Abstract
Adenocarcinoma of the rete testis is a rare and aggressive malignancy arising from the epididymal epithelium. We present a case of a 66-year-old male who presented with left testis mass. Histopathological analysis of orchiectomy specimen was consistent with adenocarcinoma of the rete testis. Subsequent retroperitoneal lymph node dissection revealed metastatic disease not detected on preoperative PET-CT. Prior reports have suggested poor response rates to both systemic chemotherapy and radiation therapy. Aggressive surgical management of the retroperitoneum should be considered even in clinically node-negative patients given the paucity of other effective treatment regimens.
Keywords: Rete testis, Retroperitoneal lymph node dissection, Adenocarcinoma
1. Introduction
Adenocarcinoma of the rete testis is a rare testicular tumor with approximately 80 cases reported in the literature. Previous work demonstrated a poor prognosis with 3- and 5-year disease free survival of 49% and 13%, respectively.1 Systemic treatments have demonstrated poor response rates. Staging retroperitoneal lymph node dissection (RPLND) has been recommended by some due to the risk of occult metastases at presentation.2 We present the case of a patient with adenocarcinoma of the rete testis found to have micrometastatic disease on RPLND despite clinically negative preoperative imaging studies including Positron Emission Tomography-Computed Tomography (PET-CT). Based on this experience and existing literature, aggressive surgical management of this disease should be considered in appropriate candidates.
1.1. Case report
A 66-year-old healthy male presented with six months of progressive dull ache in the left hemiscrotum with associated mass. Exam revealed a firm testicular mass that replaced the lower pole. Ultrasound revealed a 3.8cm heterogenous mass. Tumor markers were normal.
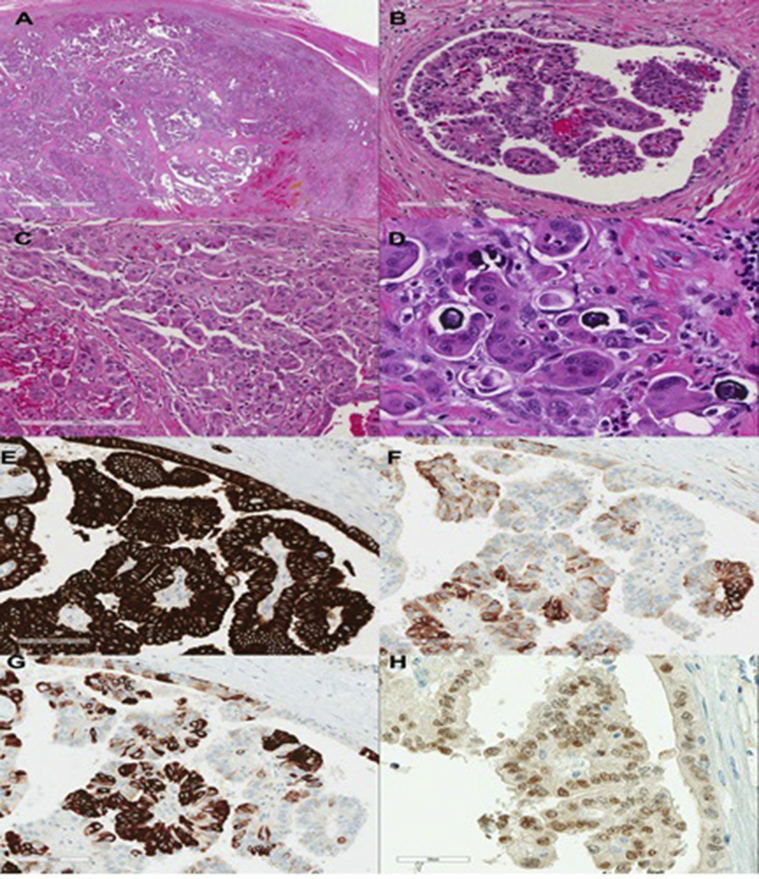
The patient underwent radical orchiectomy. Histological examination revealed replacement of the epididymal tissue with an adenocarcinoma (Fig. 1). Given the rarity of this tumor, extensive immunohistochemical staining was performed. Cells stained diffusely positive for EMA, CD10, vimentin, and had patchy staining for p53, CK20, and CK7. Pax8, which has been reported to be positive in non-neoplastic rete testis, stained positive within the neoplastic cells.3 Markers commonly positive in primary germ cell and stromal testicular tumors were negative in these cells. Cross-sectional imaging did not identify a primary site to suggest metastatic disease, and therefore a diagnosis of adenocarcinoma of the rete testis was made.
Fig. 1.
The neoplasm, which was entirely submitted for histologic examination, demonstrated a variable growth pattern (Fig. 1A), with the predominant growth pattern being tubulopapillary with glomeruloid structures (Fig. 1B) although areas with a more glandular appearance and psammoma bodies were also present (Fig. 1C and D). Perineural invasion and lymphatic but not vascular invasion was identified. Immunohistochemical studies for keratins revealed the neoplastic cells to demonstrate strong diffuse cytoplasmic staining for pancytokeratin (Fig. 1E) and Cam 5.2 while being negative for cytokeratin 903 (CK34βE12). Stains for CK7 and CK20 demonstrated patchy strong cytoplasmic staining, with these antibodies appearing to recognize different subpopulations of neoplastic cells (Fig. 1F and G). A pax8 stain, which is reportedly positive in non-neoplastic rete testes, demonstrated patchy moderate staining of the neoplastic nuclei (Fig. 1H). Molecular studies using Therascreen KRAS and EGFR RGQ PCR kits (Qiagen) failed to reveal commonly encountered mutations in the KRAS and EGFR genes respectively.
Following orchiectomy, PET-CT did not reveal any lesions suspicious for metastasis. After thorough counseling, the patient elected to undergo bilateral full template RPLND for definitive nodal staging as well as potential therapeutic benefit. Pathology revealed metastatic adenocarcinoma in 4 of 16 para-aortic lymph nodes. The patient declined adjuvant chemotherapy. There was no clinical evidence of recurrence at two month follow-up.
2. Discussion
Primary adenocarcinoma of the rete testes is a rare and fatal malignancy. Its etiology has not been elucidated. Due to their rarity, the diagnostic and immunohistochemical characteristics of primary carcinomas of the rete testes have not been firmly established, making it a diagnosis of exclusion. As reviewed by Amin, useful features for making the diagnosis of a primary carcinoma of the rete testes include a) neoplasm centered in the hilum of the testes, b) microscopic morphology incompatible with other testicular/paratesticular neoplasms, c) absence of histologically similar extra-scrotal primary neoplasms, d) immunohistochemial exclusion of other possibilities, most notably malignant mesothelioma and papillary serous carcinoma.4
This case met the above criteria. Immunohistochemical stains for antigens that are frequently positive in more commonly encountered primary testicular germ cell and sex cord-stromal tumors (CD117, SAL4, OCT4, PLAP, AFP, GATA3, CD30, glypican 3, HCG-β, and α-inhibin) were negative in the neoplastic cells. Malignant mesothelioma may have a similar morphologic appearance. The neoplastic cells in this case lacked immunoreactivity with D2-40 and WT-1 while being positive for Ber-Ep4, EMA, and monoclonal CEA, arguing against the diagnosis of malignant mesothelioma. Within the differential diagnosis, in light of the pax8 positivity, are ovarian-type epithelial tumors and a renal primary; however these were ruled out by further immunohistochemical staining. TTF1, CDX2, and prostate specific antigen, markers that are commonly positive in adenocarcinomas of lung, lower gastrointestinal, and prostate respectively, were negative.
Upon clinical evaluation, ultrasound may reveal a hypoechoic mass with poorly defined borders and increased vascularization. Abdominal imaging modalities may be useful in detecting metastasis. A report by Musser and colleagues illustrated a potential benefit of PET-CT.5 In their report, conventional CT did not reveal enlarged lymph nodes until 10 months after PET-CT showed hypermetabolic nodes. PET-CT was normal in our patient.
Optimal treatment following orchiectomy is unclear, as the rarity of this tumor has precluded comparative trials between treatment modalities. Chemotherapy and radiation therapy have been utilized, however have shown poor performance in both localized and metastatic disease.1 Methotrexate and 5-flurouracil have been attempted as have combination therapies with carboplatin and cisplatin, and have demonstrated only minimal response. A recently published case using paclitaxel, ifosfamide, and cisplatin reported a 14 month remission after metastasis, suggesting a chemotherapeutic alternative.2 Radiotherapy has been primarily used in palliative settings.1
Sanchez and colleagues1 performed a meta-analysis of 40 previous cases and found that patients in whom RPLND was performed (7 cases) had higher 3-year overall survival in bivariate analysis than those in whom it was not (83% vs 42%, log rank P = 0.03). In contrast, patients who received systemic chemotherapy after orchiectomy had similar 3-year overall survival to those who did not (60% vs 44%, log rank P = 0.3). No patient receiving adjuvant radiotherapy lived for 3 years. These findings are likely influenced by a selection bias, with surgical treatment likely only offered to patients with lower disease burden. On multivariable Cox regression, only primary tumor size <5 cm was an independent predictor of overall survival.
Our patient was offered RPLND for accurate staging and for potential therapeutic benefit given the reported poor response rates to systemic therapy. Despite a normal PET-CT, 4 positive nodes were found in the para-aortic region, the primary landing zone for left-sided testicular tumors. This finding underscores the aggressive biology of this disease, and calls into question the clinical applicability of PET-CT for detecting metastasis as suggested by Musser.5 Upfront RPLND should be considered in these patients for the identification and treatment of micrometastatic disease while disease burden remains resectable.
3. Conclusion
Adenocarcinoma of the rete testis is a rare tumor that is difficult to diagnose and treat. Reported response rates to systemic therapy are poor and until more effective regimens are described, RPLND should be considered even in patients with clinically negative retroperitoneal lymph nodes on standard imaging modalities.
Conflicts of interest
All authors have no conflict of interest to report.
References
- 1.Sanchez-Chapado M., Angulo J.C., Haas G.P. Adenocarcinoma of the rete testis. Urology. 1995;46:468–475. doi: 10.1016/S0090-4295(99)80257-X. [DOI] [PubMed] [Google Scholar]
- 2.Chovanec M. Adenocarcinoma of the rete testis - A rare case of testicular malignancy. Klin Onkol Cas Ceske a Slov Onkol Spolecnosti. 2014;27:136–137. doi: 10.14735/amko2014136. [DOI] [PubMed] [Google Scholar]
- 3.Tong G.X. PAX8 and PAX2 immunostaining facilitates the diagnosis of primary epithelial neoplasms of the male genital tract. Am J Surg Pathol. 2011;35:1473–1483. doi: 10.1097/PAS.0b013e318227e2ee. [DOI] [PubMed] [Google Scholar]
- 4.Amin M.B. Selected other problematic testicular and paratesticular lesions: rete testis neoplasms and pseudotumors, mesothelial lesions and secondary tumors. Mod Pathol Off J U. S Can Acad Pathol Inc. 2005;18(Suppl 2):S131–S145. doi: 10.1038/modpathol.3800314. [DOI] [PubMed] [Google Scholar]
- 5.Musser J.E., Ernest A.J., Thibault G.P., McMann L.P. Primary adenocarcinoma of the rete testis: improved staging accuracy with CT-PET. Urology. 2011;77:334. doi: 10.1016/j.urology.2010.02.035. [DOI] [PubMed] [Google Scholar]