Abstract
Background:
Allergic rhinitis (AR) may be overdocumented in cases of dental caries because of controversies in the literature This study was conducted to investigate the potential relationship between AR and dental caries in children.
Materials and Methods:
A total of 296 children were included in this cross-sectional study. Participants were evaluated using the decay-missing-filled (DMF) index, and their AR status was evaluated by physical examination and through a standard questionnaire. Baseline demographics and clinical characteristics were compared among groups using Student's t-test or the Mann–Whitney U-test, the Chi-square test, and/or Fisher's exact test as appropriate. A level of P < 0.05 was regarded as statistically significant.
Results:
Evidence of AR was found in 77 (35.1%) participants. There was no significant difference in the rate of tooth decay or DMF between participants with or without AR (P = 0.07), but a significant difference was observed in the number of missing and filled teeth between those with and without AR (P < 0.05). There were no significant differences in educational level, family income, milk intake, use of pacifier, use of a toothbrush, saliva secretion, or body mass index (P > 0.05 in all cases) between AR-positive and AR-negative patients. Fluoride therapy and oral breathing were identified as confounding factors and controlled using log-linear analysis. The mean rate of DMF in patients who also had AR was 20% greater than in the AR-negative group (odds ratio [OR] = 1.21, confidence interval [CI]: 1.05–1.35) and 15% greater in among children who breathed orally than those who did not (OR = 1.15 CI: 1.02–1.31).
Conclusion:
AR and oral breathing may have an effect on oral health and dental condition, leading to an increased rate of tooth loss, oral fillings, and development of dental caries.
Keywords: Rhinitis Allergic, dental caries, dental filling, mouth breathing
INTRODUCTION
Allergic rhinitis (AR) is among the most frequent chronic respiratory diseases that occur in children. The prevalence of this disease seems to vary in different countries from 1.3%–52%[1] although it is greater in some countries.[2] The reasons for the high prevalence of AR have not yet been elucidated, but the hygiene hypothesis could provide one explanation.[3] This theory suggests that living in a hygienic environment with less microbial exposure increases the susceptibility of allergic diseases.[4,5,6,7,8,9] Persistent oral breathing and infectious oral tissues are complications that may occur as a result of the clinical progression of AR, and low salivary secretion could also result from AR treatment with antihistamine drugs.[1,10,11,12] All these complications are risk factors for dental caries.
Dental caries in childhood is still a major public health challenge in most industrialized and developing countries.[13]
The disease develops in both the crowns and roots of the teeth and can arise in early childhood as aggressive tooth decay that affects the primary teeth of infants and toddlers.[14] Individuals are susceptible to dental caries throughout their lifetime. Dental caries among Iranian children was reported in two national surveys conducted by the Iranian Ministry of Health and Medical Education.[15,16] The second of these national surveys, published in 2004, aimed to describe the oral health of children in the Islamic Republic of Iran and to provide baseline data for the organization as well as an evaluation of the national oral health promotion program. The World Health Organization (WHO) pathfinder-sampling procedures were used to select representative samples of children aged 3, 6, 9, and 12 years. Data on decayed-missing-filled (DMF) teeth, caries-free rates, and treatment needs were collected from 18,946 children using the WHO standard methodology. The mean decay-missing-filled primary teeth (dmft)/decay-missing-filled permanent teeth (DMFT) indices were 1.9/- for 3-year olds, 5.0/0.2 for 6-year olds, 3.6/0.9 for 9-year olds, and 0.6/1.9 for 12-year olds.[17] Significant differences in the prevalence of dental caries were found based on an analysis of gender, province, urban/rural residence, family income, and parents’ level of education. The development of dental caries by the concurrent action of three primary factors (tooth, dental plaque, and diet) can be presented using a 3-way Venn diagram, in which the three factors are all enclosed in a larger circle symbolizing time.[14] The entire system is affected by oral environmental factors, such as saliva, buffer capacity, composition, and fluoride.[18] The outer circle that surrounds all these considerations include personal factors such as education, oral health literacy, sociodemographic status, behavior, knowledge, and attitudes, and characteristics of the oral health services.[19,20]
There are few studies that show the relationship between periodontal disease or oral bacteria and allergic disease.[18,21,22] We hypothesize that AR may result in an increased risk of developing dental caries because of heightened oral breathing, poor oral hygiene, and mouth dryness. The aim of this study was to explore the possibility of a correlation between AR and dental carries.
MATERIALS AND METHODS
We conducted a cross-sectional, school-based study in 296 children from June 2011 to May 2012. The Ethics Committee of Mashhad University of Medical Sciences approved the study. The ages of the children were 5–7 years, and they were selected using a stratified random cluster sampling method. Mashhad is located in the Northeastern region of Iran and is subdivided into seven educational regions; schools were selected from each region at random. Physical examinations were performed by a physician and a dentist. The oral cavity was examined by a dentist to evaluate the palatine tonsil and also to determine DMF factor.[20] A diagnosis of AR was based on the physical examination and the standard International Study of Asthma and Allergies in Childhood questionnaire, a validated instrument for diagnosing AR.[23]
Other information, including the medical history of participants and demographic characteristics, were acquired from their parents using a questionnaire containing questions about age, gender, body mass index (BMI), education, familial economic status, nutritional background (breast feeding vs. dietary milk intake), hygiene habits (toothbrushing practices, usage of pacifier for more than 2 years, fluoride therapy), adenoid, and AR symptoms such as oral breathing and the extent of the saliva secretion. Brushing at least once a day and at least a single fluoride therapy session performed by a dentist in a healthcare center or clinic were considered as the toothbrushing and fluoride therapy criteria. With regard to dietary milk intake, we considered at least one cup (nearly 200 mL) of milk per day as an adequate intake, with any less being considered insufficient.[24]
Statistical analysis
The Statistical Package for Social Sciences (version 11) was used for data analysis. The Kolmogorov–Smirnov test was used to assess normality. Descriptive statistics (frequency, mean, and standard deviation) were determined for all variables. Baseline demographics and clinical characteristics were compared among groups using the Student's t-test or the Mann–Whitney U-test, the Chi-square test, and/or Fisher's exact test as appropriate. Because of the nonnormal distribution of the dependent variable (DMF) and its structure, a log-linear analysis was performed to adjust for confounding variables. A level of P < 0.05 was regarded as statistically significant.
RESULTS
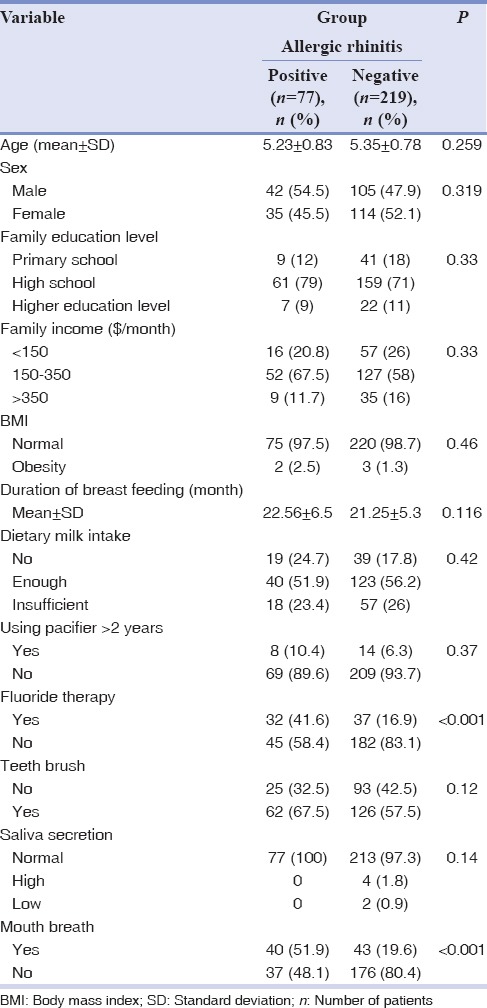
In this study, 77 subjects (35.1%) were AR-positive (AR+) and 219 subjects (64.9%) were AR-negative (AR−). The mean age in the case group was 5.23 ± 0.83 years, compared with 5.35 ± 0.78 years in the control group. There was no significant difference between groups in terms of age (P = 0.259) [Table 1]. In the AR+ group, 54.5% of participants were male, while in the AR− group, 47.5% were male, with no statistically significant difference between gender ratios in the two groups (P = 0.289) [Table 1]. In addition, there were no significant differences between the two groups in the variables listed in Table 1, including education level, family income, breastfeeding duration, dietary milk intake, use of pacifier, toothbrushing, saliva secretion, and BMI (P > 0.05), with the exception of use of fluoride therapy and rate of oral breathing (P < 0.001).
Table 1.
Demographic, nutritional, and hygiene habits data
After oral examination, there was shown to be no significant difference in the rate of tooth decay or DMF scores between the two groups (P = 0.07) although rates of missing and filled teeth differed significantly (P < 0.05) [Table 2].
Table 2.
Comparing decay, missing, filling and DMF index between children with and without allergic rhinitis
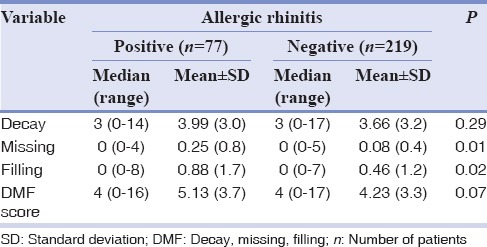
As there were significant differences in the use of fluoride therapy and rate of oral breathing at baseline, these considerations were identified as potential confounding factors. Therefore, we analyzed the relationship between DMF and AR according to the fluoride therapy and oral breathing using log-linear analysis. In this model, the mean DMF in the AR+ group was 20% greater than in the AR− group (odds ratio [OR] = 1.21, confidence interval [CI]: 1.05–1.35) and was also 15% greater among children who breathed orally than those who did not (OR = 1.15 CI: 1.02–1.31).
DISCUSSION
In this cross-sectional study, we aimed to evaluate the independent relationship between AR and DMF. In our study, the prevalence of AR among schoolchildren was 35% as confirmed by clinical presentation and patient history. AR children had more missing and filled teeth but did not show any differences with respect to mean decay and DMF compared with those without AR after crude statistical analysis. Most of the possible risk factors showed no significant differences between the two groups of children, with the exception of fluoride therapy and oral breathing. However, after controlling for two confounding variables by log-linear analysis, we found a significant increase in mean DMF among those who had AR or who breathed orally.
Widmer previously reported that children with respiratory disorders are at greater risk of oral diseases, with both dental hard and soft tissue complications being more likely in these children. These oral health problems are associated with the illness itself or its drug therapies.[25] In rhinitis, children will often need to breathe orally due to significant nasal obstruction, dried mouth, and problems similar to those of asthmatic children. Thus, treatment of AR can have a positive effect on dental health.[24]
Some studies have shown that drug therapies for AR that decrease salivary flow rate may play a role in DMF.[18,25] Drug therapy in AR, including antihistamines, decongestants, corticosteroids, mast cell stabilizers, and leukotriene modifiers, is important for patients with mild-to-moderate allergy symptoms.[26] Since saliva protects against dental caries,[27] dry mouth, which is one side effect of antihistamines, could affect oral health.[28] On the other hand, oral breathing in AR patients also leads to dry mouth, and this can increase the risk of gingiva inflammation, tooth decay, and also enamel demineralization.[29,30]
However, other studies in this field show contrary results. In a study conducted in students aged 13–15 years, Herrström and Högstedt concluded that there is no association between allergic diseases and dental health.[31] Another observational study in 40 children with AR and 40 healthy children in Thailand showed no statistically significant differences in combined DMFT/dmft between cases and controls.[18] Vázquez-Nava et al. also studied the effect of AR on dental caries in primary dentition in 1160 children aged 4–5 years.[1] This study reported that AR itself is not a risk factor for dental caries, but children who have AR and use a pacifier are at higher risk for developing dental caries.[1]
Other authors have reported that maternal educational level and socioeconomic position have an influence on dental caries.[32,33] A study in Greece showed that parental educational level is a significant factor for DMF,[34] with similar results reported by Pérez-Suárez et al. who studied the effects of educational level and prolonged pacifier use on DMF.[35] Vázquez-Nava et al. reported that BMI could have an effect on dental caries in primary dentitions.[36] The basic variables affecting dental caries between the two groups in our study were the same as those in the previously mentioned studies. However, as our study showed no significant difference between allergic and nonallergic individuals in terms of socioeconomic status and BMI, we could not assess the effect of these factors on DMF.
This study has a number of limitations. For example, because we did not perform a skin prick test to confirm the diagnosis of AR, the disease prevalence may have been greater than the calculated rate. The cross-sectional methodology of the study and the lack of data relating to microorganisms of the mouth are other limitations.
The study is completely applicable for the children with transit dentition which was the main goal of study because this type of dentition is widely during the age of preschool. Our sampling was a cluster type randomly that is a good sample of the community for this age group.
Future study with large sampling in different geographic area of the country and world were highly recommended to get a definitive conclusion, especially in condition, that the AR is confirmed through clinical tests.
CONCLUSION
AR and oral breathing may have an effect on oral health and dental condition, leading to an increased rate of missing and filled teeth.
Financial support and sponsorship
The authors acknowledge the support of Mashhad University of Medical Science Research Council for this study.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or non-financial in this article.
Acknowledgments
The Mashhad University of Medical Science Research Council supported this research. In addition, we would like to thank Dr. Hedieh Totoni and the preschool staff, children, and their parents for their cooperation in this study.
REFERENCES
- 1.Vázquez-Nava F, Vázquez RE, Saldivar GA, Beltrán GF, Almeida AV, Vázquez RC, et al. Allergic rhinitis, feeding and oral habits, toothbrushing and socioeconomic status. Effects on development of dental caries in primary dentition. Caries Res. 2008;42:141–7. doi: 10.1159/000121438. [DOI] [PubMed] [Google Scholar]
- 2.Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733–43. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 3.Strachan DP. Hay fever, hygiene, and household size. BMJ. 1989;299:1259–60. doi: 10.1136/bmj.299.6710.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Illi S, von Mutius E, Lau S, Bergmann R, Niggemann B, Sommerfeld C, et al. Early childhood infectious diseases and the development of asthma up to school age: A birth cohort study. BMJ. 2001;322:390–5. doi: 10.1136/bmj.322.7283.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramsey CD, Gold DR, Litonjua AA, Sredl DL, Ryan L, Celedón JC, et al. Respiratory illnesses in early life and asthma and atopy in childhood. J Allergy Clin Immunol. 2007;119:150–6. doi: 10.1016/j.jaci.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 6.Kramer MS, Guo T, Platt RW, Sevkovskaya Z, Dzikovich I, Collet JP, et al. Does previous infection protect against atopic eczema and recurrent wheeze in infancy? Clin Exp Allergy. 2004;34:753–6. doi: 10.1111/j.1365-2222.2004.1940.x. [DOI] [PubMed] [Google Scholar]
- 7.Balemans WA, Rovers MM, Schilder AG, Sanders EA, Kimpen JL, Zielhuis GA, et al. Recurrent childhood upper respiratory tract infections do not reduce the risk of adult atopic disease. Clin Exp Allergy. 2006;36:198–203. doi: 10.1111/j.1365-2222.2006.02423.x. [DOI] [PubMed] [Google Scholar]
- 8.Mommers M, Swaen GM, Weishoff-Houben M, Creemers H, Freund H, Dott W, et al. Childhood infections and risk of wheezing and allergic sensitisation at age 7-8 years. Eur J Epidemiol. 2004;19:945–51. doi: 10.1007/s10654-004-6016-7. [DOI] [PubMed] [Google Scholar]
- 9.Benn CS, Melbye M, Wohlfahrt J, Björkstén B, Aaby P. Cohort study of sibling effect, infectious diseases, and risk of atopic dermatitis during first 18 months of life. BMJ. 2004;328:1223. doi: 10.1136/bmj.38069.512245.FE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bessa CF, Santos PJ, Aguiar MC, do Carmo MA. Prevalence of oral mucosal alterations in children from 0 to 12 years old. J Oral Pathol Med. 2004;33:17–22. [PubMed] [Google Scholar]
- 11.Lee SL, Wong W, Lau YL. Increasing prevalence of allergic rhinitis but not asthma among children in Hong Kong from 1995 to 2001 (Phase 3 International Study of Asthma and Allergies in Childhood) Pediatr Allergy Immunol. 2004;15:72–8. doi: 10.1046/j.0905-6157.2003.00109.x. [DOI] [PubMed] [Google Scholar]
- 12.Vázquez-Nava F, Quezada-Castillo JA, Oviedo-Treviño S, Saldivar-González AH, Sánchez-Nuncio HR, Beltrán-Guzmán FJ, et al. Association between allergic rhinitis, bottle feeding, non-nutritive sucking habits, and malocclusion in the primary dentition. Arch Dis Child. 2006;91:836–40. doi: 10.1136/adc.2005.088484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh S, Vijayakumar N, Priyadarshini HR, Shobha M. Prevalence of early childhood caries among 3-5 year old pre-schoolers in schools of Marathahalli, Bangalore. Dent Res J (Isfahan) 2012;9:710–4. [PMC free article] [PubMed] [Google Scholar]
- 14.Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet. 2007;369:51–9. doi: 10.1016/S0140-6736(07)60031-2. [DOI] [PubMed] [Google Scholar]
- 15.Samadzadeh H. Oral Health Situation of Iranian Children. 1st ed. Tehran: Ministry of Health and Medical Education, Deputy for Health, Oral Health Bureau; 1999. [Google Scholar]
- 16.Bayat-Movahed S, Samadzadeh H, Ziyarati L, Memary N, Khosravi R, Sadr-Eshkevari PS, et al. Oral health of Iranian children in 2004: A national pathfinder survey of dental caries and treatment needs. East Mediterr Health J. 2011;17:243–9. [PubMed] [Google Scholar]
- 17.World Health Organization. Oral Health Surveys: Basic Methods. 4th ed. Geneva: WHO; 1997. [Google Scholar]
- 18.Wongkamhaeng K, Poachanukoon O, Koontongkaew S. Dental caries, cariogenic microorganisms and salivary properties of allergic rhinitis children. Int J Pediatr Otorhinolaryngol. 2014;78:860–5. doi: 10.1016/j.ijporl.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 19.Arora A, Schwarz E, Blinkhorn AS. Risk factors for early childhood caries in disadvantaged populations. J Investig Clin Dent. 2011;2:223–8. doi: 10.1111/j.2041-1626.2011.00070.x. [DOI] [PubMed] [Google Scholar]
- 20.Tadakamadla SK, Tadakamadla J, Tibdewal H, Duraiswamy P, Kulkarni S. Dental caries in relation to socio-behavioral factors of 6-year-old school children of Udaipur District, India. Dent Res J (Isfahan) 2012;9:681–7. [PMC free article] [PubMed] [Google Scholar]
- 21.Friedrich N, Völzke H, Schwahn C, Kramer A, Jünger M, Schäfer T, et al. Inverse association between periodontitis and respiratory allergies. Clin Exp Allergy. 2006;36:495–502. doi: 10.1111/j.1365-2222.2006.02455.x. [DOI] [PubMed] [Google Scholar]
- 22.Arbes SJ, Jr, Sever ML, Vaughn B, Cohen EA, Zeldin DC. Oral pathogens and allergic disease: Results from the Third National Health and Nutrition Examination Survey. J Allergy Clin Immunol. 2006;118:1169–75. doi: 10.1016/j.jaci.2006.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, et al. International Study of Asthma and Allergies in Childhood (ISAAC): Rationale and methods. Eur Respir J. 1995;8:483–91. doi: 10.1183/09031936.95.08030483. [DOI] [PubMed] [Google Scholar]
- 24.TIPS for Using the FOOD GUIDE PYRAMID for Young Children 2 to 6 Years Old. United States Department of Agriculture. 1999. [Last accessed on 2016 May]. Available from: https://www.cnpp.usda.gov/sites/default/files/archived_projects/FGP4KidsTipsBook.pdf .
- 25.Widmer RP. Oral health of children with respiratory diseases. Paediatr Respir Rev. 2010;11:226–32. doi: 10.1016/j.prrv.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 26.Platt M. Pharmacotherapy for allergic rhinitis. Int Forum Allergy Rhinol. 2014;4(Suppl 2):S35–40. doi: 10.1002/alr.21381. [DOI] [PubMed] [Google Scholar]
- 27.Krol DM. Dental caries, oral health, and pediatricians. Curr Probl Pediatr Adolesc Health Care. 2003;33:253–70. doi: 10.1016/s1538-5442(03)00093-2. [DOI] [PubMed] [Google Scholar]
- 28.Sweetman S. Martindale: The Complete Drug Reference. London, England, UK: Pharmaceutical Press; 2009. [Google Scholar]
- 29.Al-Awadi RN, Al-Casey M. Oral health status, salivary physical properties and salivary mutans streptococci among a group of mouth breathing patients in comparison to nose breathing. J Baghdad Coll Dent. 2013;25:152–9. [Google Scholar]
- 30.Bakor SF, Pereira JC, Frascino S, Gonçalves TC, Ladalardo P, Pignatari SS, et al. Demineralization of teeth in mouth-breathing patients undergoing maxillary expansion. Braz J Otorhinolaryngol. 2010;76:709–12. doi: 10.1590/S1808-86942010000600007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herrström P, Högstedt B. Allergic diseases, dental health, and socioeconomic situation of Swedish teenagers: Allergy, dental health, and social situation. Scand J Prim Health Care. 1994;12:57–61. doi: 10.3109/02813439408997058. [DOI] [PubMed] [Google Scholar]
- 32.Sayegh A, Dini EL, Holt RD, Bedi R. Caries prevalence and patterns and their relationship to social class, infant feeding and oral hygiene in 4-5-year-old children in Amman, Jordan. Community Dent Health. 2002;19:144–51. [PubMed] [Google Scholar]
- 33.Sayegh A, Dini EL, Holt RD, Bedi R. Oral health, sociodemographic factors, dietary and oral hygiene practices in Jordanian children. J Dent. 2005;33:379–88. doi: 10.1016/j.jdent.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 34.Boka V, Trikaliotis A, Kotsanos N, Karagiannis V. Dental caries and oral health-related factors in a sample of Greek preschool children. Eur Arch Paediatr Dent. 2013;14:363–8. doi: 10.1007/s40368-013-0097-5. [DOI] [PubMed] [Google Scholar]
- 35.Pérez-Suárez V, Carrillo-Diaz M, Crego A, Romero M. Maternal education, dental visits and age of pacifier withdrawal: Pediatric dentist role in malocclusion prevention. J Clin Pediatr Dent. 2013;37:315–9. doi: 10.17796/jcpd.37.3.p0303070101675ht. [DOI] [PubMed] [Google Scholar]
- 36.Vázquez-Nava F, Vázquez-Rodríguez EM, Saldívar-González AH, Lin-Ochoa D, Martinez-Perales GM, Joffre-Velázquez VM, et al. Association between obesity and dental caries in a group of preschool children in Mexico. J Public Health Dent. 2010;70:124–30. doi: 10.1111/j.1752-7325.2009.00152.x. [DOI] [PubMed] [Google Scholar]


