Abstract
Background:
During sliding mechanics, the frictional force (FF) is an important counterforce to orthodontic tooth movement. The purpose of this in vitro study was to investigate the static and kinetic FFs of S silica-insert ceramic (SIC) brackets with Teflon-coated (TC) and conventional S stainless steel (SS) archwires.
Materials and Methods:
The target group of this study included 80 maxillary canine 0.022 inch slot SIC brackets. Forty SS brackets were used as the control. TC and conventional uncoated SS archwires of different dimensions (0.016, 0.018, 0.016 × 0.022, and 0.018 × 0.025 inch) were examined. All tests were carried out under artificial saliva injected condition. Scanning Electron Micrographs were prepared for two samples of coated and uncoated archwires. Analysis of variance and Tukey post hoc tests were used for statistical purposes (level of significance P < 0.05).
Results:
SIC brackets showed significantly lower levels of FFs than SS brackets. TC archwires had greater frictional values than conventional uncoated ones. They also exhibited an unusual behavior of increasing kinetic FFs with time. Indentation and delamination of coating were obvious under scanning electron microscopy observations.
Conclusion:
From the standpoint of friction, SIC brackets may serve well, even better than SS brackets, in sliding mechanics. The coating layer of the archwires may delaminate and lost, causing an impediment to tooth movement.
Keywords: Artificial, Friction, orthodontic bracket, saliva
INTRODUCTION
The resistance to sliding of orthodontic brackets has three major components: Friction, binding, and notching of the archwire.[1] In situations where the contact angle θ is below the critical value, the only component existing is friction, because binding[2,3] and notching do not take place at these situations.
During orthodontic treatment, teeth can be moved either by closing loop mechanics, which minimizes the frictional forces (FFs) or by sliding mechanics, in which FFs are considerable. There are two types of friction. Static friction is the smallest force needed to initiate the motion. Kinetic friction is the force needed to resist the sliding motion of one solid object over another at a constant speed.[4] Kusy and Whitley[1] and Articolo andKusy[5] showed that 12%–60% of the applied force may have been lost due to frictional resistance.
Different factors can influence frictional resistance: Wire and bracket materials, wire section, active torque at the wirebracket interface, the surface condition of brackets and archwires, force and type of ligation, saliva, lubrication, interbracket distance and the angle between wire and brackets.[2,6,7,8]
The appearance of the orthodontic appliances has always been of great importance for orthodontic patients, especially the adult ones. Ceramic brackets were basically introduced to meet these esthetic demands, but several problems came up in practice, including brittleness of ceramics which may cause fracture of the tie wings or brackets, iatrogenic damage to enamel on debonding, enamel attrition of the opposing tooth and the most important of them all, high levels of FFs during sliding mechanics.[6] Different studies reported that the FFs of ceramic brackets were higher than stainless steel (SS) ones.[9,10] To reduce these unwanted side-effects, ceramic brackets with smoother slots, such as metal insert ceramic (MIC) brackets, were introduced. Although the FFs in MIC brackets were lower than conventional ceramic brackets,[11,12] they were still significantly higher than SS brackets.[9]
Along with the developments occurring in esthetic brackets, tooth-colored archwires were also introduced. Zufall and Kusy[13] reported that the coated composite archwires increased the friction and binding. Ion implanted coated beta-titanium archwires were reported to have frictional resistance comparable to SS wires.[14,15] The most common method for coating the archwires is using teflon or epoxy resin. There is some controversy about their effect on friction, but all the previous studies agree that these coatings are “undurable.”[16,17]
As silica-insert ceramic (SIC) brackets and coated archwires have been introduced in recent years, the purpose of this study was to evaluate the frictional behavior of this bracket in combination with coated archwires in the wet state.
MATERIALS AND METHODS
In this in vitro study, two types of maxillary canine 0.022 inch slot brackets with Roth prescription were tested: Eighty SIC brackets (GAC Int., Bohemia, New York, USA) and forty SS brackets (GAC Int., Bohemia, New York, USA). The tested archwires (GAC Int., Bohemia, New York, USA) were of two types: 80 conventional SS and 40 Teflon-coated (TC) SS. The archwires had four different dimensions: 0.016, 0.018, 0.016 × 0.022 and 0.018 × 0.025 inch. The archwires were cut into 4 cm sections. Before the tests, the diameter of the archwires was measured by a digital gauge. Scanning electron microscopy (SEM, Model S360, Oxford, England) was used to evaluate the surface morphology of the SS and TC archwires before and after the tests.
All the brackets were bonded onto a 2.5 cm diameter tubes filled with self-cure acrylic (Meliodent, Bayer Co., Germany), using a two-paste instantaneous glue.
Friction was measured with a universal testing machine (Model Z250, Zwick, Ulm, Germany) at a room temperature of 25°C. Special jigs were designed for the testing machine. The lower jig enclasped the tubes. It had a line scribed in the midline to act as a guide for reproducible bracket position. The archwire segments were fixed in the jig connected to the upper jaw. A total number of 120 bracket archwire segments were evaluated. Each bracket was tested only once, and each archwire segment was drawn through only one bracket to eliminate the effect of wear.
To better simulation of the clinical conditions, elastomeric modules (Ortho Technology Inc., Tampa, Florida, USA) were used to ligate the archwires in the brackets. The same person placed all the elastomeric modules, and it was done immediately before each test to avoid the force degradation effect. To standardize this procedure, an elastomeric module placer was used to assimilate the amount of elastomerics extension. Before the evaluation, three drops of artificial saliva (Fusayama–Meyere formula) were applied at the bracket-archwire interface using a 10 mL syringe.
The 10 N load cell was calibrated between 0 and 10 N, and the archwires were drawn through the brackets as the crosshead moved superiorly at a rate of 2.5 mm/min. The frictional values were then transmitted to a computer hard disk and analyzed with testXpert® software (Zwick, Ulm, Germany). The data were recorded on an XY recorder. The X axis showed bracket movement in millimeters. The Y axis recorded the FF between the bracket and the archwire in cN. Initial peak of movement represented static friction. Kinetic friction was calculated by averaging 5 recordings 10 s apart on the Y axis after the initial peak. Descriptive statistics, including mean, standard deviation, minimum and maximum values were calculated for each bracket-archwire combination. To ensure the normal distribution of the data, Kolmogorov–Smirnov test was used. The results were examined by using one-way analysis of variance. For the post hoc test, the Tukey test was used. The level of significance for all tests was set at P < 0.05. All statistical analyses were performed with SPSS software (version 11.5, SPSS, Chicago, IL, USA).
RESULTS
The descriptive statistics of static and kinetic FFs for each bracket-archwire combination are shown in Table 1. Two-by-two comparison between the groups was done by Tukey post hoc test and is presented in Table 2. The highest levels of static and kinetic FFs were observed in SS brackets and 0.018 × 0.025 inch SS archwires. The lowest levels were seen in SIC brackets and 0.016 inch TC wires.
Table 1.
Mean and standard deviation of static and kinetic frictional forces
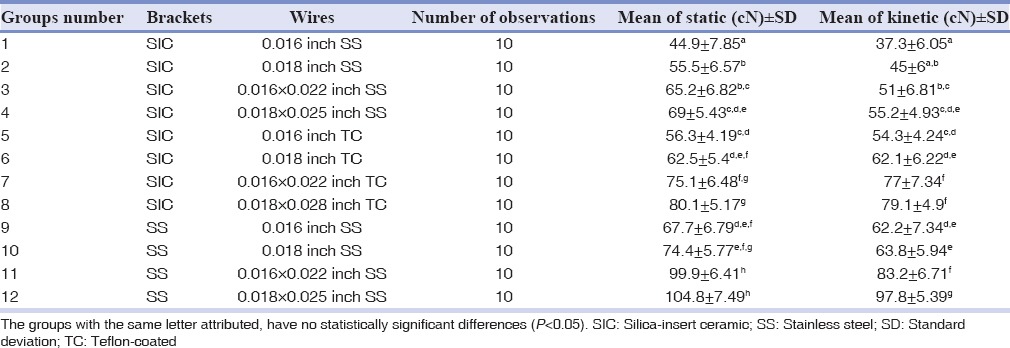
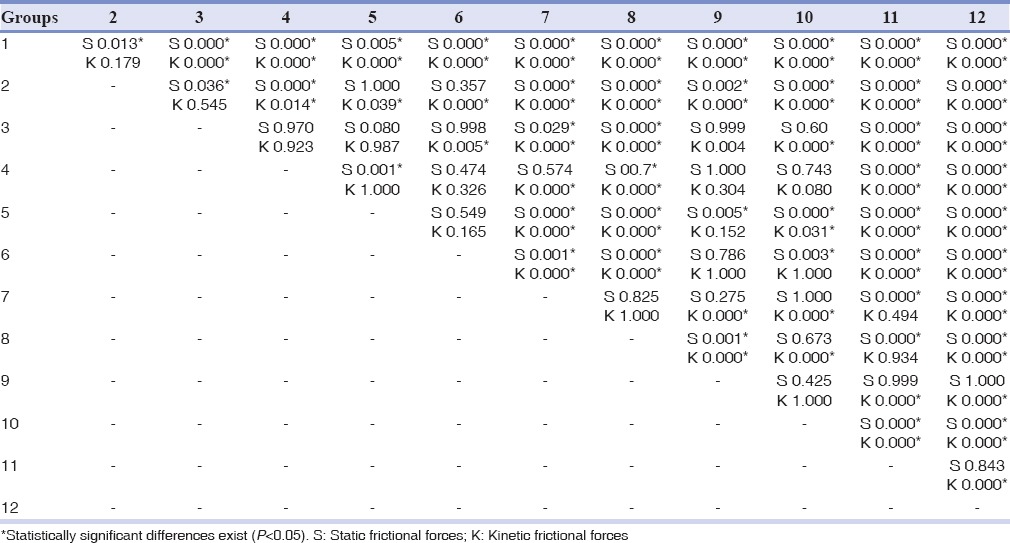
Table 2.
P values of the Tukey post hoc test for static and kinetic frictional forces between groups
The groups with SIC brackets and SS wires had the lowest amounts of FFs. The groups with SS brackets and SS wires had the highest levels.
Increasing the size of the archwires increased the levels of static and kinetic FFs. Generally speaking, rectangular wires showed higher amounts of FFs than round ones. In SIC brackets, the TC archwires had significantly greater levels of FFs (P < 0.05), compared to SS wires.
In all groups with SS archwires, the static FFs were higher than kinetic FFs. However in groups containing TF archwires, extremely small differences were observed between static and kinetic FFs. Even in one group (SIC brackets and 0.016 × 0.022 inch TC wires), the kinetic friction was higher than static friction.
SEM examination of SS archwires in SIC brackets showed a slight increase in the amounts of facets and wears [Figure 1a and b]. In contrast to SS wires, the TC ones showed a significant amount of coating deterioration and indentation [Figure 1c and d]. The coating in some parts was delaminated or missed.
Figure 1.
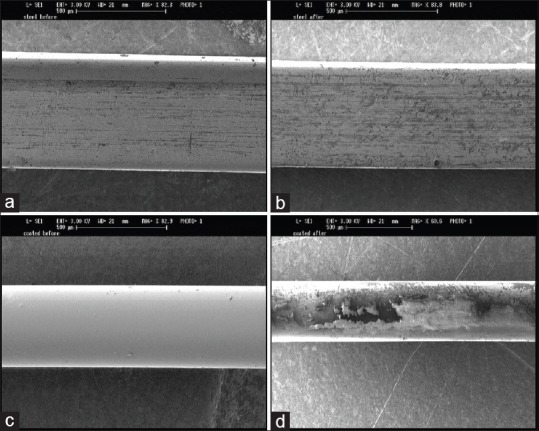
The scanning electron microscopy microphotographs of (a) the stainless steel wire before and (b) after the friction test, (c) the Teflon-coated wire before and (d) after the friction test.
Using a digital gauge, we found the size of the TC wires of this manufacturer to be on average 0.001 inch larger than their corresponding SS ones.
DISCUSSION
Considering the rising demand for esthetic brackets, the use of ceramic brackets for anterior teeth has increased. However, previous studies have demonstrated higher FFs of ceramic brackets compared to SS braces.[18,19,20] Despite the emphasis it now receives in the marketing of brackets, some believed that friction is not the major component of “resistance to sliding” in the clinic.[19] They stated that binding of the wire against the corners of the bracket is much more important than previously thought. However, in the present study, we evaluated the static and kinetic “FFs” of the SIC brackets. It does not rule out the influence of binding or notching in increased “resistance to sliding.”
The tested archwires were all steel and divided into two groups of TC and conventional SS. The SS brackets were used as the control.
Table 1 demonstrates that an increase in the size of the archwires may cause an increase in the frictional levels. Several studies so far, have investigated the effect of archwire size on the amount of friction generated. All of them, in accordance with our study, reported that larger wires would increase FFs.[21,22,23,24]
The current study showed that SIC brackets have lower FFs, even lower than SS brackets. To the best of our knowledge, very few studies have investigated the friction of SIC brackets. Cha et al.[25] reported that silica layer and rounded edges of the SIC brackets lowered the FFs. These brackets had minimal frictional resistance among ceramic brackets, comparable to the conventional SS brackets. Doshi and Bhad-Patil[26] investigated ceramic brackets with gold-palladium slots and concluded that these brackets have a smoother surface and lower friction than SS brackets and seem to be a good alternative to SS brackets in space closure with sliding mechanics.
Till date, the body of the literature considered the SS brackets as the gold standard of friction that has the lowest FFs. However, our study showed that the SIC have lower static and kinetic FFs than SS brackets. Two reasons may be hypothesized for this finding: (1) as we tried to follow clinical conditions, artificial saliva may cause the SS wires to show an adhesive behavior, as reported by Kusy et al.[27] This adhesion could be responsible for the increased FFs during the tests. (2) With the help of the modern technologies, we are now capable of manufacturing new brackets that have lower friction than SS brackets. It seems that the default notion that SS brackets have the lowest levels of FFs will be challenged even more in future.
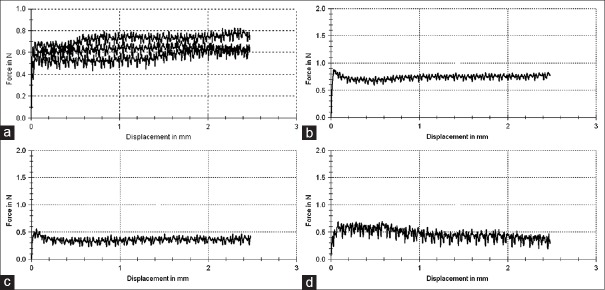
There has been some controversy on whether static or kinetic friction is more important during orthodontic therapy,[28] but the majority of the studies reported the kinetic one to be more important, because sliding of a tooth or bracket on an archwire is not a continuous or constant motion.[29] In fact, due to the dynamic condition of the oral cavity, it is relatively a series of short steps.[30] In previous studies, the static FFs were greater than kinetic FFs,[31,32] although this difference was not always significant.[33] In the current study, we found the same thing to be true about the conventional SS wires. But with TC wires, the difference between static and kinetic FFs became considerably narrow, and even in one of the test groups (SIC brackets and 0.016 × 0.022 inch TC wires), the kinetic FFs were greater than static ones. We found this unusual behavior of increasing kinetic FFs with time to be present in about half of the TC wires [Figure 2a]. One possible reason for this finding might be the indentation of TC wires when sliding in SIC brackets.
Figure 2.
Frictional diagrams of (a) three Teflon-coated wires pulling through silica-insert ceramic brackets, (b) a 0.018 inch stainless steel archwire pulling through a stainless steel bracket, (c) a 0.018 inch stainless steel archwire pulling through a silica-insert ceramic bracket and (d) a 0.018 inch Teflon-coated archwire pulling through a silica-insert ceramic bracket.
Figure 2b and c shows the frictional diagram of a 0.018 inch SS wire in SS and SIC brackets, respectively. Figure 2d shows that diagram for a 0.018 inch TC wire in a SIC bracket. The range of the differences during the tests is wider for the TC wires. This phenomenon can also be allocated to delamination or indentation of the coating of the TC wires. Elayyan et al.[17] reported that in a 4–6 weeks, 25% of the coating of the wires will be lost in the clinic. Irregularities produced in the coated wires may induce plaque accumulation. Furthermore, sticking these irregularities to the bracket edges may slow down or impede tooth movement through an increase in FFs.[34]
SEM microphotographs of a SS archwire before and after the test [Figure 1a and b], shows a slight increase in the amount of scratches and facets on the wire. In contrast, the SEM microphotographs of a TC archwire taken before and after the test [Figure 1c and d], shows a considerable delamination, indentation and destruction of the coating. These microphotographs can elucidate the unusual behaviors of the TC wires (wide range of differences in FFs during the test and increasing kinetic FFs with time).
Finally, it should be mentioned that in the present study the diameter of the TC wires were approximately 0.001 inch larger than their corresponding SS wires. This can, to some extent, contribute to the greater levels of FFs seen in these wires.
CONCLUSION
Based on our findings, the current in vitro study illustrated that as follows:
Static and kinetic FFs in SIC brackets were significantly lower than SS brackets
TC archwires showed higher frictional values than SS archwires
In SS archwires, static FFs were greater than kinetic ones, but in approximately half of the TC wires, the kinetic FFs were higher than static ones
Significant delamination and indentation were observed in coated archwires under SEM observations.
Financial support and sponsorship
Mashhad University of Medical Sciences for financial support of this project.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or nonfinancial in this article.
Acknowledgments
The authors would like to thank vice-chancellor of research of Mashhad University of Medical Sciences for financial support of this project.
The results mentioned in this manuscript are derived from a Doctoral thesis orthodontic (No: 438).
REFERENCES
- 1.Kusy RP, Whitley JQ. Friction between different wire-bracket configurations and materials. Semin Orthod. 1997;3:166–77. doi: 10.1016/s1073-8746(97)80067-9. [DOI] [PubMed] [Google Scholar]
- 2.Frank CA, Nikolai RJ. A comparative study of frictional resistances between orthodontic bracket and arch wire. Am J Orthod. 1980;78:593–609. doi: 10.1016/0002-9416(80)90199-2. [DOI] [PubMed] [Google Scholar]
- 3.Kapila S, Angolkar PV, Duncanson MG, Jr, Nanda RS. Evaluation of friction between edgewise stainless steel brackets and orthodontic wires of four alloys. Am J Orthod Dentofacial Orthop. 1990;98:117–26. doi: 10.1016/0889-5406(90)70005-W. [DOI] [PubMed] [Google Scholar]
- 4.Besancon RM. The Encyclopedia of Physics. 3rd ed. New York: Van Nostrand Reinhold Company; 1985. [Google Scholar]
- 5.Articolo LC, Kusy RP. Influence of angulation on the resistance to sliding in fixed appliances. Am J Orthod Dentofacial Orthop. 1999;115:39–51. doi: 10.1016/S0889-5406(99)70314-8. [DOI] [PubMed] [Google Scholar]
- 6.Angolkar PV, Kapila S, Duncanson MG, Jr, Nanda RS. Evaluation of friction between ceramic brackets and orthodontic wires of four alloys. Am J Orthod Dentofacial Orthop. 1990;98:499–506. doi: 10.1016/0889-5406(90)70015-5. [DOI] [PubMed] [Google Scholar]
- 7.Bourauel C, Fries T, Drescher D, Plietsch R. Surface roughness of orthodontic wires via atomic force microscopy, laser specular reflectance, and profilometry. Eur J Orthod. 1998;20:79–92. doi: 10.1093/ejo/20.1.79. [DOI] [PubMed] [Google Scholar]
- 8.Dickson JA, Jones SP, Davies EH. A comparison of the frictional characteristics of five initial alignment wires and stainless steel brackets at three bracket to wire angulations – An in vitro study. Br J Orthod. 1994;21:15–22. doi: 10.1179/bjo.21.1.15. [DOI] [PubMed] [Google Scholar]
- 9.Nishio C, da Motta AF, Elias CN, Mucha JN. In vitro evaluation of frictional forces between archwires and ceramic brackets. Am J Orthod Dentofacial Orthop. 2004;125:56–64. doi: 10.1016/j.ajodo.2003.01.005. [DOI] [PubMed] [Google Scholar]
- 10.Keith O, Jones SP, Davies EH. The influence of bracket material, ligation force and wear on frictional resistance of orthodontic brackets. Br J Orthod. 1993;20:109–15. doi: 10.1179/bjo.20.2.109. [DOI] [PubMed] [Google Scholar]
- 11.Cacciafesta V, Sfondrini MF, Ricciardi A, Scribante A, Klersy C, Auricchio F, et al. Evaluation of friction of stainless steel and esthetic self-ligating brackets in various bracket-archwire combinations. Am J Orthod Dentofacial Orthop. 2003;124:395–402. doi: 10.1016/s0889-5406(03)00504-3. [DOI] [PubMed] [Google Scholar]
- 12.Loftus BP, Artun J, Nicholls JI, Alonzo TA, Stoner JA. Evaluation of friction during sliding tooth movement in various bracket-arch wire combinations. Am J Orthod Dentofacial Orthop. 1999;116:336–45. doi: 10.1016/s0889-5406(99)70247-7. [DOI] [PubMed] [Google Scholar]
- 13.Zufall SW, Kusy RP. Sliding mechanics of coated composite wires and the development of an engineering model for binding. Angle Orthod. 2000;70:34–47. doi: 10.1043/0003-3219(2000)070<0034:SMOCCW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Burstone CJ, Farzin-Nia F. Production of low-friction and colored TMA by ion implantation. J Clin Orthod. 1995;29:453–61. [PubMed] [Google Scholar]
- 15.Cash A, Curtis R, Garrigia-Majo D, McDonald F. A comparative study of the static and kinetic frictional resistance of titanium molybdenum alloy archwires in stainless steel brackets. Eur J Orthod. 2004;26:105–11. doi: 10.1093/ejo/26.1.105. [DOI] [PubMed] [Google Scholar]
- 16.Proffit WR. Contemporary Orthodontics. St. Louis: Mosby Company; 2000. [Google Scholar]
- 17.Elayyan F, Silikas N, Bearn D. Ex vivo surface and mechanical properties of coated orthodontic archwires. Eur J Orthod. 2008;30:661–7. doi: 10.1093/ejo/cjn057. [DOI] [PubMed] [Google Scholar]
- 18.Prashant PS, Nandan H, Gopalakrishnan M. Friction in orthodontics. J Pharm Bioallied Sci. 2015;7:S334–8. doi: 10.4103/0975-7406.163439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burrow SJ. Friction and resistance to sliding in orthodontics: A critical review. Am J Orthod Dentofacial Orthop. 2009;135:442–7. doi: 10.1016/j.ajodo.2008.09.023. [DOI] [PubMed] [Google Scholar]
- 20.Fidalgo TK, Pithon MM, Maciel JV, Bolognese AM. Friction between different wire bracket combinations in artificial saliva – An in vitro evaluation. J Appl Oral Sci. 2011;19:57–62. doi: 10.1590/S1678-77572011000100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Read-Ward GE, Jones SP, Davies EH. A comparison of self-ligating and conventional orthodontic bracket systems. Br J Orthod. 1997;24:309–17. doi: 10.1093/ortho/24.4.309. [DOI] [PubMed] [Google Scholar]
- 22.Henao SP, Kusy RP. Evaluation of the frictional resistance of conventional and self-ligating bracket designs using standardized archwires and dental typodonts. Angle Orthod. 2004;74:202–11. doi: 10.1043/0003-3219(2004)074<0202:EOTFRO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Hain M, Dhopatkar A, Rock P. A comparison of different ligation methods on friction. Am J Orthod Dentofacial Orthop. 2006;130:666–70. doi: 10.1016/j.ajodo.2006.04.021. [DOI] [PubMed] [Google Scholar]
- 24.Pizzoni L, Ravnholt G, Melsen B. Frictional forces related to self-ligating brackets. Eur J Orthod. 1998;20:283–91. doi: 10.1093/ejo/20.3.283. [DOI] [PubMed] [Google Scholar]
- 25.Cha JY, Kim KS, Hwang CJ. Friction of conventional and silica-insert ceramic brackets in various bracket-wire combinations. Angle Orthod. 2007;77:100–7. doi: 10.2319/092705-333R.1. [DOI] [PubMed] [Google Scholar]
- 26.Doshi UH, Bhad-Patil WA. Static frictional force and surface roughness of various bracket and wire combinations. Am J Orthod Dentofacial Orthop. 2011;139:74–9. doi: 10.1016/j.ajodo.2009.02.031. [DOI] [PubMed] [Google Scholar]
- 27.Kusy RP, Whitley JQ, Prewitt MJ. Comparison of the frictional coefficients for selected archwire-bracket slot combinations in the dry and wet states. Angle Orthod. 1991;61:293–302. doi: 10.1043/0003-3219(1991)061<0293:COTFCF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Smart FM. Kinetic friction. Am J Orthod Dentofacial Orthop. 2004;125:17A. doi: 10.1016/j.ajodo.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 29.Thomas S, Sherriff M, Birnie D. A comparative in vitro study of the frictional characteristics of two types of self-ligating brackets and two types of pre-adjusted edgewise brackets tied with elastomeric ligatures. Eur J Orthod. 1998;20:589–96. doi: 10.1093/ejo/20.5.589. [DOI] [PubMed] [Google Scholar]
- 30.Moore MM, Harrington E, Rock WP. Factors affecting friction in the pre-adjusted appliance. Eur J Orthod. 2004;26:579–83. doi: 10.1093/ejo/26.6.579. [DOI] [PubMed] [Google Scholar]
- 31.Keith O, Kusy RP, Whitley JQ. Zirconia brackets: An evaluation of morphology and coefficients of friction. Am J Orthod Dentofacial Orthop. 1994;106:605–14. doi: 10.1016/S0889-5406(94)70085-0. [DOI] [PubMed] [Google Scholar]
- 32.Downing A, McCabe JF, Gordon PH. The effect of artificial saliva on the frictional forces between orthodontic brackets and archwires. Br J Orthod. 1995;22:41–6. doi: 10.1179/bjo.22.1.41. [DOI] [PubMed] [Google Scholar]
- 33.Kapur R, Sinha PK, Nanda RS. Comparison of frictional resistance in titanium and stainless steel brackets. Am J Orthod Dentofacial Orthop. 1999;116:271–4. doi: 10.1016/s0889-5406(99)70237-4. [DOI] [PubMed] [Google Scholar]
- 34.Neumann P, Bourauel C, Jäger A. Corrosion and permanent fracture resistance of coated and conventional orthodontic wires. J Mater Sci Mater Med. 2002;13:141–7. doi: 10.1023/a:1013831011241. [DOI] [PubMed] [Google Scholar]