Abstract
Objective:
The aims of this study were to estimate the: (1) 12-mo prevalence of suicidal thoughts, plans, and attempts in a population sample of adolescents and young adults with and without chronic illness; (2) associations among chronic illness and suicidal thoughts and behaviour (STB); and, (3) moderating roles of mood and substance use disorder on this association.
Method:
Individuals were aged 15 to 30 y (n = 5,248) from the Canadian Community Health Survey-Mental Health. Twelve-month STB and psychiatric disorder were measured using the World Health Organization Composite International Diagnostic Interview 3.0. Multinomial logistic regression examined associations between chronic illness and STB, adjusting for relevant sociodemographic and health characteristics. Product term interactions among chronic illness, mood, and substance use disorders were included in the regression models to examine potential moderating effects.
Results:
Prevalence of suicidal thoughts, plans, and attempts was higher in individuals with chronic illness (P < 0.01 for all). After adjustment, chronic illness increased the odds for suicidal thoughts [OR = 1.28 (1.01 to 1.64)], plans [OR = 2.34 (1.22 to 4.39)], and attempts [OR = 4.63 (1.52 to 14.34)]. In the presence v. absence of a mood disorder, the odds for suicidal thoughts were higher among individuals with chronic illness [OR = 1.89 (1.06 to 5.28)].
Conclusions:
Suicidal thoughts and behaviours are common among adolescents and young adults with chronic illness, particularly among those with comorbid mood disorders. Health professionals should routinely ask about STB during assessments of their adolescent and young adult patients.
Keywords: chronic disease, emerging adults, epidemiological study, psychiatric disorder, suicide
Abstract
Objectif:
Cette étude visait à estimer: (1) la prévalence de 12 mois des pensées suicidaires, des plans et des tentatives de suicide dans un échantillon dans la population d’adolescents et de jeunes adultes avec et sans maladie chronique; (2) les associations entre maladie chronique et les pensées et comportements suicidaires (PCS); et (3), les rôles modérateurs du trouble de l’humeur et du trouble d’utilisation de substances dans cette association.
Méthode:
Les sujets étaient âgés de 15 à 30 ans (n = 5 248) et provenaient de l’Enquête sur la santé dans les collectivités canadiennes – Santé mentale. Les PCS et le trouble psychiatrique de 12 mois ont été mesurés à l’aide de l’Entrevue composite diagnostique internationale 3.0. de l’Organisation mondiale de la santé. La régression logistique multinomiale a examiné les associations entre maladie chronique et PCS, en ajustant pour les caractéristiques de santé et sociodémographiques pertinentes. Les interactions du terme produit entre maladie chronique et trouble de l’humeur et d’utilisation de substances étaient incluses dans les modèles de régression pour examiner les effets modérateurs potentiels.
Résultats:
La prévalence des pensées suicidaires, des plans et des tentatives de suicide était plus élevée chez les sujets souffrant de maladie chronique (P < 0,01 pour tous). Après ajustement, la maladie chronique augmentait les probabilités des pensées suicidaires [RC = 1,28 (1,01, 1,64)], des plans [RC = 2,34 (1,22, 4,39)] et des tentatives [RC = 4,63 (1,52, 14,34)] de suicide. En la présence contre l’absence d’un trouble de l’humeur, les probabilités des pensées suicidaires étaient plus élevées chez les sujets souffrant de maladie chronique [RC = 1,89 (1,06, 5,28)].
Conclusions:
Les pensées et les comportements suicidaires sont communs chez les adolescents et les jeunes adultes souffrant de maladie chronique, particulièrement chez ceux qui souffrent de troubles de l’humeur comorbides. Les professionnels de la santé devraient systématiquement s’enquérir des PCS durant l’évaluation de leurs patients adolescents et jeunes adultes.
Among adolescents and young adults, the high prevalence of suicidal thoughts, plans, and attempts is an important public health concern, as these behaviours are strong risk factors for suicide1–4—the second leading cause of death in this population.5 A prospective study found that 13% of adolescents reported suicidal thoughts, and 4% attempted suicide in the past 12 mo.2 As young adults, 6% of these individuals reported a suicide attempt, with 30% reporting repeated attempts.2
Although we know that adolescents and young adults with a chronic illness experience elevated risk for suicidal thoughts and behaviour (STB) as compared with their healthy peers;6–11 important knowledge gaps remain. First, adolescents and young adults with chronic illness are also at increased risk for psychiatric disorder12 but the interrelationships among chronic illness, psychiatric disorder, and STB are not well-understood in this segment of the population. Among adults, the presence of a comorbid psychiatric disorder has a compounding effect on the association between having a chronic illness and suicide.13 However, it is unknown whether these findings translate to STB in adolescents and young adults. Understanding the role of psychiatric disorder in this association can inform universal (population-based) and targeted (clinic-based) prevention strategies for adolescents and young adults. Second, previous studies have focused on lifetime suicide attempts or failed to distinguish between different elements of STB. Using lifetime attempts compromises our ability to examine the temporal relationship between having a chronic illness and its influence on STB. Aggregating elements of STB ignores evidence suggesting that distinct predictors exist for suicidal thoughts, plans, and attempts.1 This has implications for the development of appropriate intervention strategies for young people. Third, although most studies attempt to adjust for covariates that may confound the association between chronic illness and STB, there are examples where relevant variables, such as socioeconomic status, are ignored.7,14,15 A lack of adequate adjustment for potential confounding variables limits the conclusion that can be made on the true association between chronic illness and STB, and, in some instances, result in biased inferences. Fourth, parameters representing these confounders are often not reported, making it difficult to understand the influence relevant covariates have on this association.
This study extends the literature by examining 3 objectives. The first estimates the 12-mo prevalence of suicidal thoughts, plans, and attempts in a population sample of adolescents and young adults aged 15 to 30 y with and without chronic illness. The second quantifies the adjusted associations between chronic illness and STB. The third objective investigates the potential moderating roles of mood and substance use disorders on these associations. We hypothesized that the prevalence of STB would be higher among adolescents and young adults with chronic illness, and that the increased odds for reporting STB among those with chronic illness would remain after adjusting for relevant sociodemographic and health-related covariates. Furthermore, it was hypothesized that mood and substance use disorders would moderate this association such that in the presence v. absence of either comorbid psychiatric disorder, the odds for reporting any STB would be higher among adolescents and young adults with chronic illness.
Method
Data Source
Data were obtained from the 2012 Canadian Community Health Survey-Mental Health (CCHS-MH), a national epidemiological study conducted by Statistics Canada to collect information about the prevalence of psychiatric disorder, functional status, and the use of health services.16 Using multistage, stratified, cluster sampling, a representative sample of respondents ≥15 y of age were enrolled (n = 25,113). Individuals residing in the Canadian territories, Aboriginal reserves, institutions, and full-time members of the Canadian Armed Forces were excluded. Computer-assisted interviews were conducted in respondents’ homes. The combined household and person response was 69%.16 We restricted the sample to participants aged 15 to 30 y (n = 5,248) to capture the developmental period of adolescence and young adulthood. Participation in the CCHS-MH is voluntary and confidentiality is guaranteed by Statistics Canada. Analyses were approved by the Hamilton Integrated Research Ethics Board.
Measures
The presence of lifetime chronic illness was assessed using a standard checklist that asked participants if they had been diagnosed by a health professional with a long-term health condition that had lasted or was expected to last ≥6 months. The conditions were: asthma (n = 622), arthritis (n = 118), back problems (not including fibromyalgia, arthritis; n = 551), high blood pressure (n=76), migraine headache (n = 641), chronic bronchitis/emphysema/chronic obstructive pulmonary disease (n = 0), diabetes (n = 38), epilepsy (n = 43), heart disease (n = 29), cancer (n = 14), effects of a stroke (n = 6), bowel disease (inflammatory bowel disease, Crohn’s disease, ulcerative colitis; n = 129), Alzheimer’s disease/dementia (n = 0), chronic fatigue syndrome (n = 24), and multiple chemical sensitivities (n = 62). These illnesses were categorized according the International Classification of Disease 10th Revision (ICD-10) to examine class-specific effects.17 Individuals with cancer only (n = 14) were excluded, because they were too few. Those with other conditions (n = 464) were excluded, because respondents may have interpreted this question to include psychiatric illnesses and ICD-10 classifications could not be assigned. Healthy controls were participants who did not endorse any chronic illness. This case ascertainment strategy resulted in 32.8% (n = 1,721) of participants having ≥1 chronic illness and 67.2% (n = 3,527) of participants as healthy controls.
Twelve-month suicidal thoughts, plans, and attempts were measured using the Suicide sub-block of the World Health Organization (WHO) version of the Composite International Diagnostic Interview (CIDI) 3.0.18 Participants were asked whether they had the following experiences in the 12 mo immediately before the interview: thoughts (‘You seriously thought about committing suicide or taking your own life?’); plans (‘You made a plan for committing suicide?’); and, attempts (‘You attempted suicide or tried to take your own life?’). The reliability and validity of the CIDI are well established,18,19 including the assessment of STB.20
The CIDI was also used to classify participants for psychiatric disorders in the 12 mo immediately before the interview, according to the Diagnostic and Statistical Manual of Mental Disorders IV-TR and ICD-10.18 Within the CCHS-MH, the mood disorders measured were major depressive episode, bipolar disorder, and generalized anxiety disorder; and substance use disorders were alcohol, cannabis, and other drugs.16 Mood disorders were collapsed into a single variable in the analyses, as were the substance use disorders. This approach was implemented to minimize potential analytical issues associated with sparse data. Our aim in this manuscript was to isolate the effect of chronic illness on reports of STB among adolescents and young adults. Given robust evidence that physical and mental health problems are highly comorbid in young people,12,21 and that psychiatric disorder is strongly associated with STB,1,2 psychiatric disorder was determined to be an important confounder in our analyses.
Covariates were included in the analyses, as they have been shown to confound the association between chronic illness and STB. These were: participant age and sex, immigrant status (born/not born in Canada), residence (urban/rural), educational attainment, annual household income (<$20 000 to ≥$150 000 in $20 000 increments), smoking status (never, former, occasional, daily), disability (WHO Disability Assessment Schedule 2.0),22 and number of chronic illnesses.
Analysis
Sampling weights based on the probabilities of selection and participation were used to ensure comparability between the sample and the Canadian population, and were applied to all analyses. Taylor Series Linearization was used to adjust variance estimates due to the complex sampling for the CCHS-MH. Missed responses were not associated with key variables and too few (0.2% for STB and 2.1% for any of the covariates) to influence parameter estimates; thus, these cases were excluded from the analysis. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were computed from multinomial logistic regressions that examined associations between chronic illness and STB. Suicidal thoughts, plans, and attempts were coded to represent a cumulative response scale (each STB was a mutually exclusive categorical outcome). Participants who endorsed more than one STB were coded as having a more extreme behaviour (thoughts < plans < attempts). Product-term interactions among chronic illness and mood and substance use disorders were included to examine potential moderating effects. Main effects were included in models containing product-term interactions.23
Results
Sample Characteristics
The characteristics of the sample are detailed in Table 1. Participants had a mean age of 22.4 (0.1) y, 47.0% were female, 20.0% were immigrants, 43.8% completed post-secondary education, and 30.2% reported annual household incomes of ≥$100,000.
Table 1.
Sociodemographic characteristics of the study sample.
| Healthy controls | Chronic illness | t / χ2 (P value) | |
|---|---|---|---|
| Age, y [mean (SE)] | 22.4 (0.1) | 22.6 (0.2) | 0.14 (0.89) |
| Female | 1,580 (44.8) | 885 (51.4) | 10.43 (<0.01) |
| Immigrant | 839 (23.9) | 212 (12.3) | 37.44 (<0.01) |
| Urban resident | 3,068 (87.0) | 1,490 (86.6) | 0.12 (0.73) |
| Educational attainment | 9.98 (0.02) | ||
| Primary school | 800 (22.7) | 441 (25.6) | |
| Secondary school | 640 (18.2) | 310 (18.0) | |
| Some post- secondary school | 464 (13.2) | 282 (16.4) | |
| Post-secondary graduate | 1,613 (45.9) | 688 (40.0) | |
| Household income | 25.90 (<0.01) | ||
| ≤$19,999 | 298 (8.0) | 201 (11.7) | |
| $20-$39,999 | 570 (15.3) | 318 (18.5) | |
| $40-$59,999 | 624 (16.7) | 296 (17.2) | |
| $60-$79,999 | 624 (16.8) | 272 (15.8) | |
| $80-$99,999 | 461 (12.4) | 198 (11.5) | |
| $100-$149,999 | 656 (17.6) | 275 (16.0) | |
| ≥$150,000 | 493 (13.2) | 160 (9.3) |
Estimates are reported as n (percentage), except for participant age.
Major depressive episode, bipolar disorder, and generalized anxiety disorder (mood disorders) were found in 6.0%, 2.1%, and 2.6% of the sample, respectively. Alcohol, cannabis, or other drug disorders (substance use disorders) were found in 7.2%, 3.7%, and 1.6%, respectively. Comorbid mood disorders were found in 1.9%, comorbid substance use disorders in 2.0%, and comorbid mood-substance use disorders in 1.9% of the participants. Nearly one-third (29.2%) had multiple chronic illnesses.
As a group, participants with a chronic illness were more likely to identify as female, be non-immigrants, and of lower socioeconomic status, as indicated by lower educational attainment and lower household income, as compared with controls (Table 1). Participants with a chronic illness, as a group or stratified by ICD-10 category, had increased odds of reporting any mood disorder, other drug disorder, comorbid mood disorders, and comorbid mood-substance use disorders, as compared with controls (Table 2). There were no differences in the proportions of psychiatric disorder across ICD-10 categories (Table 2), supporting our method of aggregating chronic illnesses into a single group (non-categorical approach).24
Table 2.
Psychiatric characteristics of the study sample.
| χ2 (P value) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Healthy controls | All chronic illness | Respiratory | Musculoskeletal | Cardiovascular | Neurological | Endocrine | Test A | Test B | Test C | |
| Mood disorders | ||||||||||
| Major depressive episode | 141 (3.8) | 186 (10.9) | 66 (10.6) | 73 (11.8) | 20 (18.9) | 83 (12.2) | 31 (19.1) | 45.43 (<0.01) | 52.80 (<0.01) | 6.10 (0.19) |
| Bipolar disorder | 42 (1.1) | 72 (4.2) | 22 (3.6) | 30 (7.7) | 10 (9.3) | 44 (6.6) | 7 (4.3) | 22.06 (<0.01) | 47.64 (<0.01) | 8.86 (0.07) |
| Generalized anxiety | 37 (1.0) | 102 (5.9) | 36 (5.9) | 47 (7.6) | 13 (12.5) | 51 (7.4) | 14 (8.5) | 67.26 (<0.01) | 65.61 (<0.01) | 3.09 (0.54) |
| Substance use disorder | ||||||||||
| Alcohol | 257 (6.9) | 131 (7.7) | 56 (9.1) | 60 (9.9) | 6 (6.3) | 32 (4.7) | 15 (8.9) | 0.50 (0.48) | 9.78 (0.08) | 8.82 (0.07) |
| Cannabis | 121 (3.3) | 79 (4.7) | 24 (4.0) | 33 (5.4) | 6 (6.3) | 35 (5.1) | 11 (6.7) | 3.15 (0.08) | 5.49 (0.36) | 1.52 (0.82) |
| Other drug | 45 (1.2) | 102 (5.9) | 12 (1.9) | 19 (3.2) | -- | 19 (2.8) | 11 (6.7) | 4.80 (0.03) | 19.32 (<0.01) | 9.26 (0.06) |
| No. psychiatric disorder | ||||||||||
| Comorbid mood | 31 (0.8) | 80 (4.7) | 26 (4.3) | 35 (5.6) | 11 (10.4) | 43 (6.3) | 7 (4.0) | 36.49 (<0.01) | 44.23 (<0.01) | 1.95 (0.75) |
| Comorbid substance | 69 (1.8) | 42 (2.9) | 14 (2.2) | 21 (3.4) | -- | 13 (1.9) | 11 (6.4) | 1.02 (0.31) | 10.72 (0.06) | 8.38 (0.08) |
| Comorbid mood and substance | 36 (1.0) | 66 (3.8) | 29 (4.7) | 26 (4.1) | -- | 24 (3.5) | 14 (8.6) | 19.52 (<0.01) | 37.70 (<0.01) | 7.70 (0.10) |
Group-specific estimates of psychiatric disorder for participants with chemical sensitivities were excluded from the table because low cell counts resulted in data suppression according to the guidelines established by Statistics Canada. However, χ2 tests with the chemical sensitivity group included were similar to those reported in the table.
Test A is the comparison between healthy controls and all chronic illnesses; Test B is the comparison across healthy controls and the ICD-10 illness categories; Test C is the comparison across the ICD-10 illness categories.
Prevalence of STB
Overall, 381 (7.3%) participants reported any STB. Of these, 373 (97.8%) had thoughts, 119 (31.2%) had plans, and 49 (12.9%) had attempts. Among those with suicidal thoughts, 235 (63.1%) did not have plans or attempts, and 81 (68.6%) of those with plans did not attempt suicide. Among those who attempted suicide, 22 (43.9%) were unplanned. Suicidal thoughts, plans, and attempts were more commonly reported among participants with chronic illness compared to controls (8.4%, 3.0%, 2.0% v. 2.6%, 0.7%, 0.2%, respectively). This translated into unadjusted ORs of 3.43 (2.61 to 4.54) for thoughts, 4.36 (2.65 to 7.37) for plans, and 10.13 (4.48 to 22.91) for attempts.
Chronic Illness and STB
After adjustment, participants with chronic illness had increased odds for suicidal thoughts [OR = 1.28 (0.99 to 1.64)], plans [OR = 2.34 (1.23 to 4.39)], and attempts [OR = 4.63 (1.52 to 14.34)]. Psychiatric disorders were also strongly associated with each STB (Table 3).
Table 3.
Adjusted associations between chronic illness and suicidal behaviour.
| Thoughts | Plans | Attempts | |
|---|---|---|---|
| Chronic illness | 1.28 (1.01 to 1.64) | 2.34 (1.23 to 4.39) | 4.63 (1.52 to 14.34) |
| No. chronic illnesses | 2.60 (1.51 to 4.44) | 4.45 (2.40 to 8.25) | 7.11 (2.75 to 18.29) |
| Mood disorder | 5.72 (3.08 to 10.60) | 10.73 (5.45 to 21.12) | 40.60 (15.13 to 88.97) |
| Substance use disorder | 2.88 (1.72 to 4.80) | 5.75 (2.68 to 12.34) | 14.57 (5.16 to 39.15) |
| Age, y | 0.99 (0.93 to 1.05) | 0.93 (0.85 to 1.02) | 0.93 (0.83 to 1.05) |
| Female sex | 0.74 (0.48 to 1.15) | 0.69 (0.35 to 1.36) | 0.70 (0.25 to 1.93) |
| Immigrant | 0.98 (0.49 to 1.94) | 0.90 (0.25 to 3.26) | 2.31 (0.75 to 7.05) |
| Urban residence | 1.39 (0.77 to 2.53) | 2.57 (0.99 to 6.71) | 4.08 (0.98 to 16.95) |
| Educational attainment | 0.87 (0.71 to 1.06) | 0.76 (0.56 to 1.04) | 0.62 (0.40 to 0.98) |
| Household income | 0.95 (0.86 to 1.05) | 0.95 (0.79 to 1.14) | 0.88 (0.69 to 1.13) |
| Smoking status | 1.02 (0.85 to 1.22) | 1.18 (0.92 to 1.53) | 1.54 (1.07 to 2.23) |
| Disability | 1.04 (1.01 to 1.06) | 1.05 (1.02 to 1.07) | 1.02 (0.99 to 1.05) |
Results are reported as ORs (95% CI) and those in bold are statistically significant. Having no suicidal thoughts, plans, or attempts was the reference category. The model adjusted for all listed variables.
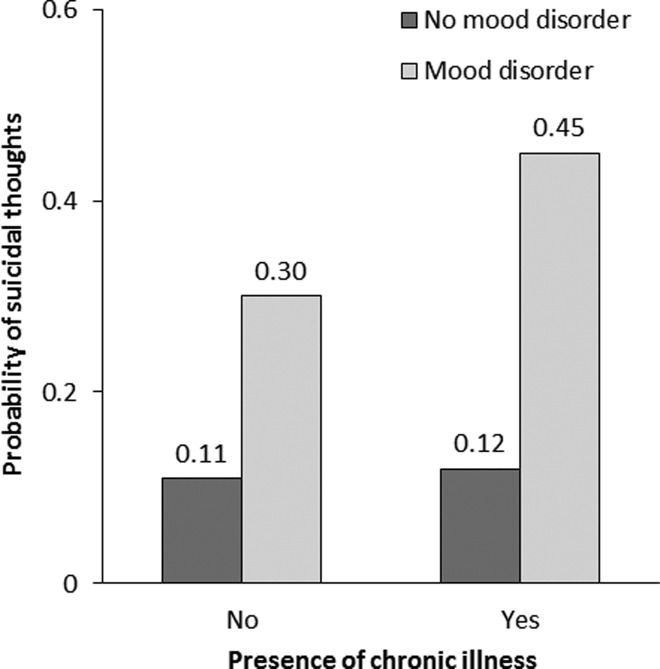
One significant interaction was found, showing that mood disorder moderated the association between chronic illness and suicidal thoughts [Table 4; OR = 1.89 (1.06 to 5.28)]. This suggested that whereas the probability of reporting suicidal thoughts was low and stable for participants without mood disorder regardless of their health status, the probability increased significantly for participants with mood disorder and chronic illness as compared with those with mood disorder and no chronic illness (Figure 1). No other moderating effects were found.
Table 4.
Moderating effects of comorbid psychiatric disorder on suicidal behaviour.
| Thoughts | Plans | Attempts | |
|---|---|---|---|
| Mood disorder | 1.89 (1.06, 5.28) | 0.68 (0.17, 2.76) | 1.06 (0.40, 6.55) |
| Substance use disorder | 1.92 (0.50, 7.38) | 0.73 (0.28, 1.93) | 1.52 (0.39, 8.14) |
Results are reported as ORs (95% CI) and those in bold are statistically significant. Having no suicidal thoughts, plans, or attempts was the reference category. Product-term interactions between having a chronic illness and mood or substance use disorder were included in the adjusted multinomial logistic regression model.
Figure 1.
Moderating effect of mood disorder on the association between having a chronic illness and suicidal thoughts.
Discussion
Summary
The findings confirm the increased odds of STB among adolescents and young adults with a chronic illness as compared with their healthy peers.6–10,25,26 Our prevalence estimates and measures of association with STB among adolescents and young adults with a chronic illness, although consistent with some studies,2,27 are lower than other population-based studies of young people with and without various chronic illnesses.8,25,28,29 These discrepancies are likely attributable to differences in study location, age of respondents (sampling), measurement, and covariate selection.
Whereas 2 of the studies that reported similar estimates were conducted in Canada,2,27 those with higher estimates were conducted elsewhere—United States, Europe, and New Zealand.8,28,29 Our study included a wider age range of adolescents and young adults as compared with previous work, which typically studied only older adolescents. Evidence suggests that the prevalence of STB and depression (which captures aspects of STB) is highest in late adolescence,8,30,31 which may partly contribute to differences in estimates.
Regarding measurement, we used the validated CIDI to assess 12-mo STB, contrasting with previous studies that used generic questions of lifetime STB. Although similar in their delivery to participants, generic questions of STB have not undergone extensive psychometric testing to ensure accuracy. These methodological differences can result in findings that are inconsistent and may limit comparisons across samples. The paucity of studies specifically examining associations between chronic illness and STB among adolescents and young adults signals the need for more research in this vulnerable population. This is particularly relevant given that approximately 1 in 10 participants in our study reported STB.
To isolate the association between chronic illness and STB, several covariates were modelled, including the presence of comorbid mood or substance use disorders. The interrelations among chronic illness, psychiatric disorder, and STB may represent a causal pathway. That is, having a chronic illness increases the risk for the development of psychiatric disorder, which in turn, increases the risk for STB. Such mediational pathways cannot be rigorously tested using cross-sectional data from the CCHS-MH. However, if such a pathway exists, the inclusion of psychiatric disorder would further attenuate the association between chronic illness and STB.
Noteworthy were the independent associations between several covariates and STB. First, the association between the number of chronic illnesses and STB mirrored that of our exposure of interest—presence of chronic illness—in that associations strengthened across the severity of STB. Second, the protective effect of socioeconomic advantage (indicated by educational attainment) was less prominent in our sample.1,32 This suggests that, in the context of having a chronic illness and adjusting for related factors (number of chronic illnesses, disability), socioeconomic status may be less influential in reports of STB among adolescents and young adults. Third, evidence for an association between smoking status and suicide attempts contributes to the converging knowledge base that smoking is a robust correlate of STB.33 Smoking prevention and cessation efforts for adolescents and young adults with chronic illness may be helpful in reducing the odds of STB. Fourth, the level of disability was also found to be associated with STB and may reflect dependency or social isolation caused by having a chronic illness.34 Interventions aimed at reducing the impact of disability on life activities for young people with chronic illness may prove beneficial in reducing STB.
The moderating effect of mood disorder on the association between chronic illness and suicidal thoughts is a novel finding. Although previous studies have noted a detrimental compounding effect of having physical–psychiatric comorbidity,8,10 no one has quantified this interaction. This finding is relevant because it suggests that adolescents and young adults with a chronic illness and comorbid psychiatric disorders might be the focus for targeted preventive interventions to reduce the incidence of suicidal thoughts, diminishing the odds of future suicide attempts.1–3
We speculate that adolescents and young adults with comorbid chronic illness and psychiatric disorders may not be accessing appropriate psychiatric services, which in turn increase their odds of STB. This finding may appear counter-intuitive given that adolescents and young adults with chronic illnesses often have regular contact with the health system, thus increasing the probability that their thoughts of suicide would be identified by a health professional. However, for adolescents and young adults with a chronic illness, the medical encounter may not provide adequate time to assess mental health, including suicidal thoughts.
While the notion that there is no health without mental health is becoming more pervasive,35 the physical and mental health systems remain segregated, and consultation-liaison psychiatric services are an exception rather than the norm, particularly in primary care. Furthermore, the age of our sample encompasses the time of transition from paediatric to adult health services, which may further impede access to appropriate psychiatric or supportive services, thereby predisposing adolescents and young adults with a chronic illness to STB.
The absence of other moderating effects is likely attributable to the low prevalence of suicidal plans and suicide attempts and, thus, the low statistical power to detect these effects in this sample. We encourage more research aimed at identifying these potential moderating effects.
Implications
Evidence from this and other studies demonstrates the consistency in the magnitude of effects across different chronic illnesses and STB.6,9,10,26 The elevated odds of STB among adolescents and young adults with a chronic illness calls attention to the need to address this problem in this vulnerable population. Given the robust evidence of the association between psychiatric disorder and STB, health professionals should be attuned to the signs and symptoms of psychiatric disorder among adolescents and young adults and inquire about STB more directly if patients present with these signs and symptoms in practice. Adolescents and young adults who are not currently being supported by a mental health practitioner and who disclose STB or significant shifts in their mental health should be immediately referred for a comprehensive psychiatric assessment and support. Efforts should be redoubled for those with chronic illness. Evidence suggests that risk for suicide attempts is highest soon after young people are diagnosed with a chronic illness,6,36 suggesting a critical window of opportunity for prevention and continued monitoring.
It is important, therefore, that health professionals working with adolescents and young adults with a chronic illness are knowledgeable about appropriate responses and referral sources when inquiring about STB, and have an awareness of the potential impact of prescribed medications for chronic illness on suicide risk.37,38 With evidence consistently showing health declines for individuals with chronic illness during the transition from paediatric to adult health services30,39,40—which may precipitate STB—it would be important to determine if assessing for suicidal risk plus referral to appropriate psychiatric or allied health services results in reduced STB within clinical settings.41,42
The adoption of mental health modules within transition programs may be useful in supporting adolescents and young adults with chronic illness to reduce STB. In addition to in-clinic sessions that aim to identify psychiatric disorder and STB, partnerships with community-based agencies can be established to provide access to support groups that promote healthy behaviours and social participation. Multipronged approaches to reduce suicide risk will have the greatest public health impact.43
Future Directions
Our findings strengthen knowledge about the elevated risk for STB among adolescents and young adults with a chronic illness and provide investigators a solid foundation to further this research agenda with longitudinal studies during this important developmental period in the life-course. Methodologically robust longitudinal studies are needed to understand the temporal effects and interrelationships among chronic illness, psychiatric disorder, and STB. In addition to examining main and moderating effects, it is prudent that investigators also consider potential mediating effects of mood and substance use disorder. There is considerable evidence linking chronic illness to mood disorders, such as depression,12,21 as well as the association between mood disorders and STB.1,44 However, the extent to which mood or substance use disorders mediate the relationship between chronic illness and STB in adolescents and young adults, as well as the magnitude of these potential mediating effects, remain unknown. Evidence of causal relationships among these variables can inform the level (i.e., primary or secondary prevention), target, and type of intervention to implement to reduce the incidence of STB, and perhaps, deaths by suicide. Finally, investigators must prioritize the development and evaluation of interventions—both targeted interventions and broad risk-reduction approaches—for this vulnerable population.
Strengths and Limitations
The notable strengths of this study are: a large representative sample of adolescents and young adults; objective assessments of 12-mo suicidal thoughts, plans, and attempts rather than lifetime STB, as well as 12-mo mood and substance use disorders; inclusion of a large number of relevant covariates to present unbiased estimates of association; and, an examination of moderating effects to determine the extent to which associations between chronic illness and STB are augmented by mood or substance use disorder.
These strengths must be considered within the following limitations. First, chronic illnesses were self-reported. This can be problematic for chronic illness with very low prevalence45 leading to misclassification and attenuation of our measures of association. However, empirical evidence suggests that this bias is negligible.46 Second, symptoms of STB (e.g., thoughts of self-harm) also informed the classification of major depressive episode in the CCHS-MH, which may overestimate the association between mood disorder and STB. Third, sparse data precluded the examination of moderating effects of specific mood or substance use disorders on specific chronic illnesses; however, the non-categorical approach employed in this study is valid in generating relevant findings for clinic and population-based samples.24 Fourth, the temporal order of variables could not be verified. Fifth, participants coded as not having a psychiatric disorder may have screened positive for other disorders not measured by CIDI in the CCHS-MH (e.g., psychosis, post-traumatic stress). Sixth, social desirability bias may have resulted in under-reporting of STB, thereby leading to underestimated effects. Seventh, relevant covariates, such as experiences of maltreatment or parental psychopathology,3 were either asked of a subset of participants or not included in the CCHS-MH and could not be adjusted for in our models.
Conclusions
Our findings strengthen knowledge about the elevated odds for STB among adolescents and young adults with chronic illness, as well as the differential effects for those with and without comorbid mood disorders, and provide a solid foundation for longitudinal studies during this period of life. Such studies could examine mediating effects of psychiatric disorder, and whether the moderating effects reported in this study can be replicated. This information would help to understand aetiology, and develop and evaluate intervention strategies—both targeted and universal—to reduce STB for this vulnerable population. Mental health and STB are often overshadowed during medical encounters for chronic illness. However, health professionals involved in the care of adolescents and young adults must be vigilant in assessing STB and being prepared to respond to patient disclosures of suicidal thoughts, plans, and attempts.
Acknowledgments
We would like to thank the Research Data Centres Program at Statistics Canada for providing access to the data. Although the research and analyses are based on data from Statistics Canada, the opinions expressed do not represent the views of Statistics Canada.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Ferro is a member of the Editorial Board for the Canadian Journal of Psychiatry. None of the remaining authors have any conflict of interest to disclose. Findings from this manuscript were presented by Dr. Ferro at the 2016 Section Meeting in Epidemiology and Social Psychiatry of the European Psychiatric Association in Gothenburg, Sweden.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: At the time the research was conducted, Dr. Ferro was supported by the Research Early Career Award from Hamilton Health Sciences. Dr. Ferro currently holds the Canada Research Chair in Youth Mental Health from the Canadian Institutes of Health Research (CIHR) and Early Researcher Award from the Ontario Ministry of Research, Innovation and Science. Dr. Kimber is supported by an Ontario Ministry of Health and Long-Term Care Women’s Health Scholar Post-Doctoral Fellowship; Dr. Boyle by the Canada Research Chair in the Social Determinants of Child Health; Dr. Georgiades by a CIHR New Investigator Award and the David R. (Dan) Offord Chair in Child Studies; and, Dr. MacMillan by the Chedoke Health Chair in Child Psychiatry.
References
- 1. Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Brezo J, Paris J, Barker ED, et al. Natural history of suicidal behaviors in a population-based sample of young adults. Psychol Med. 2007;37(11):1563–1574. [DOI] [PubMed] [Google Scholar]
- 3. Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry. 2006;47(3-4):372–394. [DOI] [PubMed] [Google Scholar]
- 4. MacKinnon N, Colman I. Factors associated with suicidal thought and help-seeking behaviour in transition-aged youth versus adults. Can J Psychiatry. 2016;61(12):789–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization. Preventing suicide: a global imperative Geneva (CH): World Health Organization; 2014. [Google Scholar]
- 6. Butwicka A, Frisen L, Almqvist C, et al. Risks of psychiatric disorders and suicide attempts in children and adolescents with type 1 diabetes: a population-based cohort study. Diabetes Care. 2015;38(3):453–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. van Tilburg MA, Spence NJ, Whitehead WE, et al. Chronic pain in adolescents is associated with suicidal thoughts and behaviors. J Pain. 2011;12(10):1032–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Barnes AJ, Eisenberg ME, Resnick MD. Suicide and self-injury among children and youth with chronic health conditions. Pediatrics. 2010;125(5):889–895. [DOI] [PubMed] [Google Scholar]
- 9. Scott KM, Hwang I, Chiu WT, et al. Chronic physical conditions and their association with first onset of suicidal behavior in the world mental health surveys. Psychosom Med. 2010;72(7):712–719. [DOI] [PubMed] [Google Scholar]
- 10. Goodwin RD, Marusic A, Hoven CW. Suicide attempts in the United States: the role of physical illness. Soc Sci Med. 2003;56(8):1783–1788. [DOI] [PubMed] [Google Scholar]
- 11. Bandiera FC, Ramirez R, Arheart KL, Canino G, Goodwin RD. Asthma and suicidal ideation and behavior among Puerto Rican older children and adolescents. J Nerv Ment Dis. 2013;201(7):587–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ferro MA. Major depressive disorder, suicidal behaviour, bipolar disorder, and generalised anxiety disorder among emerging adults with and without chronic health conditions. Epidemiol Psychiatr Sci. 2016;25(5):462–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Qin P, Hawton K, Mortensen PB, et al. Combined effects of physical illness and comorbid psychiatric disorder on risk of suicide in a national population study. Br J Psychiatry. 2014;204(6):430–435. [DOI] [PubMed] [Google Scholar]
- 14. Miauton L, Narring F, Michaud PA. Chronic illness, life style and emotional health in adolescence: results of a cross-sectional survey on the health of 15-20-year-olds in Switzerland. Eur J Pediatr. 2003;162(10):682–689. [DOI] [PubMed] [Google Scholar]
- 15. Gili-Planas M, Roca-Bennasar M, Ferrer-Perez V, et al. Suicidal ideation, psychiatric disorder, and medical illness in a community epidemiological study. Suicide Life Threat Behav. 2001;31(2):207–213. [DOI] [PubMed] [Google Scholar]
- 16. Statistics Canada. Canadian Community Health Survey (CCHS) - Mental Health User guide: microdata files. Ottawa (Canada): Statistics Canada; 2013. [Google Scholar]
- 17. International statistical classification of diseases and related health problems. World Health Organization, 2010. [Cited 2016 Nov 25]. Available from: http://apps.who.int/classifications/icd10/browse/2010/en.
- 18. Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res. 2004;13(2):93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kessler RC, Abelson J, Demler O, et al. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI). Int J Methods Psychiatr Res. 2004;13(2):122–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Christl B, Wittchen HU, Pfister H, et al. The accuracy of prevalence estimations for suicide attempts. how reliably do adolescents and young adults report their suicide attempts? Arch Suicide Res. 2006;10(3):253–263. [DOI] [PubMed] [Google Scholar]
- 21. Merikangas KR, Calkins ME, Burstein M, et al. Comorbidity of physical and mental disorders in the neurodevelopmental genomics cohort study. Pediatrics. 2015;135(4):e927–e938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Üstün TB, Kostanjsek N, Chatterji S, et al. , Measuring health and disability: manual for WHO Disability Assessment Schedule: WHODAS 2.0 Geneva (CH): World Health Organization; 2010. [Google Scholar]
- 23. Vittinghoff E, Glidden DV, Shiboski SC, et al. Regression methods in biostatistics Linear, logistic, survival, and repeated measures models. New York (NY): Springer; 2005. [Google Scholar]
- 24. Stein RE, Bauman LJ, Westbrook LE, et al. Framework for identifying children who have chronic conditions: the case for a new definition. J Pediatr. 1993;122(3):342–347. [DOI] [PubMed] [Google Scholar]
- 25. Steinberg L, Aldea I, Messias E. Asthma, depression, and suicidality: results from the 2007, 2009, and 2011 youth risk behavior surveys. J Nerv Ment Dis. 2015;203(9):664–669. [DOI] [PubMed] [Google Scholar]
- 26. Crump C, Sundquist K, Sundquist J, et al. Sociodemographic, psychiatric and somatic risk factors for suicide: a Swedish national cohort study. Psychol Med. 2014;44(2):279–289. [DOI] [PubMed] [Google Scholar]
- 27. Swanson SA, Colman I. Association between exposure to suicide and suicidality outcomes in youth. CMAJ. 2013;185(10):870–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kokkevi A, Rotsika V, Arapaki A, et al. self-reported suicide attempts, self-harm thoughts and their correlates across 17 European countries. J Child Psychol Psychiatry. 2012;53(4):381–389. [DOI] [PubMed] [Google Scholar]
- 29. Fergusson DM, Woodward LJ, Horwood LJ. Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychol Med. 2000;30(1):23–39. [DOI] [PubMed] [Google Scholar]
- 30. Ferro MA, Gorter JW, Boyle MH. Trajectories of depressive symptoms during the transition to young adulthood: the role of chronic illness. J Affect Disord. 2015;174:594–601. [DOI] [PubMed] [Google Scholar]
- 31. Ferro MA, Gorter JW, Boyle MH. Trajectories of depressive symptoms in Canadian emerging adults. Am J Public Health. 2015;105(11):2322–2327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Poorolajal J, Darvishi N. Smoking and suicide: a meta-analysis. PLoS One. 2016;11(7):e0156348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Burcu E. Disability and youth suicide: a focus group study of disabled university students. Rev Disabil Studies. 2014;3:299. [Google Scholar]
- 35. Prince M, Patel V, Saxena S, et al. Global mental health 1 - No health without mental health. Lancet. 2007;370(9590):859–877. [DOI] [PubMed] [Google Scholar]
- 36. Christiansen E, Stenager E. Risk for attempted suicide in children and youths after contact with somatic hospitals: a Danish register based nested case-control study. J Epidemiol Community Health. 2012;66(3):247–253. [DOI] [PubMed] [Google Scholar]
- 37. Mula M, Sander JW. Suicide and epilepsy: do antiepileptic drugs increase the risk? Expert opinion on drug safety. 2015;14(4):553–558. [DOI] [PubMed] [Google Scholar]
- 38. Schumock GT, Stayner LT, Valuck RJ, et al. Risk of suicide attempt in asthmatic children and young adults prescribed leukotriene-modifying agents: a nested case-control study. J Allergy Clin Immunol. 2012;130(2):368–375. [DOI] [PubMed] [Google Scholar]
- 39. Ferro MA, Boyle MH. Longitudinal invariance of measurement and structure of global self-concept: a population-based study examining trajectories among adolescents with and without chronic illness. J Pediatr Psychol. 2013;38(4):425–437. [DOI] [PubMed] [Google Scholar]
- 40. Maslow GR, Haydon AA, Ford CA, et al. Young adult outcomes of children growing up with chronic illness: an analysis of the National Longitudinal Study of Adolescent Health. Arch Pediatr Adolesc Med. 2011;165(3):256–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Scott MA, Wilcox HC, Schonfeld IS, et al. School-based screening to identify at-risk students not already known to school professionals: the Columbia suicide screen. Am J Public Health. 2009;99(2):334–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Joiner TE, Jr, Pfaff JJ, Acres JG. A brief screening tool for suicidal symptoms in adolescents and young adults in general health settings: reliability and validity data from the Australian National General Practice Youth Suicide Prevention Project. Behav Res Ther. 2002;40(4):471–481. [DOI] [PubMed] [Google Scholar]
- 43. Gould MS, Greenberg T, Velting DM, et al. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42(4):386–405. [DOI] [PubMed] [Google Scholar]
- 44. Kim JW, Szigethy EM, Melhem NM, et al. Inflammatory markers and the pathogenesis of pediatric depression and suicide: a systematic review of the literature. J Clin Psychiatry. 2014;75(11):1242–1253. [DOI] [PubMed] [Google Scholar]
- 45. Muggah E, Graves E, Bennett C, et al. Ascertainment of chronic diseases using population health data: a comparison of health administrative data and patient self-report. BMC Public Health. 2013;13:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Baumeister H, Kriston L, Bengel J, et al. High agreement of self-report and physician-diagnosed somatic conditions yields limited bias in examining mental-physical comorbidity. J Clin Epidemiol. 2010;63(5):558–565. [DOI] [PubMed] [Google Scholar]