Abstract
Background:
Hip arthroscopic surgery is intended to treat multiple abnormalities in an effort to delay the progression to osteoarthritis, especially in young patients. However, the length of time in which patients experience joint pain before seeking a specialist for a diagnosis can delay hip preservation surgery and influence clinical outcomes.
Purpose:
To investigate the relationship between age at symptom onset and findings during hip arthroscopic surgery as well as outcomes after 2 years of clinical follow-up.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
From February 2008 to March 2015, data were prospectively collected on all patients undergoing hip arthroscopic surgery at a single institution. Anatomic and pathological characteristics were recorded intraoperatively. The mean age at onset of symptoms was calculated and correlated with intraoperative findings using Pearson correlation and logistic regression. All patients were assessed preoperatively and postoperatively with 4 patient-reported outcome measures: the modified Harris Hip Score (mHHS), the Non-Arthritic Hip Score (NAHS), the Hip Outcome Score–Activities of Daily Living (HOS-ADL), and the Hip Outcome Score–Sport-Specific Subscale (HOS-SSS). Pain was estimated using a visual analog scale (VAS). Furthermore, patients with an age at onset of symptoms below the mean (34.6 years) were compared with those of an age at onset of symptoms above the mean. The 2 groups were compared using the Student t test and the chi-square test. P values <.05 were considered significant.
Results:
A total of 1697 patients met the inclusion criteria. Body mass index was weakly correlated with age (r = 0.3). Younger patients had a lower prevalence of combined Seldes type 1 and 2 labral tears; acetabular labrum articular disruption (ALAD) grade 2, 3, and 4 acetabular chondral lesions; and Outerbridge grade 2, 3, and 4 femoral head chondral lesions (P < .05 for all). More advanced age was correlated with wider labral tears and chondral lesions based on a clock face (r ≥ 0.2, P < .05). Patients younger than 34.6 years had a lower prevalence of gluteus medius and ligamentum teres tears (P ≤ .001). The prevalence of synovitis was positively correlated with age, while instability was negatively correlated with age (P = .04). The improvement of scores from preoperatively to 2-year follow-up in the younger patient group was 62.69 to 83.82 for the mHHS, 64.97 to 87.35 for the HOS-ADL, 43.46 to 73.37 for the HOS-SSS, 63.01 to 85.19 for the NAHS, and 5.61 to 2.53 for pain VAS. All score improvements were statistically significant (P < .001). Regarding the older patient group, the improvement of scores from preoperatively to 2-year follow-up was 58.55 to 78.27 for the mHHS, 57.59 to 79.66 for the HOS-ADL, 35.63 to 61.88 for the HOS-SSS, 55.28 to 77.55 for the NAHS, and 5.72 to 3.01 for pain VAS. All score improvements were statistically significant (P < .001).
Conclusion:
Of the multiple intraoperative findings in hip arthroscopic surgery, many are related to age at onset of symptoms. Although we found a statistically significant improvement in clinical outcomes in both groups after 2-year follow-up, apparently the less complex and smaller lesions observed in both the articular cartilage and the labrum of younger patients result in better outcomes compared with older patients.
Keywords: hip arthroscopic surgery, labrum, cartilage, age
The current literature on hip arthroscopic surgery and femoroacetabular impingement (FAI) focuses on diagnosis and treatment in an effort to delay the progression to osteoarthritis, especially in young patients.1,2,15,20,34 However, the length of time in which patients experience joint pain before seeking a specialist for a diagnosis can delay hip preservation surgery and influence clinical outcomes. Usually, patients affected by FAI present with persistent insidious deep groin, lateral, or buttock pain (C-sign), worsened by prolonged sitting or standing and hip flexion–type movements.37 Often presenting with concomitant labral tears, patients may report mechanical symptoms, such as catching, locking, and clicking.18 In younger patients, the onset of symptoms is often a consequence of an acute injury or minor trauma, especially in athletes, for whom pain may be exacerbated by excessive demand.16 On physical examination, decreased range of motion is evident, particularly with passive flexion, internal rotation, and adduction of the affected hip, often referred to as an “impingement test.”5 With pincer-type FAI and posteroinferior impingement, hip extension and external rotation may also elicit pain.11 The Drehmann sign is positive if there is obligatory passive external rotation of the hip while performing hip flexion.21 Gluteus medius tears are more common in women and have a peak incidence within the fourth to sixth decades of life.35 Patients can present with either acute or chronic symptoms. Chronic presentation is more common, with patients typically complaining of the insidious onset of dull pain over the proximal aspect of the lateral hip that may worsen by lying on the affected hip, walking, or climbing stairs.9,13 There is usually tenderness on palpation of the greater trochanter, limping, or lurch on examination and reduced power on resisted abduction of the hip.26 In contrast, patients with acute symptoms for traumatic tears can precisely pinpoint the onset of their pain.36
On the other hand, an onset of symptoms at older age is related more with the normal degenerative process. Although numerous previous studies have considered the relationship between the patient’s age and the outcomes of hip arthroscopic surgery, the possible relationships of age to specific abnormalities of the hip identified during surgery have not been fully evaluated.12,27,31–33 The purpose of this study was to investigate the relationship between age at onset of symptoms and intraoperative pathological findings during hip arthroscopic surgery with clinical outcomes after 2-year follow-up.
Methods
From February 2008 to March 2015, data were prospectively collected on all patients undergoing hip arthroscopic surgery at a single institution. Demographic factors, including sex, age at onset of symptoms, height, weight, and body mass index (BMI), were recorded. Anatomic and pathological characteristics, including the type/grade of labral tears, acetabular and femoral head chondral lesions, gluteus medius tears, and ligamentum teres tears, were measured intraoperatively. Patients were included if they underwent hip arthroscopic surgery for any related abnormality and had a minimum 2-year follow-up. Exclusion criteria were revision arthroscopic surgery, Tönnis grade ≥2, and previous hip conditions (such as Legg-Calves-Perthes disease, avascular necrosis, and prior surgical intervention). Relationships between age and intraoperative findings were identified both in the overall cohort and in younger and older subgroups. An institutional review board approved this study.
Indications for Surgery
A complete physical examination was conducted on all hips before surgery. Anterior impingement test findings were considered positive if pain was elicited in forced flexion combined with internal rotation of the hip.5 Lateral impingement test findings were considered positive if symptoms were produced in forced abduction with external rotation. The evaluation of internal snapping of the iliopsoas tendon was performed as the hip was brought from a flexed, abducted, and externally rotated position into extension with internal rotation.5 Gluteus medius tears were considered positive when there was reduced power on resisted abduction of the hip and tenderness on palpation of the greater trochanter.10 All physical examinations were performed and documented in degrees by the senior surgeon in a clinical setting.
Surgical Technique
All surgical procedures were performed by the senior author (B.G.D.) with the patient in the modified supine position using a minimum of 2 portals (anterolateral and midanterior).6,22 After establishing the portals and capsulotomy site, diagnostic arthroscopic surgery of the hip joint was performed.
Intraoperative Data Collection
A detailed intraoperative data sheet was completed for all patients undergoing hip arthroscopic surgery at our institution. At the time of surgery, the width of the labrum (in mm) was measured using a calibrated 5-mm probe at the anterosuperior, anteroinferior, posterosuperior, and posteroinferior positions of the acetabulum. Labral tears were described using the Seldes classification, in which type 1 tears represent separation at the chondrolabral junction and type 2 tears represent intrasubstance damage.14 The position of the labral tear and acetabular chondral damage were recorded using the clock-face system, in which the notch was defined as 12 o’clock and the midpoint of the transverse ligament was defined as 6 o’clock.16 Using this system, the acetabulum was divided into 4 quadrants: anterosuperior (from 12 o’clock to 3 o’clock), anteroinferior (from 3 o’clock to 6 o’clock), posterosuperior (from 12 o’clock to 9 o’clock), and posteroinferior (from 9 o’clock to 6 o’clock). The middle of the acetabular lesion was defined as the clock-face position halfway between the most anterior and the most posterior extents of the lesion ; the area of the lesion was measured (in cm2). Acetabular chondral lesions were described using the acetabular labrum articular disruption (ALAD)8 and Outerbridge29 classifications, and their topology was measured using the previously described clock-face system.
Surgical Outcome Measurement
All patients undergoing hip arthroscopic surgery were assessed using 4 patient-reported outcome measures: the modified Harris Hip Score (mHHS), Non-Arthritic Hip Score (NAHS), Hip Outcome Score–Activities of Daily Living (HOS-ADL), and Hip Outcome Score–Sport-Specific Subscale (HOS-SSS). All 4 questionnaires were used because it has been reported that there is no conclusive evidence for the use of a single patient-reported outcome questionnaire for patients undergoing hip arthroscopic surgery.24,30 Pain was estimated on a visual analog scale (VAS) from 0 to 10 (10 being the worst). Failure was defined as conversion to total hip arthroplasty, the need for revision hip arthroscopic surgery during the study period, or a change in the NAHS value of <10 points.
Statistical Analysis
In the overall cohort, Pearson correlation was used to identify significant correlations between age and continuous measurements such as the size or position of chondral lesions. Similarly, logistic regression was used to identify significant correlations between age at onset of symptoms and categorical measurements such as the grade of chondral lesions or the presence of loose bodies. The overall cohort was also divided into 2 subgroups. The younger and older groups contained patients with an age below and above the mean age of the overall cohort, respectively. The 2 groups were compared using the Student t test for continuous measurements and the chi-square test for categorical measurements. P values <.05 were considered significant.
Results
From February 2008 to March 2015, there were 1697 patients who met the inclusion criteria. The mean age at onset of symptoms was 34.6 years. The younger group included 825 patients with an age at onset of symptoms less than the overall mean (mean age, 22.2 years), whereas the older group included the remaining 872 patients with an age at onset of symptoms greater than the overall mean (mean age, 46.4 years) (Table 1). Overall, male patients constituted 36.3% of the cohort. Age at onset of symptoms was not related to sex. The mean follow-up was 28.98 months. A significant but weak correlation was found between age and BMI (r = 0.3, P < .0001). While the mean BMI was 25.8 kg/m2 overall, it was 24.4 kg/m2 for patients in the younger group and 27.1 kg/m2 for patients in the older group.
TABLE 1.
Demographic Characteristicsa
| Overall Cohort | Younger Group (Age <34.6 y) | Older Group (Age >34.6 y) | P Value Between Groups | |
|---|---|---|---|---|
| No. of patients | 1697 | 825 | 872 | NA |
| Male sex | 616 (36.30) | 294 (35.64) | 322 (36.93) | .58 |
| Right laterality | 910 (53.62) | 434 (52.61) | 476 (54.59) | .41 |
| Age at onset of symptoms, y | 34.6 (8.4-76.2) | 22.2 (8.4-34.6) | 46.4 (34.6-76.2) | <.0001 |
| Height, inches | 67.3 (41-86) | 67.5 (57-86) | 67.2 (41-84) | .19 |
| Weight, lbb | 167 (79-357) | 159 (79-357) | 174.5 (81-350) | <.0001 |
| BMI, kg/cm2c | 25.8 (13.5-71.1) | 24.4 (13.5-49.8) | 27.1 (13.9-71.1) | <.0001 |
| Subsequent revision arthroscopic surgery | 92 (5.42) | 57 (6.91) | 35 (4.01) | .009 |
aData are presented as n (%) for categorical variables and mean (range) for continuous variables. BMI, body mass index; NA, not applicable.
bPearson r = 0.2.
cPearson r = 0.3.
Significant relationships to age were found in the grade of labral tears and chondral lesions measured intraoperatively. Although the prevalence of labral tears did not significantly differ with age, patients in the younger group had a greater prevalence of Seldes type 1 tears, while patients in the older group had a greater prevalence of Seldes type 1 and 2 tears (P < .0001 for both) (Table 2). The younger group demonstrated a higher prevalence of ALAD grades 0 and 1 and a lower prevalence of grades 2, 3, and 4 compared with the older group (P < .05 for all). Similarly, patients in the younger group had a higher prevalence of acetabular Outerbridge grades 0 and 1 and a lower prevalence of grades 2 and 4 (P < .01). Logistic regression showed significant or near-significant negative correlations between age and the prevalence of ALAD grade 1 or acetabular Outerbridge grade 1 chondral lesions (P = .06 and P = .04, respectively) as well as a near-significant positive correlation between age at onset of symptoms and the prevalence of ALAD grade 4 chondral lesions (P = .06) (Table 2). Patients in the younger group had a higher prevalence of no femoral head chondral damage and a lower prevalence of femoral head chondral damage measured as Outerbridge grades 2, 3, and 4 (P < .05).
TABLE 2.
Classification of Labral Tears, Acetabular Chondral Lesions, and Femoral Head Chondral Lesionsa
| Overall Cohort | P Value of Regressionb | Younger Group | Older Group | P Value Between Groups | |
|---|---|---|---|---|---|
| Labral tear (Seldes) | <.0001 | ||||
| None | 17 (1.00) | .48 | 12 (1.45) | 5 (0.57) | .06 |
| Type 1 | 624 (36.77) | .67 | 380 (46.06) | 244 (27.98) | <.0001 |
| Type 2 | 481 (28.34) | .99 | 218 (26.42) | 263 (30.16) | .13 |
| Types 1 and 2 | 545 (32.12) | .85 | 194 (23.52) | 351 (40.25) | <.0001 |
| Acetabular chondral lesion (ALAD) | <.0001 | ||||
| None | 227 (13.38) | .50 | 131 (15.88) | 96 (11.01) | .003 |
| Grade 1 | 532 (31.35) | .06 | 318 (38.55) | 214 (24.54) | <.0001 |
| Grade 2 | 452 (26.64) | .40 | 201 (24.36) | 251 (28.78) | .04 |
| Grade 3 | 378 (22.27) | .65 | 145 (17.58) | 233 (26.72) | <.0001 |
| Grade 4 | 97 (5.72) | .06 | 25 (3.03) | 72 (8.26) | <.0001 |
| Acetabular chondral lesion (Outerbridge) | <.0001 | ||||
| None | 157 (9.25) | .12 | 106 (12.85) | 51 (5.85) | <.0001 |
| Grade 1 | 572 (33.71) | .04c | 339 (41.09) | 233 (26.72) | <.0001 |
| Grade 2 | 418 (24.63) | .24 | 182 (22.06) | 236 (27.06) | .009 |
| Grade 3 | 263 (15.50) | .14 | 116 (14.06) | 147 (16.86) | .08 |
| Grade 4 | 188 (11.08) | .17 | 44 (5.33) | 144 (16.51) | <.0001 |
| Femoral head chondral lesion (Outerbridge) | <.0001 | ||||
| None | 1293 (76.19) | .01d | 699 (84.73) | 594 (68.12) | <.0001 |
| Grade 1 | 24 (1.41) | .79 | 9 (1.09) | 15 (1.72) | .27 |
| Grade 2 | 82 (4.83) | .20 | 18 (2.18) | 64 (7.34) | <.0001 |
| Grade 3 | 101 (5.95) | .07 | 17 (2.06) | 84 (9.63) | <.0001 |
| Grade 4 | 73 (4.30) | .23 | 21 (2.55) | 52 (5.96) | .0005 |
aData are presented as n (%). ALAD, acetabular labrum articular disruption.
b P values of logistic regression versus age at onset of symptoms.
cLinear coefficient from logistic regression = –0.007.
dLinear coefficient from logistic regression = 0.01.
Furthermore, significant relationships to age were found in the size and position of labral tears and chondral lesions measured intraoperatively. Patients in the older group tended to have larger labral tears based on the clock-face system (Table 3). Compared with patients in the older group, patients in the younger group had labral tears that were 0.9 clock-face hours smaller (P < .0001), acetabular chondral lesions that were 0.3 clock-face hours smaller (P < .0001), and femoral head chondral lesions that were 0.5 clock-face hours larger (P = .008) (Table 3). The area of acetabular chondral lesions also tended to be positively correlated with age (r = 0.2, P < .0001) and was 0.3 cm2 smaller in patients in the younger group compared with patients in the older group (P < .0001). Labral tears and acetabular chondral lesions tended to be centered slightly more posteriorly in younger patients (r = 0.2 and r = 0.09, respectively; P < .0001 for both).
TABLE 3.
Size and Position of Labra, Labral Tears, Acetabular Chondral Lesions, and Femoral Head Chondral Lesionsa
| Overall Cohort | P Value of Regressionb | Younger Group | Older Group | P Value Between Groups | |
|---|---|---|---|---|---|
| Labral width, mm | |||||
| Anterosuperior | 5.0 ± 1.6 | .01 | 4.9 ± 1.5 | 5.1 ± 1.7 | .09 |
| Anteroinferior | 4.8 ± 1.2 | .3 | 4.8 ± 1.2 | 4.8 ± 1.3 | .72 |
| Posterosuperior | 5.2 ± 1.1 | .009 | 5.2 ± 1.0 | 5.3 ± 1.1 | .05 |
| Posteroinferior | 4.3 ± 1.0 | .08 | 4.3 ± 1.0 | 4.4 ± 1.0 | .19 |
| Mean | 4.9 ± 1.1 | .02 | 4.8 ± 1.0 | 4.9 ± 1.1 | .12 |
| Labral tear | |||||
| Clock-face most posterior | 12.1 ± 1.3 | <.0001 | 12.5 ± 1.3 | 11.8 ± 1.3 | <.0001 |
| Clock-face most anterior | 14.8 ± 0.9 | .006 | 14.8 ± 0.8 | 14.9 ± 1.1 | .04 |
| Clock-face center | 13.5 ± 0.9 | <.0001 | 13.7 ± 0.9 | 13.3 ± 0.9 | <.0001 |
| Clock-face range | 2.7 ± 1.3 | <.0001 | 2.3 ± 1.1 | 3.2 ± 1.3 | <.0001 |
| Acetabular chondral lesion | |||||
| Clock-face most posterior | 12.3 ± 0.9 | <.0001 | 12.5 ± 0.8 | 12.2 ± 0.9 | <.0001 |
| Clock-face most anterior | 14.4 ± 0.7 | .3 | 14.4 ± 0.7 | 14.4 ± 0.8 | .21 |
| Clock-face center | 13.4 ± 0.7 | .001 | 13.4 ± 0.6 | 13.3 ± 0.7 | .01 |
| Clock-face range | 2.1 ± 0.9 | <.0001 | 1.9 ± 0.8 | 2.2 ± 0.9 | <.0001 |
| Size, cm2 | 1.1 ± 1.0 | <.0001 | 0.9 ± 0.7 | 1.2 ± 1.2 | <.0001 |
| Femoral head chondral lesion | |||||
| Clock-face most posterior | 10.6 ± 2.6 | .1 | 10.4 ± 1.1 | 10.7 ± 2.9 | .49 |
| Clock-face most anterior | 13.2 ± 1.5 | .1 | 13.6 ± 1.4 | 13.1 ± 1.5 | .04 |
| Clock-face center | 11.9 ± 1.2 | .7 | 12.0 ± 1.1 | 11.8 ± 1.2 | .25 |
| Clock-face range | 2.8 ± 1.3 | .005 | 3.1 ± 1.2 | 2.6 ± 1.3 | .008 |
aData are presented as mean ± SD.
b P values of logistic regression versus age at onset of symptoms.
Significant relationships between age at onset of symptoms and several other intraoperative findings were found. Patients in the younger group had a lower prevalence of <25% gluteus medius tears, 25% to 50% tears, greater than 50% tears, and full tears (P = .2) (Table 4). Patients in the younger group also had a higher prevalence of no ligamentum teres tears and a lower prevalence of grade 1, 2, and 3 tears based on either the percentile4 or Gray and Villar17 classifications (P ≤ .0001) (Table 4). Patients in the younger group had a lower prevalence of notch osteophytes, synovitis, trochanteric bursitis, and loose bodies (P < .05) (Table 4). Logistic regression showed that the prevalence of synovitis was positively correlated with age (P = .01) (Table 4). Patients in the younger group had a higher prevalence of subspine impingement, iliopsoas bursitis, and instability; logistic regression showed that the prevalence of instability was negatively correlated with age (P = –.007).
TABLE 4.
Other Intraoperative Findingsa
| Overall Cohort | Younger Group | Older Group | P Value Between Groups | |
|---|---|---|---|---|
| Dysplasia | 27 (1.59) | 14 (1.70) | 13 (1.49) | .73 |
| Excessive femoral anteversion | 4 (0.24) | 3 (0.36) | 1 (0.11) | .58 |
| Heterotopic ossification | 3 (0.18) | 1 (0.12) | 2 (0.23) | >.99 |
| Iliopsoas bursitis | 260 (15.32) | 155 (18.79) | 105 (12.04) | .0001 |
| Iliopsoas impingement/lesion | 147 (8.66) | 75 (9.09) | 72 (8.26) | .54 |
| Instability/microinstabilityb | 641 (37.77) | 419 (50.79) | 222 (25.46) | <.0001 |
| Loose bodies | 235 (13.85) | 92 (11.15) | 143 (16.40) | .002 |
| Notch osteophytes | 75 (4.42) | 13 (1.58) | 62 (7.11) | <.0001 |
| Subspine impingement | 38 (2.24) | 25 (3.03) | 13 (1.49) | .03 |
| Synovitisc | 210 (12.37) | 77 (9.33) | 133 (15.25) | .0002 |
| Trochanteric bursitis | 216 (12.73) | 37 (4.48) | 179 (20.53) | <.0001 |
| Gluteus medius tear | .2 | |||
| None | 1376 (81.08) | 161 (19.52) | 677 (77.64) | |
| <25% | 13 (0.77) | 3 (0.36) | 10 (1.15) | |
| 25% to 50% | 12 (0.71) | 0 (0) | 12 (1.38) | |
| >50% | 27 (1.59) | 1 (0.12) | 26 (2.98) | |
| Full | 24 (1.41) | 2 (0.24) | 22 (2.52) | |
| Ligamentum teres tear (descriptive classification) | <.0001 | |||
| No tear | 784 (46.2) | 504 (61.09) | 280 (32.11) | |
| Low-grade tear (<50% torn) | 480 (28.29) | 203 (24.61) | 277 (31.77) | |
| High-grade tear (>50% torn) | 334 (19.68) | 88 (10.67) | 246 (28.21) | |
| Full-thickness tear (100% torn) | 76 (4.48) | 19 (2.3) | 57 (6.54) | |
| Ligamentum teres tear (Villar classification) | <.0001 | |||
| None | 781 (46.02) | 501 (60.73) | 280 (32.11) | |
| Grade 1 | 57 (3.36) | 21 (2.55) | 36 (4.13) | |
| Grade 2 | 498 (29.35) | 234 (28.36) | 264 (30.28) | |
| Grade 3 | 320 (18.86) | 50 (6.06) | 270 (30.96) |
aData are presented as n (%).
bLinear coefficient from logistic regression = –0.007.
cLinear coefficient from logistic regression = 0.01.
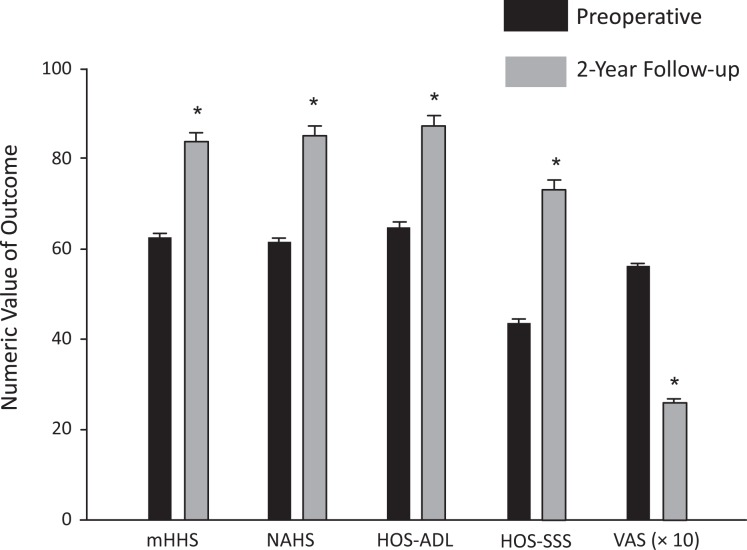
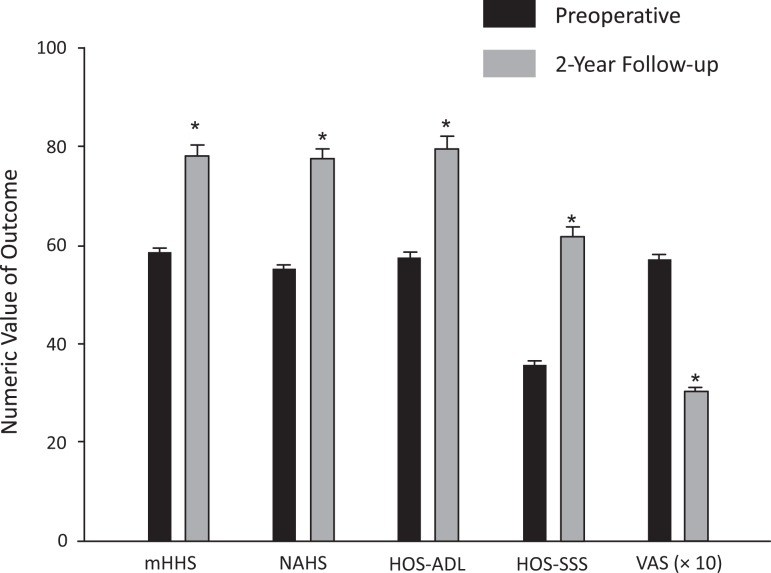
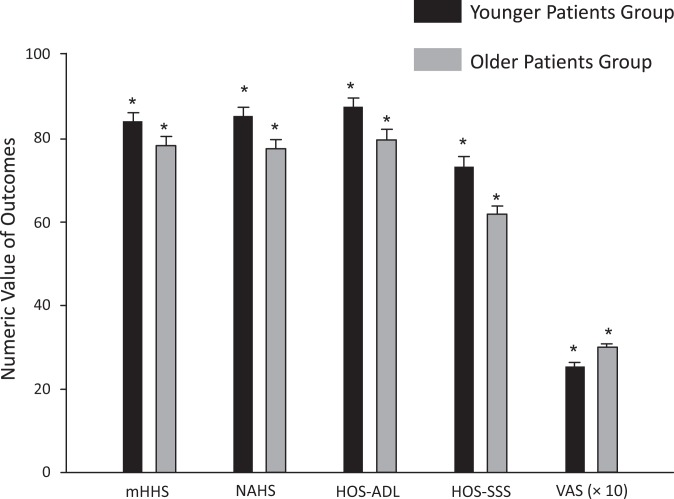
The improvement in scores from preoperatively to 2-year follow-up in the younger group was 62.69 to 83.82 for the mHHS, 64.97 to 87.35 for the HOS-ADL, 43.46 to 73.37 for the HOS-SSS, 63.01 to 85.19 for the NAHS, and 5.61 to 2.53 for pain VAS (Table 5 and Figure 1). Regarding the older group, the improvement in scores from preoperatively to 2-year follow-up was 58.55 to 78.27 for the mHHS, 57.59 to 79.66 for the HOS-ADL, 35.63 to 61.88 for the HOS-SSS, 55.28 to 77.55 for the NAHS, and 5.72 to 3.01 for pain VAS (Table 6 and Figure 2). All scores demonstrated a statistically significant improvement (P ≤ .001) in both groups. Also, when we compared the clinical outcomes after 2-year follow-up between the groups, the results showed that all of the scores were statistically significantly better in the younger group versus the older group (P ≤ .001) (Table 7 and Figure 3).
TABLE 5.
Patient-Reported Outcome Scores for Younger Groupa
| Preoperative | Postoperative | P Value | |
|---|---|---|---|
| mHHS | 62.69 ± 14.93 | 83.82 ± 15.46 | ≤.001 |
| HOS-ADL | 64.97 ± 28.20 | 87.35 ± 43.79 | ≤.001 |
| HOS-SSS | 43.46 ± 25.41 | 73.37 ± 40.75 | ≤.001 |
| NAHS | 63.01 ± 24.23 | 85.19 ± 43.81 | ≤.001 |
| VAS for pain | 5.61 ± 2.55 | 2.53 ± 2.03 | ≤.001 |
aData are presented as mean ± SD. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SSS, Hip Outcome Score–Sport-Specific Subscale; mHHS, modified Harris Hip Score; NAHS, Non-Arthritic Hip Score; VAS, visual analog scale.
Figure 1.
Mean range of patient-reported outcomes in the younger patient group. Error bars represent SDs. *P ≤ .001. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SSS, Hip Outcome Score–Sport-Specific Subscale; mHHS, modified Harris Hip Score; NAHS, Non-Arthritic Hip Score; VAS, visual analog scale for pain.
TABLE 6.
Patient-Reported Outcome Scores for Older Groupa
| Preoperative | Postoperative | P Value | |
|---|---|---|---|
| mHHS | 58.55 ± 15.95 | 78.27 ± 18.10 | ≤.001 |
| HOS-ADL | 57.59 ± 28.12 | 79.66 ± 40.81 | ≤.001 |
| HOS-SSS | 35.63 ± 24.77 | 61.88 ± 30.81 | ≤.001 |
| NAHS | 55.28 ± 17.91 | 77.55 ± 19.36 | ≤.001 |
| VAS for pain | 5.72 ± 2.70 | 3.01 ± 2.23 | ≤.001 |
aData are presented as mean ± SD. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SSS, Hip Outcome Score–Sport-Specific Subscale; mHHS, modified Harris Hip Score; NAHS, Non-Arthritic Hip Score; VAS, visual analog scale.
Figure 2.
Mean range of patient-reported outcomes in the older patient group. Error bars represent SDs. *P ≤ .001. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SSS, Hip Outcome Score–Sport-Specific Subscale; mHHS, modified Harris Hip Score; NAHS, Non-Arthritic Hip Score; VAS, visual analog scale for pain.
TABLE 7.
Patient-Reported Outcome Scores Comparing Both Groups at 2-Year Follow-upa
| Younger Group | Older Group | P Value | |
|---|---|---|---|
| mHHS | 83.82 ± 43.17 | 78.27 ± 40.56 | ≤.001 |
| HOS-ADL | 87.35 ± 43.79 | 79.66 ± 40.81 | ≤.001 |
| HOS-SSS | 73.37 ± 40.75 | 61.88 ± 36.56 | ≤.001 |
| NAHS | 85.19 ± 43.81 | 77.57 ± 40.53 | ≤.001 |
| VAS for pain | 2.53 ± 2.03 | 3.01 ± 2.23 | ≤.001 |
aData are presented as mean ± SD. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SSS, Hip Outcome Score–Sport-Specific Subscale; mHHS, modified Harris Hip Score; NAHS, Non-Arthritic Hip Score; VAS, visual analog scale.
Figure 3.
Mean range of patient-reported outcomes compared between both groups. Error bars represent SDs. *P ≤ .001. HOS-ADL, Hip Outcome Score–Activities of Daily Living; HOS-SSS, Hip Outcome Score–Sport-Specific Subscale; mHHS, modified Harris Hip Score; NAHS, Non-Arthritic Hip Score; VAS, visual analog scale for pain.
Discussion
The results of this study suggest that younger age at onset of symptoms is related to less complex and smaller lesions in both the labrum and the articular cartilage. In addition, older patients tended to have a greater prevalence of gluteus medius injuries, ligamentum teres injuries, notch osteophytes, synovitis, trochanteric bursitis, and loose bodies.
Hip arthroscopic surgery is becoming the preferred surgical method for treating many intra- and extra-articular abnormalities around the hip, including labral tears, chondral injuries, FAI, and loose bodies.6 The treatment of such hip disorders is particularly crucial for hip preservation in young and active patients.22 Several studies have shown an association between labral tears and the early onset of osteoarthritis.37 The presence of osteoarthritis negatively affects improvements in pain and function after hip arthroscopic surgery and open preservation hip surgery.3,38
As such, the correct selection of patients is an important consideration for preoperative planning. Byrd and Jones7 showed that younger patients are more likely to benefit from hip arthroscopic surgery, which prolongs the time until total hip replacement is required. In addition, Haviv and O’Donnell19 found that the interval from primary hip arthroscopic surgery to subsequent total hip arthroplasty was longer in patients younger than 55 years with minimal osteoarthritic changes. Larson et al23 reported a 52% failure rate in patients who underwent hip arthroscopic surgery in the presence of osteoarthritis.
McCormick et al28 evaluated the influence of age and arthritis on hip arthroscopic surgery for labral tears. They found that the presence of osteoarthritic changes at the time of arthroscopic surgery was predictive of worse outcome scores compared with the nonarthritic cohort. In addition, age younger than 40 years was predictive of good to excellent results (odds ratio, 7; 95% CI, 2.9-16.9; P < .0001). In contrast, Domb et al14 showed that patients aged ≥50 years may benefit as much as patients aged ≤30 years for arthroscopic treatment. The current study found that older patients did tend to have worse labral and chondral damage, as well as a greater frequency of several other pathological findings, at the time of surgery.
The outcomes of hip arthroscopic surgery, in relation to age, depend on the extent of arthritic changes. Philippon et al33 suggested using joint space width to predict survivorship and recommended not performing hip preservation surgery in patients who have a joint space below 2 mm. At our institution, we do not perform hip arthroscopic surgery in patients with a Tönnis grade ≥2 or in patients with a joint space of less than 2 mm. However, neither joint space nor Tönnis grade assesses cartilage integrity directly; rather, they offer an indirect assessment of the cartilage.
The issue of patient age is further complicated by the time between the onset of symptoms and treatment. The onset of symptoms is often ambiguous, particularly when the development of symptoms is not preceded by a specific traumatic event. MacDonald et al25 found that in patients who experienced symptoms of osteoarthritis before they were diagnosed, the average time was 7.7 years, and the average age at which people with osteoarthritis had been diagnosed was 50.4 years. In the current study, surgery took place 1.9 years, on average, after the onset of symptoms. Of the overall cohort, 68.9%, 80.1%, and 90.7% of patients underwent surgery less than 2, 3, and 5 years after the onset of symptoms, respectively. Younger and older patients showed no significant differences in the time from the onset of symptoms to surgery.
The effect of patient age on hip arthroscopic surgery is a multifaceted issue that requires further investigation. However, findings have not been entirely consistent, in part because of complicating factors such as the extent of osteoarthritis. The current study sought to provide a context for these previous studies by exploring the differences between younger and older patients in the frequency of various abnormalities that may be identified during surgery. In particular, the large sample size of the current study may make it a valuable resource in contextualizing the results of previous and future investigations.
Limitations
All surgical procedures were performed at a dedicated hip preservation referral center, and the extrapolation of results from one center to another may present challenges. We acknowledge the potential for selection bias but suggest that the large sample size may nevertheless lead toward generalizable trends. Furthermore, we were unable to identify possible confounding factors related to age that may have led to the significant relationships reported in this study. Whether the set of pertinent patient characteristics related with age may be generalized to a population beyond this study cohort is unclear.
Conclusion
Of the multiple intraoperative findings in hip arthroscopic surgery, many are related to age at onset of symptoms. Although we found a statistically significant improvement in clinical outcomes in both groups after 2-year follow-up, apparently the less complex and smaller lesions observed in both the articular cartilage and the labrum in younger patients result in better outcomes compared with older patients.
Acknowledgment
The authors acknowledge Tomas Llano, MD, for his contribution to the statistical analysis of this study and Leslie Yuen for her contribution with the figures.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: B.G.D. is a consultant for Arthrex, Pacira, Amplitude, Medacta, and Stryker and receives royalties from Arthrex, Orthomerica, and DJO Global. The American Hip Institute receives research support from Arthrex, Breg, ATI, Pacira, Stryker, Medacta, and Adventist Hinsdale Hospital.
Ethical approval for this study was obtained from Advocate Health Care (IRB00001341).
References
- 1. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. Bone Joint Surg Br. 2005;87-B(7):1012–1018. [DOI] [PubMed] [Google Scholar]
- 2. Bedi A, Chen N, Robertson W, Kelly BT. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24(10):1135–1145. [DOI] [PubMed] [Google Scholar]
- 3. Bedi A, Kelly BT, Khanduja V. Arthroscopic hip preservation surgery: current concepts and perspective. Bone Joint J. 2013;95-B(1):10–19. [DOI] [PubMed] [Google Scholar]
- 4. Botser IB, Martin DE, Stout CE, Domb BG. Tears of the ligamentum teres: prevalence in hip arthroscopy using 2 classification systems. Am J Sports Med. 2011;39(1):117–125. [DOI] [PubMed] [Google Scholar]
- 5. Byrd JW. Evaluation of the hip: history and physical examination. N Am J Sports Phys Ther. 2007;2(4):231–240. [PMC free article] [PubMed] [Google Scholar]
- 6. Byrd JW. Hip arthroscopy: the supine position. Clin Sports Med. 2001;20:703–731. [PubMed] [Google Scholar]
- 7. Byrd JW, Jones KS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up. Arthroscopy. 2009;25(4):365–368. [DOI] [PubMed] [Google Scholar]
- 8. Callaghan JJ, Rosenberg AG, Rubash HE. The Adult Hip. 2nd ed Philadelphia: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 9. Cates HE, Schmidt MA, Person RM. Incidental “rotator cuff tear of the hip” at primary total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2010;39:131–133. [PubMed] [Google Scholar]
- 10. Chandrasekaran S, Gui C, Hutchinson MR, Lodhia P, Suarez-Ahedo C, Domb BG. Outcomes of endoscopic gluteus medius repair. J Bone Joint Surg Am. 2015;97:1340–1347. [DOI] [PubMed] [Google Scholar]
- 11. Clohisy JC, McClure JT. Treatment of anterior femoroacetabular impingement with combined hip arthroscopy and limited anterior decompression. Iowa Orthop J. 2005;25:164–171. [PMC free article] [PubMed] [Google Scholar]
- 12. Cooper AP, Basheer SZ, Maheshwari R, Regan L, Madan SS. Outcomes of hip arthroscopy: a prospective analysis and comparison between patients under 25 and over 25 years of age. Br J Sports Med. 2013;47(4):234–238. [DOI] [PubMed] [Google Scholar]
- 13. Cormier G, Berthelot JM, Maugars Y. Gluteus tendon rupture is underrecognized by French orthopedic surgeons: results of a mail survey. Joint Bone Spine. 2006;73:411–413. [DOI] [PubMed] [Google Scholar]
- 14. Domb BG, Linder D, Finley Z, et al. Outcomes of hip arthroscopy in patients aged 50 years or older compared with a matched-pair control of patients aged 30 years or younger. Arthroscopy. 2015;31(2):231–238. [DOI] [PubMed] [Google Scholar]
- 15. Fabricant PD, Heyworth BE, Kelly BT. Hip arthroscopy improves symptoms associated with FAI in selected adolescent athletes. Clin Orthop Relat Res. 2012;470(1):261–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed] [Google Scholar]
- 17. Gray AJR, Villar RN. The ligamentum teres of the hip: an arthroscopic classification of its pathology. Arthroscopy. 1997;13(5):575–578. [DOI] [PubMed] [Google Scholar]
- 18. Groh MM, Herrera J. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med. 2009;2(2):105–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Haviv B, O’Donnell J. The incidence of total hip arthroplasty after hip arthroscopy in osteoarthritic patients. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ikeda T, Awaya G, Suzuki S, Okada Y, Tada H. Torn acetabular labrum in young patients: arthroscopic diagnosis and management. J Bone Joint Surg Br. 1988;70-B:13–16. [DOI] [PubMed] [Google Scholar]
- 21. Kamegaya M, Saisu T, Nakamura J, Murakami R, Segawa Y, Wakou M. Drehmann sign and femoro-acetabular impingement in SCFE. J Pediatr Orthop. 2011;31(8):853–857. [DOI] [PubMed] [Google Scholar]
- 22. Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21:1496–1504. [DOI] [PubMed] [Google Scholar]
- 23. Larson CM, Giveans MR, Taylor M. Does arthroscopic FAI correction improve function with radiographic arthritis. Clin Orthop Relat Res. 2011;469(6):1667–1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lodhia P, Slobogean GP, Noonan VK, Gilbart MK. Patient-reported outcome instruments for femoroacetabular impingement and hip labral pathology: a systematic review of the clinimetric evidence. Arthroscopy. 2011;27:279–286. [DOI] [PubMed] [Google Scholar]
- 25. MacDonald KV, Sanmartin C, Langlois K, Marshall DA. Symptom onset, diagnosis and management of osteoarthritis. Health Rep. 2014;25(9):10–17. [PubMed] [Google Scholar]
- 26. Maffulli N, Longo UG, Denaro V. Novel approaches for the management of tendinopathy. J Bone Joint Surg Am. 2010;92:2604–2613. [DOI] [PubMed] [Google Scholar]
- 27. McCarthy J, Barsoum W, Puri L, Lee JA, Steven M, Peter C. The role of hip arthroscopy in the elite athlete. Clin Orthop Relat Res. 2003;406(1):71–74. [DOI] [PubMed] [Google Scholar]
- 28. McCormick F, Nwachukwu BU, Alpaugh K, Martin SD. Predictors of hip arthroscopy outcomes for labral tears at minimum 2-year follow-up: the influence of age and arthritis. Arthroscopy. 2012;28(10):1359–1364. [DOI] [PubMed] [Google Scholar]
- 29. Outerbridge RE. The etiology of chondromalacia patellae: 1961. Clin Orthop Relat Res. 2001;389:5–8. [DOI] [PubMed] [Google Scholar]
- 30. Parvizi J, Campfield A, Clohisy JC, Rothman RH, Mont MA. Management of arthritis of the hip in the young adult. J Bone Joint Surg Br. 2006;88-B(10):1279–1285. [DOI] [PubMed] [Google Scholar]
- 31. Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91-B(1):16–23. [DOI] [PubMed] [Google Scholar]
- 32. Philippon MJ, Ejnisman L, Ellis HB, Briggs KK. Outcomes 2 to 5 years following hip arthroscopy for femoroacetabular impingement in the patients aged 11 to 16 years. Arthroscopy. 2012;28(9):1255–1261. [DOI] [PubMed] [Google Scholar]
- 33. Philippon MJ, Schroder E, Souza BG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy. 2012;28(1):59–65. [DOI] [PubMed] [Google Scholar]
- 34. Philippon MJ, Yen YM, Briggs KK, Kuppersmith DA, Maxwell RB. Early outcomes after hip arthroscopy for femoroacetabular impingement in the athletic adolescent patient: a preliminary report. J Pediatr Orthop. 2008;28(7):705–710. [DOI] [PubMed] [Google Scholar]
- 35. Robertson WJ, Gardner MJ, Barker JU, Boraiah S, Lorich DG, Kelly BT. Anatomy and dimensions of the gluteus medius tendon insertion. Arthroscopy. 2008;24:130–136. [DOI] [PubMed] [Google Scholar]
- 36. Stanton MC, Maloney MD, Dehaven KE, Giordano BD. Acute traumatic tear of gluteus medius and minimus tendons in a patient without antecedant peritrochanteric hip pain. Geriatr Orthop Surg Rehabil. 2012;3:84–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tibor LM, Sekiya JK. Differential diagnosis of pain around the hip joint. Arthroscopy. 2008;24(12):1407–1421. [DOI] [PubMed] [Google Scholar]
- 38. Tijssen M, van Cingel R, van Melick N, de Visser E. Patient-reported outcome questionnaires for hip arthroscopy: a systematic review of the psychometric evidence. BMC Musculoskelet Disord. 2011;12:117. [DOI] [PMC free article] [PubMed] [Google Scholar]