Abstract
Background
The ABCDE interprofessional bundle (Awakening and Breathing Coordination, Delirium monitoring and management, and Early mobility) is recommended practice in intensive care, but adoption is limited.
Objective
To examine the relationship between ICU provider attitudes regarding the ABCDE bundle and ABCDE bundle adherence.
Methods
A one-time survey of ICU providers (N=268) was conducted in ten ICUs across the country. ICU providers must have worked ≥4 shifts/month. We examined the following provider attitudes: workload burden, difficulty carrying out the bundle, perceived safety, confidence, and perceived strength of evidence. Logistic regression models were used to examine the relationship of unit level provider attitudes with patient level (N=101) ABCDE bundle adherence, adjusted for patient age, severity of illness, and comorbidity.
Results
For every unit increase in workload burden, there was a 53% decrease in adherence to the ABCDE bundle (OR=0.47, CI=0.28–0.79, p=0.004). Bundle difficulty (OR=0.29, CI=0.08–1.07), perceived safety (OR=0.51, CI=0.10–2.65), confidence (OR=0.37, CI=0.10–1.35), and perceived strength of evidence (OR=0.69, CI=0.14–3.35) were not associated with ABCDE bundle adherence. For every unit increase in perceived difficulty carrying out the bundle, there was a 59% reduction in adherence with early mobility (OR=0.41, CI=0.19–0.90, p=0.027). Additionally, ABCDE bundle adherence (i.e., ventilator bundle) was less than DE bundle adherence (i.e., ventilator-free bundle) (97% vs. 72%, z=5.47, p<0.001).
Conclusions
Reported workload burden influences ABCDE bundle adherence. High perceived difficulty carrying out the bundle impacts adherence with early mobility. Focusing interventions on workload burden and factors influencing bundle difficulty may facilitate ABCDE bundle adherence.
Keywords: intensive care unit, interprofessional, implementation, adherence, guidelines, framework
Background
Intensive Care Unit (ICU) delirium and ICU-acquired weakness (ICU-AW) are common and serious public health problems. Duration of ICU delirium has been associated with reduced probability of survival after hospital discharge and long-term cognitive impairment.1–3 Likewise, ICU-AW is independently associated with post discharge mortality and reduced physical functioning up to five years following critical illness.4,5 Attention is now turning to the long-term outcomes of ICU survivors and the role of critical care therapies on daily life. Interprofessional approaches are a solution for taking the complexity of critical care therapies and bundling them into organized, practical, and traceable procedures.6
The ABCDE bundle (Awakening and Breathing Coordination, Delirium assessment/management, and Early mobility), is an interprofessional, evidence-based bundle that, when implemented, has resulted in a reduction in ventilator, delirium, and hospital days; an increase in ICU mobilization; and significant financial benefits.7–9 Implementation of the ABCDE bundle is not only endorsed by critical care societies (i.e., Society of Critical Care Medicine, American Association of Critical-Care Nurses), but also national quality improvement agencies (i.e., Institute for Healthcare Improvement, Agency for Healthcare Research and Quality, and the Centers for Disease Control and Prevention) as a means to enhance the quality and safety of critical care. Despite endorsements and evidence for effectiveness of the ABCDE bundle, uptake is limited.10–17 A recent survey of 212 interprofessional Michigan ICU healthcare professionals reported that only 12% have implemented the ABCDE bundle despite a statewide quality improvement initiative.18
Factors affecting interprofessional ICU protocol implementation and adherence are poorly understood. Review of the literature suggests that provider attitudes (i.e., prevailing tendencies and way of thinking) influence protocol implementation and adherence.19–21 For example, a study to evaluate factors influencing nurses administration of sedatives in mechanically ventilated patients found that nurse attitudes toward the efficacy of sedation was associated with reports of sedative administration. Nurse attitudes toward the mechanical ventilation experience was positively correlated with sedation practices (rs=0.28, p<0.01) and the intention to administer sedatives to all mechanically ventilated patients (rs=0.58, p<0.01).22
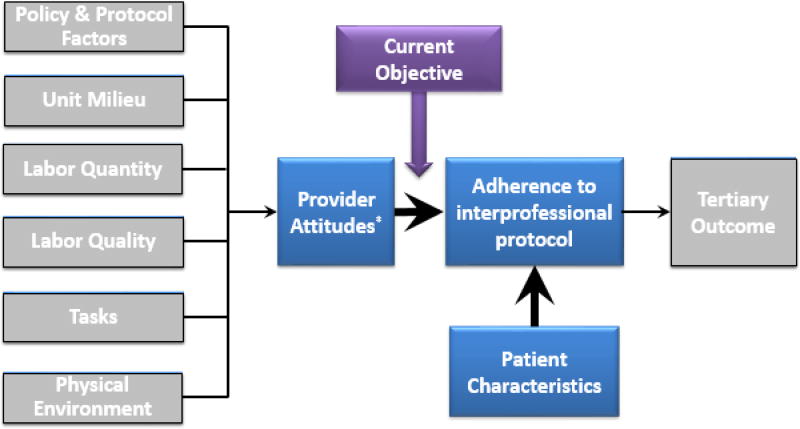
The Interprofessional Bundle Implementation conceptual framework (Figure 1) illustrates earlier studies’ findings that organizational domains (such as policy and protocol factors [i.e., accessibility, clarity, complexity], unit milieu [i.e., coordination among disciplines], tasks [i.e., autonomy and time demands], physical environment [i.e., unit layout and access to supplies]) can have a direct influence on provider attitudes; The association of ICU provider attitudes, however, on adherence to the ABCDE bundle is unknown. Therefore, the objective of this study was to examine the associations of ICU provider attitudes with ABCDE bundle adherence. Specific provider attitudes include 1) workload burden, 2) difficult to carry out, 3) perceived safety, 4) confidence, and 5) perceived strength of evidence of the ABCDE bundle. We hypothesized that provider attitudes are associated with execution of the ABCDE bundle.20,23
Figure 1. Conceptual Framework for Interprofessional Bundle Implementation.
Organizational domains such as policy and protocol factors, unit milieu, labor quantity, labor quality, tasks, and physical environment are proposed to influence provider attitudes and, thus, adherence to the ABCDE bundle. This study is looking for the associations of provider attitudes with ABCDE bundle adherence in particular.
*Provider attitudes: workload burden, difficult to carry out, perceived safety of ABCDE bundle implementation, confidence in performing the ABCDE bundle, and perceived strength of evidence for the ABCDE bundle.
Methods
This was a multicenter, prospective, cohort study funded by the American Association of Critical-Care Nurses and Sigma Theta Tau International Critical Care Grant. Approval was obtained from the Institutional Review Board at each of the participating centers. Vanderbilt University was the coordinating center for the study. Recruitment was conducted within the medical and surgical ICUs in six participating centers: Baystate Medical Center (Springfield, MA), Vanderbilt University Hospital (Nashville, TN), University Hospital San Antonio (San Antonio, TX), University of Maryland Medical Center (Baltimore, MD), University of Michigan Health System (Ann Arbor, MI), and Harborview Medical Center (Seattle, WA).
Sample
A total sample of 268 ICU healthcare professionals included registered nurses (RNs), advanced practice nurses, physical therapists (PTs), occupational therapists (OTs), respiratory therapists (RTs), pharmacists, and physicians providing care to patients (≥4 shifts/month) nested in eligible medical and surgical ICUs practicing the ABCDE bundle in participating hospitals. A waiver of documentation of informed consent was obtained for administration of the anonymous survey for ICU healthcare professionals. Patients included those with qualifying organ failure (i.e., mechanical ventilation, noninvasive ventilation, treatment for shock) enrolled in an ongoing clinical trial with daily tracking of ABCDE bundle adherence.
Procedures
A 71-item content-validated electronic ABCDE Provider Survey was used to collect data on the provider attitudes (CVI=0.96, p=.05, α=0.95).23 The investigator conducted in-person meetings with the leadership of each unit and department at participating hospitals to describe survey distribution requirements. An electronic survey link was forwarded to the targeted ICU healthcare professionals by unit and departmental leadership. Survey participation was facilitated through the use of unit signage and recruitment postcards. Site-specific methods were employed to reach the target sample while, at the same time, reducing sampling error. Reminders were sent to ICU healthcare professionals at four and eight weeks to maximize survey response rates.
Daily conduct of the ABCDE bundle was at the discretion of the ICU team and guided by a standardized protocol (see Supplementary Materials). The investigators had no role in performing ABCDE bundle components. Adherence was tracked via the ABCDE adherence checklist (see Supplementary Materials). The checklist was placed at the patient bedside and completed daily (i.e., 24h calendar day) by the RN and other healthcare professionals involved in completing ABCDE bundle components. ABCDE bundle adherence checklists were distributed, collected and recorded daily by trained study staff. All study data were managed using Research Electronic Data Capture (REDCap) tools hosted at Vanderbilt University by either the study principal investigator or trained personnel.24
Variables and Measures
Provider attitudes are defined as the internal disposition of healthcare professionals to adhere to the ABCDE bundle. Provider attitudes were calculated from 10-point visual analog scale responses. Higher scores represented more positive views for all but workload burden and difficult to carry out attitudes. Five analyses of two individual items and three subscales of provider attitudes were run. The three provider attitude subscales, perceived safety of ABCDE bundle implementation (α=0.73), confidence in performing the ABCDE bundle (α=0.69), and perceived strength of evidence for the ABCDE bundle (α=0.86) were used for ease of analysis. Workload burden and difficult to carry out were each analyzed as individual items due to poor subscale reliability (α=0.16). Averages for each of the provider attitude subscales and individual items were subsequently calculated and aggregated by unit (see Supplementary Materials).
ABCDE bundle adherence was defined as all five components (ABCDE bundle) requiring completion during ventilator ICU days and Delirium assessment/management and Early mobility components (DE bundle) requiring completion during ventilator-free ICU days, as Awakening and Breathing trial Coordination are not relevant for patients who are not on the ventilator. ABCDE bundle adherence was computed for the entire period of ventilator ICU days as [(days of ABCDE adherence) / (total ventilator ICU days)]. DE bundle adherence was computed for the entire period of ventilator-free ICU days as [(days of DE adherence) / (total ventilator-free ICU days)]. Adherence to individual components on ventilator days (ABCDE bundle) and ventilator-free days (DE bundle) was computed separately using the same equation.
Statistical Analysis
Statistical analyses were conducted using IBM SPSS version 23 and STATA version 14. Graphical and descriptive statistical methods were used to summarize and evaluate data distributions. Frequency distributions summarized nominal data. Continuous variable distributions for provider attitudes and adherence data were skewed, therefore median and interquartile ranges were used to summarize the data. Provider attitude data were first aggregated at the unit level. Subsequently, those unit level provider attitude scores were linked with the patient adherence records in the respective units. Logistic regression models were used to test the effects of unit level provider attitude values on ABCDE bundle adherence and select individual bundle components (i.e., Coordination and Early mobility) while controlling for relevant patient characteristics (i.e., age, Charlson comorbidity index, APACHE II score, ventilator status). There were not enough cases of nonadherence to evaluate logistic regression in the remaining individual bundle components. To maintain the statistical power and variability in ABCDE adherence among assessments for the same patient the standard errors in each model were adjusted for patient data clustering.25 Tests of statistical significance maintained a Type I error rate of 0.05 (p<0.05).
Results
Patient Characteristics
A total of 101 patients were enrolled in the study, N=70 enrolled in medical units (median=11, min=3, max=22) and N=31 enrolled in surgical units (median=10, min=2, max=13). Patients were a majority Caucasian (89%) and male (58%) with a mean age of 58 years (Table 1). Patients were admitted to the ICUs for several different medical and surgical reasons with the highest percentage presenting for management of sepsis and/or septic shock (39%). APACHE II scores for the sample population indicated a high severity of illness (mean=27.7, SD=9.3), yet there was a minimal comorbidity per the Charlson Comorbidity Index (median=1.5, IQR=0,2.3).26,27
Table 1.
Characteristics of patients monitored for ABCDE bundle adherence*
| Characteristic | Patient values (N=101) |
|---|---|
|
| |
| Age, mean (SD) | 54.6 (13.6) |
|
| |
| Female, n (%) | 42 (41.6) |
|
| |
| Male, n (%) | 59 (58.4) |
|
| |
| Caucasian, n (%) | 89 (88.1) |
|
| |
| APACHE II, mean (SD) | 27.7 (9.3) |
|
| |
| Charlson Comorbidity Index, median (IQR) | 1.5 (0, 2.3) |
|
| |
| Admitting diagnosis, n (%) | |
| • Sepsis/Septic Shock | 38 (37.6) |
| • Airway protection, Other pulmonary | 26 (25.7) |
| • COPD/Asthma | 15 (14.8) |
| • Acute Lung Injury | 10 (9.9) |
| • Transplants | 4 (4.0) |
| • Metabolic Imbalance or Cirrhosis | 3 (3.0) |
| • Cardiomyopathy or Arrhythmia | 2 (2.0) |
| • Other reason | 3 (3.0) |
Abbreviations: ABCDE=Awakening and Breathing trial Coordination, Delirium assessment/management, Early mobility; APACHE II=Acute Physiology and Chronic Health Evaluation II; IQR=interquartile range; SD=standard deviation
Patient inclusion criteria include age ≥18 years, in one of the study ICUs with qualifying organ failure (i.e., mechanical ventilation, noninvasive ventilation, treatment for shock). This sample represents a population highly susceptible to the development of delirium and ICU-AW and require the full ABCDE bundle. Patient exclusion criteria included severe dementia, neurological injuries, pregnancy, moribund, active seizures, and prisoners.
Provider Characteristics and Attitudes
The survey response rate was 25% with N=268 included in the analysis. Surveys were excluded for the following reasons: wrong unit (n=9), and lack of provider attitude data for analysis (n=106). The majority of participants were nurses (58%) and physicians (24%). The remainder of the sample included nurse practitioners (n=6), occupational therapists (n=7), pharmacists (n=10), physical therapists (n=20), and respiratory therapists (n=30).
Participants reported a high perceived strength of evidence (median=9.4, IQR=8.3,9.9) for the ABCDE bundle. Most participants reported feeling confident (median=8.6, IQR=7.0,9.5) with ABCDE bundle implementation with a moderate perceived level of safety (median=8.75, IQR=7.7,9.6). Workload burden associated with the bundle was neutral (median=5.2, IQR=2.8,7.0) and participants tended to disagree with having difficulty carrying out the bundle (median=4.0, IQR=2.0,5.9).
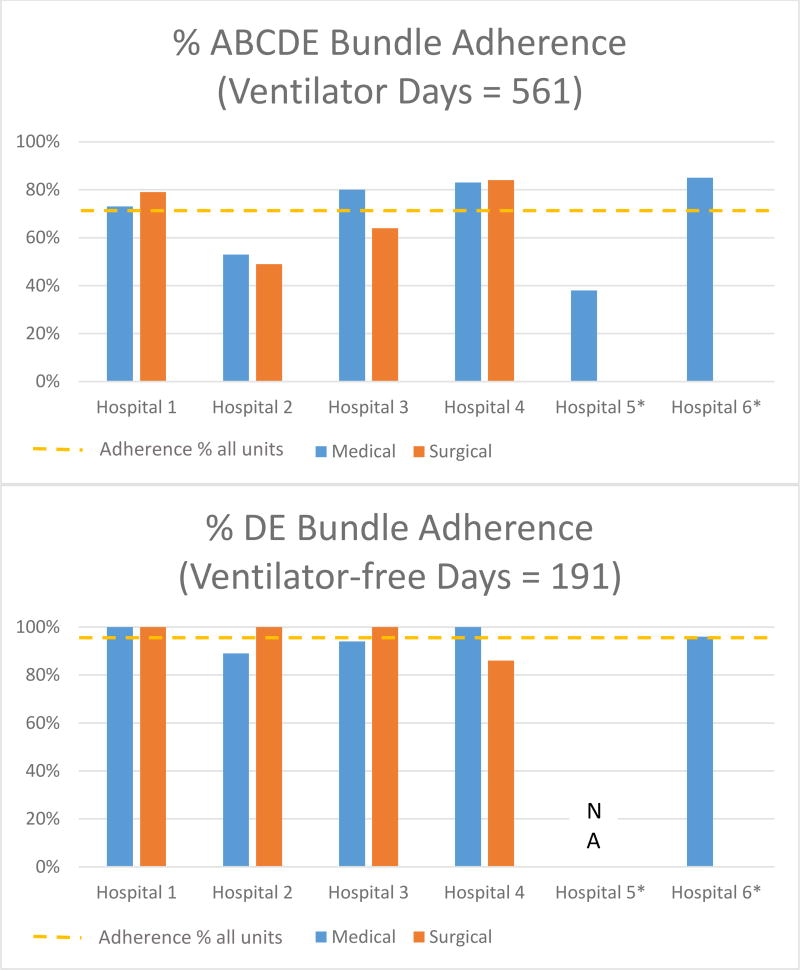
ABCDE (ventilator days) and DE (ventilator-free days) Bundle Adherence
Adherence was measured for 101 patients on a total of 752 ICU days (Figure 2). Variation in ABCDE bundle adherence (on ventilator days) was noted across units, ranging between 38% and 85%. DE bundle adherence (on ventilator-free days) was less variable among units, ranging between 86% and 100%. Overall bundle adherence was greater on ventilator-free (DE bundle) days compared to ventilator (ABCDE bundle) days across all units (97% vs. 72%, z=5.47, p<0.001). Overall ABCDE bundle adherence was lower in surgical units compared to medical units, but did not reach statistical significance (63% vs. 75%, z=1.89, p=0.059). When bundle components were evaluated individually (see Supplementary Materials), Coordination (i.e., breathing trial preceded by awakening trial, 89%) and Early mobility (86%) had the lowest levels of adherence for mechanically ventilated patients. Reasons for ABCDE bundle components not being completed are recorded in Table 2. The most common reason for Awakening trials not being completed was respiratory instability (33.3%). The most common reason for Breathing trials not being completed was PEEP >7.5 (36.9%). The most common reason for Early mobility not being completed was RASS -4 or -5 (23.8%). Reasons for not completing Coordination and Delirium assessment/management were not tracked.
Figure 2. Unit adherence to ABCDE (while on the ventilator) and DE (while off the ventilator) bundle**.
Abbreviations: ABCDE=Awakening and Breathing trial Coordination, Delirium assessment/management, Early mobility, DE=Delirium assessment/management and Early mobility
101 patients were observed for adherence over 561 ventilator ICU days and 191 ventilator-free ICU days across 10 ICUs (6 medical units, 4 surgical units). Overall ABCDE bundle adherence (72% represented by orange dash line) was less than DE bundle adherence (97% represented by orange dash line) in all units (p<0.001) as well as when compared by medical (p<0.001) and surgical units (p<0.001). Overall ABCDE bundle adherence was not statistically significantly greater in medical vs. surgical units (p=0.059).
**NOTE explaining the rationale behind ABCDE vs. DE adherence metrics: The ABCDE Bundle definitions used in this investigation were defined at the time of the initiation of this study, and have subsequently been modified as part of the ICU Liberation initiative to include the current ABCDEF Bundle (www.icudelirium.org and www.iculiberation.org). According to the originally defined steps, ABC are not necessarily relevant in non-ventilated patients, and for our study we anticipated that most ICUs were focusing on just the DE steps in non-ventilated patients. Thus it was decided a priori that we would assess “DE Adherence” for non-ventilated patients.
*Hospital 5 and 6 surgical ICUs did not participate in the study. Hospital 5 did not have DE bundle data, all measured bundle days were on the ventilator.
Table 2.
Documented reasons for ABCDE bundle components not being completed
| Bundle Component | Reason not completed, % (N) |
|---|---|
|
| |
| Awakening trial | Adherent – Failed Screen |
| 33.3 (65) Respiratory instability | |
| 26.2 (51) Agitation | |
| 17.4 (34) Myocardial ischemia | |
| 13.3 (26) Paralytic infusion or neuro instability | |
| NonAdherent | |
| 5.1 (10) Patient off unit | |
| 4.6 (9) Other, SAT was indicated | |
|
| |
| Breathing trial | Adherent – Failed Screen |
| 36.9 (168) PEEP >7.5 | |
| 19.7 (87) FiO2 >50% | |
| 13.4 (61) Failed SAT, no SBT | |
| 11.6 (53) Significant vasopressor infusion | |
| 6.2 (28) Agitation | |
| 4.6 (21) Respiratory or myocardial instability | |
| NonAdherent | |
| 3.1 (12) Patient off unit/other | |
| 3.7 (17) Other, SBT was indicated | |
|
| |
| Coordination | Not recorded |
|
| |
| Delirium assessment/management | Not recorded |
|
| |
| Early mobility | Adherent – Failed Screen |
| 23.8 (113) RASS -4 or -5 | |
| 17.7 (84) PEEP >10 | |
| 11.8 (56) FiO2 >60% | |
| 9.9 (47) Increased vasopressors in last 2 hours | |
| 3.4 (16) Respiratory or myocardial instability | |
| Adherent – Other reason | |
| 8.4 (40) Recent effect of sedative medications | |
| 4.9 (23) Clinical team refused | |
| 1.7 (8) Other, mobility not indicated | |
| NonAdherent | |
| 16.7 (79) Unknown, mobility was indicated | |
| 1.3 (6) No staff or staff unavailable | |
| <1 (2) Patient of unit | |
Abbreviations: FiO2=Fraction of inspired oxygen, PEEP=Positive End Expiratory Pressure, RASS=Richmond Agitation-Sedation Scale, SAT=Spontaneous Awakening Trial, SBT=Spontaneous Breathing Trial
Associations of provider attitudes and ABCDE bundle adherence
Results of the logistic regression analyses are presented in Table 3. After controlling for patient characteristics (i.e., age, Charlson comorbidity index, APACHE II score, ventilator status), there was a 53% decrease in likelihood of adherence to the ABCDE bundle for every unit increase in the response to workload burden (OR=0.47, CI=0.28–0.79, p=0.004). Provider attitudes of difficult to carry out, perceived safety, confidence, and perceived strength of evidence were not statistically significantly associated with ABCDE bundle adherence.
Table 3.
| Provider Attitudes |
Results, OR (CI)* | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| ABCDE bundle |
Aǂ | Bǂ | C | Dǂ | E | |
|
| ||||||
| Perceived Ease of Completion | ||||||
| •Workload burden | 0.47 (0.28–0.79) | - | - | 0.69 (0.35–1.36) | - | 0.65 (0.37–1.14) |
| •Difficult to carry out | 0.29 (0.08–1.07) | - | - | 0.39 (0.15–1.02) | - | 0.41 (0.19–0.90) |
|
| ||||||
| Perceived Safety of ABCDE Bundle Implementation | 0.51 (0.10–2.65) | - | - | 0.84 (0.13–5.58) | - | 2.63 (0.75–9.23) |
|
| ||||||
| Confidence Performing ABCDE Bundle | 0.37 (0.10–1.35) | - | - | 0.31 (0.08–1.18) | - | 1.25 (0.41–3.81) |
|
| ||||||
| Perceived Strength of Evidence for ABCDE Bundle | 0.69 (0.14–3.35) | - | - | 1.08 (0.23–5.10) | - | 3.46 (0.81–14.87) |
Abbreviations: A=Awakening trial, B=Breathing trial, C=Coordination (breathing trial preceded by awakening trial), D=Delirium assessment/management, E=Early mobility, ABCDE=Awakening and Breathing trial Coordination, Delirium assessment/management, Early mobility, OR=odds ratio, CI=confidence interval
Select patient covariates included in all regression analyses included age, APACHE II score, and Charlson Comorbidity Index. Ventilator status was also included as a covariate in the logistic regression for ABCDE bundle and Early mobility adherence.
This table reflects the attitudes of 268 unique providers who cared for 101 patient clusters with 727 total opportunities for ABCDE bundle and individual component adherence at the unit level.
Bolded results are statistically significant at a p <0.05 level.
There was not enough variation (i.e., nonadherence) in Awakening trial, Breathing trial, and Delirium assessment/management adherence; therefore, odds ratios could not be calculated.
Upon evaluation of individual bundle components, for every unit increase in the response to difficult to carry out, there was a 59% decrease in the likelihood of Early mobility adherence (OR=0.41, CI=0.19–0.90, p=0.027). Provider attitudes of difficult to carry out, perceived safety, confidence, and perceived strength of evidence were not statistically significantly associated with Coordination adherence. There was minimal variation in Awakening trial, Breathing trial, and Delirium assessment/management adherence; thus odds ratios could not be calculated for these components.
Discussion
Although previous investigations associated nurses’ attitudes with sedation practices, no one has linked interprofessional provider attitudes with ABCDE bundle adherence.22 A multisite, multidisciplinary study of ICU healthcare professionals was conducted to investigate whether provider attitudes are associated with ABCDE bundle adherence. We demonstrated statistically significant relationships between provider attitudes and ABCDE bundle adherence (Table 3). After adjusting for select patient characteristics, the odds of ABCDE bundle adherence were 53% less with perceptions of high workload burden as compared to low workload burden. Additionally, adherence to Early mobility was 59% less likely when reported difficulty with carrying out the bundle was high. Therefore, focusing interventions on reducing workload burden and simplifying task implementation may facilitate ABCDE bundle adherence.
Overall, adherence to the ABCDE bundle was 72% on ventilator days, when all bundle components are required, and 97% on ventilator-free days, when only Delirium assessment/management and Early mobility components are required (p<0.001). Upon evaluation of previous work, we were unable to find reports of full ABCDE bundle adherence on ventilator days or DE bundle adherence on ventilator-free days for comparison. Various studies report adherence to individual ABCDE bundle components as follows: Awakening trials 71–100%8,19,28,29, Breathing trials 67–100%19,28,29, Coordination 87%29, Delirium assessment/management 46–92%8,19,21,28, and Early mobility 82%21,28. Differing definitions for adherence across studies make comparisons difficult. For example, Balas et al. reported breathing trial adherence as patients receiving a breathing trial at least once during the ICU stay while Klompas et al. reported breathing trial adherence as the percent of days with a breathing trial done when indicated. In spite of that, our individual component adherence results are consistent with the previous reports of ABCDE bundle implementation.
The adherence results found in this investigation support previous findings suggesting bundle complexity influences adherence.19,20 Those components of the ABCDE bundle that require the most coordination across disciplines (i.e., Coordination of awakening and breathing trials and Early mobility) have the lowest percent of adherence on ventilator days, 89% and 86%, respectively. Awakening trial (97%), Breathing trial (96%), and Delirium (100%) bundle components, which are essentially single discipline activities, had higher rates of adherence on ventilator days. This is further evidenced by increased adherence to Early mobility (98%) on ventilator-free days when mobilization may not necessitate respiratory, physical, or occupational therapy presence for execution.
Understanding the particular provider attitudes associated with ABCDE bundle adherence provide a basis for devising interventions to improve implementation. Guided by the conceptual framework, we suggest intervening upon organizational domains that influence perceived ease of completion (i.e., workload burden and difficulty carrying out the bundle), which in turn may lead to improved adherence to the overall ABCDE bundle and those bundle components that require the most coordination across disciplines (i.e., awakening and breathing trial coordination and early mobility). We had found (reported elsewhere) that policy and protocol factors, unit milieu, and access to supplies and equipment are organizational domains most closely associated with difficulty carrying out the bundle.23 Thus, for example, access to supplies and equipment can be improved by keeping necessary ABCDE bundle supplies (e.g., ambu bag, ventilator extension tubing, gait belt, etc.) and equipment (e.g., walker, high-back chair, oxygen tank, lift, etc.) in the patient room and/or geographically convenient supply rooms so as to maximize nurse efficiency of movement Specific strategies that target both policy and protocol factors as well as unit milieu include the development of standardized protocols (e.g., checklists, daily goal sheets); structured rounding processes (e.g., interprofessional rounds); and interprofessional training (e.g., simulation training, core competencies).30
We hypothesized that provider attitudes regarding perceived safety, confidence, and perceived strength of evidence would be associated with ABCDE bundle adherence, but the findings were not statistically significant. The internal consistency of both our perceived safety (α=0.73) and confidence (α=0.69) subscales may not have been reliable enough to make associations and likely require further refinement prior to future attempts to evaluate relationships. Further investigation of perceived safety and confidence with refined subscales is necessary to elucidate whether a relationship with ABCDE adherence is present. Further refinement of the perceived strength of evidence subscale items may also be required to ensure that the appropriate constructs are being captured. A second potential explanation for the null findings include the studies small sample size. Future studies employing larger sample sizes may be more able to identify relationships between provider attitudes and ABCDE bundle adherence.
Strengths of the current study include interprofessional input for provider attitudes regarding the ABCDE bundle and a statistical analysis that allowed us the ability to control for covariates. Still, there are limitations to address. First, we applied the ABCDE bundle framework as originally described by Vasilevskis et al.31 At this time, the bundle was described as an evolving framework open to new strategies being included. Since its original publication, the bundle has now developed into the ABCDEF bundle to include family engagement and recommendations from recent guidelines.6,32 Next, ABCDE adherence data were not collected on every patient in the ICU. Bedside providers were encouraged to perform ABCDE bundle components daily; thus, adherence data for this study is likely an overestimation of the actual unit adherence. Lastly, there is the potential for nonresponse bias due to a low survey response rate. The assistance of ICU leadership was solicited for guidance on the best methods to achieve survey response goals, but it is possible that only those with strong opinions for or against the ABCDE bundle participated in the survey.
Conclusions
The ABCDE bundle is recommended practice in critical care, but there is evidence that utilization is low and implementation varies. In this study, adherence to the ABCDE bundle was influenced by workload burden of the bundle. Secondary analysis demonstrated adherence to early mobility was influenced by perceived difficulty with carrying out the bundle. Focusing on interventions to address workload burden and difficulty with carrying out the bundle may optimize implementation. Consider use of checklists, daily goal sheets, and interprofessional training in addition to evaluating geographic convenience of ABCDE bundle supplies and equipment as interventions to optimize implementation. Future research requires refinement of provider attitude subscales, which will allow us to further investigate relationships with ABCDE bundle adherence using larger sample sizes for ICU providers, patients, and units. A prospective study is indicated to determine if interventions to influence provider attitudes regarding workload and simplicity of task implementation result in improved ABCDE bundle adherence.
Supplementary Material
Acknowledgments
Sources of Support: This research project was supported by the AACN-Sigma Theta Tau Critical Care grant (#20170) and the Vanderbilt Institute for Clinical and Translational Research (UL1 TR000445 from NCATS/NIH). Dr. Vasilevskis is supported by the NIH (K23AG040157), the Veterans Affairs Clinical Research Center of Excellence, and the Geriatric Research, Education and Clinical Center (GRECC). Dr. Ely and Pandharipande are supported by the NIH (AG027472, HL111111, AG035117, AG034257) and the Veterans Affairs Clinical Science Research and Development Service. Dr. Ely is supported by the Geriatric Research, Education and Clinical Center (GRECC). The authors’ funding sources did not participate in the planning, collection, analysis or interpretation of data or in the decision to submit for publication.
References
- 1.Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA : the journal of the American Medical Association. 2004;291(14):1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 2.Pisani MA, Kong SY, Kasl SV, Murphy TE, Araujo KL, Van Ness PH. Days of delirium are associated with 1-year mortality in an older intensive care unit population. American journal of respiratory and critical care medicine. 2009;180(11):1092–1097. doi: 10.1164/rccm.200904-0537OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pandharipande PP, Girard TD, Jackson JC, et al. Long-term cognitive impairment after critical illness. The New England journal of medicine. 2013;369(14):1306–1316. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wieske L, Dettling-Ihnenfeldt DS, Verhamme C, et al. Impact of ICU-acquired weakness on post-ICU physical functioning: a follow-up study. Crit Care. 2015;19:196. doi: 10.1186/s13054-015-0937-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Herridge MS, Tansey CM, Matte A, et al. Functional disability 5 years after acute respiratory distress syndrome. The New England journal of medicine. 2011;364(14):1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 6.Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Critical care medicine. 2013;41(1):263–306. doi: 10.1097/CCM.0b013e3182783b72. [DOI] [PubMed] [Google Scholar]
- 7.Balas MC, Vasilevskis EE, Olsen KM, et al. Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Critical care medicine. 2014;42(5):1024–1036. doi: 10.1097/CCM.0000000000000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kram SL, DiBartolo MC, Hinderer K, Jones RA. Implementation of the ABCDE Bundle to Improve Patient Outcomes in the Intensive Care Unit in a Rural Community Hospital. Dimensions of critical care nursing : DCCN. 2015;34(5):250–258. doi: 10.1097/DCC.0000000000000129. [DOI] [PubMed] [Google Scholar]
- 9.Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Archives of physical medicine and rehabilitation. 2010;91(4):536–542. doi: 10.1016/j.apmr.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Patel RP, Gambrell M, Speroff T, et al. Delirium and sedation in the intensive care unit: survey of behaviors and attitudes of 1384 healthcare professionals. Critical care medicine. 2009;37(3):825–832. doi: 10.1097/CCM.0b013e31819b8608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devlin JW, Nava S, Fong JJ, Bahhady I, Hill NS. Survey of sedation practices during noninvasive positive-pressure ventilation to treat acute respiratory failure. Critical care medicine. 2007;35(10):2298–2302. doi: 10.1097/01.CCM.0000284512.21942.F8. [DOI] [PubMed] [Google Scholar]
- 12.Hodgin KE, Nordon-Craft A, McFann KK, Mealer ML, Moss M. Physical therapy utilization in intensive care units: results from a national survey. Critical care medicine. 2009;37(2):561–566. doi: 10.1097/CCM.0b013e3181957449. quiz 566–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Society of Critical Care Medicine. ICU Liberation. [Accessed February 10, 2016]; http://www.iculiberation.org/Pages/default.aspx.
- 14.American Association of Critical-Care Nurses. Implementing the ABCDE Bundle at the Bedside. [Accessed February 10, 2016];2016 http://www.aacn.org/wd/practice/content/actionpak/withlinks-abcde-toolkit.pcms?menu=practice.
- 15.Institute for Healthcare Improvement. Sedation, Delirium, and Mobility in ICU Patients. [Accessed February 10, 2016];2016 http://www.ihi.org/topics/SedationDeliriumMobility/Pages/default.aspx.
- 16.Agency for Healthcare Research and Quality. Implementing the ABCDE Bundle at the Bedside. https://innovations.ahrq.gov/qualitytools/implementing-abcde-bundle-bedside.
- 17.Centers for Disease Control and Prevention. Wake Up and Breathe Collaborative. [Accessed February 10, 2016];2016 http://www.cdc.gov/hai/epiCenters/wake-up-and-breath.html.
- 18.Miller MA, Govindan S, Watson SR, Hyzy RC, Iwashyna TJ. ABCDE, but in that order? A cross-sectional survey of Michigan intensive care unit sedation, delirium, and early mobility practices. Ann Am Thorac Soc. 2015;12(7):1066–1071. doi: 10.1513/AnnalsATS.201501-066OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Balas MBWJ, Gannon D, Cohen MZ, Colburn L, Bevil C, Franz D, Olsen KM, Ely EW, Vasilevskis EE. Implementing the Awakening and Breathing Coordination, Delirium Monitoring/Management, and Early Exercise/Mobility Bundle into Everyday Care: Opportunities, Challenges, and Lessons learned for Implementing the ICU Pain, Agitation, and Delirium Guidelines. Critical care medicine. 2013;41(9):S116–127. doi: 10.1097/CCM.0b013e3182a17064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boehm LM, Vasilevskis EE, Mion LC. Interprofessional Perspectives on ABCDEF Bundle Implementation: A Focus Group Study. Dimensions of critical care nursing : DCCN. 2016 doi: 10.1097/DCC.0000000000000208. pending review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bassett R, Adams KM, Danesh V, et al. Rethinking critical care: decreasing sedation, increasing delirium monitoring, and increasing patient mobility. Joint Commission journal on quality and patient safety / Joint Commission Resources. 2015;41(2):62–74. doi: 10.1016/s1553-7250(15)41010-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guttormson JL, Chlan L, Weinert C, Savik K. Factors influencing nurse sedation practices with mechanically ventilated patients: a U.S. national survey. Intensive & critical care nursing : the official journal of the British Association of Critical Care Nurses. 2010;26(1):44–50. doi: 10.1016/j.iccn.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Boehm LM, Dietrich MS, Vasilevskis EE, Wells N, Ely WE, Mion LC. Organizational domains explain variation in ICU provider attitudes regarding the ABCDE bundle. American Journal of Critical Care. 2016 doi: 10.4037/ajcc2017297. pending review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 26.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Critical care medicine. 1985;13(10):818–829. [PubMed] [Google Scholar]
- 27.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of chronic diseases. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 28.Carrothers KM, Barr J, Spurlock B, Ridgely MS, Damberg CL, Ely EW. Contextual Issues Influencing Implementation and Outcomes Associated With an Integrated Approach to Managing Pain, Agitation, and Delirium in Adult ICUs. Critical care medicine. 2013;41(9):S128–S135. doi: 10.1097/CCM.0b013e3182a2c2b1. [DOI] [PubMed] [Google Scholar]
- 29.Klompas M, Anderson D, Trick W, et al. The preventability of ventilator-associated events. The CDC Prevention Epicenters Wake Up and Breathe Collaborative. American journal of respiratory and critical care medicine. 2015;191(3):292–301. doi: 10.1164/rccm.201407-1394OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dietz AS, Pronovost PJ, Mendez-Tellez PA, et al. A systematic review of teamwork in the intensive care unit: what do we know about teamwork, team tasks, and improvement strategies? Journal of critical care. 2014;29(6):908–914. doi: 10.1016/j.jcrc.2014.05.025. [DOI] [PubMed] [Google Scholar]
- 31.Vasilevskis EE, Pandharipande PP, Girard TD, Ely EW. A screening, prevention, and restoration model for saving the injured brain in intensive care unit survivors. Critical care medicine. 2010;38(10 Suppl):S683–691. doi: 10.1097/CCM.0b013e3181f245d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frimpong K, Stollings JL, Carlo ME, Ely EW. ICU Delirium Viewed Through the Lens of the PAD Guidelines and the ABCDEF Implementation Bundle. 2014 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.