templates, neither of which have been specifically used at our institution in regards to the new labor guidelines.29 Peer review has been tried in efforts to lower the cesarean delivery rate with variable success, although not in our institution.30–32
Of note, we found increasing rates of both maternal and neonatal morbidity over the study period even after adjustment for multiple potential confounders including preeclampsia. There was an increase in neonatal respiratory morbidity in patients with longer periods of arrested dilation, although overall there were no associations between length of arrest and maternal or neonatal morbidity. Some have posited that adoption of the Consensus guidelines could result in increased rates of morbidity, which may be reflected in our study findings.6, 8 In particular there has been controversy regarding the recommendation to extend the second stage, as prolonged second stage has been associated with maternal and neonatal morbidity.33–38
The reason for the dramatic increase in suspected sepsis is unclear, but may be due to changes in neonatology practice as opposed to an actual increase in the rate of true sepsis. The rate of preeclampsia increased in our population. This is likely due to the change in diagnostic criteria that occurred during the study period.19 Severe maternal morbidity has been increasing throughout the United States, and thus our findings deserve further inquiry.39, 40 Since the driver of the increase in maternal morbidity in 2014 was “other,” this may be due to ascertainment bias in our data collection system. Due to the observational nature of our study we cannot draw causal inferences with regard to the association between the change in labor practices and changes in morbidity. Considering the increase in morbidity as well as the lack of effect on CD rates seen in our study, a cost-benefit analysis is needed.
Conclusion
Despite significant changes in labor management that have occurred over the initial years since publication of the Zhang labor curves and associated guidelines, there was no decrease in the primary CD rate at this single tertiary care institution, and there has been an increase in maternal and neonatal morbidity. A randomized controlled trial is needed to fully ascertain the effect of the new guidelines on CD rates and morbidities.
Condensation.
Despite changes in labor management, there was no reduction in the cesarean delivery rate and there was an increase in morbidity in our institution.
Acknowledgments
Funding: This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01: HD 06161619-01A1). The funder had no role in the study design, collection, analysis or interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: The authors report no conflict of interest.
References
- 1.Zhang J, Landy HJ, Branch DW, Burkman R, Haberman S, Gregory KD, et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol. 2010;116(6):1281–7. doi: 10.1097/AOG.0b013e3181fdef6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Friedman EA. Primigravid labor; a graphicostatistical analysis. Obstet Gynecol. 1955;6(6):567–89. doi: 10.1016/s0029-7844(02)02398-0. [DOI] [PubMed] [Google Scholar]
- 3.American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine. Obstetric care consensus no. 1: safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014;123(3):693–711. doi: 10.1097/01.AOG.0000444441.04111.1d. [DOI] [PubMed] [Google Scholar]
- 4.Spong CY, Berghella V, Wenstrom KD, Mercer BM, Saade GR. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol. 2012;120(5):1181–93. doi: 10.1097/aog.0b013e3182704880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dietz HP, Campbell S. Toward normal birth-but at what cost? Am J Obstet Gynecol. 2016;215(4):439–44. doi: 10.1016/j.ajog.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 6.Cohen WR, Friedman EA. Misguided guidelines for managing labor. Am J Obstet Gynecol. 2015;212(6):753 e1–3. doi: 10.1016/j.ajog.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Zhang J, Troendle J, Grantz KL, Reddy UM. Statistical aspects of modeling the labor curve. Am J Obstet Gynecol. 2015;212(6):750 e1–4. doi: 10.1016/j.ajog.2015.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen WR, Friedman EA. Perils of the new labor management guidelines. Am J Obstet Gynecol. 2015;212(4):420–7. doi: 10.1016/j.ajog.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 9.Laughon SK, Branch DW, Beaver J, Zhang J. Changes in labor patterns over 50 years. Am J Obstet Gynecol. 2012;206(5):419 e1–9. doi: 10.1016/j.ajog.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang J, Troendle J, Mikolajczyk R, Sundaram R, Beaver J, Fraser W. The natural history of the normal first stage of labor. Obstet Gynecol. 2010;115(4):705–10. doi: 10.1097/AOG.0b013e3181d55925. [DOI] [PubMed] [Google Scholar]
- 11.Cohen WR. The natural history of the normal first stage of labor. Obstet Gynecol. 2010;116(3):772. doi: 10.1097/AOG.0b013e3181ee9fdf. author reply -3. [DOI] [PubMed] [Google Scholar]
- 12.Wilson-Leedy JG, DiSilvestro AJ, Repke JT, Pauli JM. Reduction in the Cesarean Delivery Rate After Obstetric Care Consensus Guideline Implementation. Obstet Gynecol. 2016;128(1):145–52. doi: 10.1097/AOG.0000000000001488. [DOI] [PubMed] [Google Scholar]
- 13.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458–65. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 14.Morris ZS, Wooding S, Grant J. The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med. 2011;104(12):510–20. doi: 10.1258/jrsm.2011.110180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Westfall JM, Mold J, Fagnan L. Practice-based research–“Blue Highways” on the NIH roadmap. JAMA. 2007;297(4):403–6. doi: 10.1001/jama.297.4.403. [DOI] [PubMed] [Google Scholar]
- 16.Bonanno C, Wapner RJ. Antenatal corticosteroids in the management of preterm birth: are we back where we started? Obstet Gynecol Clin North Am. 2012;39(1):47–63. doi: 10.1016/j.ogc.2011.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Laughon SK, Zhang J, Troendle J, Sun L, Reddy UM. Using a simplified Bishop score to predict vaginal delivery. Obstet Gynecol. 2011;117(4):805–11. doi: 10.1097/AOG.0b013e3182114ad2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Expert Committee on the Diagnosis Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):S5–20. doi: 10.2337/diacare.26.2007.s5. [DOI] [PubMed] [Google Scholar]
- 19.American College of Obstetricians and Gynecologists. Hypertension in pregnancy. Washington, DC: American College of Obstetricians and Gynecologists; 2013. Task Force on Hypertension in Pregnancy. [DOI] [PubMed] [Google Scholar]
- 20.Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med. 2005;353(15):1574–84. doi: 10.1056/NEJMcps050929. [DOI] [PubMed] [Google Scholar]
- 21.Lindenskov PH, Castellheim A, Saugstad OD, Mollnes TE. Meconium aspiration syndrome: possible pathophysiological mechanisms and future potential therapies. Neonatology. 2015;107(3):225–30. doi: 10.1159/000369373. [DOI] [PubMed] [Google Scholar]
- 22.Tuuli MG, Stout MJ, Macones GA, Cahill AG. Umbilical Cord Venous Lactate for Predicting Arterial Lactic Acidemia and Neonatal Morbidity at Term. Obstet Gynecol. 2016;127(4):674–80. doi: 10.1097/AOG.0000000000001339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higgins RD, Saade G, Polin RA, Grobman WA, Buhimschi IA, Watterberg K, et al. Evaluation and Management of Women and Newborns With a Maternal Diagnosis of Chorioamnionitis: Summary of a Workshop. Obstet Gynecol. 2016;127(3):426–36. doi: 10.1097/AOG.0000000000001246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Herbst A, Kallen K. Time between membrane rupture and delivery and septicemia in term neonates. Obstet Gynecol. 2007;110(3):612–8. doi: 10.1097/01.AOG.0000277632.36186.84. [DOI] [PubMed] [Google Scholar]
- 25.Hoenig JM, Heisey DM. The abuse of power. The American Statistician. 2001;55(1):19–24. [Google Scholar]
- 26.Martin JA, Hamilton BE, Osterman MJ. Births in the United States, 2015. NCHS Data Brief. 2016;(258):1–8. [PubMed] [Google Scholar]
- 27.Norman SM, Tuuli MG, Odibo AO, Caughey AB, Roehl KA, Cahill AG. The effects of obesity on the first stage of labor. Obstet Gynecol. 2012;120(1):130–5. doi: 10.1097/AOG.0b013e318259589c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kominiarek MA, Zhang J, Vanveldhuisen P, Troendle J, Beaver J, Hibbard JU. Contemporary labor patterns: the impact of maternal body mass index. Am J Obstet Gynecol. 2011;205(3):244 e1–8. doi: 10.1016/j.ajog.2011.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flodgren G, Hall AM, Goulding L, Eccles MP, Grimshaw JM, Leng GC, et al. Tools developed and disseminated by guideline producers to promote the uptake of their guidelines. Cochrane Database Syst Rev. 2016;(8):CD010669. doi: 10.1002/14651858.CD010669.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bickell NA, Zdeb MS, Applegate MS, Roohan PJ, Sui AL. Effect of external peer review on cesarean delivery rates: a statewide program. Obstet Gynecol. 1996;87(5 Pt 1):664–7. doi: 10.1016/0029-7844(96)00024-5. [DOI] [PubMed] [Google Scholar]
- 31.Liang WH, Yuan CC, Hung JH, Yang ML, Yang MJ, Chen YJ, et al. Effect of peer review and trial of labor on lowering cesarean section rates. J Chin Med Assoc. 2004;67(6):281–6. [PubMed] [Google Scholar]
- 32.Elferink-Stinkens PM, Brand R, Amelink-Verburg MP, Merkus JM, den Ouden AL, Van Hemel OJ. Randomised clinical trial on the effect of the Dutch obstetric peer review system. Eur J Obstet Gynecol Reprod Biol. 2002;102(1):21–30. doi: 10.1016/s0301-2115(01)00553-x. [DOI] [PubMed] [Google Scholar]
- 33.Gimovsky AC, Berghella V. Prolonged Second Stage: What Is the Optimal Length? Obstet Gynecol Surv. 2016;71(11):667–74. doi: 10.1097/OGX.0000000000000368. [DOI] [PubMed] [Google Scholar]
- 34.Gimovsky AC, Berghella V. Randomized controlled trial of prolonged second stage: extending the time limit vs usual guidelines. Am J Obstet Gynecol. 2016;214(3):361 e1–6. doi: 10.1016/j.ajog.2015.12.042. [DOI] [PubMed] [Google Scholar]
- 35.Grobman WA, Bailit J, Lai Y, Reddy UM, Wapner RJ, Varner MW, et al. Association of the Duration of Active Pushing With Obstetric Outcomes. Obstet Gynecol. 2016;127(4):667–73. doi: 10.1097/AOG.0000000000001354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laughon SK, Berghella V, Reddy UM, Sundaram R, Lu Z, Hoffman MK. Neonatal and maternal outcomes with prolonged second stage of labor. Obstet Gynecol. 2014;124(1):57–67. doi: 10.1097/AOG.0000000000000278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leveno KJ, Nelson DB, McIntire DD. Second-stage labor: how long is too long? Am J Obstet Gynecol. 2016;214(4):484–9. doi: 10.1016/j.ajog.2015.10.926. [DOI] [PubMed] [Google Scholar]
- 38.Rouse DJ, Weiner SJ, Bloom SL, Varner MW, Spong CY, Ramin SM, et al. Second-stage labor duration in nulliparous women: relationship to maternal and perinatal outcomes. Am J Obstet Gynecol. 2009;201(4):357 e1–7. doi: 10.1016/j.ajog.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012;120(5):1029–36. doi: 10.1097/aog.0b013e31826d60c5. [DOI] [PubMed] [Google Scholar]
- 40.Grobman WA, Bailit JL, Rice MM, Wapner RJ, Reddy UM, Varner MW, et al. Frequency of and factors associated with severe maternal morbidity. Obstet Gynecol. 2014;123(4):804–10. doi: 10.1097/AOG.0000000000000173. [DOI] [PMC free article] [PubMed] [Google Scholar]


