Abstract
Synchysis scintillans is a vitreous condition in which multiple golden brown opacities are formed as a result of chronic vitreous hemorrhage. Anterior chamber synchysis scintillans was described in patients with afakia or lens subluxation.
We report a case of a 63-year-old man with a history of left eye trauma and complete loss of vision, who presented for left eye discomfort. The slit lamp examination revealed crystals of synchysis scintillans and rare inflammatory cells in the anterior chamber, stromal iris atrophy, circumferential posterior iris synechiae, and complete lens opacity. Total retinal detachment was observed on ocular ultrasonography. Intraocular pressure value was in normal range.
The distinctiveness of this case is the mechanism of vitreous crystals mobilization into the anterior chamber through an atrophic iris while intraocular pressure remains normal.
Keywords: synchysis scintillans, anterior chamber, eye trauma
Introduction
Synchysis scintillans is a result of chronic vitreous hemorrhage and is formed of multiple vitreous opacities that are flat, mobile, and golden brown in color [1]. The condition is also known as “cholesterolosis bulbi”, as the presence of cholesterol crystals was demonstrated in these opacities [2].
Synchysis scintillans is usually noted in the vitreous cavity, but there were reported cases of anterior chamber synchysis scintillans due to lens subluxation and anterior mobilization of the vitreous through the pupillary area [3, 4], although afakia or lens subluxation may not be required [5].
We report a case of anterior chamber synchysis scintillans with normal position of the lens and circumferential posterior iris synechiae.
Case report
A 63-year-old man presented to his family physician with complaints of discomfort in his left eye. The medical history revealed a blunt eye trauma during childhood with complete loss of vision in the left eye. The family physician noted an aspect “similar to hypopyon” and referred the patient to an eye care department.
The ophthalmological examination revealed best corrected visual acuity of 20/20 in the right eye and no light perception in the left eye. The slit lamp examination showed peripheral corneal opacities consistent with arcus senilis in both eyes. In the left eye there were also noticed mild conjunctival congestion, anterior chamber with mobile sparkling crystals with tendency to accumulate inferiorly and inflammatory cells 1+, stromal iris atrophy, fixed pupil, 360° posterior iris synechiae and complete lens opacity (Fig. 1).
Fig. 1.
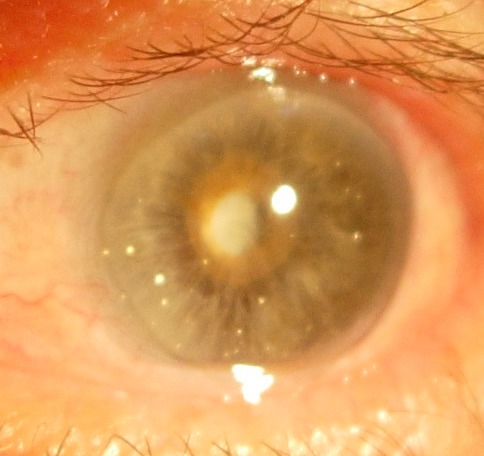
Left eye with synchysis scintillans in the anterior chamber.
The fundus exam was normal in the right eye and not visible in the left eye. Ocular ultrasonography revealed complete retinal detachment in the left eye. Intraocular pressure was 14 mmHg in the right eye and 18 mmHg in the left eye.
The patient was treated with topical fixed combination of tobramycin 0.3% - dexamethasone 0.1% q. i. d. for one week, with the remission of inflammatory cells. The patient underwent surgical intervention for the removal of the anterior chamber crystals, as these particles were considered to be the cause of ocular inflammation; bimanual irrigation/ aspiration probes were used. During the surgical intervention a large number of crystals were seen to migrate from posterior into the anterior chamber through the atrophic iris (Fig. 2), and were also aspired. The intraocular pressure decreased to 16 mmHg on postoperative day one, and intraocular pressure monitoring was recommended.
Fig. 2.
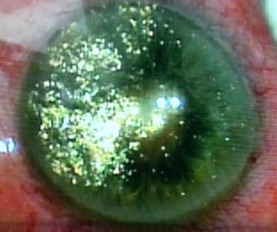
Intraoperative aspect of the left eye: vitreous crystals were aspired into the anterior chamber through the iris.
Discussion
The main feature responsible for the disease course in this case is the presence of the iris atrophy. The presence of the atrophy only in the left eye suggests its traumatic etiology [6]. The atrophic iris explains the absence of iris bombé although circumferential posterior iris synechiae were present. The atrophic iris created a way of communication between the anterior and posterior chambers. Functionally the left eye became a single compartment.
Most probably, the retinal detachment and lens opacity are consequences of the eye trauma the patient reported. The retinal detachment itself could cause the leakage of a cholesterol-rich fluid that contributed to the formation of synchysis scintillans in the absence of other vitreous hemorrhages [5]. The retinal detachment also prevents the ocular hypertension as the aqueous humor can be drained through the subretinal space.
The posterior iris synechiae might have been formed either in the context of eye trauma or during the inflammatory episode which appeared years later. However at the moment of examination the mechanism which allowed the vitreous particles to migrate into the anterior chamber was the filtering through the atrophic iris and not the passage through the pupillary area. The number and position of the crystals located in the anterior chamber varied with eye position and movements. If the patient was in orthostatism, the crystals had the tendency to form a pseudohypopyon; in dorsal decubitus the crystals were drained through the iris and disappeared from the anterior chamber. Eye movements determined the crystals to move.
Treatment options for anterior chamber synchysis scintillans are limited and address the underlying disease, or the symptoms. In this case the vision loss is irreversible and the patient would not benefit from cataract or retinal surgery because the retinal detachment is more than 40 years old. Periodical ophthalmologic examination is recommended in order to monitor the presence of ocular inflammation or increased intraocular pressure, and consequently prevent painful eye.
In conclusion, synchysis scintillans appears in damaged eyes and iris atrophy contributes to the anterior chamber mobilization of the vitreous crystals.
References
- 1.Sebag J. Vitreous Anatomy and Pathology. In: Ophthalmology, Yanoff M, Duker JS, editors. 4th ed. Elsevier Saunders; 2014. pp. 430–436. [Google Scholar]
- 2.Andrews JS, Lynn C, Scobey JW, Elliott JH. Cholesterosis bulbi. Case report with modern chemical identification of the ubiquitous crystals. Br J Ophthalmol. 1973;57(11):838–844. doi: 10.1136/bjo.57.11.838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park J, Lee H, Kim YK, Chae JD, Lee HJ. A Case of Cholesterosis Bulbi with Secondary Glaucoma Treated by Vitrectomy and Intravitreal Bevacizumab. Korean J Ophthalmol. 2011;25(5):362–365. doi: 10.3341/kjo.2011.25.5.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beebe J. Synchysis Scintillans and a Crystal Pseudohypopyion. EyeRounds Online Atlas of Ophthalmology. [cited May 2015]. Available from: http://webeye.ophth.uiowa.edu/eyeforum/atlas/pages/Synchysis-scintillans-crystal-pseudohypopion/index.htm. [Google Scholar]
- 5.Sanmugasunderam S, Giligson A, Choi SB. A “sparkling” eye. Can Med Assoc J. 2003;169(4):319. [PMC free article] [PubMed] [Google Scholar]
- 6.Edward DP. Degeneration and Atrophy of the Iris. In: Duane’s Ophthalmology on CD-ROM. Tasman W, Jaeger EA, editors. 2006. [Google Scholar]


