Abstract
Introduction. Neovascular glaucoma (NVG), participates in the group of secondary glaucoma causing the increase of intraocular pressure (IOP) as a result of iridocorneal angle enclosure with the development of neovase derived from the retinal ischemic and other inflamatory diseases.
Purpose of the study. Is to show the incidence, etiopathogenesis, clinical development and the management of NVG by comparing the contemporary and referring literature to other clinics.
Methods. In this study there were presented the results of NVG treatment for the 2010-2014 interval. The data processing were conducted using statistically package SPSS 22. Results. In this scientific study were included 61 patients with NVG containing 4.3% of all cases with glaucoma and 14% of cases with secondary glaucoma, aged 22-79. The mean age of the patients was 60.9 year (SD + 10.6 year), 39 cases or 63.9% were of masculine gender and 22 cases or 36.1% of feminine gender, as it seems there is a differentiation with a statistical significance (X2=4.74, P=0.03, therefore P˂0.05). The most frequent cause of NVG was PDR in 55 cases or 55.6% of them, then, ischemic CRVO with 11 cases or 11.1%. The most frequent complications to the NVG were hemophthalmos, cataract and absolute glaucoma.
Conclusion. In many aspects our results were in line with the results of other authors. Therefore we should focus on the adequate treatment of ocular ischemic in time, as it is only prevention method of NVG.
Keywords: Diabetic retinopathy, retina ischemy, neovascular glaucoma
Introduction
Neovascular glaucoma (NVG) is an eye disease not commonly encountered, but it is a serious disease, as it appears as a result of iris and iridocorneal neovascularization, increased intraocular pressure - IOP, thus causing irreversible sensorineural damage [1]. It takes part in the secondary glaucoma discovered in 1871 [2]. NVG is a consequence of retinal ischemia, resulting from the genetic, inflammatory disease, traumatological, endocrinological, and intraocular tumors complications, all these mentioned complications having a main role in the appearance of new vessels etc. The most frequent diseases causing the NVG are: diabetic retinopathy - DR, central retinal vein occlusion - CRVO and systematically inflammatory diseases. [3]. Seldom, glaucoma appears after CRVO, idiopathic retinal periphlebitis - Eales disease, trauma, intraocular tumors, coats syndrome, uveitis, endoftalmite, retinal ablation. Pathogenesis at the NVG retinal ischemia having a main role-capable of causing neovascularization [4]. The positive diagnosis can be determined by biomicroscopic, ophthalmoscopic and gonioscopic examination. The angio-fluorographic examination of the anterior segment can identify in iris and irido-corneal angle neovascularization from its beginning especially when biomicroscopic examination is difficult [5]. Complicated cases of NVG, where the intraocular mediums are less transparent, the treatment effectiveness though the pan-retinal cryo-therapy (PRC) is useful. The filtration surgery is mandatory in these cases through the silicon valvula or with supramid as well as mitomycin - C (MMC) and 5-fluorouracil (5-FU) administration. [6]. Medication treatment: the most important drugs in this stage include the following: cycloplegics like atropine 1%, anti-inflammatory steroids like prednisolone e.g. Pred Forte, Inflamase Forte for lowering the inflammation. The miotics, e.g. sol. Pilocarpine is contraindicated because it may increase inflammation. Existing anti glaucoma drugs to manage the IOP are: beta-blockers, carbonic anhydrase inhibitors, prostaglandins [7]. Timely treatment of proliferative diabetic retinopathy with Pan-retinal photocoagulation (PRP) and Anti-vascular endothelial growth factor (AVEGF) may prevent successfully NVG and its heavy consequences [8, 9, 10]
Purpose of the study
The purpose of the study is to indicate the incidence of NVG according to age and gender, researching and analyzing the incidence of NVG in cases with diabetic retinopathy where only Partial retinal photocoagulation (P- RP) as well as in cases where is applied PRP together with application of therapy with Anti-VEGF intravitreal injection (e.g. Avastin). On the other hand, this study indicates the frequency of diseases with probability of other associated diseases and complications.
Material and methods
One of retrospective, being conducted between 2010 and 2014 at the HSCUK (Hospital Services and Clinical University of Kosovo), Ophthalmological Department, especially at the eyes wards of Regional Hospital in Gjilan. In this study, 61 patients or 99 eyes, aged between 22 and 79 with NVG were included. The mean age was 60.9 (DS± 10.6 year; SEM ± 1.4 years). The female patients had the newest mean age 58.8 years while the male patients were of aged 62.1%, by the Man-Whitney test we did not get statistically significant differentiations of the mean age according to gender (U=445, P=0.815, well P>0.05).
Results
During this time period 1403 cases with glaucoma have been treated, 66 or 4.7% having congenital glaucoma, 902 or 64.4% primary glaucoma and 435 or 30.9% secondary glaucoma. 61 cases with NVG or 4.3% of all cases with glaucoma and 14.0% of cases with secondary glaucoma were treated in this study (Table 1).
Table 1.
Cases treated with glaucoma from 2010-2014
| Types of glaucoma | Glaucoma all cases | Secondary glaucoma | ||
|---|---|---|---|---|
| N | % | % | ||
| Congenital | Total congenital | 66 | 4.7 | |
| Primary | Glaucoma simplex | 357 | 25.5 | |
| Glaucoma pigmentosa | 18 | 1.3 | ||
| Glaucoma capsularis | 242 | 17.3 | ||
| Glaucoma angularis ac. | 123 | 8.8 | ||
| Glaucoma angularis chr. | 162 | 11.6 | ||
| Primary glaucoma | 902 | 64.4 | ||
| Secondary | Glaucoma secundum ac. | 126 | 9.0 | 29.1 |
| Glaucoma secundum chr. | 171 | 12.2 | 39.5 | |
| Absolute glaucoma | 77 | 5.5 | 17.9 | |
| Neovascular glaucoma | 61 | 4.3 | 14.0 | |
| Secondary glaucoma | 435 | 30.9 | 100.0 | |
| In total | 1403 | 100.0 |
Discussion
In the time span 2010-2014, 61 cases with NVG, including 4.3% of the cases were with glaucoma, and 14% with secondary glaucoma (Table 1). In our research with NVG, 39 or 63.9% were of male gender and 22 or 36.1% of female gender, noticing statistically significant differentiations (X=4.74, P=00.3, well P>0.05) being in line with the research of other authors. According to age, the NVG is mainly a disease of old people, though, it does not exclude the young people. The youngest patient was aged 22 and the oldest was aged 79, (Table 2).
Table 2.
Cases of NVG treated by age-group and gender
| Gender | |||||||
|---|---|---|---|---|---|---|---|
| F | M | In total | |||||
| Age-group | N | % | N | % | N | % | |
| <40 | 3 | 13.6 | 1 | 2.6 | 4 | 6.6 | |
| 40-59 | 6 | 27.3 | 9 | 23.1 | 15 | 24.6 | |
| 60+ | 13 | 59.1 | 29 | 74.4 | 42 | 68.9 | |
| Total | N | 22 | 100.0 | 39 | 100.0 | 61 | 100.0 |
| % | 36.1 | - | 63.9 | - | 100.0 | - |
Primary disease: the most frequent primary disease associated with NVG was proliferative diabetic retinopathy PDR in 55 cases or 55.6% of them, then CRVO in 11 cases or 11.1% of them and uveitis recidivans in 8 cases or 8.1%, (Graphic 1).
Graphic 1.
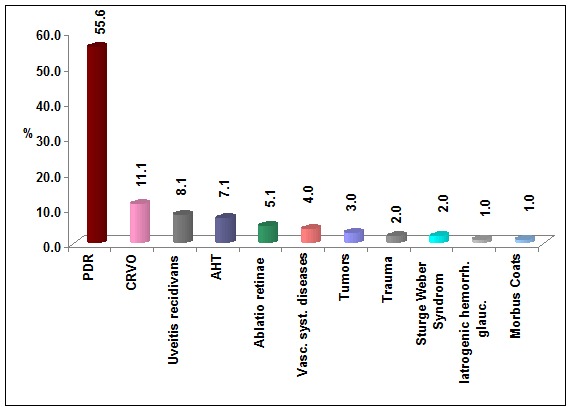
The range of primary disease in patients with NVG
Associated diseases: in the group of patients with NVG comprised in the research from 99 examined eyes, 9 or 9.1% have been associated with refraction anomaly as well as 7 or 7.1% with other glaucoma and so on (Graphic 2). Complications: the most frequent complications associated with NVG were hemophthalmos in 20 eyes or 20.2% of cases, then cataract in 15 cases or 15.2% as well as absolute glaucoma in 11 cases or 11.1% (Graphic 3).
Graphic 2.
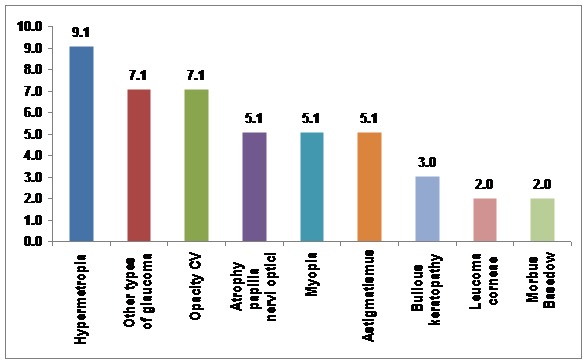
Associated disease in patients with NVG
Graphic 3.
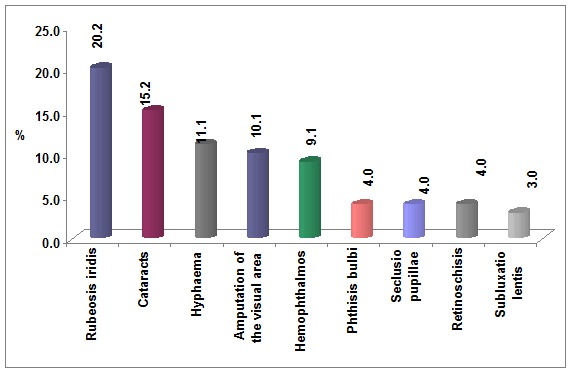
The structure of complications in patients with NVG
Treatment with surgical therapy: 95 eyes or 96% of the patients have been cured. The most frequent method was cryotherapy with 20% stabilization and 8% improvement. The therapy with AVGF, the treatment with AVGF in cases comprised in the research: the most frequent was the therapy with Bevacizumab (avastin) up to 69.7%, then Ranibizumab with 16.2%. Pegaptanib sodium with 9.1% and 5FI- Uracil with 5.1%, without differentiations depending on the eyes (Table 3). For the treatment of NVG For the treatment of NVG, concerning lowering the level of IOP (intraocular pressure) the following medical therapy has been used: betablocators, carbonic anhydrase inhibitors, prostaglandins eye drops, anti-inflammatory steroids, and cycloplegic, etc. The medical therapy in all cases was combined. The most frequent combination was sol. Timolol, sol. Lumigan, sol. Pred Forte and sol. Atropine sulphate with 48.5%, while in the second place comes therapeutic combination: sol. Lumigan, tab. Diamox, then sol. Pred Forte and sol Atropine sulphate with 31.3%. According to postoperative clinical discourse – POCD , following the treatment with PRP 27.3%, Pan-retinal cryo-therapy (PRC) 8.0% and Pars-plana vitrectomy (PPV) 57.9% we noticed the improvement of clinical state, taking into consideration connection between IOP, PNO and visual acuity, where we came to this correlation, X2 = 13.63; Df=4; P<0.01 (Graph. 4).
Table 3.
AVGF therapy in cases included in the research
| Eye with NVG | ||||||
|---|---|---|---|---|---|---|
| OD | OS | Total | ||||
| Th: with AVGF | N | % | N | % | N | % |
| Avastin ® (Bevacizumab) | 33 | 67.3 | 36 | 72.0 | 69 | 69.7 |
| Macugen ® (Pegaptanib sodium) | 5 | 10.2 | 4 | 8.0 | 9 | 9.1 |
| Lucentis ® (Ranibizumab) | 8 | 16.3 | 8 | 16.0 | 16 | 16.2 |
| 5 – FU ® (5-fluorouracil) | 3 | 6.1 | 2 | 4.0 | 5 | 5.1 |
| Total | 49 | 100.0 | 50 | 100.0 | 99 | 100.0 |
Graphic 4.
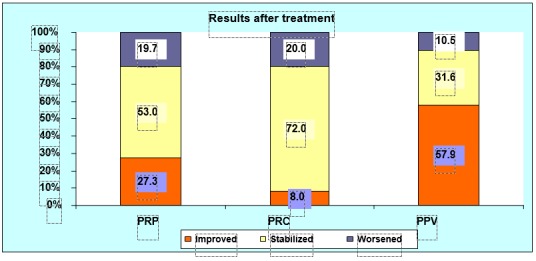
Scheme of the treatment results
Conclusion
According to our analysis results we came to these conclusions: NVG contains 4.3% of all cases with glaucoma and 14.0% of cases with secondary glaucoma. The most affected age by NVG is over 60 years, the mean age being 60.9 (SD±10.6 year; SEM±1.4 year). The most affected gender is the male one with 63.9% and 36.1% of female gender, with a statistically significant differentiation (X2=4.74, P=0.03 well P<0.05). The primary diseases that most frequently disease in cases there was not applied PRP and AVGF. The main complications in patients with NVG are: hemoftalmus, cataract, absolute and other glaucoma. It was proven that the most successful method in preventive and functional aspects of NVG is the therapy with PRP with application of AVGF. The prevention of NVG is the adequate and timely treatment of retinal ischemia.
References
- 1.Ajvazi H. Neovascular glaucoma treated in the Eye Clinic in Prishtina, Magistrature’s study. Faculty of Medicine at University of Prishtina /public presentation on. 2009 Mar 25;46:53. [Google Scholar]
- 2.Mocanu C, Barascu D, Marinescu F. Neovascular glaucoma-Retrospective study. Ophthalmologica. 2005;49:58–65. [PubMed] [Google Scholar]
- 3.Kim D, Singh A, Annapurna S. Neovascular Glaucoma. En: Shaarawy TM. Glaucoma Medical Diagnosis and Therapy I. Saint Louis (EEUU): Saunders Elsevier; 2009. pp. 409–417. [Google Scholar]
- 4.Ajvazi H, Goranci I, et al. Correlations of the changes between the iridocorneal angle and other parametres at the neovascular glaucoma: In the 7th Congress of SEEOS. GLAUCOMA SESSION - 035.20.June.2010, Tiranë. [Google Scholar]
- 5.Călugăru D, Călugăru M. Neovascular glaucoma--etipathogeny and diagnosis. Oftalmologia. 2012;56(2):3–14. [PubMed] [Google Scholar]
- 6.Ignjatović Z. Neovascular glaucoma. International Symposium on Glaucoma, under auspices: SEEOS and EGS - European Glaucoma Society. Belgrad: 2012. Apr 21, [Google Scholar]
- 7.Ajvazi H, Goranci I, Lutaj P. Management of neovascular glaucoma. Oftalmologia. 2013;57(4):39–43. [PubMed - indexet for MEDLINE] [PubMed] [Google Scholar]
- 8.Masaru I, et al. Management of neovascular glaucoma. Ophthalmology. 2014;9(1):33–42. [Google Scholar]
- 9.Ajvazi H, Lutaj P, Goranci I. Management of diabetic retinopathy, prevalence and clinical clasification. Oftalmologia. 2014;58(4):47–50. [PubMed] [Google Scholar]
- 10.Ajvazi H. Proliferative diabetic retinopathy-results of the microsurgical and laser treatment. Med Arh. 2010;64(3):165–167. PMID: 20645511 [PubMed - indexed for MEDLINE] [PubMed] [Google Scholar]


