Abstract
Total knee arthroplasty (TKA) is a rewarding procedure in patients with hemophilia and end stage knee hemophilic arthropathy. However, this procedure might be associated with complications such as infection. There periprosthetic joint infection in patients with hemophilia is very well known, though we are not aware of any previous report on Brucella infection in this group of patients. Here, we reported a 28-year old man with Brucella infection of total knee replacement who initially underwent a conservative treatment followed bya two-stage revision. We believe that this report will alert physicians who work in endemic area for brucellosis to consider this in differential diagnosis and do the right intervention at the right time.
Keywords: Arthritis, Brucella, Hemophilia, Total knee arthroplasty
Introduction
Over the past years there has been a significant increase in the number of joint replacements for end stage joint destruction worldwide, which approximately about 800,000 hip and knee arthroplasties were only recorded in the United States (1). In patients with hemophilia, total knee arthroplasty (TKA) is a good option for end stage hemophilic arthropathy (2). The most serious complication of joint prosthesis which is also the second cause of revision TKA is periprosthetic joint infection (PJI), with an incidence of 1.5-2.5% for primary interventions in general population and 7% to 26.5% in haemophilic patients (3-5). The most frequent etiologic agents are staphylococci, accounting for more than 50% (4, 5). Brucellosis, also known as “undulant fever”, “Mediterranean fever” or “Malta fever” is a zoonosis and the infection is almost invariably transmitted by direct or indirect contact with infected animals or their products, whichis caused by small, gram-negative Coccobacilli (5, 6). Osteoarticular disease is the most common complication of brucellosis, globally (7, 8). Prosthetic infection due to Brucella spp. is extremely rare (9). To the best of our knowledge, only a few cases of Brucellosis after total prosthetic knee in the literature were reported (4, 5, 9-13). However, we are not aware of any previous report on Brucella infection of the total knee replacement in patients with hemophilia. We, therefore, report on knee PJI causing by Brucella species in a patient with hemophilia.
Case Report
A 28-year old man referred with pain and swelling of the right knee joint started 7 months ago. He was a known case of severe hemophilia type A and had a TKA of the right knee joint 4 years before the presentation at our institution because of severe destructive hemophilic arthropathy. After the surgery he didn’t have any problem with the knee until he started feeling pain, swelling and limitations in the range of motion in the operated knee joint for two months. He also complained of general symptoms including fatigue, low-grade fever and night sweats. He did not have any history of trauma. Laboratory tests showed white blood cell count of4900cells/mm3 (Neutrophil: 56%, Lymphocyte: 42%), hemoglobin 12.7 g/dl, platelets count 216×109/l, C-reactive protein (CRP) 44 mg/L and erythrocyte sedimentation rate (ESR) 51mm/h. We have performed joint aspiration for diagnosis of periprosthetic infection and the specimens interpreted based on the results of the culture as well as the white cell count and differential. However, the results revealed nothing in favor of an acute bacterial infection. Considering the indolent and sub-acute course of the disease and positive history of using the non-pasteurized dairy products, we did the serological tests for brucellosis, which confirmed high titer of brucellosis standard tube agglutination (STA) (1/1280). We reaspirated the synovial fluid to run PCR test for brucellosis and tuberculosis. It was positive for brucellosis (Brucella Melitensis) and negative for tuberculosis. We also sent a sample for culture in special media (BACTEC) and brucella has been isolated on the 14th day of incubation in Bac-Tec media. Plain radiography of the right knee joint showed effusion and soft tissue swelling but the prosthesis was stable and had no evidence of loosening. We started antibiotic therapy using doxycycline (200mg/d), rifampin (900mg/d) and trimethorim-sulfamethoxazole (800mg of sulfamethoxazole and 160 mg of trimethoprim). Patient didn’t reply to one-month course of antibiotic therapy, therefore, we continued the treatment for the next six months based on infectious disease consult. A remission of clinical symptoms such as pain and joint swelling as well as a reduction in titer of brucellosis STA test (1/640) made us to discontinue the drug after this course. Unfortunately the disease relapsed after one month with clinical symptoms such as fever, night sweats, pain and swelling of the right knee joint. Serologic tests revealed an upsurge in the titer of brucella STA test (1/2560). A combination therapy of gentamycin (intravenous for one week) and ceftriaxone (intravenous for two weeks) accompanied with doxycycline, rifampin and ciprofloxacin (oral for one month) was administered and followed by additional six months of combination therapy of rifampin and doxycycline. The clinical response was suitable but again with cessation of drugs, clinical relapse and a rise in titer of brucella STA test (1/2560) occurred. The requested plain radiography revealed loosening of prosthesis [Figure 1]. After eighteen months of conservative treatment, a two-stage surgery was planned in order to eradicate the infection. At the first stage, a radical debridement and copious irrigation were performed along the removal of prosthetic components. During the surgery, the femoral component was obviously loose and we could remove the both components without any bone loss. Following the surgery, combination therapy with doxycycline and rifampin continued. We sent three intra-operative specimens for culture on specialized media and all of them remained negative after prolonged incubation period. After four months, improvement in clinical symptoms, returning of serum markers including ESR and CRP back to the normal, and a significant decrease in serum titer of STA test led us to proceed with the second stage of surgery including removal of spacer and insertion of final prosthesis [Figure 2]. We continued antibiotic therapy for 6 months following the second stage. At the latest follow up, which took place 36 months after reimplantation, the patient did not show symptoms and his knee function was excellent. All serum markers including brucella STA test were in the normal range and latest radiographs revealed no abnormality.
Figure 1.
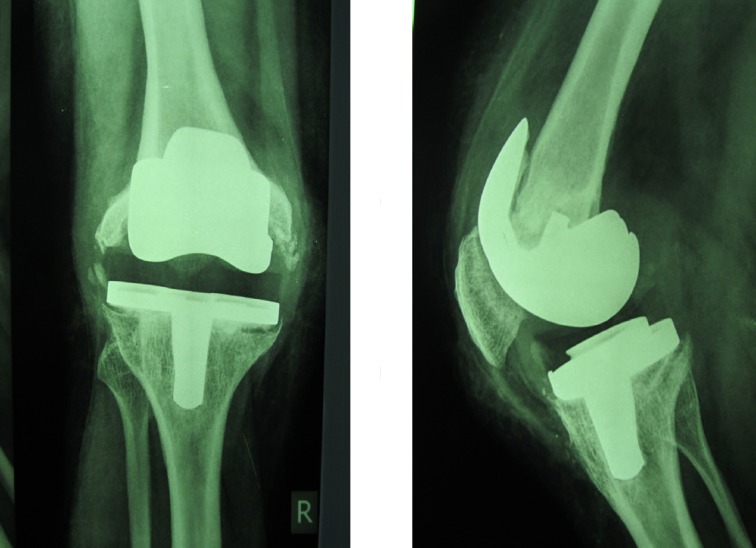
AP and Lateral X ray of knee after long term antibiotic therapy showed loosening of both components.
Figure 2.
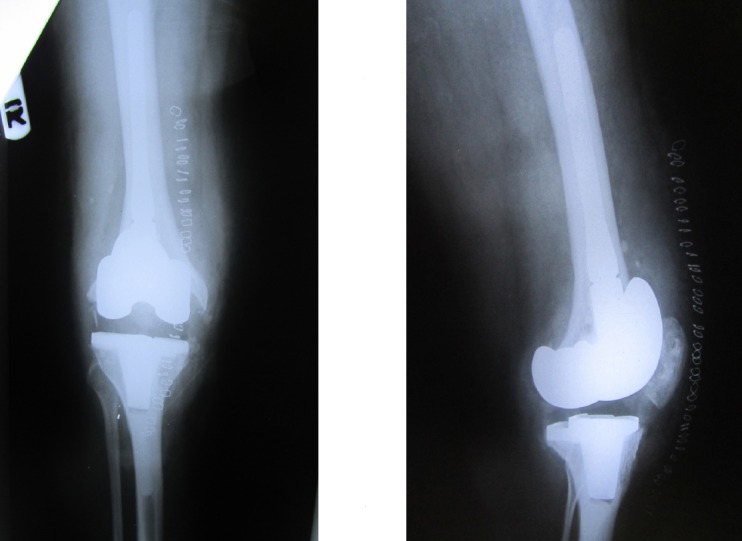
Ap and Latera x-ray following second stage.
Molecular Procedure Sample Processing for PCR
Genomic DNA was extracted from peripheral blood samples, included whole blood and serum carried out by commercial DNA extraction kit (BIONEER Co, Korea). When referring to literature several pairs of primers have been described for the detection of Brucella DNA by PCR (14, 15). However, we have used the primers B4 (5’-TGGCTCGGTTGCCAATATCAA-3’) and B5 (5’- CGCGCTTGCCTTTCAGGTCTG-3’) to amplify a target sequence of 223-bp within a gene code to produce a 31-kDa outer membrane protein specific, which is conserved in all Brucella species (16, 17). The composition of the 10X buffer contained 100 mM Tris-HCl pH 8.4, 1.5 mM MgCl2, 50 mM KCl. PCR was performed in 25 μl solutions containing 100 ng of genomic DNA, 1X PCR buffer, 200 μM each deoxyribonucleotide triphosphate (dATP, dGTP, dTTP, dCTP, Fermentas Co), 10 pmol of each primer and 0.5 U of Taq DNA polymerase (Fermentas Co.). Reactions were carried out in a thermal cycler (Eppendorf™ Mastercycler™) as follows: 95°C for 5 min, 35 cycles (94°C for 1 min, 55°C for 1 min, and 72°C for 30 s) and 72°C for 7 min. Finally, the products were analyzed (15 μl from each reaction mixture) using agarose gel (1.5%) electrophoresis at 80 V for 50 min stained with EtBr and photographed on a UV Transilluminator.
Discussion
Brucellosis is a zoonosis disease caused by small, gram-negative Coccobacilli. Mediterranean and Middle Eastern countries such as Saudia Arabia, Syria and Iran are considered to have a very high rate of incidence, despite control interventions (7, 17, 18). In 2008, 17,905 cases (25 cases per 100,000) of brucellosis were identified in Iran (16). Routes of transmission from animal to human include direct contact with infected animals or their secretions through cuts or abrasions in the skin or conjunctival sac, inhalation of contaminated aerosols and ingestion of unpasteurized dairy products (6, 18). The symptoms of brucellosis are nonspecific (e.g., fever, sweats, malaise, anorexia, headache, back pain) (6, 17). Osteoarticular disease is universally the most common complication of brucellosis (7, 8).
Arthritis is one of the common manifestations of brucellosis. Two mechanisms of joint involvement have been described, a septic process leading to destructive changes and a reactive arthritis. The most common mechanism of joint involvement is reactive arthritis. The septic form develops via invasion of the joint by Brucella spp. circulating in blood, as in other bacterial arthritis (8).
Over the past years, there has been a significant increase in the number of joint replacements worldwide (1). Infection is the most serious complication of total joint replacement and it is one of the leading causes of revision TKA. Therefore, it is important to consider PJI in the differential diagnosis of painful TKA. However, PJI due to Brucella species is extremely rare (10). To our best of knowledge, there are only 7 cases of PJI after TKA in the English language literature [Table 1]. In addition, we are not aware of any previous PJI due to Brucella species in patients with hemophilia. We think that clinicians should consider Brucellosis as a cause of PJI at least in endemic area for this infection.
Table 1.
Previous reports on Total Knee Arthroplasty infection by Brucella. Please note that none of them happened in patients with hemophilia
| Study | Age (year) | Time between arthroplasty to infection | Joint | Management |
|---|---|---|---|---|
| Agarwal et al (18) | 24 | 2 months | Knee | Medical therapy |
| Malizos et al (19) | 74 | 4 months | Knee | Medical therapy |
| Orti et al (20) | 60 | 14 months | Knee | Medical therapy |
| Weil et al (16) | 61 | 2.5 years | Knee | Two stage revision arthroplasty |
| Weil et al (16) | 67 | 14 years | Knee | Two stage revision arthroplasty |
| Tassinari et al (21) | 68 | NA | Knee | Medical therapy |
| Emel Sesli et al (13) | 72 | 4 years | Knee | Arthroscopic lavage and debridement |
| Sazegari et al (14) | 78 | 5 years | Knee | Medical therapy |
| Current case | 28 | 3.5 years | Knee | Relapse despite medical therapy then perform double stage revision arthroplasty |
The main goals in the treatment of PJI are infection eradication, prevent its recurrence and preserve mechanical joint function (19). However, there are many controversies on how to achieve these goals. Recently, there was an international consensus meeting in Philadelphia on PJI, in which experts from around the world tried to answer the questions with regard to PJI based on the current evidence and their experience (20, 21). In that consensus, they considered irrigation and debridement for those cases that have stable prosthesis, less than 3 weeks of infection and good soft tissue coverage. In our case, despite eighteen months of conservative treatment with antibiotic combination therapy, we had no good clinical response and prosthetic loosening occurred. This reiterates that surgical irrigation and debridement should be part of treatment early in the disease. We performed two-stage revision TKA and after eighteen months of follow up, no clinical relapse occurred. Although there is a relative consensus on approaches to frequent etiologic agents such as staphylococci, the management of Brucella prosthetic joint infection is not standardized and there is no consensus because of the lack of data in large scale, randomized, controlled trials and the rare occurrence (13). Modalities of treatment depend on loosening, chronicity and other factors. It is divided in to antibiotic administration, with or without surgery. Surgical intervention included irrigation and debridement with prosthesis retention or prosthesis removal. Prosthetic replacement can be performed in one stage or two stages (9, 11, 13).
In conclusion, Brucella infection of total joint prosthesis should be considered in patients with hemophilia and joint replacement who are living in endemic area for brucellosis and have pain or swelling in the index joint. Based on the latest consensus, surgical intervention such irrigation and debridement in early stage of disease (first 3 weeks) and one- or two-stage exchange in chronic cases should be part of a treatment.
Acknowledgment
The authors stated that they had no interests that might be perceived as posing a conflict or bias for this paper.
References
- 1.Cataldo MA, Petrosillo N, Cipriani M, Cauda R, Tacconelli E. Prosthetic joint infection: recent developments in diagnosis and management. J Infect. 2010;61(6):443–8. doi: 10.1016/j.jinf.2010.09.033. [DOI] [PubMed] [Google Scholar]
- 2.Tahmasebi MN, Bashti K, Ghorbani G, Sobhan MR. Intraarticular administration of tranexamic acid following total knee arthroplasty: a case-control study. Arch Bone Jt Surg. 2014;2(3):141–5. [PMC free article] [PubMed] [Google Scholar]
- 3.Powell DL, Whitener CJ, Dye CE, Ballard JO, Shaffer ML, Eyster ME. Knee and hip arthroplasty infection rates in persons with haemophilia: a 27 year single center experience during the HIV epidemic. Haemophilia. 2005;11(3):233–9. doi: 10.1111/j.1365-2516.2005.01081.x. [DOI] [PubMed] [Google Scholar]
- 4.Cerit ET, Aydin M, Azap A. A case of brucellar monoarthritis and review of the literature. Rheumatol Int. 2012;32(5):1465–8. doi: 10.1007/s00296-011-1917-8. [DOI] [PubMed] [Google Scholar]
- 5.Stiehl JB, Sterkin LA, Brummitt CF. Acute pasteurella multocida in total knee arthroplasty. J Arthroplasty. 2004;19(2):244–7. doi: 10.1016/j.arth.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 6.Andriopoulos P, Tsironi M, Deftereos S, Aessopos A, Assimakopoulos G. Acute brucellosis: presentation, diagnosis, and treatment of 144 cases. Int J Infect Dis. 2007;11(1):52–7. doi: 10.1016/j.ijid.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 7.Hashemi SH, Keramat F, Ranjbar M, Mamani M, Farzam A, Jamal-Omidi S. Osteoarticular complications of brucellosis in Hamedan, an endemic area in the west of Iran. Int J Infect Dis. 2007;11(6):496–500. doi: 10.1016/j.ijid.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 8.Turan H, Serefhanoglu K, Karadeli E, Timurkaynak F, Arslan H. A case of brucellosis with abscess of the iliacus muscle, olecranon bursitis, and sacroiliitis. Int J Infect Dis. 2009;13(6):e485–7. doi: 10.1016/j.ijid.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Tena D, Romanillos O, Rodriguez-Zapata M, de la Torre B, Perez-Pomata MT, Viana R, et al. Prosthetic hip infection due to Brucella melitensis: case report and literature review. Diagn Microbiol Infect Dis. 2007;58(4):481–5. doi: 10.1016/j.diagmicrobio.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 10.Agarwal S, Kadhi SK, Rooney RJ. Brucellosis complicating bilateral total knee arthroplasty. Clin Orthop Relat Res. 1991;267(1):179–81. [PubMed] [Google Scholar]
- 11.Dauty M, Dubois C, Coisy M. Bilateral knee arthroplasty infection due to Brucella melitensis: a rare pathology?Joint Bone Spine. 2009; 76(2):215–6. doi: 10.1016/j.jbspin.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 12.Orti A, Roig P, Alcala R, Navarro V, Salavert M, Martin C, et al. Brucellar prosthetic arthritis in a total knee replacement. Eur J Clin Microbiol Infect Dis. 1997;16(11):843–5. doi: 10.1007/BF01700416. [DOI] [PubMed] [Google Scholar]
- 13.Weil Y, Mattan Y, Liebergall M, Rahav G. Brucella prosthetic joint infection: a report of 3 cases and a review of the literature. Clin Infect Dis. 2003;36(7):e81–6. doi: 10.1086/368084. [DOI] [PubMed] [Google Scholar]
- 14.Sazegari MA, Bahramian F, Mirzaee F, Zafarani Z, Aslani H. Loosening of Total Knee Arthroplasty after Brucellosis Infection: A Case Report. Arch Bone Jt Surg. 2017;5(1):70–72. [PMC free article] [PubMed] [Google Scholar]
- 15.Baily GG, Krahn JB, Drasar BS, Stoker NG. Detection of Brucella melitensis and Brucella abortus by DNA amplification. J Trop Med Hyg. 1992;95(4):271–5. [PubMed] [Google Scholar]
- 16.Navarro E, Casao MA, Solera J. Diagnosis of human brucellosis using PCR. Expert Rev Mol Diagn. 2004;4(1):115–23. doi: 10.1586/14737159.4.1.115. [DOI] [PubMed] [Google Scholar]
- 17.McGill PE. Geographically specific infections and arthritis, including rheumatic syndromes associated with certain fungi and parasites, Brucella species and Mycobacterium leprae. Best Pract Res Clin Rheumatol. 2003;17(2):289–307. doi: 10.1016/s1521-6942(02)00127-4. [DOI] [PubMed] [Google Scholar]
- 18.Zamani A, Kooraki S, Mohazab RA, Zamani N, Matloob R, Hayatbakhsh MR, et al. Epidemiological and clinical features of Brucella arthritis in 24 children. Ann Saudi Med. 2011;31(3):270–3. doi: 10.4103/0256-4947.81543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jamsen E, Varonen M, Huhtala H, Lehto MU, Lumio J, Konttinen YT, et al. Incidence of prosthetic joint infections after primary knee arthroplasty. J Arthroplasty. 2010;25(1):87–92. doi: 10.1016/j.arth.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 20.Haasper C, Buttaro M, Hozack W, Aboltins CA, Borens O, Callaghan JJ, et al. Irrigation and debridement. J Arthroplasty. 2014;29(2 Suppl):100–3. doi: 10.1016/j.arth.2013.09.043. [DOI] [PubMed] [Google Scholar]
- 21.Haasper C, Buttaro M, Hozack W, Aboltins CA, Borens O, Callaghan JJ, et al. Irrigation and debridement. J Orthop Res. 2014;32(Suppl 1):S130–5. doi: 10.1002/jor.22556. [DOI] [PubMed] [Google Scholar]


