Abstract
Frequently, in literature and curent practice, accessory iris membrane (AIM) and persistant pupillary membrane (PPM) are confused. Both AIM and PPM are congenital iris anomalies in which fine or thick iris strands arrise form the collarette and obscure the pupil. AIM, which is also called iris duplication, closely resembles the normal iris tissue in color and thickness and presents a virtual second pseudopupil aperture in the centre while PPM even in its extreme forms presents as a translucent or opaque membranous structure that extends across the pupil and has no pseudopupil.
Mydriatiscs, laser treatment or surgery is used to clear the visual axis and optimize visual development. Surgical intervention is reserved for large, dense AIMs and PPMs.
Our patient, a 29 year old male, has come with bilateral dense AIM, bilateral compound hyperopic astigmatism, BCVA OD = 0.6, BCVA OS = 0.4, IOP OU = 17 mmHg. To improve the visual acuity of the patient we decided to do a bilateral membranectomy, restoring in this way transparency of the visual axis. After surgery, the visual acuity improved to BCVA OD= 0.8, BCVA OS=0.8.
Keywords: accessory iris membrane, membranectomy
Introduction
If 95% of newborns and 20% of adults have PPM (persistent pupillary membrane), few cases of AIM have been reported in literature [1]. Levy reported in 1957 a case of bilateral AIM associated with PMM, in 1998 Bhatti reported a case of bilateral AIM associated with microcornea while in 1979 Suh published a paper presenting 2 cases of AIM without other ocular anomaly associated [2] [3] [4].
Accessory iris membrane (AIM) represents a rare congenital ocular anomaly that appears as iris tissue strands arising from the iris collarette and going along the pupil, which closely resembles the normal iris tissue in color and thickness. It also presents a virtual second pseudopupil aperture in the centre with no muscular activity [2].
Persistent pupillary membrane (PPM) represents a common congenital ocular anomaly that appears as fine iris strands along the pupil, which are remnants of anterior tunica vasculosa lentis that supplies nutrition to the lens in the first six month of fetal life [5].
Frequently, in current practice, AIM is confused with extreme tick PPM [3]. It is true that these two conditions have similar origin but the clinical appearance is quite different. PPM even in its extreme forms presents as a translucent or opaque membranous structure that extends across the pupil and has no pseudopupil [2]. PPM can be unilateral or bilateral and can be quite variable in appearance, size, configuration and density while AIM seems to appear always bilateral.
Sometimes this kind of membranes can get attached to the anterior lens capsule creating a small cataract or to the posterior surface of the cornea [6] [7].
Histopathology examination shows that in cases of accessory iris membrane the tissue has an extensive anomalous hyperplasia even when compared with pupillary membrane at the stage in fetal life when it has reached its maximum development [8].
Since a pupillary diameter of only 1.5 mm is necessary for normal retinal image formation rarely this anomaly causes significant decrease in visual acuity but dens AIM can be associated with PPM, amblyopia, anterior polar cataract, coloboma, strabismus and anterior segment abnormalities [9] [10].
Treatment options of this kind of membranes include mydriatics, Nd:YAG laser therapy and surgical excision. If visual acuity is relatively good, a conservative management with mydriatics is recommended, this way preventing the risk of operative complications like traumatic cataract, anterior capsular lens rupture, pigment dispersion and hiphema.
Case report
We report the case of a 29 years old male patient with bilateral and dense AIM which presented to Laser Optisan Clinic from Cluj-Napoca in 2013 complaining of bilateral reduced visual acuity since birth. The patient was otherwise healthy. He had no family history of any ocular pathology and his parents were not consanguineous.
Examination showed: BCVA OD = 0.6, BCVA OS = 0.4 and IOP OU = 17 mmHg. The patient had a regular hyperopic astigmatism: OD +6.00 DSf –4.50Cyl /1610, OS +4.75 DSf –4.00 Cyl /180, OD: K1=38.50, K2=42.00, OS: K1=39.00, K2=42.00.
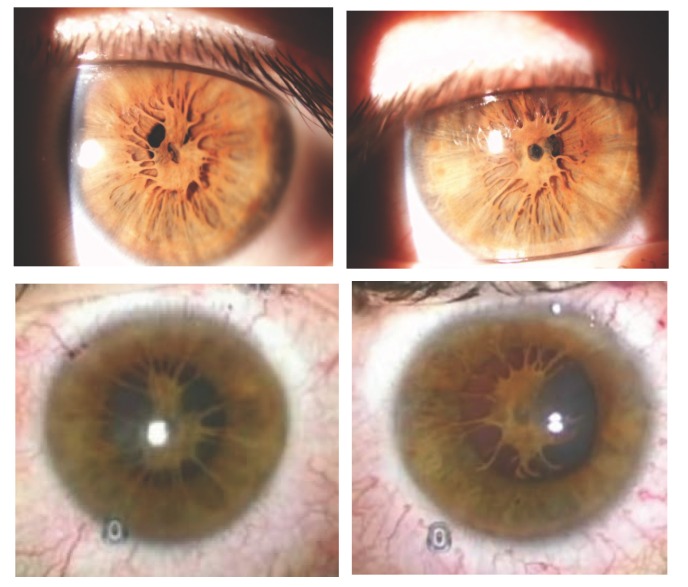
Extraocular muscle movements were normal in both eyes. Slit lamp examination revealed OU clear cornea, normally-reacting pupillary margin and iris, dens strands of tissue attached to the iris collarette along the pupil. In the center of this tissue was a 1 mm diameter pseudo-pupil.
Gonioscopy showed in both eyes a Shaffer grade III/IV angle with ciliary body band visible, normal structures and the angle was 36.20 OD and 37.10 OS. Ophthalmoscopy was impossible to do due to the dens AIM. Ocular echography was normal.
Differential diagnosis was done with:
• Persistent pupillary membrane (PPM) even in its extreme forms present as translucent or opaque membranous structure and extend across the pupil; also it doesn’t present with a pseudopupil [2];
• Posterior synechiae secondary to iridocyclitis is characterized by iris strands attach to the pupil margin while in AIM the iris strands arise from the iris collarette;
• Axenfeld–Rieger syndrome is associated with presence of microcornea or megalocornea, anterior displaced Schwalbe’s line (posterior embryotoxon) with attached iris strands, smooth and scriptless iris surface with high iris insertion, corectopia and ectropion uveae; also implies facial bone and teeth defects, hypospadias, redundant periumbilical skin [11];
• Peters anomaly involves posterior corneal defect with stromal opacification (leukoma) that may become vascularized, iris strands inserting into corneal defect, adhesions of lens to corneal defect [11];
• Iridocorneal endothelium syndrome (ICE) implies corneal edema, abnormal corneal endothelium and posterior synechiae with onset in young adults [1].
Fig. 1.
Anterior segment photographs of bilateral AIM obtained before surgery
Nd – Yag laser membranectomy was not an option in this case even if this technique has been successfully used in older patients with PMM. Although this approach is preferred because it avoids intraocular surgery, laser lysis is difficult in cases of thick membranes [12] [13]. Besides, because the membranes may have active vasculature, Nd – Yag laser membranectomy could lead to hyphema and pigment dispersion. [13] [14].
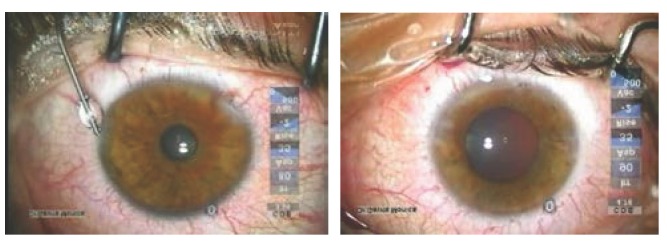
The patient underwent bilateral AIM membranectomy on a non-dilated pupil using lots of viscoelastics for endothelial protection and microincision surgery instruments to cut the strands at their origins and get the AIM out of the anterior chamber. We used 2 side-port incisions which at the end didn’t need suture. We didn’t encounter attachments to the anterior lens capsule. The patient had excellent outcome and no surgery complications were encountered.
Visual acuity improved to BCVA OD= 0.8, BCVA OS=0.8 which stands for a deprivation amblyopia. IOP OU was 15 mmHg. The refractive error remained the same: OD +6.00DSf –4.50Cyl /1610, OD +4.75DSf –4.00Cyl /180, OD: K1=38.50, K2=42.00, OS: K1=39.00, K2=42.00.
Slit lamp examination revealed: clear cornea, reactive, round and symmetric pupil, free anterior chamber, iris pigment on the anterior capsule, clear lens. Ophthalmoscopy showed a normal retina and optic nerve.
The patient gave his consent for the use of his data in this study.
Fig. 2.
Anterior segment photographs of bilateral AIM obtained during surgery
Conclusions
Membranectomy done under dispersive viscoelastic protection and with microincision instruments represents the right approach in dense AIM restoring this way transparency of the visual axis. The risk of developing traumatic iatrogenic cataract, if surgical instruments are not carefully manipulated, represents the most important surgery complication that can appear.
Even if AIM and PMM have the same origin and the same treatment, we must differentiate the two conditions and use the right nomenclature.
Disclosures: none
References
- 1.Tasman W, Jaeger E. Duane’s ophthalmology. 2007 Ed. Philadelphia: Lippincott Williams & Wilkins; 2007. pp. 24–258. [Google Scholar]
- 2.Bhatti S.M., Kapoor H.K. Bilateral accessory iris membrane. Indian Journal of Ophthalmology. 1998;46:110–111. [PubMed] [Google Scholar]
- 3.Levy W.J. Congenital iris lesion. British Journal of Ophthalmology. 1957;41:120–123. doi: 10.1136/bjo.41.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Suh D.H. 2 cases of accessory iris membrane. Journal of the Korean Ophthalmology Society. 1979;20(1):107–111. [Google Scholar]
- 5.Trattler W.B., Keiser P, Friedman N.J. Review of ophthalmology. 2nd Ed. Elsevier Inc; 2012. pp. 105–278. [Google Scholar]
- 6.Levin A.V., Wilson T.W. Hospital for Sick Children's - The Atlas of Pediatric Ophthalmology and Strabismus. 1st Ed. Lippincott Williams & Wilkins; 2007. p. 77. [Google Scholar]
- 7.Mukherjee P.K. Pediatric Ophtalmology. 1st Ed. New Delhi: New Age International (P) Ltd., Publishers; 2005. p. 235. [Google Scholar]
- 8.Duke-Elder S. System of Ophthalmology, Vol. 3. 1st Ed. London: Henry Kimpton; 1964. pp. 587–775. [Google Scholar]
- 9.Levy W.J. Congenital iris lesion. British Journal of Ophthalmology. 1957;41:120–123. doi: 10.1136/bjo.41.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller D, Johnson R. Quantification of the stenopeic effect. Survey of Ophthalmology. 1977;21:347–350. doi: 10.1016/0039-6257(77)90114-x. [DOI] [PubMed] [Google Scholar]
- 11.Strominger M. Pediatric Ophthalmology and Strabismus. 1st Ed. Elsevier Inc; 2008. p. 46. [Google Scholar]
- 12.Kumar H, Sakhuja N, Sachdev M.S. Hyperplastic pupillary membrane and laser therapy. Ophthalmic Surgery. 1994;25:189–190. [PubMed] [Google Scholar]
- 13.Gupta R, Kumar S, Sonika S.S. Laser and surgical management of hyperplastic persistent pupillary membrane. Ophthalmic Surgery. 2003;34:136–139. [PubMed] [Google Scholar]
- 14.Brusini P, Beltrame G. Spontaneous hyphaema from persistent remnant of the pupillary membrane: a case report. Acta Ophthalmologica (Copenhagen) 1983;61:1099–1103. doi: 10.1111/j.1755-3768.1983.tb01497.x. [DOI] [PubMed] [Google Scholar]