Abstract
Background
Adjuvant therapy after breast cancer surgery decreases recurrence and increases survival, yet not all women receive and complete it. Previous research has suggested that distrust in medical institutions plays a role in who initiates adjuvant treatment, but has not assessed treatment completion treatment, nor the potential mediating role of physician distrust.
Methods
Women listed in Pennsylvania and Florida cancer registries, who were under the age of 65 when diagnosed with localized invasive breast cancer between 2005 and 2007, were surveyed by mail in 2007-2009. Survey participants self-reported: demographics; cancer stage and treatments; treatment discordance, as defined by not following their surgeon or oncologist treatment recommendation; healthcare system distrust, and physician trust. Age and cancer stage were verified against cancer registry records. Logistic regression assessed the relationship between highest and lowest tertiles of healthcare system distrust and the dichotomous outcome of treatment discordance, controlling for demographics and clinical treatment factors, and testing for mediation by physician trust.
Results
Of the 2,754 participants, 30.2% (n=832) reported not pursing at least one recommended treatment. The mean age was 52. Patients in the highest tertile of healthcare system distrust were 22% more likely to report treatment discordance than the lowest tertile; physician trust did not mediate the association between healthcare system distrust and treatment discordance.
Conclusions
Healthcare system distrust is positively associated with treatment discordance, defined as failure to initiate or complete physician recommended adjuvant treatment after breast cancer.
Impact
Interventions should test whether or not resolving institutional distrust reduces treatment discordance.
Keywords: distrust, breast cancer, adjuvant treatment, USA
Introduction
Adjuvant therapy after breast cancer surgery, which includes chemotherapy, radiation therapy, and hormone therapy (1), has been successful in decreasing recurrence and increasing survival after breast cancer (2), yet not all women choose to pursue adjuvant therapy or complete the full regimen of treatment (3-6). Understanding the determinants of acceptance of adjuvant therapy is important to maximize the impact of this effective therapy on breast cancer mortality. One potentially important and modifiable factor that may influence receipt of adjuvant therapy is healthcare related distrust (3).
Healthcare system distrust includes subdomains of values and competence: values distrust refers to the fidelity, honesty, and belief that the trusted party will act in the best interest of the patient, while competence distrust refers to the perceptions of the trusted party’s ability and knowledge to perform in the expected way (7). Healthcare system distrust is a form of institutional trust related to the institutions of the health care system (e.g. hospitals, insurers, pharmaceutical companies), in contrast with physician trust, which is a form of interpersonal trust related to a specific physician (8-12). Although it is widely accepted that health care system and physician trust are likely to be correlated, it is not known whether the effect of health care system distrust on acceptance of recommended therapies is mediated by physician trust or if there is a distinct effect of health care system distrust beyond physician trust.
Relatively little is currently known about the relationship between healthcare system distrust and cancer treatment. A previous study of distrust and adjuvant cancer treatment (3) found that distrust in medical institutions was associated with increased risk of not initiating adjuvant treatment in a sample of 258 early stage (Stage I and II) breast cancer patients from one urban area. However, that study did not include the following in their analysis: which treatments were recommended by the physician, the extent to which physician distrust mediated the relationship between healthcare system distrust and cancer treatment, and an assessment of those who may have initiated treatment but did not fully adhere to the treatment plan. Other studies of distrust among women with a history of breast cancer have focused on healthcare system distrust and: mental health or psychosocial outcomes (13), quality of care (14,15), greater emotional, physical, financial, and sexual problems after treatment (16), less comfort with the use of de-identified information from medical records for research (17), less endorsement of the necessity of adjuvant chemotherapy (18); and provider distrust and quality of care (19).
The current study was designed to answer two related questions: Is healthcare system distrust associated with whether or not patients follow their physician’s recommendations for adjuvant treatment after breast cancer; and does physician trust mediate the relationship between healthcare system distrust and receipt of adjuvant treatment? It expands on prior work by including a large population based sample in two different US states, Pennsylvania and Florida, based on physician recommendations for several adjuvant treatments with explicit testing of the potential mediating role of physician distrust, and assesses patients who did not complete the full treatment plan. To our knowledge, it is the largest study of healthcare system distrust among women with a history of breast cancer and adds innovation of recruiting through a cancer registry to survey participants about healthcare system distrust.
Materials and Methods
Study Sample
The data for the present analysis were obtained from a large, population-based study designed to assess the racial differences in breast cancer treatment among women, including the use of BRCA1/2 testing. Between January 1, 2007 and December 31, 2009, women identified through Pennsylvania and Florida cancer registries were mailed paper surveys. As a study on racial differences in cancer treatment, these states were ideal due to the size, racial diversity of their populations, and the ability to recruit patients directly from cancer registry files. Study inclusion criteria included: biological female; localized invasive breast cancer; lobular or ductal histology; age under 65 at the time of diagnosis; lived in one of the two states (i.e., PA or FL); and diagnosed between January 1, 2005 and December 31, 2007. Exclusion criteria included: over 65 years of age (due to lower prevalence of BRCA1/2 mutations in that population); cognitive impairment; unable to speak English or Spanish; diagnosis at autopsy; and metastatic disease at presentation. The overall response rate was 61% (62% among white women, 58% among black women) (20). The study was approved by University of Pennsylvania’s Institutional Review Board, Florida Cancer Registry IRB, and Pennsylvania Cancer Registry. Completion of the questionnaire was considered implicit informed consent.
Treatment Discordance
The outcome of cancer treatment discordance was defined as any difference in the treatment that a patient reported receiving compared to the treatment that the patient reported was recommended to receive by her treating surgeon or oncologist at diagnosis. Self-report of breast cancer treatment has been validated as over 90% accurate (21). Patients reported “yes/no” about treatment recommendation and use of radiation therapy, chemotherapy, and hormonal therapy separately for each type of treatment and for surgeon and then oncologist. A combined measure of any treatment discordance was defined as the presence of discordance between treatment received and treatment recommended for any of the three treatments. If a patient was not recommended for a particular type of adjuvant treatment, she was not considered discordant. Patients who were missing an overall discordance outcome (n=24) were excluded.
Covariates
Participants completed the validated 9-item Health Care System Distrust scale (healthcare system distrust (8,11), which measures of domains of values and competence distrust on a 5-point agreement scale (1 = strongly disagree, 5 = strongly agree), which ranges from 9 to 45. The measure has acceptable construct validity (16) and high internal consistency (α=0.84 in the current sample). Physician trust was measured with the validated 7-item Trust in Physician Scale (22), (α=0.82 in the current sample) on a 7-point agreement scale (1=strongly disagree, 7=strongly agree), which ranges from 7 to 49. Participants provided information on socio-demographic factors, including age, race, ethnicity, income, education, marital status, employment status, health insurance status, and state of residence at time of diagnosis, and clinical treatment factors, including stage of breast cancer, surgical removal of cancer, and recurrence. Age and cancer stage were verified against cancer registry records.
Participant data were not included in the analysis if the participant: did not receive surgical treatment for breast cancer (n=15), had metastatic (stage 4) breast cancer (n=24), or were missing data on the key covariates (n=318).
Statistical Analysis
Descriptive statistics were calculated overall and by discordance status; comparisons of discordance were tested using chi-square and two-sample t-tests, as appropriate. Bivariate and adjusted ordinal logistic regression models assessed which covariates were significantly associated with healthcare system distrust. A logistic regression model was generated to assess the relationship between tertiles of low, medium, and high healthcare system distrust and the dichotomous outcome of discordance, controlling for demographic and clinical treatment factors. Separate models assessed (1) associations between healthcare system distrust and treatment discordance for chemotherapy, radiation therapy, and hormone therapy as separate outcomes; and (2) as a sensitivity analysis, oncologist and surgeon’s recommendations were explored as separate outcomes in independent models, to assess if findings were robust among patients who were fully concordant with one physician but not the other. Tests of physician trust as a potential mediator between healthcare system distrust and discordance were assessed using Barron & Kenney’s criteria for mediation (23,24), to test whether or not: (a) healthcare system distrust, the independent variable, is associated with physician trust, the mediator; (b) healthcare system distrust is associated with treatment discordance, the dependent variable; and (c) physician trust completely or partially attenuates the association between healthcare system distrust and treatment discordance (24). Bootstrapped estimates of standard errors and confidence intervals of direct and indirect effects were calculated. Statistical significance was assessed at p<0.05. Analyses were performed using Stata 14.1.
Results
As shown in Table 1, a total of 2,754 women were included in the final analytic sample, of which 69.8% (n=1,922) reported always receiving the cancer treatments their surgeon or oncologist recommended, and 30.2% (n=832) reported not pursing at least one recommended treatment. When considering each treatment separately, 10% were discordant with radiation treatment; 11% were discordant with chemotherapy; and 18% were discordant with hormone therapy. The mean age was 52. The majority of participants were White (69%) or Black (27%), and Non-Hispanic (94%). Nearly three-quarters of the sample made over $30,000, and had at least some college education. The majority of participants were married (66%), employed for wages (58%), and had health insurance (95%). Roughly half of participants had Stage 1 cancer at diagnosis, with 45% at Stage 2 and 6% at Stage 3. A little more than half the participants were from Florida (53%).
Table 1.
Baseline Characteristics by Outcome
| Overall | Non-Discordant | Discordant | |||||
|---|---|---|---|---|---|---|---|
| N = 2,754 | n = 1,922 (69.8%) | n = 832 (30.2%) | |||||
| N | % | N | % | N | % | P value | |
| Health Care System Distrust | 0.003 | ||||||
| Tertile 1 + Tertile 2 | 1,871 | 67.9 | 1,339 | 69.7 | 532 | 63.9 | |
| Tertile 3 | 832 | 32.1 | 583 | 30.3 | 300 | 36.1 | |
| Physician Trust Tertiles | 0.26 | ||||||
| Tertile 1 + Tertile 2 | 1,992 | 72.3 | 1,373 | 71.7 | 614 | 73.8 | |
| Tertile 3 | 762 | 27.7 | 544 | 28.3 | 218 | 26.2 | |
| Race | 0.36 | ||||||
| White | 1,888 | 68. 6 | 1,313 | 68.3 | 575 | 69.1 | |
| Black | 746 | 27.1 | 531 | 27.6 | 215 | 25.8 | |
| Other | 120 | 4.4 | 78 | 4.1 | 42 | 5.1 | |
| Hispanic | 0.92 | ||||||
| Non-Hispanic | 2,590 | 94.1 | 1,807 | 94.0 | 783 | 94.1 | |
| Hispanic | 164 | 6.0 | 115 | 5.9 | 49 | 5.9 | |
| Income | 0.17 | ||||||
| < $10,000 | 185 | 6.7 | 140 | 7.3 | 45 | 5.4 | |
| $10,001 to $30,000 | 521 | 19.1 | 368 | 19.2 | 153 | 18.4 | |
| $30,001 to $70,000 | 948 | 34.4 | 643 | 33.5 | 305 | 36.7 | |
| > $70,000 | 1,100 | 39. 9 | 771 | 40.1 | 329 | 39.5 | |
| Education | 0.34 | ||||||
| High school grad or less | 699 | 25.4 | 503 | 26.2 | 196 | 23.6 | |
| Some college | 957 | 34.8 | 658 | 34.2 | 299 | 35.9 | |
| College grad or more | 1,098 | 39.9 | 761 | 39.6 | 337 | 40.5 | |
| Marital Status | 0.06 | ||||||
| Not married or coupled | 926 | 33.6 | 625 | 32.5 | 301 | 36.2 | |
| Married or coupled | 1,828 | 66.4 | 1,297 | 67.5 | 531 | 63.8 | |
| Employment Status | 0.36 | ||||||
| Employed for wages | 1,585 | 57.6 | 1,117 | 58.1 | 468 | 56.3 | |
| Not employed for wages | 1,169 | 42.5 | 805 | 41.9 | 364 | 43.8 | |
| Insurance Status | 0.79 | ||||||
| Uninsured | 141 | 5.1 | 97 | 5.0 | 44 | 5.3 | |
| Insured | 2,613 | 94.9 | 1,825 | 95.0 | 788 | 94.7 | |
| Stage at diagnosis | < .001 | ||||||
| Stage 1 | 1,365 | 49.6 | 897 | 46.7 | 468 | 55.3 | |
| Stage 2 | 1,228 | 44.6 | 899 | 46.8 | 329 | 39.5 | |
| Stage 3 | 161 | 5.9 | 126 | 6.6 | 35 | 4.2 | |
| State | 0.003 | ||||||
| Florida | 1,446 | 52.5 | 973 | 50.6 | 473 | 56.9 | |
| Pennsylvania | 1,308 | 47.5 | 949 | 49.4 | 359 | 43.2 | |
|
| |||||||
| Mean | SD | Mean | SD | Mean | SD | P value | |
|
|
|||||||
| Age (in years) | 52 | 10 | 52 | 10 | 53 | 10 | 0.04 |
The mean healthcare system distrust score was 28 (SD=3; range 9-40), while the mean physician trust score was 29 (SD=4; range 9-35). Bivariate models suggested that greater healthcare system distrust was significantly associated with older age, being Black, having attended some college, and being employed, while less healthcare system distrust was associated with greater physician trust, being married, having health insurance, and living in Pennsylvania. Only marital status, being employed, physician trust, and living in Pennsylvania were still associated with distrust in a fully adjusted model (Table 2). Participants reporting treatment discordance were significantly in the top tertile of healthcare system distrust (p=0.003) as well as being more likely to be older (p=0.04), be diagnosed at Stage 1 (p<0.001), and live in Florida (p=0.003). In contrast, physician trust was not a significant predictor of discordance (p=0.49). Although healthcare system distrust was significantly associated with discordance (p=0.03) and physician trust (p<0.001) (Figure 1), a mediation analysis (Table 3: Models A & B) suggested that physician trust was not a mediator of the relationship between healthcare system distrust and treatment discordance (total indirect OR=1.00 [1.00,1.01]). Thus, rather than treat physician trust as a mediator, it was included in the final model as a covariate.
Table 2.
Factors Associated with Healthcare System Distrust: Ordinal Logistic Regression of Healthcare System Distrust Tertiles
| Bivariate Models | Adjusted Model | |||||
|---|---|---|---|---|---|---|
| OR | SE | P | OR | SE | P | |
| Physician Trust Tertiles | ||||||
| Tertile 1 & Tertile 2 | Ref | Ref | ||||
| Tertile 3 | 0.56 | 0.05 | <0.001 | 0.56 | 0.06 | <0.001 |
| Age | 1.00 | 0.004 | 0.04 | 1.00 | 0.005 | 0.70 |
| Race | ||||||
| White | Ref | Ref | ||||
| Black | 1.31 | 0.12 | 0.003 | 1.13 | 0.11 | 0.21 |
| Other | 1.14 | 0.23 | 0.67 | 1.05 | 0.22 | 0.82 |
| Hispanic/Latino | 0.88 | 0.15 | 0.48 | 0.80 | 0.15 | 0.24 |
| Income | ||||||
| < $10,000 | Ref | Ref | ||||
| $10,001 to $30,000 | 1.40 | 0.25 | 0.07 | 1.53 | 0.30 | 0.03 |
| $30,001 to $70,000 | 1.27 | 0.22 | 0.16 | 1.64 | 0.32 | 0.01 |
| > $70,000 | 0.96 | 0.17 | 0.82 | 1.40 | 0.29 | 0.12 |
| Education | ||||||
| High school grad or less | Ref | Ref | ||||
| Some college | 1.32 | 0.14 | 0.009 | 1.40 | 0.15 | 0.003 |
| College grad or more | 1.06 | 0.11 | 0.60 | 1.20 | 0.14 | 0.13 |
| Married or coupled | 0.78 | 0.07 | 0.003 | 0.80 | 0.08 | 0.02 |
| Not employed for wages | 1.28 | 0.10 | 0.002 | 1.30 | 0.12 | 0.004 |
| Health Insurance | 0.69 | 0.12 | 0.03 | 0.74 | 0.14 | 0.11 |
| Stage at diagnosis | ||||||
| Stage 1 | Ref | Ref | ||||
| Stage 2 | 0.85 | 0.07 | 0.06 | 0.84 | 0.07 | 0.05 |
| Stage 3 | 1.09 | 0.19 | 0.62 | 1.09 | 0.20 | 0.65 |
| State | ||||||
| Florida | Ref | Ref | ||||
| Pennsylvania | 0.71 | 0.06 | <0.001 | 0.73 | 0.06 | <0.001 |
Figure 1.
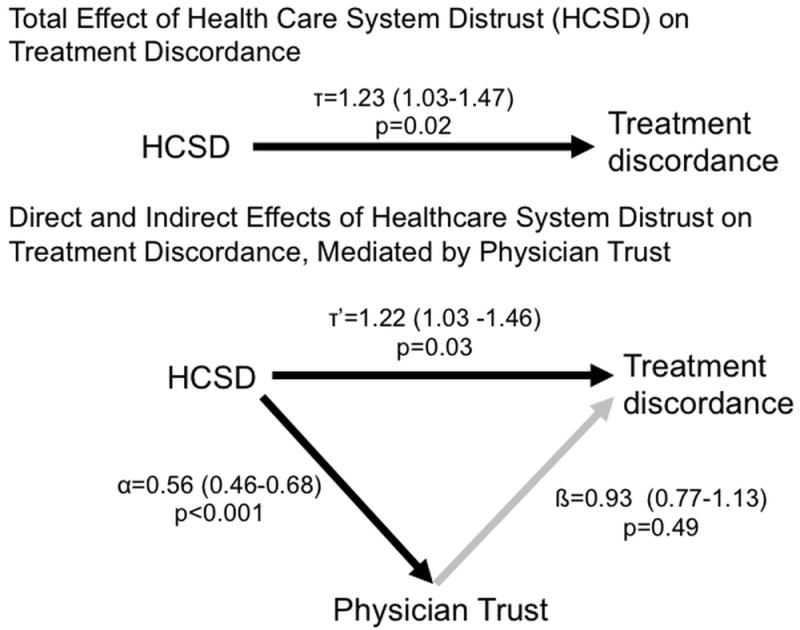
Mediation Analysis Examining the Relationship between Healthcare System Distrust and Treatment Discordance, with Physician Trust as a Mediator
Figure 1 shows contains two directed acylic graphs showing the paths of mediation analysis with accompanying odds ratios for each path tested in the analysis.
*Odds ratios are adjusted for race, age, education, income, marital status, employement status, health insurance status, cancer stage, and state of residence
Table 3.
Adjusted Logistic Regression Mediation Models for Healthcare System Distrust (independent variable), Physician Trust (mediator), and Adjuvant Breast Cancer Treatment Discordance (dependent variable)
| MEDIATION MODEL A: Physician Trust (mediator) regressed on Healthcare System Distrust | MEDIATION MODEL B: Discordance (dependent variable) regressed on Healthcare System Distrust | FINAL MODEL: Discordance regressed on Healthcare System Distrust and Physician Trust | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | Lower 95% CI | Upper 95% CI | P | OR | Lower 95% CI | Upper 95% CI | P | OR | Lower 95% CI | Upper 95% CI | P | |
| Health Care System Distrust | ||||||||||||
| Tertiles 1&2 | Ref | Ref | Ref | |||||||||
| Tertile 3 | 0.56 | 0.46 | 0.68 | <0.001 | 1.23 | 1.03 | 1.47 | 0.02 | 1.22 | 1.03 | 1.46 | 0.03 |
| Physician Trust | ||||||||||||
| Tertiles 1&2 | Ref | Ref | Ref | |||||||||
| Tertile 3 | -- | -- | -- | -- | -- | -- | -- | -- | 0.94 | 0.77 | 1.13 | 0.49 |
| Age (in years) | 0.98 | 0.97 | 0.99 | <0.001 | 1.00 | 0.99 | 1.01 | 0.56 | 1.00 | 0.99 | 1.01 | 0.60 |
| Race | ||||||||||||
| White | Ref | Ref | Ref | |||||||||
| Black | 0.81 | 0.66 | 1.01 | 0.06 | 0.89 | 0.73 | 1.09 | 0.25 | 0.89 | 0.72 | 1.09 | 0.24 |
| Other | 0.64 | 0.40 | 1.01 | 0.05 | 1.26 | 0.84 | 1.88 | 0.26 | 1.25 | 0.84 | 1.87 | 0.27 |
| Hispanic | 1.21 | 0.85 | 1.74 | 0.29 | 0.90 | 0.63 | 1.29 | 0.57 | 0.90 | 0.63 | 1.30 | 0.58 |
| Income | ||||||||||||
| < $10,000 | Ref | Ref | Ref | |||||||||
| $10,001 to $30,000 | 1.19 | 0.78 | 1.83 | 0.42 | 1.31 | 0.88 | 1.94 | 0.19 | 1.31 | 0.88 | 1.95 | 0.19 |
| $30,001 to $70,000 | 1.50 | 0.99 | 2.28 | 0.06 | 1.60 | 1.08 | 2.37 | 0.02 | 1.61 | 1.08 | 2.39 | 0.02 |
| > $70,000 | 1.66 | 1.06 | 2.59 | 0.03 | 1.52 | 0.99 | 2.33 | 0.05 | 1.53 | 1.00 | 2.34 | 0.05 |
| Education | ||||||||||||
| High school grad or less | Ref | Ref | Ref | |||||||||
| Some college | 1.14 | 0.90 | 1.44 | 0.27 | 1.12 | 0.89 | 1.40 | 0.33 | 1.12 | 0.90 | 1.40 | 0.32 |
| College grad or more | 1.01 | 0.79 | 1.29 | 0.95 | 1.09 | 0.86 | 1.39 | 0.46 | 1.09 | 0.86 | 1.39 | 0.46 |
| Married or Coupled | 0.92 | 0.75 | 1.13 | 0.42 | 0.78 | 0.64 | 0.94 | 0.01 | 0.78 | 0.64 | 0.94 | 0.01 |
| Not employed for wages | 1.11 | 0.92 | 1.34 | 0.30 | 1.12 | 0.93 | 1.35 | 0.22 | 1.12 | 0.93 | 1.35 | 0.22 |
| Insured | 1.26 | 0.82 | 1.94 | 0.29 | 0.91 | 0.62 | 1.34 | 0.63 | 0.91 | 0.62 | 1.34 | 0.64 |
| Stage at diagnosis | ||||||||||||
| Stage 1 | Ref | Ref | Ref | |||||||||
| Stage 2 | 1.13 | 0.94 | 1.35 | 0.20 | 0.71 | 0.60 | 0.84 | <0.001 | 0.71 | 0.60 | 0.85 | <0.001 |
| Stage 3 | 1.32 | 0.92 | 1.90 | 0.13 | 0.53 | 0.36 | 0.80 | <0.001 | 0.54 | 0.36 | 0.80 | <0.001 |
| State | ||||||||||||
| Florida | Ref | Ref | Ref | |||||||||
| Pennsylvania | 0.90 | 0.75 | 1.08 | 0.25 | 0.78 | 0.66 | 0.93 | 0.01 | 0.78 | 0.66 | 0.93 | 0.01 |
OR = odds ratio; CI = confidence interval
A mediation model (Figure 1) suggested that physician distrust was not a mediator of the relationship between healthcare system distrust and treatment discordance. Although healthcare system distrust was significantly associated with discordance (p=0.03) and physician trust (p<0.001) in mediation models, the indirect effects of physician distrust and healthcare system distrust on discordance showed that physician distrust was not a significant predictor of discordance (p=0.49) and thus not a mediator between healthcare system distrust and treatment discordance (total indirect OR=1.00 [1.00,1.01]). Rather than treat it as a mediator, physician distrust was then included in the main model as a covariate, as seen in the model in Table 3 (Final Model).
Table 3 (Final Model) includes the final adjusted logistic regression results, which estimate a higher odds of reporting treatment discordance for those in the highest tertile of distrust, compared with the two lowest tertiles (OR=1.22, p=0.03). In separate models, elevated ORs for healthcare system distrust’s association with discordance of radiation (OR=1.26, p=0.09) and hormone therapy (OR=1.20, p=0.12) and hormone therapy (OR=1.20, p=0.12) were similar to the overall effect but did not reach statistical significance. There was no evidence of association with chemotherapy in a model examining chemotherapy discordance alone. Those in income categories above $30,000 were significantly more likely to report treatment discordance ($30,000-$70,000: OR=1.61, p=0.02; <$70,000: OR=1.53, p=0.05). Factors associated with less discordance, or greater likelihood of fully following the physician recommended treatment included: being married (OR=0.78, p=0.01), being diagnosed at Stage 2 (OR=0.71, p<0.001) or Stage 3 (OR=0.43, p=0.002), and living in Pennsylvania (OR=0.78, p=0.005). Results were essentially unchanged in sensitivity analysis using oncologist and surgeon discordance as separate outcomes.
Discussion
This analysis was designed to explore whether or not healthcare system distrust was associated with discordance between the adjuvant treatments received and the treatments recommended among early stage breast cancer patients. The present study results align with a previous investigation suggesting that lack of trust in the medical delivery system, but not lack of trust in physicians, is associated with underuse of adjuvant treatment after breast cancer among urban early stage breast cancer patients (3). In contrast to previous work, the current study expands this finding in a larger sample of women who have Stage I, II, or III breast cancer, from two states, and includes both those who were untreated or discontinued treatment for adjuvant therapy. Race-based differences in healthcare system distrust had been established in our previous work (9), and were observed in bivariate associations with distrust, but not in adjusted models. Results suggest that patients in the highest tertile of health care system distrust have 22% greater odds of not receiving a treatment recommended by their provider than those in the lowest tertile of distrust, but physician trust is not associated with adjuvant cancer treatment discordance. The use of adjuvant treatment has been shown to be associated with quality of insurance and characteristics of the treatment facility (25), suggesting that trust in broader healthcare system factors may play an important and distinct role. The association between healthcare system distrust and treatment discordance in the current sample is stronger than previously suggested (3), which may be because the present study included both those who did not receive treatment, as well as those who started but did not complete treatment. This suggests that some patients may start treatment, despite feelings of distrust, but later discontinue it, which indicates that distrust is an important risk factor for failure to initiate and failure to complete recommended treatments.
Further, while studies have previously focused on race and income disparities as drivers of breast cancer adjuvant treatment discordance (26,27), neither race nor socioeconomic position were significant drivers in this sample. These finding are particularly promising because, unlike race, healthcare system distrust is a potentially modifiable factor that may be responsive to intervention. In support of the modifiability of trust, the field of corporate business ethics has embraced increasing trust as a necessary part of building ethical practice (28) and part of engaging consumers (29), which is a concept that can be integrated into healthcare and medical systems.
The limited research to date about reducing distrust in healthcare has focused on increasing trust in physicians with null to modest (30-32) results. However, given that the relationship between distrust and treatment discordance was not mediated by physician trust, these results suggest that addressing healthcare system distrust may be an important and distinct effort from strategies focused on lack of physician trust. Rather than playing a mediating role, patients may view physician trust as independent of their trust in the healthcare system as an institution; that is, even if patients distrust the healthcare system, they may still have trust in their personal physicians. Patients may be able to exercise greater choice in physicians, but may not have the same breadth of choices in using the healthcare system. Addressing healthcare system distrust might be informed by strategies that have addressed distrust in other types of institutions, such as corporations (29), according to the values and competence domains. For example, addressing the subdomain of values might be achieved through expanded access to adjuvant care, while addressing the subdomain of competence might be achieved through expanded access to health professionals while deciding to start or continue adjuvant treatment. Of course, any intervention to reduce healthcare system distrust would first need to be tested before implementing wide-scale changes.
Yet, motivation to reduce healthcare system distrust is based on the presumption that greater cancer treatment discordance would lead to worse patient outcomes. Instead, it is possible that distrust could perform a function in course-correcting treatment that is overprescribed or too aggressive. This might lead to treatment discordance that was ultimately beneficial rather than detrimental; however, a separate model of treatment discordance and cancer recurrence suggested a 40% increased odds of cancer recurrence for those who reported treatment discordance (p=0.02), after adjusting for healthcare system and physician distrust, race, income, marital status, employment status, health insurance, stage and state of residence. This provides initial support that discordance that arises due to distrust may lead to poorer health outcomes.
In addition to distrust, having higher income, being unmarried, having more severe stage of diagnosis, and living in the state of Florida were associated with greater treatment discordance. Lower income has been previously associated with greater adjuvant treatment discordance (25,33), but in the current study, higher income was associated with greater treatment discordance. This may be because women at higher incomes were less likely to be diagnosed with later stage cancer (p=0.002). As has been found in previous study, unmarried women were more likely to be discordant with adjuvant therapy recommendations than partnered women, which has been suggested to be due to unmarried women lacking the post-operative social and transportation resources that would allow them to fully complete adjuvant treatment regimens (34). Patients diagnosed at later stages may have been more concordant with treatment recommendations due to the severity of their cancer, and may have had more to gain from initiating and adhering to adjuvant treatment (4,35). Insurance status was not associated with treatment discordance, but over 95% of the sample had some form of insurance so there may not have been enough variation to assess a difference by insurance status. A significantly lower proportion of participants (p<0.001) from FL were insured (93%) compared to PA (97%), which may have increased the likelihood that Florida patients would be discordant.
While this study demonstrated an association between healthcare system distrust and adjuvant breast cancer treatment discordance, it could not assess the degree to which distrust caused treatment discordance. Distrust was measured 24-36 months after treatment, meaning that experiences with treatment, effectiveness of treatment, or emergence of adverse treatment effects may have shaped subsequent level of distrust; however, this timeline overlaps with previous studies of healthcare system distrust and adjuvant treatment (3). Despite non-zero odds ratios for chemotherapy, radiation therapy, and hormone therapy, distrust was not significantly associated with these adjuvant treatments in separate models, which may be due to the relatively small amount of discordance within each treatment type. Physician adjuvant treatment recommendation was based on patient recall, and those with highest levels of distrust may have more strongly endorsed not being compliant with physician adjuvant treatments, leading to a more robust odds ratio. We were unable to access medical records for the study participants and recognize that validation of physician recommendation may be challenging even with full medical records. However, we believe the critical issue is what patients perceived their physician recommended, and whether or not patients perceived going against what their physician recommended. Physician’s recommendation for adjuvant treatment may not have aligned with current guidelines, but even if patients were discordant because the physician recommended treatment that was not aligned with what clinical guidelines dictate, it still suggests that patients did not trust the physician’s recommendation (possibly rightfully so), and bolsters our hypothesis of a role for distrust. Our conclusions are also limited in that it is possible that those who are most distrustful of the healthcare system may not participate in a survey from a healthcare system entity; however, the maximum endorsed distrust score was 40 out of a possible 45, indicating that most of the range of the score was used. Results may not be generalizable to samples beyond women diagnosed with breast cancer in PA and FL; however, this includes a broad and diverse sample of both urban and rural women.
As the largest study to explore the role of healthcare system distrust in receipt of breast cancer adjuvant treatment, the results suggest that healthcare system distrust may play a role in who does or does not receive adjuvant treatment, and that healthcare system distrust is distinct from physician distrust. Consequently, healthcare system distrust may need separate intervention, that specifically address breast cancer patient’s attitudes toward the healthcare system distrust, and that address the larger structural factors that may be barriers to full use of breast cancer adjuvant treatment.
Acknowledgments
The Florida cancer incidence data used in this report were collected by the Florida Cancer Data System (FCDS) under contract with the Florida Department of Health (FDOH) (Project N.:BE0910). The views expressed herein are solely those of the author(s) and do not necessarily reflects those of the FCDS or FDOH. The Bureau of Health Statistics & Registries, Pennsylvania Department of Health also has provided data for this study (Project N.: IF-0317). The Pennsylvania Department of Health specifically disclaims responsibility for any analyses, interpretations or conclusions.
Financial Support: Dr. Dean was supported by the National Cancer Institute grant K01CA184288; the Sidney Kimmel Cancer Center grant P30CA006973; Johns Hopkins University Center for AIDS Research grant P30AI094189, and National Institute of Mental Health grant R25MH083620. Shadiya L. Moss was supported by the National Institutes of Health grant R25GM062454 and the National Institute of Drug Abuse grant T32DA031099. This work was supported by the NIH grant from the National Cancer Institute (5-R01-CA133004-3). The funding organization disclaims responsibility in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication
References
- 1.National Cancer Institute. [22 May 2017];Adjuvant Therapy. NCI Dictionary of Cancer Terms. 2017 May 22; < https://www.cancer.gov/publications/dictionaries/cancer-terms?cdrid=45587>.
- 2.Early Breast Cancer Trialists’ Collaborative Group. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. The Lancet. 2006;366(9503):2087–106. doi: 10.1016/S0140-6736(05)67887-7. [DOI] [PubMed] [Google Scholar]
- 3.Bickell NA, Weidmann J, Fei K, Lin JJ, Leventhal H. Underuse of breast cancer adjuvant treatment: patient knowledge, beliefs, and medical mistrust. Journal of Clinical Oncology. 2009;27(31):5160–7. doi: 10.1200/JCO.2009.22.9773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neugut AI, Hillyer GC, Kushi LH, Lamerato L, Leoce N, Nathanson SD, et al. Non-initiation of adjuvant hormonal therapy in women with hormone receptor-positive breast cancer: The Breast Cancer Quality of Care Study (BQUAL) Breast cancer research and treatment. 2012;134(1):419–28. doi: 10.1007/s10549-012-2066-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huiart L, Ferdynus C, Giorgi R. A meta-regression analysis of the available data on adherence to adjuvant hormonal therapy in breast cancer: summarizing the data for clinicians. Breast cancer research and treatment. 2013;138(1):325. doi: 10.1007/s10549-013-2422-4. [DOI] [PubMed] [Google Scholar]
- 6.Freedman RA, Fedewa SA, Punglia RS, Lin CC, Ward EM, Jemal A, et al. Factors associated with radiation therapy incompletion for patients with early-stage breast cancer. Breast cancer research and treatment. 2016;155(1):187–99. doi: 10.1007/s10549-015-3660-4. [DOI] [PubMed] [Google Scholar]
- 7.Hovland C, Janis I, Kelley H. Communication and Persuasion. New Haven, CT: Yale University Press; 1953. [Google Scholar]
- 8.Shea JA, Micco E, Dean LT, McMurphy S, Armstrong K. Development of a Revised Health Care System Distrust Scale. Journal of General Internal Medicine. 2008;23(6):727–32. doi: 10.1007/s11606-008-0575-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Armstrong K, McMurphy S, Dean LT, Micco E, Putt M, Hughes-Halbert C, et al. Differences in the Patterns of Health Care System Distrust between Blacks and Whites. Journal of General Internal Medicine. 2008;23(6):827–33. doi: 10.1007/s11606-008-0561-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Armstrong K, Rose A, Peters N, Long JA, McMurphy S, Shea J. Distrust of the health care system and self-reported health in the United States.[see comment] Journal of General Internal Medicine. 2006;21(4):292–7. doi: 10.1111/j.1525-1497.2006.00396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rose A, Peters N, Shea J, Armstrong K. Development and Testing of the Health Care System Distrust Scale. J Gen Intern Med. 2004;19(1):57–63. doi: 10.1111/j.1525-1497.2004.21146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hall MA. Researching medical trust in the United States. Journal of health organization and management. 2006;20(5):456–67. doi: 10.1108/14777260610701812. [DOI] [PubMed] [Google Scholar]
- 13.Sheppard VB, Harper FW, Davis K, Hirpa F, Makambi K. The importance of contextual factors and age in association with anxiety and depression in black breast cancer patients. Psycho-Oncology. 2014;23(2):143–50. doi: 10.1002/pon.3382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones DP. Knowledge, Beliefs and Feelings about Breast Cancer: The Perspective of African American Women. ABNF Journal. 2015;26(1) [PubMed] [Google Scholar]
- 15.Waljee JF, Hu ES, Newman LA, Alderman AK. Correlates of patient satisfaction and provider trust after breast‐conserving surgery. Cancer. 2008;112(8):1679–87. doi: 10.1002/cncr.23351. [DOI] [PubMed] [Google Scholar]
- 16.Barsevick AM, Leader A, Bradley PK, Avery T, Dean LT, DiCarlo M, et al. Post-treatment problems of African American breast cancer survivors. Supportive Care in Cancer. 2016;24(12):4979–86. doi: 10.1007/s00520-016-3359-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jagsi R, Griffith KA, Sabolch A, Jones R, Spence R, De Vries R, et al. Perspectives of Patients With Cancer on the Ethics of Rapid-Learning Health Systems. Journal of Clinical Oncology. 2017 doi: 10.1200/JCO.2016.72.0284. JCO. 2016.72.0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang Y, Sereika SM, Bender CM, Brufsky AM, Rosenzweig MQ. Beliefs in Chemotherapy and Knowledge of Cancer and Treatment Among African American Women With Newly Diagnosed Breast Cancer. Oncology nursing forum. 2016;43(2):180–9. doi: 10.1188/16.onf.180-189. [DOI] [PubMed] [Google Scholar]
- 19.Sheppard VB, Hurtado-de-Mendoza A, Talley CH, Zhang Y, Cabling ML, Makambi KH. Reducing Racial Disparities in Breast Cancer Survivors’ Ratings of Quality Cancer Care: The Enduring Impact of Trust. Journal for healthcare quality : official publication of the National Association for Healthcare Quality. 2016;38(3):143–63. doi: 10.1097/jhq.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 20.Definitions S. American Association for Public Opinion Research. 4. Deerfield, IL: American Association for Public Opinion Research; 2008. Response Rate#4: Final Dispositions of Case Codes and Outcome Rates for Surveys. [Google Scholar]
- 21.Oberst K, Bradley CJ, Schenk M. Breast and prostate cancer patient’s reliability of treatment reporting. Journal of registry management. 2008;36(1):12–5. [PubMed] [Google Scholar]
- 22.Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the Trust in Physician Scale. Medical care. 1999;37(5):510–7. doi: 10.1097/00005650-199905000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 24.Kenny DA. Mediation. < http://davidakenny.net/cm/mediate.htm>.
- 25.Wu X-C, Lund MJ, Kimmick GG, Richardson LC, Sabatino SA, Chen VW, et al. Influence of race, insurance, socioeconomic status, and hospital type on receipt of guideline-concordant adjuvant systemic therapy for locoregional breast cancers. Journal of Clinical Oncology. 2011;30(2):142–50. doi: 10.1200/JCO.2011.36.8399. [DOI] [PubMed] [Google Scholar]
- 26.Bickell NA, Wang JJ, Oluwole S, Schrag D, Godfrey H, Hiotis K, et al. Missed opportunities: racial disparities in adjuvant breast cancer treatment. Journal of Clinical Oncology. 2006;24(9):1357–62. doi: 10.1200/JCO.2005.04.5799. [DOI] [PubMed] [Google Scholar]
- 27.Curtis E, Quale C, Haggstrom D, Smith-Bindman R. Racial and ethnic differences in breast cancer survival. Cancer. 2008;112(1):171–80. doi: 10.1002/cncr.23131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Castaldo S, Premazzi K, Zerbini F. The meaning (s) of trust. A content analysis on the diverse conceptualizations of trust in scholarly research on business relationships. Journal of Business Ethics. 2010;96(4):657–68. [Google Scholar]
- 29.Gustafsson C. Trust as an instance of asymmetrical reciprocity: An ethics perspective on corporate brand management. Business Ethics: A European Review. 2005;14(2):142–50. [Google Scholar]
- 30.Thom DH. Physician behaviors that predict patient trust. Journal of Family Practice. 2001;50(4):323–8. [PubMed] [Google Scholar]
- 31.Thom DH. Training physicians to increase patient trust. Journal of Evaluation in Clinical Practice. 2000;6(3):245–53. doi: 10.1046/j.1365-2753.2000.00249.x. [DOI] [PubMed] [Google Scholar]
- 32.Thom DH, Hessler D, Willard-Grace R, Bodenheimer T, Najmabadi A, Araujo C, et al. Does health coaching change patients’ trust in their primary care provider? Patient education and counseling. 2014;96(1):135–8. doi: 10.1016/j.pec.2014.03.018. [DOI] [PubMed] [Google Scholar]
- 33.Kimmick G, Anderson R, Camacho F, Bhosle M, Hwang W, Balkrishnan R. Adjuvant hormonal therapy use among insured, low-income women with breast cancer. Journal of Clinical Oncology. 2009;27(21):3445–51. doi: 10.1200/JCO.2008.19.2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guy GP, Lipscomb J, Gillespie TW, Goodman M, Richardson LC, Ward KC. Variations in Guideline-Concordant Breast Cancer Adjuvant Therapy in Rural Georgia. Health services research. 2015;50(4):1088–108. doi: 10.1111/1475-6773.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neugut AI, Hillyer GC, Kushi LH, Lamerato L, Leoce N, Nathanson SD, et al. Noninitiation of adjuvant chemotherapy in women with localized breast cancer: the breast cancer quality of care study. Journal of Clinical Oncology. 2012;30(31):3800–9. doi: 10.1200/JCO.2012.43.8168. [DOI] [PMC free article] [PubMed] [Google Scholar]


