Abstract
Rationale
Correctional healthcare providers’ limited cultural and clinical competence to care for transgender patients represents a barrier to care for incarcerated transgender individuals.
Objective
The present study aimed to adapt, deliver, and evaluate a transgender cultural and clinical competence intervention for correctional healthcare providers.
Method
In the summer of 2016, a theoretically-informed, group-based intervention to improve transgender cultural and clinical competence was delivered to 34 correctional healthcare providers in New England. A confidential survey assessed providers’ cultural and clinical competence to care for transgender patients, selfefficacy to provide hormone therapy, subjective norms related to transgender care, and willingness to provide gender-affirming care to transgender patients before and after (immediately and 3-months) the intervention. Linear mixed effects regression models were fit to assess change in study outcomes over time. Qualitative exit interviews assessed feasibility and acceptability of the intervention.
Results
Providers’ willingness to provide gender-affirming care improved immediately post-intervention (β = 0.38; SE = 0.41, p < 0.001) and from baseline to 3-months post-intervention (β = 0.36; SE = 0.09; p < 0.001; omnibus test of fixed effects χ2 = 23.21; p < 0.001). On average, transgender cultural competence (χ2 = 22.49; p < 0.001), medical gender affirmation knowledge (χ2 = 11.24; p = 0.01), self-efficacy to initiate hormones for transgender women, and subjective norms related to transgender care (χ2 = 14.69; p = 0.001) all significantly increased over time. Providers found the intervention to be highly acceptable and recommended that the training be scaled-up to other correctional healthcare providers and expanded to custody staff.
Conclusion
The intervention increased correctional healthcare providers’ cultural and clinical competence, selfefficacy, subjective norms, and willingness to provide gender-affirming care to transgender patients. Continued efforts should be made to train correctional healthcare providers in culturally and clinically competent gender-affirming care in order to improve the health of incarcerated transgender people. Future efficacy testing of this intervention is warranted.
Keywords: Transgender, Healthcare, Incarceration, Providers, Intervention
1. Introduction
Societies across modern Western history have created and reinforced a binary gender system (i.e., male and female) based on biological sex characteristics (e.g., chromosomes and genitalia) (West and Zimmerman, 1987). Under this binary system, having a gender that aligns with one’s sex characteristics is considered normative, while transgender people – those who have a gender identity that differs from their assigned birth sex – are labeled as the “other” and experience widespread stigma as a result (Goffman, 1963). Structural (e.g., cultural norms and beliefs, restrictive social policies) and interpersonal (e.g., discrimination) forms of stigma constrain access to necessary resources for transgender people, including education, employment, income, and healthcare (White Hughto et al., 2015). Excluded from the legitimate economy, some transgender individuals turn to street economies such as sex work to survive or substance use to cope with mistreatment, placing them at risk for arrest, incarceration, and poor health (Garofalo et al., 2006; Grant et al., 2011; James et al., 2016; Reisner et al., 2014). Biased policing and sentencing practices also contribute to the disproportionate incarceration of transgender individuals (Grant et al., 2011; James et al., 2016; Wolff and Cokely, 2007). While there are no systematic efforts to identify transgender individuals in U.S. prisons, estimates suggest that 16% of the estimated 1.4 million transgender adults in the U.S (Flores et al., 2016) have been incarcerated in their lifetime (Grant et al., 2011), compared to just 3% of the U.S. general population (Glaze and Kaeble, 2014).
Prior research with currently and formerly incarcerated transgender individuals shows that transgender people are a highly stigmatized inmate population who are at risk for stigma-driven verbal harassment and physical assault (Jenness et al., 2009; Lydon et al., 2015; White Hughto et al., in press). Interpersonal forms of stigma-based discrimination and violence have been linked to physical trauma and mental health conditions that often require treatment, including depression, anxiety, and suicidality (White Hughto et al., 2015). Moreover, incarcerated transgender people seeking physical and mental health treatment report being verbally harassed by their healthcare providers (White Hughto et al., in press), and denied necessary general and transgender-specific care, such as hormones to medically affirm one’s gender and other treatments for gender dysphoria (Brown and McDuffie, 2009; James et al., 2016; Lydon et al., 2015; Reisner et al., 2014; White Hughto et al., in press). Further, denial of necessary healthcare has been linked to depression, non-suicidal self-injury, and death by suicide in incarcerated transgender populations (Brown, 2014; Brown and McDuffie, 2009; Edney, 2004; Tarzwell, 2006).
Gender-affirming care refers to acknowledging and respecting a patient’s gender identity and supporting access to hormones and other therapies for transgender patients seeking to medically affirm their gender (Reisner et al., 2015). In some cases, the lack of access to gender-affirming care that incarcerated transgender people face is grounded in correctional healthcare providers’ limited transgender cultural competence (e.g., knowledge and ability to use gender-affirming terminology, supportive attitudes and interactions) (Clark et al., 2017; White Hughto et al., in press). In other cases, mistreatment is driven by providers’ lack of clinical competence (e.g., knowledge and ability to administer hormones) to appropriately care for transgender patients (Clark et al., in press; Rosenblum, 1999; Tarzwell, 2006; White Hughto et al., in press). A recent qualitative study of recently incarcerated transgender women in New England found that correctional healthcare providers frequently misgendered transgender women by using male names and pronouns. Transgender women in the study also reported that some providers did not recognize the medical necessity of providing medical gender affirmation therapies and in some cases, trans-gender inmates had to educate their providers in order to receive appropriate medical care (White Hughto et al., in press). Research suggests that while some correctional providers possess transphobic attitudes and are unwilling to provide gender-affirming care to trans-gender patients, many providers want to provide gender-affirming care, but lack the requisite knowledge and skills to do so (Clark et al., 2017). Research also highlights that providers working in correctional settings face structural barriers in providing transgender inmates with appropriate and necessary care. These barriers include restrictive hormone policies, limited healthcare budgets, and inadequate institutional support (Clark et al., 2017; Routh et al., 2015; Tarzwell, 2006; White Hughto et al., in press). While structural barriers to the delivery of gender-affirming care for transgender patients must be intervened upon at the institutional level, educational efforts to increase correctional healthcare providers’ cultural and clinical competence to care for transgender patients must accompany structural changes in order to increase providers’ ability and willingness to provide gender-affirming care. Further, educational efforts may be more easily implemented than policy changes, and thus, hold promise for immediately improving healthcare access, and ultimately, the health of incarcerated trans-gender people.
Educational efforts to increase transgender cultural competence (e.g., trainings covering terminology and transgender discrimination) have been successful in improving provider awareness and understanding of transgender patients by exposing them to the healthcare barriers that transgender people encounter (Hanssmann et al., 2008). Interventions to improve providers’ transgender clinical knowledge have also demonstrated success. For example, a lecture covering the durability of gender identity and hormone treatment regimens significantly increased physician-residents’ knowledge and willingness to provide hormone therapy to transgender patients (Thomas and Safer, 2015). To our knowledge, only one other transgender-affirming educational intervention has been evaluated in a correctional setting. The study, which involved the delivery of a lesbian, gay, bisexual, and transgender (LGBT) health curriculum, found that healthcare-related complaints by transgender inmates dropped by over 50% three months after the training; however, baseline data were not collected from providers, and the training focused on LGBT issues broadly, rather than specifically on the unique healthcare needs of transgender individuals (Jaffer et al., 2016). Transgender cultural and clinical competence interventions that are adapted to the correctional context and assess changes in provider knowledge, attitudes, and behaviors over time are urgently needed.
The present study aimed to adapt a transgender cultural and clinical competence intervention (White Hughto and Clark, in press) and open field-test the intervention with healthcare providers working in correctional settings. Grounded in theoretical models of behavioral change (Ajzen, 1991; Fisher et al., 2002), the study engaged correctional administrators, embedded the intervention into continuing education trainings, and delivered a transgender cultural and clinical competence curriculum that was responsive to the unique structural contexts of providing care in correctional settings (e.g., gender binary institutions, restrictive hormone policies, limited institutional support for trans-gender care). Using a longitudinal design, the intervention was assessed for initial feasibility and acceptability and preliminary efficacy via changes in providers’ knowledge, attitudes, and behavioral intentions to care for transgender patients from baseline to follow-up. Given the documented healthcare challenges that incarcerated transgender people face and the mental and physical health sequelae of insufficient access to culturally and clinically appropriate care, interventions that address providers’ lack of cultural and clinical competencies – a primary source of these healthcare barriers – has the potential to improve health outcomes for incarcerated transgender populations.
2. Method
2.1. Sampling and procedures
Between June and August 2016, correctional healthcare providers participated in a single session, group-based intervention to improve transgender cultural and clinical competencies and willingness to care for transgender patients. The intervention was piloted during three separate trainings with healthcare providers working in correctional facilities in Connecticut and Massachusetts. The intervention was led by two cisgender facilitators with extensive experience conducting trans-gender health trainings and who were not affiliated with the correctional system. Participants were eligible if they were: 18 years of age or older; fluent in English; identified as a healthcare provider (e.g., medical doctor, nurse, physician’s assistant, psychologist, psychiatrist, social worker, mental health counselor); and currently practicing in a correctional institution in Connecticut or Massachusetts.
The initial recruitment of providers was coordinated by correctional healthcare administrators/supervisors in each state. Eligible staff were sent an email three weeks prior to the scheduled training inviting them to participate in the intervention and requesting that they complete a confidential electronic survey. Participation in the baseline survey was voluntary, and participants had the option to decline survey participation and still attend the training. All participants provided informed consent before initiating the survey. Participants created a unique ID to link their consent form to their survey data. After the intervention, participants were invited by email to complete the post-training survey one day following the intervention and again three months following the intervention. All participants received continuing education credits for their participation in the training.
After completing the 3-month survey, a randomly selected subset of participants (n = 12) was invited to participate in a brief telephone exit interview. After providing verbal consent, nine participants completed a semi-structured interview assessing intervention feasibility and acceptability. The one-on-one, in-depth interviews lasted approximately 15–20 minutes and were conducted by the first author who has extensive experience conducting community-based qualitative research with diverse populations, including correctional healthcare providers. The interviews were audio-recorded and transcribed verbatim. To protect anonymity, participant names were not recorded. Participants received a gift card as compensation.
Overall, 58 providers participated in the training and 40 completed the baseline survey. Of the 40 participants who completed the baseline survey and participated in the intervention, 34 completed the immediate follow-up survey (T1) (82.5% retention), and 28 completed the 3-month follow-up survey (T2) (70.0% retention). The Institutional Review Board of Yale University approved all study activities.
2.2. Transgender cultural and clinical competence intervention
Theoretical framework
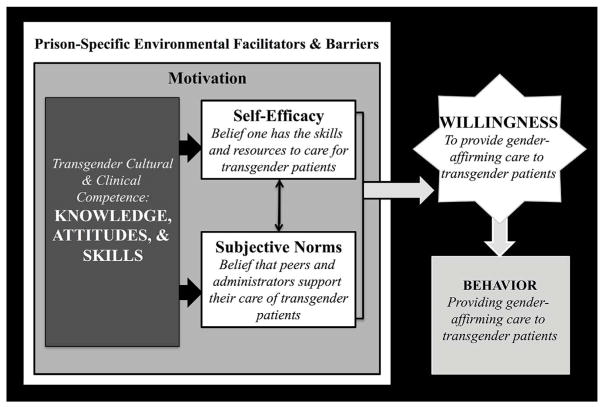
The Theory of Planned Behavior (Ajzen, 1991) and the Information, Motivation, and Behavioral Skills (Fisher et al., 2002) models specify effective strategies for producing behavioral changes in diverse groups, including healthcare providers (Chau and Hu, 2002; Starace et al., 2006). Drawing on both models, the present study hypothesized that transgender-specific knowledge and attitudes and transgender-affirming skills drive a provider’s intention to provide gender-affirming care and provide the capacity for providers to increase their provision of gender-affirming care to transgender patients (behavioral change). The piloted intervention targeted providers’ Knowledge, Attitudes, and Skills by providing them with transgender cultural (e.g., transgender terminology, impact of transgender stigma) and clinical (e.g., cross-sex hormone use, mental health comorbidities) competencies. The information provided during the intervention aimed to change provider Knowledge about the healthcare needs of trans-gender individuals and personal Attitudes or biases towards transgender patients as a means of Motivating providers’ intentions to provide gender-affirming care to transgender patients. The intervention also aimed to equip providers with the Skills to increase their Self-Efficacy (Bandura, 1977) to care for transgender patients (e.g., ability to interact with transgender patients in a gender-affirming manner and follow transgender standards of care) (Coleman et al., 2012; Deutsch, 2012; Reisner et al., 2015). By delivering the group-based intervention in the workplace with the support of administrators and supervisors, the intervention also aimed to change perceptions of institutional norms and support related to transgender care (i.e., Subjective Norms) (Ajzen and Fishbein, 1980). Additionally, the intervention content was sensitive to the correctional context as it accounted for institutional factors that may inhibit (e.g., restrictive policies, limited institutional support) or facilitate (e.g., current use of non-gendered language, such as referring to inmates by their last names) providers’ ability to provide trans-gender-affirming care to transgender patients. Together, increased Knowledge, Attitudes, Skills, Self-Efficacy, and Subjective Norms related to transgender care are hypothesized to lead to increased willingness to provide gender-affirming care for transgender patients (primary study outcome), with the long-term goal of increasing the provision of gender-affirming care to transgender patients.
The components of the theoretical model presented here can be mapped onto the behavior change technique (BCT) taxonomy developed by Michie et al. (2013). In order to increase providers’ willingness to provide gender-affirming care, this study utilized the following behavior change techniques: (1) providing information about antecedent risk factors for incarceration among transgender individuals (theoretical mechanisms: knowledge and attitudes); (2) providing information about health, social, and environmental consequences, such as the health benefits of providing gender-affirming care for transgender patients (theoretical mechanisms: knowledge and attitudes); (3) instructing providers on how to interact with transgender patients in gender-affirming ways and reviewing standards-of-care guidelines (theoretical mechanisms: skill building and knowledge); (4) problem solving, including discussing challenging social interactions involving transgender patients (theoretical mechanisms: knowledge, skills, and self-efficacy); (5) behavioral rehearsal, including role-playing effective communication with transgender people using affirming language (theoretical mechanisms: self-efficacy and skills); and (6) providing information about others’ approval, including embedding the training into participants’ workday and highlighting administrators/supervisors’ support for the delivery of gender-affirming care (theoretical mechanism: subjective norms).
Approach to intervention adaptation and development
A staged intervention approach (Rounsaville and Carroll, 2001) was used to adapt and evaluate a transgender cultural and clinical competence intervention for correctional healthcare providers. The approach included: (1) qualitative interviews with recently incarcerated trans-gender individuals to examine their experiences accessing healthcare in correctional settings, including structural and interpersonal barriers to care (White Hughto et al., in press); (2) key informant interviews with correctional administrators to assess the transgender-related training needs of correctional healthcare providers and the feasibility of delivering a transgender cultural and clinical competence intervention to correctional providers (White Hughto et al., in press); (3) development and pilot testing of the Phase I curriculum to assess the initial acceptability of the intervention content and feasibility of delivery, post-intervention (White Hughto and Clark, in press); (4) qualitative interviews with correctional healthcare providers to assess multilevel barriers and facilitators to caring for transgender patients (Clark et al., 2017); (5) adaptation and Phase II pilot testing to assess robust measures of intervention feasibility, acceptability, and preliminary efficacy via a mixed-methods, pre-post, longitudinal design; (6) Phase III efficacy testing of the intervention via a randomized controlled trial; and (7) Phase IV translation of the intervention into practice. The present paper focuses on stages 4 and 5: adaptation and Phase II pilot testing of the intervention. Stages 1–3 have been reported elsewhere (White Hughto and Clark, in press); and stages 6 and 7 are in progress.
Throughout the intervention development process an implementation science framework (Rycroft-Malone, 2004) was used to maximize the potential impact and sustainability of the intervention by working with correctional administrations to strengthen existing training efforts, implement the intervention as part of continuing education activities, and ensure the intervention was responsive to the transgender-related training needs of correctional healthcare providers. Given that the training aimed to increase providers’ transgender cultural and clinical competence as a means of improving incarcerated transgender patients’ access to gender-affirming care, the experiences of correctional providers and criminal-justice-involved transgender people directly informed the content and delivery of the intervention.
Intervention adaptation
The present study adapted the Phase I curriculum using findings from the initial feasibility trial (stage 3) (White Hughto and Clark, in press) and qualitative interviews with correctional healthcare providers (stage 4) (Clark et al., 2017). The specific content of the Phase I curriculum is described in-depth elsewhere (White Hughto and Clark, in press). Briefly, the Phase I curriculum primarily included cultural competence content including terminology, definitions, barriers to care, stigma as a risk factor for incarceration, and the experiences of transgender people in the criminal justice system drawn from formative research with recently incarcerated transgender women (White Hughto et al., in press). The clinical competence content of the Phase I curriculum covered best practices for interacting with transgender patients in clinical settings and the basics of taking a medical history. Findings from qualitative interviews with correctional healthcare providers (stage 4) highlighted significant training defficits related to transgender health, including misconceptions regarding the etiology of transgender experience (e.g., belief that trauma causes gender dysphoria), limited self-efficacy regarding the provision of hormone therapy to transgender patients, and institutional barriers to providing transgender care such as restrictive hormone policies (Clark et al., 2017). The clinical competence section of the Phase II intervention developed and tested here was significantly expanded to provide requisite clinical knowledge, while ensuring that any best practice recommendations were feasible in the context of existing structural barriers to care. The newly added clinical content was based on current best practice models of transgender care (Cavanaugh et al., 2016; Coleman et al., 2012; Deutsch, 2012; Reisner et al., 2015), and drew in part from existing clinical trainings from leading experts in transgender health (Cavanaugh et al., 2016; Makadon et al., 2008; Reisner et al., 2015). Drawing on the interviews with recently incarcerated transgender individuals (White Hughto et al., in press) and correctional providers (Clark et al., 2017), case studies pertaining to interactions with transgender inmates and patient care were added to the curriculum. Providers who participated in the Phase I pilot cited the opportunities to ask questions, discuss lecture components, and participate in role-play activities as highly valuable; thus, the intervention was expanded to include ample time for these activities. Finally, the Phase I curriculum was not grounded in a theoretical framework; thus, the Phase II intervention was refined to ensure that each intervention component mapped onto the hypothesized theoretical model described above and depicted in Fig. 1.
Fig. 1.
Hypothesized theoretical model.
Intervention components
The modular components of the intervention are shown in Table 1. The total intervention session lasted 90 minutes. Each intervention module lasted approximately 15–20 minutes and sought to target a primary or secondary outcome using the hypothesized theoretical framework (Fig. 1). Briefly, Module 1 aimed to address general transgender cultural competence through a lecture and group discussion. Module 2 aimed to address cultural competence related to transgender people’s experience in the criminal justice system and motivate providers’ willingness to provide gender-affirming care through a lecture and group discussion. Module 3 targeted general transgender clinical competence, subjective norms, and self-efficacy to care for transgender patients through a lecture and role-play exercises. Module 4 targeted clinical competence related to medical gender affirmation, clinical self-efficacy, and skills to provide clinical care to transgender patients through a lecture, case studies, and group discussion.
Table 1.
Intervention components.
| Module | Outcome Target | Theoretical Mechanism | Content |
|---|---|---|---|
| 1. Transgender 101 | |||
| Lecture & Discussion | Cultural Competence | Knowledge, Attitudes & Self-Efficacy |
|
| 2. Transgender People in the Criminal Justice System | |||
| Lecture & Discussion | Cultural Competence Willingness to Provide Care | Knowledge & Attitudes |
|
| 3. Healthcare Interactions with Transgender People | |||
| Lecture & Discussion | Clinical Competence Subjective Norms | Knowledge, Attitudes & Subjective Norms |
|
| Role Playing | Self-Efficacy | Self-Efficacy & Skills |
|
| 4. Transgender Medical Care | |||
| Lecture | Clinical Competence Subjective Norms | Knowledge, Attitudes, & Subjective Norms |
|
| Case Study & Discussion | Self-Efficacy | Self-Efficacy & Skills |
|
2.3. Measures
2.3.1. Provider characteristics
Demographics
Age was assessed in years. Participants were asked to indicate their race/ethnicity, which was coded as: White, Black, Hispanic, and Asian. Participants checking more than one category were coded as more than one race/ethnicity. Participants were also asked to report their sex at birth (i.e., male/female), gender identity (e.g., man, woman), sexual orientation (i.e., straight/heterosexual, gay/lesbian/homosexual, bisexual, other), and their political orientation (1 = very liberal to 5 = very conservative). All participants were cis-gender; thus, only gender identity is reported.
Training and experience
Participants were asked to indicate the number of years they had worked in their profession; their primary job role (e.g., administrator, counselor, nurse, physician, social worker); specialty training (e.g., family medicine, psychiatry, mental health counseling); and motivation for working in their profession (check all that apply: e.g., intellectual challenge, income/benefits, helping others). A provider type variable (i.e., mental health, physical health provider) was also created. Additionally, participants were asked whether they had cared for a transgender patient and whether they had previously attended trainings on transgender health topics.
Workplace
Participants were asked whether they worked primarily at a male or female correctional facility or a facility where males and females were housed separately. Participants also noted the state where the intervention was conducted/where participants were employed (Connecticut vs. Massachusetts).
2.3.2. Test of potential intervention efficacy: Primary outcome
Willingness to provide gender-affirming care
Providers were asked whether they were willing to provide gender-affirming care to trans-gender patients with response options ranging from 1 = strongly disagree to 5 = strongly agree.
2.3.3. Tests of potential intervention efficacy: Secondary outcomes
Cultural competence
Cultural competence related to transgender care was assessed using the 22-item Transgender Knowledge, Attitudes, and Beliefs (TKAB) scale, previously validated among the general population (Clark and White Hughto, 2017) and healthcare providers (White Hughto et al., 2017). The TKAB quantifies providers’ knowledge about transgender individuals (e.g., transgender terminology and definitions) and assesses beliefs including transgender stigma and willingness to interact with transgender individuals across a variety of social contexts (e.g., workplace, socially). Each item was assessed from 1 = strongly disagree to 4 = strongly agree. Items were summed (theoretical range: 22–88), with higher scores representing greater cultural competence (i.e., greater cultural knowledge, more supportive attitudes, less bias). Cronbach’s α for the sample was 0.96 for all time points.
Clinical competence
Clinical competence was assessed using the 21-item Transgender Clinical Competence (TCC) scale, previously validated in a sample of healthcare providers (White Hughto et al., 2017). The scale includes two components: General Healthcare Knowledge (12 items) and Medical Gender Affirmation Knowledge (9 items). Examples of general knowledge items include: “Gender identity issues are often caused by trauma” and “Transgender people may avoid healthcare because they fear mistreatment.” Examples of medical gender affirmation knowledge items include, “Heredity and age limit the effectiveness of hormone therapy” and “Facial/body hair growth is often an effect of testosterone therapy.” All items were measured from 1 = strongly disagree to 4 = strongly agree. Items were summed (theoretical range: General Knowledge = 12–48; Medical Gender Affirmation Knowledge: 9–36), with higher scores representing greater clinical competence. Cronbach’s α was: General Healthcare Knowledge: 0.80 at baseline and 0.77 at immediate follow-up; 0.76 at 3-month follow-up; and Gender Affirmation Knowledge: 0.77 at baseline, 0.81 at immediate follow-up, and 0.75 at 3-month follow-up.
Self-efficacy
Self-efficacy to provide medical gender affirmation therapies was assessed using three items used in prior intervention research on transgender health topics (Thomas and Safer, 2015). Participants were asked from 1 = strongly disagree to 4 = strongly agree whether they felt “sufficiently knowledgeable” to help a Female-to-Male (FtM) transgender person (i.e., transgender man) initiate hormone therapy; help a Male-to-Female (MtF) transgender person (i.e., trans-gender woman) initiate hormone therapy; and help a transgender person who has been on hormone therapy for five years continue hormone therapy.
Subjective norms
Subjective norms to provide gender-affirming care (referred to as “gender affirmative” care in the following items) was assessed using an 8-item scale previously validated in a sample of healthcare providers (White Hughto et al., 2017). Items were measured from 1 = strongly disagree to 5 = strongly agree and included: “Providing gender affirmative care to transgender patients is a priority at my workplace” and “People who influence my clinical behavior think that I should provide gender affirmative care to transgender patients.” Items were summed to create one continuous measure (theoretical range: 8–40) where higher scores indicate more supportive norms related to transgender care. Cronbach’s α was: 0.84 at baseline, 0.85 at immediate follow-up, and 0.86 at 3-month follow-up.
Intervention feasibility and acceptability
Participant enrollment, training attendance, and survey completion were documented to assess the feasibility of recruitment and retention. Intervention acceptability was assessed via the immediate post-intervention survey by asking participants to report whether the study benefited them in any way (1 = yes, 0 = no); and if yes, the specific benefits the intervention provided (all items: 1 = yes, = no): increased knowledge; increased skills; continuing medical education credits; personal fulfillment; and time off work. Participants were also asked whether they would recommend the training to others (1 = yes, = no). Additionally, participants were provided with open-ended survey questions assessing intervention acceptability and feasibility, including whether they had access to the necessary resources to adhere to study procedures (e.g., time and computer to take the survey), the usefulness of intervention content, and recommendations to improve the intervention curriculum and/or study procedures. At 3-month follow-up participants were asked to indicate whether they had cared for one or more transgender patient in the past 3-months (1 = yes, 0 = no) and whether they had applied what they learned in the training in caring for transgender patients (1 = yes, 0 = no). A semi-structured interview guide was used to obtain in-depth feedback on intervention feasibility and acceptability from the participants (n = 9) who completed exit interviews (Tarnowski and Simonian, 1992). Interviews assessed participants’ perceptions regarding the feasibility and acceptability of the survey procedures, intervention delivery and structure (e.g., training location, length, and format), and curriculum content, including which aspects of the intervention were most relevant to their work. Participants were also asked about future recommendations, including which aspects of the intervention should be retained or improved upon and whether or not they would recommend the training to others.
2.4. Data analysis
SAS version 9.4 was used for all quantitative analyses, with statistical significance determined at p < 0.05. Descriptive statistics were obtained for all variables (frequencies, means, standard deviations, ranges) and the presence of outliers was evaluated. Demographic differences between the recruited and enrolled providers, as well as study completers, were analyzed using T-Tests (continuous variables) and Chi-Square analyses (categorical variables).
Effect sizes were calculated for mean changes in all outcomes from baseline to post-intervention (Cohen’s d for same sample size) and baseline to 3-months post-intervention (Hedges’ g for different sample sizes). Mean outcome scores were plotted in graphs. Tests for normality were obtained for all continuous measures to ensure that all statistical assumptions were met for linear regression (e.g., linearity, normality). Because a longitudinal, repeated measures design was utilized to collect identical measures on the same individuals over three measurement occasions, all measures were positively correlated over each measurement occasion—violating the fundamental assumption of independence required for many standard regression techniques (Fitzmaurice et al., 2004; Singer and Willett, 2003). The PROC MIXED procedure in SAS was used to obtain maximum likelihood estimates (METHOD = ML) and REPEATED = ID was used to account for correlated measurements. Different covariance structures were examined, and model fit was compared using the Akaike Information Criterion (AIC). Based on model fit (lowest AIC), a compound symmetry covariance structure was used for all models (TYPE = CS).
A series of linear regression models were fit to assess change over time for the primary continuous outcome: (1) willingness to provide gender-affirming care to transgender patients and the secondary outcomes: (2) transgender cultural competence; transgender clinical competence: (3) general transgender healthcare knowledge and (4) gender affirmation clinical knowledge; (5) institutional subjective norms to care for transgender patients; and self-efficacy to provide medical gender affirmation care; (6) initiate hormones for transgender men; (7) initiate hormones for transgender women; and (8) continue hormones for a transgender patient. Time was the primary predictor (main effects) and baseline (time 0) was the specified referent in each fitted model. All models adjusted for providers’ baseline age and provider type.
Due to the small sample size, it was not possible to test the full hypothesized theoretical model; however, correlations between the outcomes were examined post-intervention to assess whether they were related and in the hypothesized direction.
Qualitative data were analyzed using thematic analysis (Braun and Clarke, 2006). Specifically, the first author organized open-ended survey data and exit interview data according to codes derived from the exit interview research questions (e.g., utility of intervention, acceptability of intervention, areas for improvement). Qualitative findings were then compared to quantitative findings to further contextualize intervention feasibility and acceptability. The first author met frequently with the authorship team to discuss the application of codes and develop and refine the analysis.
3. Results
3.1. Sample characteristics
Sample characteristics of the 34 participants who enrolled in the study and completed at least one follow-up survey are shown in Table 2. Participants had a mean age of 44.3 years (SD = 11.4) and had worked as a correctional healthcare provider for an average of 14.5 years (SD = 10.2). The majority of the sample were White (61.8%), cisgender women (61.8%), and straight/heterosexual (94.1%); one woman identified as bisexual and one man identified as gay. Regarding, political beliefs, half of the sample identified as liberal (44.1% liberal; 5.9% very liberal), while the other half identified as moderate (38.2%) or conservative (11.8%). The majority (64.7%) of participants were physical health providers (e.g., primary care providers) and 35.3% were mental health providers (e.g., psychologists, social workers). More than half of participants worked exclusively in a male correctional facility (58.8%), 32.4% worked in facilities that house males and females separately, and 8.8% worked exclusively in a female facility. At baseline, 29.4% of participants had no prior experience caring for a transgender patient and less than a quarter (23.5%) had ever attended a training on transgender health topics.
Table 2.
Baseline characteristics of study participants (N = 34).
| Mean | SD | |
|---|---|---|
| Age, continuous | 44.3 | 11.4 |
| Range | 24 | 70 |
| Years in Profession | 14.5 | 10.2 |
| Range | 0.8 | 35.0 |
| Race/Ethnicity | N | % |
|
| ||
| White | 21 | 61.8 |
| Black | 5 | 14.7 |
| Hispanic | 2 | 5.9 |
| Asian | 4 | 11.8 |
| More than one race | 2 | 5.9 |
| Gender Identity | ||
| Man | 13 | 38.2 |
| Woman | 21 | 61.8 |
| Location | ||
| Connecticut | 21 | 61.8 |
| Massachusetts | 13 | 38.2 |
| Sexual Orientation | ||
| Straight | 32 | 94.1 |
| Bisexual | 1 | 2.9 |
| Gay/Lesbian | 1 | 2.9 |
| Political Orientation | ||
| Very Liberal | 2 | 5.9 |
| Liberal | 15 | 44.1 |
| Moderate | 13 | 38.2 |
| Conservative | 4 | 11.8 |
| Job Rolea | ||
| Administrator | 2 | 5.9 |
| Case manager | 1 | 2.9 |
| Counselor | 2 | 5.9 |
| Nurse | 10 | 29.4 |
| Nurse Practitioner | 5 | 14.7 |
| Optometrist | 1 | 2.9 |
| Primary Care Physician | 6 | 17.6 |
| Psychiatrist | 1 | 2.9 |
| Social Worker | 8 | 23.5 |
| Facility where Employed | ||
| Male | 20 | 58.8 |
| Female | 3 | 8.8 |
| Bothb | 11 | 32.4 |
| Cared for Transgender Patient | ||
| Yes | 24 | 70.6 |
| No | 10 | 29.4 |
| Attended Training on Transgender Health | ||
| Yes | 8 | 23.5 |
| No | 26 | 76.5 |
Not mutually exclusive (check all that apply response format).
Both = Worked in a facility that houses males and females.
3.2. Tests of preliminary efficacy
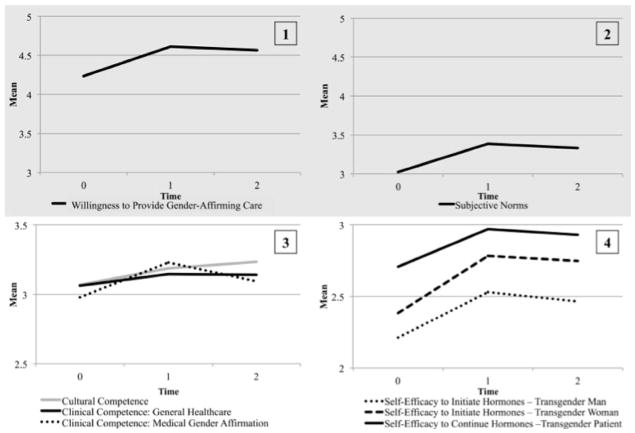
Table 3 presents the means, standard deviations at baseline, immediate follow-up, and 3-months post-intervention as well as effect sizes. At baseline, participants demonstrated moderate levels of: willingness to provide care to transgender patients (M = 4.20; SD = 0.61), cultural competence (M = 67.54; SD = 11.61), and clinical competence (general healthcare knowledge: M = 36.74; SD = 4.29; medical gender affirmation knowledge: M = 26.81; SD = 3.00). Self-efficacy to provide medical gender affirmation tended to be low, with the mean value for continuing hormone therapy for a transgender patient (M = 2.71; SD = 0.80) higher than the mean value for initiating hormone therapy for a transgender man (M = 2.21; SD = 0.74) or transgender woman (M = 2.38; SD = 0.78). Subjective norms related to caring for transgender patients were in the moderate range at baseline (M = 24.15; SD = 5.37). Compared to baseline, all outcome variables increased immediately post-intervention, with a moderate effect size for the primary outcome: willingness to provide gender-affirming care (time 1: Cohen’s d = 0.76; time 2: Hedges’ g = 0.66), and small to moderate effect sizes for the secondary outcomes. Fig. 2 depicts the change in outcomes over time.
Table 3.
Primary and secondary outcomes at baseline, acute follow-up, and 3-month follow-up.
| Baseline (N = 34) | Immediate follow-up (N = 34) | Effect size | 3 month follow-up (N = 28) | Effect size | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Mean | SD | Mean | SD | Δ T0 - T1 | Mean | SD | Δ T0 - T2 | |
| Primary Outcome | ||||||||
| 1. Willingness to Provide Gender-Affirming Care | 4.20 | 0.61 | 4.62 | 0.49 | 0.76 | 4.57 | 0.50 | 0.66 |
| Range | 3 | 5 | 4 | 5 | 4 | 5 | ||
| Secondary Outcomes | ||||||||
| 2. Transgender Cultural Competence | 67.54 | 11.64 | 70.15 | 10.69 | 0.23 | 71.21 | 10.92 | 0.32 |
| Range | 43 | 88 | 45 | 88 | 51 | 88 | ||
| Transgender Clinical Competence | ||||||||
| 3. General Health Knowledge | 36.74 | 4.29 | 37.76 | 4.36 | 0.24 | 37.71 | 4.07 | 0.23 |
| Range | 28 | 44 | 29 | 47 | 29 | 47 | ||
| 4. Medical Gender Affirmation Knowledge | 26.81 | 3.00 | 29.09 | 3.32 | 0.72 | 27.86 | 2.97 | 0.35 |
| Range | 22 | 36 | 25 | 36 | 24 | 36 | ||
| Self-Efficacy | ||||||||
| 5. Initiate Hormones - Transgender Man | 2.21 | 0.74 | 2.53 | 0.76 | 0.43 | 2.46 | 0.84 | 0.32 |
| Range | 1 | 4 | 1 | 5 | 1 | 5 | ||
| 6. Initiate Hormones -Transgender Woman | 2.38 | 0.78 | 2.78 | 0.55 | 0.59 | 2.75 | 0.70 | 0.50 |
| Range | 1 | 5 | 1 | 5 | 1 | 5 | ||
| 7. Continue Hormones - Transgender Patient | 2.71 | 0.80 | 2.97 | 0.64 | 0.36 | 2.93 | 0.66 | 0.30 |
| Range | 1 | 5 | 1 | 5 | 1 | 5 | ||
| 8. Subjective Norms Related to Transgender Care | 24.15 | 5.37 | 27.06 | 5.33 | 0.54 | 26.68 | 5.24 | 0.48 |
| Range | 15 | 37 | 16 | 37 | 17 | 36 | ||
Note. Theoretical Ranges: Willingness (1–5); Cultural Competence (22–88); General Health Knowledge (12–48); Gender Affirmation Knowledge (9–36); All Self-Efficacy items (1–4); and Subjective Norms (8–40). Effect size: Cohen’s d used for T0-T1 comparison; Hedges’ g used for T0-T2 comparison due to different sample sizes at each time point. Effect size interpretation: 0.30 = small; 0.50 = medium; 0.80 = large.
Fig. 2.
Graphical display of mean change in study outcomes over time. Note. The measures depicted in graphs 1 and 2 were assessed on a 5-point scale from 1 = strongly disagree to 5 = strongly agree. The measures depicted in graphs 3 and 4 were assessed on a 4-point scale from 1 = strongly disagree to 4 = strongly agree. The subjective norms (graph 2) and competence measures (graph 3) were divided by the number of scale items to obtain an average score at each time point.
Table 4 presents fitted linear models regressing the outcomes on time. Mean willingness to provide gender-affirming care increased significantly from baseline to immediately post-intervention (β = 0.38; SE = 0.09; p < 0.0010) and from baseline to 3-months post-intervention (β = 0.36; SE = 0.09; p < 0.001) (Model 1: test of fixed effects χ2 = 23.21; df = 2, 60; p < 0.001). Similarly, mean cultural competence scores significantly increased from baseline to post-intervention (β = 2.21; SE = 1.21; p = 0.03) and from baseline to 3-months post-intervention (β = 3.66; SE = 1.30; p = 0.01) (Model 2: test of fixed effects χ2 = 8.86; df = 2, 60; p = 0.01). Regarding clinical competence, the mean medical gender affirmation knowledge score significantly increased from baseline to post-intervention (β = 2.28; SE = 0.48; p < 0.001), but only approached significance from baseline to 3-months post-intervention (β = 0.93; SE = 0.52; p = 0.08), although the global test of fixed effects was significant (Model 4: χ2 = 22.49; df = 2, 60; p < 0.001). For general medical knowledge, scores increased post-intervention, but only approached statistical significance from baseline to post-intervention (β = 1.02; SE = 0.57; p = 0.08) and from baseline to 3-months post-intervention (β = 1.05; SE = 0.61; p = 0.09) (Model 3: test of fixed effects χ2 = 4.16; df = 2, 60; p = 0.13). All self-efficacy scores significantly increased from baseline to immediately post-intervention: initiate hormones for a transgender man (β = 0.32; SE = 0.15; p = 0.04); initiate hormones for a transgender woman (β = 0.39; SE = 0.13; p = 0.004); continue hormones for a transgender patient (β = 0.27; SE = 0.12; p = 0.03). From baseline to 3-months post intervention, however, only increases in the initiating hormones for a transgender woman score was statistically significant (β = 0.36; SE = 0.14; p = 0.01; Model 6: test of fixed effects χ2 = 11.24; df = 2, 60; p = 0.01), while self-efficacy to initiate hormones for a transgender man (β = 0.31; SE = 0.16; p = 0.06; Model 5: test of fixed effects χ2 = 5.67; df = 2, 60; p = 0.07) and selfefficacy to continue hormones for a transgender patient increased, but did not reach statistical significance (β = 0.19; SE = 0.13; p = 0.15; Model 7: test of fixed effects χ2 = 4.94; df = 2, 60; p = 0.09). Finally, increases in subjective norms were statistically significant from baseline to immediately post-intervention (β = 2.87; SE = 0.84; p = 0.001) and from baseline to 3-months post-intervention (β = 2.78; SE = 0.89; p = 0.003; Model 8: test of fixed effects χ2 = 14.69; df = 2, 60; p = 0.001).
Table 4.
Repeated measures linear models regressing outcomes on time of assessment.
| Models | Intercept | Base (T0) | Immediate follow-up (T1) | 3-month follow-up (T2) | Test of fixed effects | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||||
| Beta | SE | P-Value | Ref | Beta | SE | P-Value | Beta | SE | P-Value | X2 | df, N, D | P-Value | |
| Primary Outcome | |||||||||||||
| 1. Willingness to Provide Gender-Affirming Care | 5.11 | 0.41 | < 0.001 | Ref | 0.38 | 0.09 | < 0.001 | 0.36 | 0.09 | < 0.001 | 23.21 | 2, 60 | < 0.001 |
| Secondary Outcomes | |||||||||||||
| 2. Transgender Cultural Competence | 83.4 | 9.17 | < 0.001 | Ref | 2.61 | 1.21 | 0.03 | 3.66 | 1.30 | 0.01 | 8.86 | 2, 60 | 0.01 |
| Transgender Clinical Competence | |||||||||||||
| 3. General Health Knowledge | 41.96 | 3.57 | < 0.001 | Ref | 1.02 | 0.57 | 0.08 | 1.05 | 0.61 | 0.09 | 4.16 | 2, 60 | 0.13 |
| 4. Medical Gender Affirmation Knowledge | 31.89 | 2.61 | < 0.001 | Ref | 2.28 | 0.48 | < 0.001 | 0.93 | 0.52 | 0.08 | 22.49 | 2, 60 | < 0.001 |
| Self-Efficacy | |||||||||||||
| 5. Initiate Hormones - Transgender Man | 1.4 | 0.56 | 0.02 | Ref | 0.32 | 0.15 | 0.04 | 0.31 | 0.16 | 0.06 | 5.67 | 2, 60 | 0.07 |
| 6. Initiate Hormones - Transgender Woman | 1.91 | 0.56 | 0.002 | Ref | 0.39 | 0.13 | 0.004 | 0.36 | 0.14 | 0.01 | 11.24 | 2, 60 | 0.01 |
| 7. Continue Hormones - Transgender Patient | 2.03 | 0.59 | < 0.001 | Ref | 0.27 | 0.12 | 0.03 | 0.19 | 0.13 | 0.15 | 4.94 | 2, 60 | 0.09 |
| 8. Subjective Norms Related to Transgender Care | 27.38 | 4.14 | < 0.001 | Ref | 2.87 | 0.84 | 0.001 | 2.78 | 0.89 | 0.003 | 14.69 | 2, 60 | 0.001 |
Note. SE = Standard Error; df, N, D = degrees of freedom, Number, Density. Bolded p-values = significant at p < 0.05; italicized = Marginally significant p < 0.10; all models adjusted for providers’ baseline age and provider type.
Correlations between outcome variables were in the hypothesized direction, consistent with the theoretical model (Table 5). Specifically, willingness to provide gender-affirming care (primary outcome) was positively correlated with cultural competence, clinical competence (i.e., general health knowledge and medical gender affirmation knowledge), clinical self-efficacy (i.e., initiate hormones for a trans-gender woman), and subjective norms related to transgender care. Cultural competence was not correlated with any measures of clinical self-efficacy; however, it was positively correlated with subjective norms and general healthcare competence. The measures of clinical competence were positively correlated with one another and subjective norms to care for transgender patients. Medical gender affirmation knowledge was also positively correlated with clinical self-efficacy to continue hormones for a transgender patient, and all measures of selfefficacy were positively correlated with one another.
Table 5.
Bivariate correlations of study outcomes.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Willingness to Provide Gender-Affirming Care | 1.00 | 0.47** | 0.61** | 0.50** | 0.01 | 0.44** | 0.16 | 0.53** |
| 2. Transgender Cultural Competence | 1.00 | 0.64** | 0.34 | 0.11 | 0.02 | 0.19 | 0.52* | |
| Transgender Clinical Competence | ||||||||
| 3. General Health Knowledge | 1.00 | 0.59** | 0.06 | 0.18 | 0.26 | 0.56** | ||
| 4. Medical Gender Affirmation Knowledge | 1.00 | −0.04 | 0.14 | 0.44* | 0.37* | |||
| Self-Efficacy | ||||||||
| 5. Initiate Hormones - Transgender Man | 1.00 | 0.44* | 0.36* | 0.37* | ||||
| 6. Initiate Hormones - Transgender Woman | 1.00 | 0.52** | 0.24 | |||||
| 7. Continue Hormones - Transgender Patient | 1.00 | 0.16 | ||||||
| 8. Subjective Norms Related to Transgender Care | 1.00 | |||||||
p < 0.05;
p < 0.01.
3.3. Feasibility and acceptability
At 3-month follow-up, 67.9% of the sample reported having cared for a transgender patient since participating in the intervention. All of the providers who had cared for a transgender patient at follow-up (n = 19) reported having applied what they learned during the training to patient care, demonstrating the utility of the intervention to impact the care provided to transgender patients.
Qualitative data from the open-ended survey questions (n = 34) and in-depth exit interviews (n = 9) revealed that participants found the intervention curriculum to be highly acceptable (see online appendix). Participants appreciated the diversity of topics covered and found the medical/correctional healthcare case studies and depth of the cultural competence content valuable. Participants highlighted the role-playing exercises, discussions, and multiple opportunities to ask questions as particularly useful components of the intervention. Participants also appreciated that the intervention was sponsored by their employer and embedded into their workday. Overall, participants found the length and format of the training appropriate; two participants indicated that they would like the training to be longer to allow more time for role-playing exercises and discussions. When asked what areas of the intervention could be improved, the majority of participants indicated via both the survey and exit interviews that they did not believe that any changes were needed. Among those who suggested changes to the intervention, there was some disagreement. One participant indicated that there was too much content, which the participant found overwhelming. Conversely, a few participants reported that they were already culturally competent and would like to see more medical content related to hormone dosing and monitoring as well as mental health therapies. Additionally, several participants indicated via the survey that they would like to see more stories from transgender individuals integrated into the training. Various methods of including transgender people’s stories were proposed to participants during the exit interviews (e.g., the inclusion of a transgender facilitator, more case studies, video clips). Exit interviewees overwhelmingly agreed that video clips of transgender individuals telling their stories would be an optimal platform as these clips would place less burden on a single transgender facilitator, allow for a diversity of experiences to be shared, and provide the space for participants to ask sensitive questions.
All but one participant indicated that the intervention benefited them in some way. Increased knowledge was the most frequently reported benefit (97.1%), followed by increased skills (41.1%); continuing medical education credits (26.5%); personal fulfillment (5.8%), and time off work (5.8%). During exit interviews, nearly all participants reported that this was a much-needed training for correctional health-care providers, as most participants had not received any formal training in transgender care. Finally, 100% of providers indicated that they would recommend the training to others, including correctional healthcare providers in other facilities and states, and custody staff.
4. Discussion
Findings from this study demonstrate the feasibility, acceptability, and preliminary efficacy of a novel transgender cultural and clinical competence intervention for correctional healthcare providers. Building on formative work (White Hughto and Clark, in press), the present study represents the first theoretically-informed intervention to exhibit significant improvements in correctional healthcare providers’ trans-gender cultural and clinical competence, self-efficacy to care for transgender patients, subjective norms related to transgender care, and willingness to provide gender-affirming care to transgender patients. The intervention is novel in its use of a curriculum informed by behavioral change theory (Ajzen, 1991; Fisher et al., 2002), and adapted to the correctional environment. Consistent with the goals of this study, a cultural and clinical competence curriculum was successfully delivered to providers who had limited prior training in transgender health. The majority of correctional healthcare providers found the intervention to be both feasible and acceptable. Given the potential for this intervention to increase access to gender-affirming care and ultimately improve the health of incarcerated transgender patients, future testing of the intervention using a randomized controlled design is warranted.
While not the primary aim of this feasibility and acceptability study, this intervention for correctional healthcare providers demonstrated significant increases in the primary outcome, willingness to provide gender-affirming care, and nearly all secondary outcomes including measures of cultural and clinical competence, self-efficacy to care for transgender patients, and perceived subjective norms surrounding transgender care. Interventions that only target transgender cultural and clinical knowledge, without giving participants the skills necessary to provide culturally and clinically competent care (self-efficacy), are unlikely to increase a provider’s willingness to provide gender-affirming care to transgender patients (Ajzen, 1991). Further, while self-efficacy enables providers to affirm their patients’ gender in the context of care (Ajzen, 1991), willingness to provide care can be diminished in unsupportive environments (Clark et al., 2017). Indeed, in qualitative research with correctional healthcare providers, many clinicians felt that providing gender-affirming care was not a priority at their work-place, which lessened their motivation to provide such care (Clark et al., 2017). By embedding the present intervention into a day of training sponsored by the participants’ employer, working with supervisors to recruit participants, and ensuring that supervisors were in attendance at the training, the present study was able to highlight the institutional support required for the provision of gender-affirming care, which likely increased participants’ subjective norms regarding institutional support for transgender patient care. Additionally, in light of prior research showing that correctional providers may face other structural challenges to providing gender-affirming care, such as lack of support from correctional officers and other custody staff (Clark et al., 2017), the intervention alerted providers to aspects of their workplace that could be leveraged in overcoming these barriers to care. For example, using case studies developed from formative work with correctional healthcare providers (Clark et al., 2017), participants were encouraged to the extent possible to use the privacy of their exam room to affirm patients’ gender (e.g., referring to patients by their preferred name and pronoun) regardless of whether these behaviors were congruent with the practices of custody staff. In cases where providers felt that the use of gendered terminology might be problematic for patients (e.g., that doing so would “out” patients to other inmates or custody staff), participants were encouraged to capitalize on the normative, genderless language used by custody staff and refer to patients using only their last name – a strategy appreciated and encouraged by recently incarcerated transgender women (White Hughto et al., in press). Together, these strategies helped to shape providers’ subjective norms and instill the essential competencies and self-efficacy necessary to increase providers’ capacity and willingness to deliver gender-affirming care to incarcerated transgender patients.
While the increase in willingness to provide gender-affirming care was significant at all time points, a few of the secondary outcomes did not reach statistical significance at one or more follow-up points. For example, only one measure of clinical competence (i.e., medical gender affirmation knowledge) reached statistical significance at the first time point, while two of the three measures of self-efficacy (i.e., ability to initiate hormones for a transgender man and ability to continue hormones for any transgender patient) significantly increased post-intervention, but were not sustained at 3-month follow-up. The limited increase in general medical knowledge may be indicative of the technical nature of this content, which may be difficult to retain without regular application (Marinopoulos et al., 2007). Since a third of the sample had not cared for a transgender patient in the 3-months following the intervention, it is possible that the limited opportunity to apply their medical knowledge to the care of transgender patients resulted in reductions in this knowledge over time. Also, the majority of participants worked in male facilities and would be more likely to care for trans-gender women in these settings rather than transgender men; thus, the lack of clinical exposure to transgender men might be responsible for participants’ reduced self-efficacy to provide hormones to this population over time. Given that transgender individuals continue to face disproportionate incarceration (Grant et al., 2011) relative to the general population (Glaze and Kaeble, 2014) and access to gender-affirming care is critical to their psychological and physical health while incarcerated (Brown and McDuffie, 2009; Edney, 2004; Tarzwell, 2006; White Hughto et al., in press), correctional providers must be prepared to meet the needs of incarcerated transgender patients. Continuing transgender health education should be made available to providers through semi-annual refresher courses. Additionally, interactive, web-based trainings should be developed for primary and refresher courses to ensure that both new and existing staff are appropriately trained in transgender health competencies and thus capable and willing to provide gender-affirming care to their incarcerated transgender patients.
Finally, most providers reported limited prior exposure to trans-gender health topics and indicated that the intervention filled a gap in their training and was particularly needed in correctional settings. To accommodate the diverse medical specialties of participating providers, the intervention curriculum was designed to cover extensive cultural competence issues and the essential clinical competencies that are relevant to all providers, regardless of medical specialty. Overall, the intervention met the needs of most providers; however, a small subset of providers indicated that they were already culturally competent and expressed the need for more training on mental health treatments for transgender patients as well as hormone dosing and monitoring. Given the variability in baseline exposure to transgender health topics and the different training goals of physical health providers as compared to mental health providers, future testing of the intervention might entail refining and piloting the training or specific modules by provider type in order to deliver tailored information that meets the needs of primary care and mental health providers. Additionally, while the intervention includes case studies and personal narratives of transgender people who accessed healthcare in correctional settings, the intervention was delivered by cisgender facilitators, and time constraints precluded the discussion of numerous case studies. Participants endorsed the creation video clips of diverse transgender individuals sharing their incarceration experiences that could be integrated into future trainings. Participants perceived the inclusion of video clips, rather than a transgender speaker, as placing less burden on a single transgender facilitator, while also allowing for the presentation of varied experiences, the space to ask sensitive questions, and a curriculum that is consistent and sustainable over time.
These findings are most appropriately interpreted in the context of study design limitations and participant non-response at follow-up. While recruitment and retention were largely feasible, selection bias might have influenced which providers completed the surveys (e.g., providers with less time or interest in the topic may have been less likely to take the surveys than those with more time or interest). Moreover, due to scheduling challenges and an inability to reach one provider, only nine of the 12 recruited providers completed the in-depth exit interviews. Limited research-related resources, such as inconsistent access to a computer for all staff and limited work time to take the survey, may have also contributed to recruitment and retention issues. However, comparison of provider demographics did not show any significant differences among those who enrolled in the study, those who only attended the training, and those who completed the study. Additionally, while the small sample size precluded the testing of the theoretical mechanisms underlying the significant changes in provider willingness to provide gender-affirming care, correlations between all variables were consistent with the hypothesized model, highlighting the potential utility of the model in future efficacy testing of the intervention. Additionally, the present study only assessed willingness to provide gender-affirming care to transgender patients and did not measure whether improvements in provider competencies, selfefficacy, norms, and willingness impacted the quality of healthcare provided to incarcerated transgender patients.
Although this study showed promising changes in provider outcomes from pre- to post-intervention, future research should test these changes against an active control group, including a standard clinical competence curriculum. Also, given the implementation science approach used, which included working with correctional administrators to recruit participants and embed the training into continuing education trainings, the feasibility findings may not generalize to other correctional institutions where administrators may be less amenable to supporting efforts to train their staff in transgender cultural and clinical competencies. Further, although the intervention was developed in consultation with leading transgender health clinicians and delivered by facilitators with transgender health expertise, the facilitators were not clinicians. Nonetheless, the facilitators were able to answer all clinical questions asked by participants. Additionally, while the content of the intervention was considered appropriate for the varied types of providers in attendance (e.g., primary care providers, mental health providers, social workers), future iterations of the intervention will aim to include breakout sessions by provider specialty led by clinical experts in that specialty. Finally, future research should assess inmate outcomes alongside provider outcomes in order to assess whether intervention effects translate into improved health.
Overall, this study represents an essential formative step towards developing and testing a potentially efficacious intervention for increasing correctional healthcare providers’ transgender cultural and clinical competence. Significant and sustained increases and moderate effect sizes in the primary outcome and most secondary outcomes suggest that the intervention has potential to improve providers’ willingness to care for transgender patients and improve their cultural and clinical competence, self-efficacy, and subjective norms for providing this care. Together with high levels of curriculum acceptability, these preliminary improvements suggest that the intervention is worthy of efficacy testing in a future randomized controlled trial. Educational efforts to increase correctional healthcare providers’ cultural and clinical competence to care for transgender patients represent a formidable step toward reducing barriers and improving transgender patients’ access to gender-affirming care in correctional settings.
Supplementary Material
Acknowledgments
This research was conducted with support from the Yale Fund for Gay and Lesbian Studies. Jaclyn White Hughto is supported by the National Institute on Minority Health and Health Disparities (1F31MD011203-01). Kirsty Clark acknowledges funding support from the Graduate Division, UCLA Fielding School of Public Health (Fellowship in Epidemiology, #104733842).
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.socscimed.2017.10.004.
References
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. [Google Scholar]
- Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behaviour. Prentice-Hall; Englewood Cliffs, NJ: 1980. [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- Brown GR. Qualitative analysis of transgender inmates’ correspondence implications for departments of correction. J Correct Health Care. 2014;20(4):334–342. doi: 10.1177/1078345814541533. [DOI] [PubMed] [Google Scholar]
- Brown GR, McDuffie E. Health care policies addressing transgender inmates in prison systems in the United States. J Correct Health Care. 2009;15(4):280–291. doi: 10.1177/1078345809340423. [DOI] [PubMed] [Google Scholar]
- Cavanaugh T, Hopwood R, Lambert C. Informed consent in the medical care of transgender and gender-nonconforming patients. AMA J Ethics. 2016;18(11):1147–1155. doi: 10.1001/journalofethics.2016.18.11.sect1-1611. [DOI] [PubMed] [Google Scholar]
- Chau PYK, Hu PJH. Investigating healthcare professionals’ decisions to accept telemedicine technology: an empirical test of competing theories. Inf Manag. 2002;39(4):297–311. [Google Scholar]
- Clark KA, White Hughto JM. Development and psychometric evaluation of the Transgender Knowledge, Attitudes, and Beliefs (T-KAB) scale. Paper presented at the 2017 USPATH Conference; Los Angeles, CA. 2017. [Google Scholar]
- Clark KA, White Hughto JM, Pachankis JE. “What’s the right thing to do?” Correctional healthcare providers’ knowledge, attitudes and experiences caring for transgender inmates. Soc Sci Med. 2017;193(Supplement C):80–89. doi: 10.1016/j.socscimed.2017.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, Fraser L, Green J, Knudson G, Meyer WJ. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgenderism. 2012;13(4):165–232. [Google Scholar]
- Deutsch MB. Use of the informed consent model in the provision of cross-sex hormone therapy: a survey of the practices of selected clinics. Int J Transgenderism. 2012;13(3):140–146. [Google Scholar]
- Edney R. To keep me safe from harm-transgender prisoners and the experience of imprisonment. Deakin Law Rev. 2004;9(2):327–338. [Google Scholar]
- Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychol. 2002;21(2):177–186. [PubMed] [Google Scholar]
- Fitzmaurice G, Laird N, Ware J. Applied Longitudinal Analysis. John Wiley & Sons, Inc; Hoboken, NJ: 2004. [Google Scholar]
- Flores AR, Herman JL, Gates GJ, Brown TNT. How Many Adults Identify as Transgender in the United States? Los Angeles, CA: 2016. http://williamsinstitute.law.ucla.edu/wp-content/uploads/How-Many-Adults-Identify-as-Transgender-in-the-United-States.pdf. [Google Scholar]
- Garofalo R, Deleon J, Osmer E, Doll M, Harper GW. Overlooked, misunderstood and at-risk: exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. J Adolesc Health. 2006;38(3):230–236. doi: 10.1016/j.jadohealth.2005.03.023. [DOI] [PubMed] [Google Scholar]
- Glaze L, Kaeble D. Correctional Populations in the United States, 2013. Washington, DC: 2014. http://www.bjs.gov/index.cfm?ty=pbdetail&iid=5177. [Google Scholar]
- Goffman E. Stigma: Notes on the Management of Spoiled Identity. Prentice-Hall; Englewood Cliffs, NJ: 1963. [Google Scholar]
- Grant JM, Mottet LA, Tanis LA, Harrison J, Herman JL, Keisling M. Injustice at Every Turn: a Report of the National Transgender Discrimination Survey. Washington, DC: 2011. http://www.thetaskforce.org/downloads/reports/reports/ntds_full.pdf. [Google Scholar]
- Hanssmann C, Morrison D, Russian E. Talking, gawking, or getting it done: provider trainings to increase cultural and clinical competence for transgender and gender-nonconforming patients and clients. Sex Res Soc Policy. 2008;5(1):5–23. [Google Scholar]
- Jaffer M, Ayad J, Tungol JG, MacDonald R, Dickey N, Venters H. Improving transgender healthcare in the New York City correctional system. LGBT health. 2016;3(2):116–121. doi: 10.1089/lgbt.2015.0050. [DOI] [PubMed] [Google Scholar]
- James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. The Report of the 2015 U.S. Transgender Survey. Washington, DC: 2016. http://www.ustranssurvey.org/report/ [Google Scholar]
- Jenness V, Sexton L, Sumner J. Transgender inmates in California’s prisons: an empirical study of a vulnerable population. The California Department of Corrections and Rehabilitation Wardens’ Meeting. 2009 Retrieved from. http://ucicorrections.seweb.uci.edu/files/2013/06/Transgender-Inmates-in-CAs-Prisons-An-Empirical-Study-of-a-Vulnerable-Population.pdf.
- Lydon J, Carrington K, Low H, Miller R, Yazdy M. Coming Out of Concrete Closets: a Report on Black and Pink’s LGBTQ Prisoner’ Survey. 2015 Retrieved from. http://www.blackandpink.org/wp-content/upLoads/Coming-Out-of-Concrete-Closets.-Black-and-Pink.-October-21-2015.pdf.
- Makadon HJ, Mayer KH, Potter J, Goldhammer H, editors. The Fenway Guide to Lesbian, Gay, Bisexual, and Transgender Health. ACP Press; Philadelphia, PA: 2008. [Google Scholar]
- Marinopoulos SS, Dorman T, Ratanawongsa N, Wilson LM, Ashar BH, Magaziner JL, Miller RG, Thomas PA, Prokopowicz GP, Qayyum R. Effectiveness of continuing medical education. Evid Report/Technology Assess. 2007;149(1):1–69. [PMC free article] [PubMed] [Google Scholar]
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, Eccles MP, Cane J, Wood CE. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- Reisner SL, Bailey Z, Sevelius J. Racial/ethnic disparities in history of incarceration, experiences of victimization, and associated health indicators among transgender women in the US. Women Health. 2014;54(8):750–767. doi: 10.1080/03630242.2014.932891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Bradford J, Hopwood R, Gonzalez A, Makadon H, Todisco D, Cavanaugh T, VanDerwarker R, Grasso C, Zaslow S. Comprehensive transgender healthcare: the gender affirming clinical and public health model of Fenway Health. J Urban Health. 2015;92(3):584–592. doi: 10.1007/s11524-015-9947-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblum D. Trapped in Sing Sing: transgendered prisoners caught in the gender binarism. Mich J Gend Law. 1999;6:499–571. [Google Scholar]
- Rounsaville BJ, Carroll KM. A stage model of behavioral therapies research: getting started and moving on from stage 1. Clin Psychol Sci Pract. 2001;8:133–142. [Google Scholar]
- Routh D, Abess G, Makin D, Stohr MK, Hemmens C, Yoo J. Transgender inmates in prisons: a review of applicable statutes and policies. Int J Offender Ther Comp Criminol. 2015;61(6):645–666. doi: 10.1177/0306624X15603745. [DOI] [PubMed] [Google Scholar]
- Rycroft-Malone J. The PARIHS framework — a framework for guiding the implementation of evidence-based practice. J Nurs Care Qual. 2004;19(4):297–304. doi: 10.1097/00001786-200410000-00002. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford University Press; New York, NY: 2003. [Google Scholar]
- Starace F, Massa A, Amico KR, Fisher JD. Adherence to antiretroviral therapy: an empirical test of the information-motivation-behavioral skills model. Health Psychol. 2006;25(2):153–162. doi: 10.1037/0278-6133.25.2.153. [DOI] [PubMed] [Google Scholar]
- Tarnowski KJ, Simonian SJ. Accessing treatment acceptability: the abbreviated acceptability rating profile. J Behav Ther Exp Psychiatry. 1992;23:101–106. doi: 10.1016/0005-7916(92)90007-6. [DOI] [PubMed] [Google Scholar]
- Tarzwell S. Gender liens are marked with razor wire: addressing state prison policies and practices for the management of transgender prisoners. Columbia Hum Rights Law Rev. 2006;38:167–219. [Google Scholar]
- Thomas DD, Safer JD. A simple intervention raised resident-physician willingness to assist transgender patients seeking hormone therapy. Endocr Pract. 2015;21(10):1134–1142. doi: 10.4158/EP15777.OR. [DOI] [PubMed] [Google Scholar]
- West C, Zimmerman DH. Doing gender. Gend Soc. 1987;1(2):125–151. [Google Scholar]
- Wolff KB, Cokely CL. “To protect and to serve?”: an exploration of police conduct in relation to the gay, lesbian, bisexual, and transgender community. Sex Cult. 2007;11(2):1–23. [Google Scholar]
- White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: a critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med. 2015;147:222–231. doi: 10.1016/j.socscimed.2015.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White Hughto JM, Clark K, Pachankis JE. Correlates of transgender cultural and clinical competency among healthcare providers in Massachusetts. Paper presented at the 145th American Public Health Association Conference; Atlanta, GA. 2017. [Google Scholar]
- White Hughto JM, Clark KA. Designing a transgender health training for correctional healthcare providers: a feasibility study. Prison J. doi: 10.1177/0032885519837237. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- White Hughto JM, Clark KA, Altice FL, Reisner SL, Kershaw TS, Pachankis JE. Creating, reinforcing, and resisting the gender binary: a qualitative study of transgender women’s healthcare experiences in sex-segregated jails and prisons. Int J Prison Health. doi: 10.1108/IJPH-02-2017-0011. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.