Abstract
Mindfulness-Based Cognitive Therapy (MBCT) has been shown to effectively prevent relapse and reduce residual depressive symptoms (RDS), yet it faces barriers to dissemination. The present study examined Mindful Mood Balance (MMB), the first web-based approach to deliver the core content of MBCT. Of the 107 recurrently depressed individuals screened, 100 elected to enroll in the study and received MMB in an 8-session open trial with 6-month follow-up. Outcomes included depressive symptom severity, rumination and mindful awareness, and program engagement. A quasi-experimental comparison between MMB patients and propensity matched case-controls receiving usual depression care (UDC) (N = 100) also was conducted. The full sample and the subgroup with residual depressive symptoms (N=42) showed significantly reduced depressive severity, which was sustained over six months, and improvement on rumination and mindfulness. Examination of acceptability of MMB indicated that 42% of participants within the full sample and 36% of the RDS subgroup completed all 8 sessions and 53% within the full sample and 50% within the RDS subgroup completed at least 4 sessions, and that participants engaged with daily mindfulness practice. MMB also was associated with significant reduction in RDS severity as compared to quasi-experimental propensity matched controls. Although the use of a non-randomized design, with potential unmeasured differences between groups, and short interval of clinical follow-up were limitations, findings from this first study of a mindfulness-based program support the web-based delivery of MBCT and suggest clinical benefits for patients with histories of depression and with RDS, relative to patients receiving usual care alone.
Keywords: residual depressive symptoms, web-based treatments, mindfulness-based cognitive therapy, major depressive disorder, dissemination
Introduction
Depression is characterized by a chronic and impairing course for most individuals (Judd, 1997). The risk of developing a chronic course increases with successive episodes experienced; and even among patients who achieve clinical remission, residual depressive symptoms (RDS) following first-line antidepressant pharmacotherapy are common (Paykel, 2008; Zajecka, Kornstein, & Blier, 2013). Among patients treated in the trial of Sequenced Treatment Alternatives to Relieve Depression (STAR*D), 80–90% of patients reported at least one RDS that persisted for 12 months (Nierenberg et al., 2010). In addition to the individual symptom burden imposed by untreated RDS, the economic costs are significant and closely approach those associated with major depressive disorder itself (Cuijpers et al., 2007). Moreover, clinical inertia among practitioners treating patients with persistent, low severity symptoms has been reported (Henke, Zaslavsky, McGuire, Ayanian, & Rubenstein, 2009) and may be one factor contributing to their suboptimal clinical management (Gilbody, Bower, Fletcher, Richards, & Sutton, 2006; Katon et al., 1996).
The use of sequenced, phase-specific treatments within an envelope spanning both acute phase and post-acute care has been advocated (e.g., Fava, Ruini, & Belaise, 2007). In this context, Mindfulness Based Cognitive Therapy (MBCT) shows particular promise with evidence provided by secondary analyses reported in MBCT trials whose primary outcomes were differences in relapse rates (Kuyken et al., 2008; Segal et al., 2010) and randomized trials targeting RDS as a primary aim, with moderate to large effect sizes for MBCT in reducing RDS as compared to usual care (Geschwind, Peeters, Huibers, van Os, & Wichers, 2012; van Aalderen et al., 2012).
Despite such evidence supporting MBCT for treating RDS, common challenges to dissemination exist, including service costs, waiting lists, and time and distance to access care (Butler et al., 2008; Kessler et al., 2003). Indeed, results from a population-based service planning simulation study highlighted the need for alternative, self-guided delivery models given the predicted shortage of trained MBCT therapists (Patten & Meadows, 2009). Such recommendations are convergent with the recent emergence of web-based treatments targeting the acute phase of depression (Richards & Richardson, 2012). However, few web-based resources have been developed for patients beyond the acute phase of illness, with a focus on treating residual symptoms and preventing relapse (Holländare et al., 2013).
In an effort to reduce barriers to accessing MBCT, we developed an individually tailored, web-based treatment, Mindful Mood Balance (MMB), which provides high fidelity, widespread access to the core benefits of the in-person MBCT program. MMB teaches specific emotion regulation and depression self-management skills that address mood outcomes in a broader context of well-being, which has particular relevance for patients with RDS.
The present study examined the clinical benefit of MMB in the context of, first, an open trial design, and, second, a quasi-experimental design that compared the clinical outcomes for MMB to propensity score matched case-controls. All participants were at risk based on prior history of depression and were receiving usual depression care (UDC) at Kaiser-Permanente Colorado (KPCO), either in a primary care or behavioral health clinic. In the open trial context, we addressed two aims. First, we examined depressive symptom severity outcomes associated with MMB in the open trial. We predicted that patients receiving MMB would experience significantly greater depressive symptom severity reduction than patients receiving UDC alone. We also predicted that treatment response would be associated with benefit on our secondary outcomes of rumination and mindful awareness, which have been suggested in prior studies to be change as a function of MBCT (e.g., Kuyken 2010; Michalak, Heidenreich, Meibert, & Schulte, 2008; Michalak, Holz, & Teismann, 2011; Shahar, Britton, Sbarra, Figueredo, & Bootzin, 2010). Second, we examined the acceptability of the MMB intervention based on session attendance and home practice completion. We predicted that patients would show acceptance of this non-traditional method of training in mindfulness meditation by both attending sessions and completing home practices, which we examined descriptively. We also explored the association of session attendance and depression severity improvement. In the quasi-experimental design context, we addressed the aim of investigating differences between MMB and propensity matched case-controls receiving UDC on residual depressive symptoms. We predicted that patients receiving MMB would experience significantly greater depressive symptom severity reduction than patients receiving UDC. All outcomes were investigated within the full sample of at-risk patients and explored within the more stringently defined subgroup with current RDS.
Method
Participants
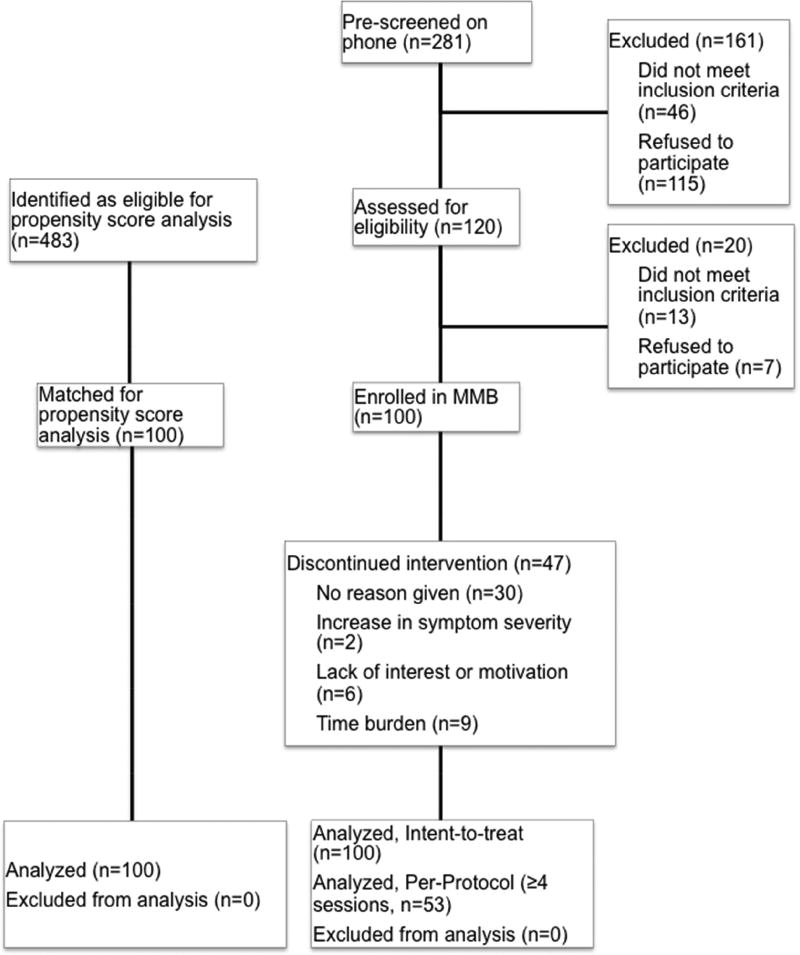
A CONSORT diagram illustrating participant flow in the study is presented in Figure 1. A total of 100 participants were recruited in the open trial between September 2012 and February 2013, based on self-referral, referred by primary care or behavioral health clinicians, or identification by electronic medical records. Project staff conducted a phone screen to assess initial eligibility criteria and potentially eligible participants were scheduled for an intake evaluation. An additional 100 participants receiving only UDC in primary care or behavioral health clinics were identified between December 2011 and July 2013 for the propensity matched control group. For the open trial, patients met the following inclusion criteria: prior major depressive episode according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR; American Psychiatric Association, 2000), baseline score of ≤ 12 on the Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, 2001), aged 18 or older, internet access, and grade 8 English proficiency. Exclusion criteria included: current major depressive episode; schizophrenia or current psychosis; organic mental disorder or pervasive developmental delay; current substance dependence; imminent suicide or homicide risk; an Axis I or II disorder that necessitated primary treatment not provided in the study, or having started on an antidepressant or changed antidepressant medication within the past 8 weeks.
Figure 1.
Participant Flow Diagram
The study protocol was approved by institutional review boards at the Centre for Addiction and Mental Health (CAMH), Kaiser-Permanente Colorado (KPCO) and the University of Colorado Boulder. Written informed consent was obtained by a study coordinator with MMB participants, and a waiver of informed consent was obtained for the procedure to identify participants for the propensity matched control group. MMB participants received a $25 gift card.
Measures
Administration
All measures were completed in person at a KPCO clinic or online using the secure survey website Qualtrics.
Depression diagnoses
The Structured Clinical Interview for DSM-IV Axis I Disorders – Patient Version (SCID-I/P; First, Spitzer, Gibbon, & Williams, 1994) was conducted at the intake interview by one of three KPCO research coordinators, whose training included watching instructional videos, conducting practice interviews, and observing study participant interviews with comparison of ratings to established rating standards.
Depressive symptoms
The PHQ-9 (Kroenke, Spitzer, & Williams, 2001) provides an overall severity score based on the sum of all items, and was completed at baseline, weekly during MMB, post-treatment, and 2.5- and 6-month follow-ups. Propensity matched controls completed the PHQ-9 at time points parallel to the baseline and post-treatment MMB assessments. The PHQ-9 also was used to define the RDS group (N=42), based on prior work that has operationalized RDS as PHQ-9 scores ≥ 5 and ≤ 9 (Manea et al., 2012); in this sample, we also allowed the inclusion of participants with scores > 5 and < 12. Participants with scores exceeding 12 were not included in the study given the likelihood of higher scores detecting an acute episode of depression, rather than RDS, and thereby necessitating acute intervention.
Rumination and Mindfulness
Both rumination and mindfulness were assessed by self-report using the Response Styles Questionnaire (RSQ; Nolen-Hoeksema & Morrow, 1991) and the Five Facet Mindfulness Questionnaire (FFMQ; Baer et al., 2008), respectively, at baseline and post-treatment.
Engagement
Attendance was recorded at each MMB session, and participants recorded frequency of at home formal mindfulness and the 3-minute breathing space practices each week.
Interventions
Mindful Mood Balance (MMB)
MMB was developed to provide the core components of the in person MBCT program in a web-based, 8-session self-administered platform. It teaches patients how to disengage from habitual, automatic, dysfunctional cognitive patterns (i.e., depression-related ruminative thought patterns), as a way to reduce RDS and vulnerability to relapse. Each of the eight MMB sessions incorporates a sequential tripartite learning cycle (experiential practice, video-based vicarious learning, and didactic information) that is core to the in-person MBCT program and that is designed to integrate learning and application of mindfulness and CBT exercises. Participants, thus, have access to the threefold presentation of content through unique and overlapping receptive learning modes (Dirkx, 2008; Eastmond, 1998). For example, one of the core MBCT practices is a Body Scan meditation practice in which participants are asked to direct their attention systematically to regions of their body. In MMB, patients are asked to: (1) perform the Body Scan by listening to guided instructions provided on the website and a downloadable audio file, (2) watch a video interaction between instructors and participants in an MBCT class as they explore their experience of the Body Scan, and (3) answer questions in an interactive learning module that inquires about a participant’s own experience with the Body Scan and relevance to managing RDS and relapse risk. A similar structure is used for the delivery of cognitive behavioral components, including didactic delivery of content from the instructors, direct experience via interactive modules, and personal reflections on relevance to managing RDS and relapse risk. Mindfulness meditation instruction includes formal practice (sitting meditation, yoga stretching, body scan), brief daily practice (e.g., the 3-minute breathing space), and informal practice (e.g., eating mindfully). Accompanying materials are provided online in each session, including handouts and audio guides. MMB participants were encouraged to engage in between-session home practice 6 days per week and to record frequency of practice.
Usual Depression Care (UDC)
UDC followed the Kaiser Permanente Adult Depression National Guidelines, an adaptation of STAR*D (Rush et al., 2006) for antidepressant management and the IMPACT model for therapy (Unutzer et al., 2002; Unutzer et al., 2008, p.2), in which care pathways are determined by severity level and include treatment with antidepressants or psychotherapy, or both.
Statistical Analyses
To test our primary hypotheses that patients receiving MMB would report a reduction in depressive symptoms and that this reduction would sustain across a 2.5- and 6- month follow up, we implemented hierarchical linear modeling (HLM; Raudenbush & Bryk, 2001) to model approximate linear change among patients enrolled in MMB, with time operationalized as session. The HLM consisted of level 1, within subject-level, where individuals’ scores changed over time. The level 2 model, between subject-level, examined the on-average intercept and on-average slope. The examination of the on-average slope provides a significance test of assessing whether the on-average slope is different from zero, corresponding to an assessment of significant improvement. We implemented the HLM model within SAS Version 9.3 procedure PROC MIXED. We include subject-specific terms for the intercept and slope, referred to as random intercept and random slope. With regards to time, we found a better fitting model, as measured by Restricted Log-Likelihood function, Akaike Information Criteria, and Bayesain Information Criteria using time as Session number rather than calendar weeks.
To test our secondary hypotheses, we used t-tests to examine our prediction of improvement from baseline to post-treatment in measures of rumination and mindfulness. To examine our hypotheses regarding engagement with MMB, we report descriptively session completion and daily home practice. To test our hypothesis of significantly greater improvement in RDS severity associated with MMB plus UDC as compared to UDC only, we employed a propensity score matching approach. We constructed a group of case-control patients receiving UDC at KPCO, separately for the full sample and for the RDS subgroup. Specifically, a logistic regression model was computed with participants’ treatment status (intervention=1 vs. control=0) as the outcome and baseline values as predictors, including PHQ-9 score, gender, race (Caucasian versus other), mental health visits (prior year), primary care visits (prior year), specialty care visits (prior year), care site (primary care or behavioral health), and comorbid anxiety. Using this model, the predicted probabilities of being chosen for the intervention (propensity scores) were estimated for each participant, providing a summary of the covariate imbalance across intervention versus control participants. These propensity scores, which provide an adjustment for the observed imbalance, were used as a matching variable based on the nearest neighbor approach in all subsequent analyses (Leon & Hedeker, 2005). This allowed us to compare the two groups with respect to change on the PHQ-9, such that the two samples had an equivalent distribution of demographic and clinical characteristics at baseline, as quantified through the matching (Rosenbaum & Rubin, 1984). To test the contrast between the MMB sample and the UDC group, we employed Analysis of Covariance to compare the residualized change based on the intake and the post-treatment PHQ-9 scores. Although the control sample had complete data, attrition was expected and observed among MMB patients; thus, we used the observed endpoints and the within MMB group HLM model-based estimated outcome for this analysis. This analysis used an intent-to-treat approach incorporating all available data from the MMB cohort regardless of the number of sessions or home practices completed.
SAS software, Version 9.3 (Copyright 2011 SAS Institute, Inc.) was used for all analyses. Degrees of freedom were estimated with the Kenward and Roger (1997) approximation, which accommodates small sample inferences. Overall significant effects were set with an alpha-level < 0.05; within group effect sizes are reported as partial correlation, r, estimated for longitudinal data as illustrated in Lipsitz et al. (2001) showing the strength of the association of the amount of reduction with time. Effect sizes for differences between MMB and propensity matched controls are reported as Cohen’s d using the formula of Raudenbush and Liu (2001). All analyses were conducted for the full sample of at risk patients and explored among the more stringently defined subgroup with RDS.
Results
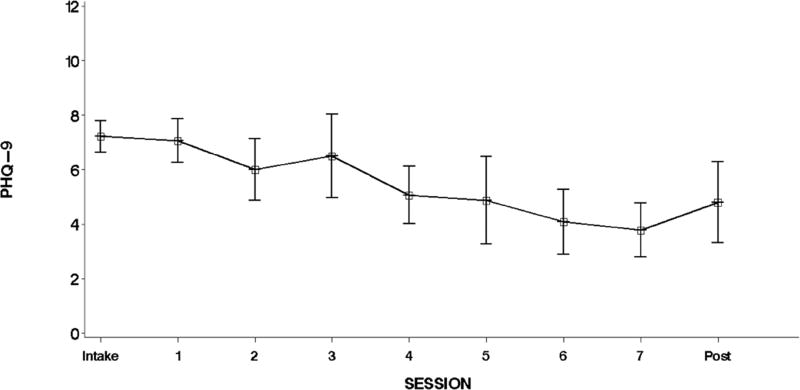
Demographic and clinical characteristics are presented in Table 1, and depressive severity, rumination, and mindfulness descriptive data by time are presented in Table 2 for both the full sample and the RDS subgroup. Participant flow is illustrated in Figure 1. Results supported our primary hypothesis that patients receiving MMB would report a reduction in depressive symptoms over the intervention, within both the full sample, t(40) = −2.83, p = 0.007, r=0.27, and the RDS subgroup, t(165) = −3.54, p = 0.003, r=0.48. Within the full sample, rate of change was 0.145 (SE = 0.052) units per session, corresponding to a change of 1.16 (SE = 0.44) units on-average from intake to post-treatment. Within the RDS subgroup, rate of change was 0.357 (SE = 0.101) units per session, corresponding to a change of 2.86 (SE = 0.807) units on-average from intake to post-treatment (see Figure 2). We also found preliminary evidence for the durability of these benefits, observing a 2.17 (SD = 3.07) point reduction from baseline to 10 weeks and a 2.33 (SD = 2.87) reduction from baseline to 6 months (all pairwise comparisons to baseline at p < 0.041).
Table 1.
Baseline characteristics of MMB and propensity score matched participants.
| Full Sample | RDS Subgroup | |||
|---|---|---|---|---|
|
|
|
|||
| Variable | MMB (n = 100) |
Case- Controls (n = 100) |
MMB (n = 42) |
Case-Controls (n = 42) |
| Age (SD) | 47.40 (11.43) | 51.0 (16.8) | 49.29 (10.26) | 50.6 (18.3) |
| Gender | ||||
| Female | 73% | 70% | 81% | 86% |
| Male | 27% | 30% | 19% | 14% |
| Race | ||||
| Asian | 2% | 0% | 2.4% | 5% |
| Black/African American | 4% | 2% | 4.8% | 0% |
| White | 87% | 81% | 85.7% | 80% |
| Other | 7% | 17% | 7.1% | 15% |
| Ethnicity | ||||
| Hispanic or Latino | 6% | 4% | 9.5% | 0% |
| Not Hispanic or Latino | 94% | 96% | 90.5% | 100% |
| Marital Status | ||||
| Single | 20% | 30.95% | ||
| Married | 64% | 47.62% | ||
| Separated/Divorced | 16% | 21.43% | ||
| Employment Status | ||||
| Unemployed | 23% | 35.7% | ||
| Full-time | 58% | 42.9% | ||
| Part-time | 14% | 19% | ||
| Student | 5% | 2.4% | ||
| # prior depressive episodes | ||||
| One | 12% | 24% | 14.3% | 14.3% |
| Two | 20% | 23% | 11.9% | 28.6% |
| Three or more | 68% | 41% | 73.8% | 42.8% |
| Antidepressant use (past year) | 84% | 82% | ||
| Psychotherapy (past year) | 19% | 19% | ||
| Past psych hospitalization | 9% | 7% | 9.5% | 7.1% |
Table 2.
Depressive Severity, Rumination, and Mindfulness by Time
| Full Sample | RDS | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| M | SD | n | M | SD | n | |
| Baseline PHQ-9 | 4.21 | 3.03 | 100 | 7.21 | 1.89 | 42 |
| Post-Treatment PHQ-9 | 2.89 | 2.69 | 38 | 4.79 | 2.78 | 14 |
| 10 week follow up PHQ-9 | 3.40 | 3.01 | 35 | 5.92 | 3.00 | 12 |
| 6 month follow up PHQ-9 | 3.04 | 2.53 | 27 | 5.38 | 2.20 | 8 |
| Intake RRS | 45.12 | 13.67 | 100 | 49.50 | 13.39 | 42 |
| Post RRS | 40.45 | 15.11 | 40 | 43.36 | 16.78 | 13 |
| Intake FFMQ | 126.52 | 18.87 | 100 | 121.40 | 19.81 | 42 |
| Post FFMQ | 132.35 | 18.42 | 40 | 127.50 | 18.43 | 14 |
Figure 2.
RDS subgroup observed means and confidence bounds for the PHQ-9 measure per session.
Consistent with our hypotheses, the level of rumination significantly decreased from baseline to post-treatment for the full sample, t(39) = 3.03, p < 0.005, r=0.23, and the RDS subsample, t(13) = 2.51, p < 0.03, r=0.57. Self-reported mindfulness significantly increased from baseline to post-treatment within the full sample, t(39) = −2.60, p < 0.02, r=0.20, but was not statistically significant among the RDS subgroup, t(13) = −0.93, p = 0.37, r=0.52.
Consistent with our prediction that MMB would be acceptable, within the full sample, 42 participants (42%) completed all 8 sessions, and 53 (53%) completed at least 4 sessions, considered a minimum therapeutic exposure in past trials of in person MBCT (Godfrin & van Heeringen, 2010; Kuyken et al., 2008; Teasdale et al., 2000). Within the RDS subgroup, 15 participants (36%) completed all 8 sessions, and 21 (50%) completed at least 4 sessions. A significant positive correlation between the number of MMB sessions completed and depressive severity improvement existed, for the full sample (r(82) = 0.22, p < 0.05) and the RDS subgroup (r(36) = 0.37, p < 0.03).
With regard to self-reported home mindfulness practice, which was assigned to be completed six days per week, within the full sample, mean weekly frequency of formal practice was 2.56 times (SD = 2.15) and 55.80 minutes (SD = 50.67) and of the 3-minute breathing space practices was 8.91 times (SD = 7.34) and 28.55 minutes (SD = 24.13) per week. Within the RDS subsample, the mean weekly frequency of formal mindfulness practice was 2.01 times (SD = 1.66) and 46.93 minutes (SD = 44.04) per week, and of the 3-minute breathing space practices was 6.73 times (SD = 6.34) per week or 23.19 minutes (SD = 22.26).
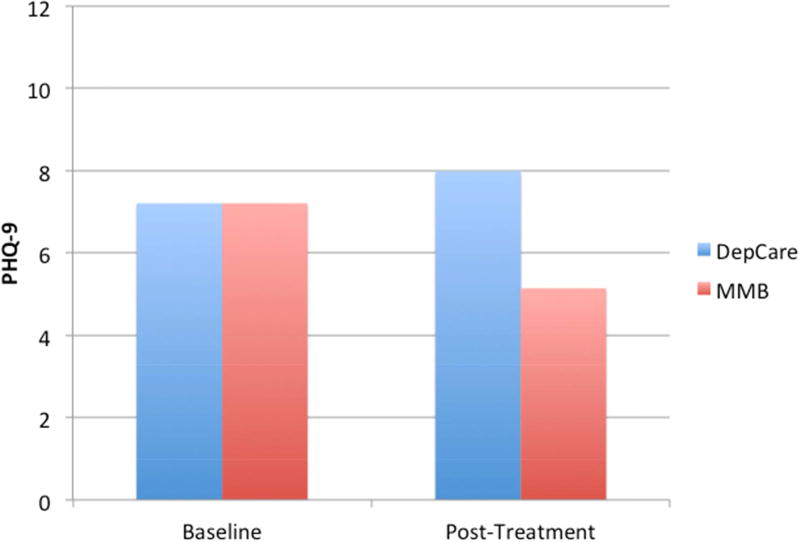
Consistent with our prediction that patients receiving MMB would experience significantly greater depressive symptom severity reduction than patients receiving UDC, within the full sample, we found a significant difference between MMB and UDC in change in PHQ-9 scores from intake to post-treatment, corresponding to an average difference of the difference of 3.75 (SE = 0.646), t(196) = 5.52, p < 0.0001, d = 0.78. Within UDC, on average, there was a significant increase over time of 2.87 (SD = 6.47), t(98) = 4.41, p < 0.0001, d = 0.88; whereas within MMB, on average, there was a significant decrease over time of 0.88 (SD = 2.26), t(99) = −3.90, p = 0.0002, d = 0.78. Within the RDS subgroup (see Figure 3), we observed a significant difference between MMB and UDC in change from intake to post-treatment corresponding to an average difference of the difference of 2.74 (SE = 0.955), t(81) = 8.22, p = 0.005, d = 1.79. Within UDC, on average, there was a non-significant increase of 0.76 (SD = 5.76), t(41) = 0.86, p = 0.40, d = 0.26; within MMB, on average, there was a significant decrease of 1.98 (SD = 2.57), t(41) = −4.99, p < 0.0001, d = 1.54.
Figure 3.
RDS Subgroup quasi-experimental comparison of MMB to propensity score matched Usual Depression Care controls.
Discussion
Sustained recovery from major depression is not the norm, as many patients experience elevated risk of relapse and impairment following an acute episode. Relapse risk increases by 16% with each additional episode, and RDS following acute phase treatment are both common and associated with negative prognosis (Zajecka et al., 2013). Web-based depression interventions represent a rapidly emerging approach with potential to address long-term care needs of patients with depressive histories generally and those with RDS. MMB is the first web-based intervention with integrated training in mindfulness and CBT with specific application for patients vulnerability to relapse, including those with RDS.
Patients reported significant reduction in depressive severity during MMB, with preliminary indications that these gains were sustained over a six-month follow-up period, and significant improvement on rumination and mindfulness. In comparison to effect sizes reported by randomized trials of MBCT in-person for participants with RDS (Geschwind et al., 2012 = 0.56, Strauss et al., 2014 =0.73), MMB’s quasi-experimental comparison with UDC indicated an ES of 0.78, suggesting similar levels of efficacy. Although these benefits may be moderate for any single patient, the effect may have importance when considered in the context of the prevalence of recurrent depression and the scalability of web-based delivery. The quasi-experimental comparison to UDC within a large healthcare system also suggests that MMB may provide significantly greater reduction in depressive symptoms. MMB may offer a viable option for extending the reach of treatments for depression (Glasgow, 2007), and in light of the potentially lower costs and increased accessibility of the web-based format, may offer significant benefit to individuals and healthcare systems. Such results, however, must be interpreted with caution given potential problems with non-randomized designs, as detailed below.
Although some might view the teaching of mindfulness meditation over the web as a questionable departure from traditional formats (Grossman & Van Dam, 2011), participants also demonstrated strong acceptance of MMB and home practice, albeit at lower levels than have been reported for in-person groups. Home practice was completed approximately 50% of the time as compared to 80% as reported by in-person class participants (Carmody & Baer, 2008). MMB retention rates of approximately 50% are similarly lower than those reported for in person MBCT groups (80–85%; Geschwind et al., 2012; Teasdale et al., 2000). In contrast, MMB retention rates are notably higher than the figure of 43% reported for other web-based depression treatments in a recent meta-analysis of 36 studies (Richards & Richardson, 2012). Although MMB was not developed as a replacement for in-person intervention, it may be a valuable tool for expanding the array of options in settings where access to programs such as in-person MBCT is limited. As such, it will be important for future research to explore ways to increase engagement, particularly given that completion of MMB sessions was associated with magnitude of clinical benefit. Specific options to explore might include: 1) automated email and online messaging to promote connection with the program between sessions, 2) increasing ease of downloadable recorded home practices, 3) options for interacting with an MMB user community, 4) availability of a mobile app for just in time reminders and monitoring of mindfulness home practices, 5) a coaching protocol that features motivational enhancement strategies for online treatments and troubleshooting for challenges with engagement. Ultimately, however, the field as a whole will need to grapple with key questions regarding expectations of session attendance and homework completion for web-based training in mindfulness meditation.
Three primary limitations of the study are important to consider. First, the lack of randomization precludes drawing causal inferences about the efficacy of MMB. The quasi-experimental design drew from the same population of patients within the Kaiser Permanente system over the same time period, and the propensity matching method allowed us to control for specific demographic and clinical characteristics. It is possible, however, that unmeasured variables distinguish the groups and contribute to differences in outcome. Importantly, the participants who received MMB may differ in terms of motivation for self-care generally in ways that influence outcomes independent of MMB exposure. In addition, the pattern of change evident among patients in the UDC group may not generalize to patients treated in other settings. For these reasons, future randomized controlled trials are essential. Second, we did not examine formally the fidelity of the MMB program with respect to the original MBCT manual. Third, the six-month follow-up period did not allow us to examine relapse, and the sample available for study decreased after the intervention phase. Although we examined change in constructs linked by prior research to prevention effects, we did not examine the relapse preventive effects of MMB. It will be vital for future studies to assess outcomes over a longer duration.
The initial outcomes of MMB in both the open trial and the quasi-experimental comparison speak to its promise as a scalable approach for the treatment of RDS and potential application for prevention of depressive relapse. The delivery of core strategies and skills of MBCT within the web-based MMB framework may promote long-term wellness among vulnerable patients.
Highlights.
First study of online MBCT for recurrent depression and residual symptoms.
MMB reduced depressive severity and rumination while increasing mindfulness.
Greater improvement compared to Usual Depression Care in a large health system.
Initial support for web-based delivery of the core skills and strategies of MBCT.
Acknowledgments
We acknowledge funding by the National Institute of Mental Health (R34MH087723; PI Segal). The authors wish to thank all the study team members at the University of Colorado Boulder, Kaiser Permanente Colorado, and University of Toronto who contributed to the completion of this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- van Aalderen JR, Donders ART, Giommi F, Spinhoven P, Barendregt HP, Speckens AEM. The efficacy of mindfulness-based cognitive therapy in recurrent depressed patients with and without a current depressive episode: a randomized controlled trial. Psychological Medicine. 2012;42(5):989–1001. doi: 10.1017/S0033291711002054. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, A. Diagnostic and statistical manual of mental disorders: DSM-IV-TR®. 4th ed. Washington, DC: American Psychiatric Pub; 2000. [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Williams JMG. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Butler M, Kane RL, McAlpine D, Kathol RG, Fu SS, Hagedorn H, Wilt TJ. Integration of mental health/substance abuse and primary care. Evidence Reports/Technology Assessments, No. 173. 2008 from http://www.ncbi.nlm.nih.gov/books/NBK38632/ [PMC free article] [PubMed]
- Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine. 2008;31(1):23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Smit F, Oostenbrink J, De Graaf R, Ten Have M, Beekman A. Economic costs of minor depression: a population based study. Acta Psychiatrica Scandinavica. 2007;115(3):229–236. doi: 10.1111/j.1600-0447.2006.00851.x. [DOI] [PubMed] [Google Scholar]
- Dirkx JM. The meaning and role of emotions in adult learning. New directions for adult and continuing education. 2008;2008(120):7–18. [Google Scholar]
- Eastmond DV. Adult learners and Internet based distance education. New directions for adult and continuing education. 1998;1998(78):33–41. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for Axis I DSM-IV Disorders--Patient Edition. Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- Geschwind N, Peeters F, Huibers M, van Os J, Wichers M. Efficacy of mindfulness-based cognitive therapy in relation to prior history of depression: randomised controlled trial. British Journal of Psychiatry. 2012;201(4):320–325. doi: 10.1192/bjp.bp.111.104851. [DOI] [PubMed] [Google Scholar]
- Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Archives of Internal Medicine. 2006;166(21):2314. doi: 10.1001/archinte.166.21.2314. [DOI] [PubMed] [Google Scholar]
- Glasgow RE. eHealth evaluation and dissemination research. Am J Prev Med. 2007;32(5 Suppl):S119–126. doi: 10.1016/j.amepre.2007.01.023. [DOI] [PubMed] [Google Scholar]
- Godfrin KA, van Heeringen C. The effects of mindfulness-based cognitive therapy on recurrence of depressive episodes, mental health and quality of life: A randomized controlled study. Behaviour Research and Therapy. 2010;48(8):738–746. doi: 10.1016/j.brat.2010.04.006. [DOI] [PubMed] [Google Scholar]
- Grossman P, Van Dam NT. Mindfulness, by any other name…: trials and tribulations of sati in western psychology and science. Contemporary Buddhism. 2011;12(1):219–239. [Google Scholar]
- Henke RM, Zaslavsky AM, McGuire TG, Ayanian JZ, Rubenstein LV. Clinical inertia in depression treatment. Medical Care. 2009;47(9):959–967. doi: 10.1097/MLR.0b013e31819a5da0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holländare F, Anthony SA, Randestad M, Tillfors M, Carlbring P, Andersson G, Engström I. Two-year outcome of internet-based relapse prevention for partially remitted depression. Behav Res Ther. 2013;51(11):719–22. doi: 10.1016/j.brat.2013.08.002. [DOI] [PubMed] [Google Scholar]
- Judd LL. The clinical course of unipolar major depressive disorders. Archives of General Psychiatry. 1997;54(11):989–991. doi: 10.1001/archpsyc.1997.01830230015002. [DOI] [PubMed] [Google Scholar]
- Katon W, Robinson P, Von Korff M, Lin E, Bush T, Ludman E, Walker E. A multifaceted intervention to improve treatment of depression in primary care. Archives of General Psychiatry. 1996;53(10):924. doi: 10.1001/archpsyc.1996.01830100072009. [DOI] [PubMed] [Google Scholar]
- Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997:983–997. [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Wang PS. The epidemiology of major depressive disorder - Results from the National Comorbidity Survey Replication (NCS-R) JAMA-Journal of the American Medical Association. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9 - Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuyken W, Byford S, Taylor RS, Watkins E, Holden E, White K, Teasdale JD. Mindfulness-Based Cognitive Therapy to Prevent Relapse in Recurrent Depression. Journal of Consulting and Clinical Psychology. 2008;76(6):966–978. doi: 10.1037/a0013786. [DOI] [PubMed] [Google Scholar]
- Kuyken W, Watkins E, Holden E, White K, Taylor RS, Byford S, Dalgleish T. How does mindfulness-based cognitive therapy work? Behaviour Research and Therapy. 2010;48(11):1105–1112. doi: 10.1016/j.brat.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Leon AC, Hedeker D. A mixed-effects quintile-stratified propensity adjustment for effectiveness analyses of ordered categorical doses. Statistics in Medicine. 2005;24(4):647–658. doi: 10.1002/sim.2042. [DOI] [PubMed] [Google Scholar]
- Lipsitz SR, Leong T, Ibrahim J, Lipshultz S. A partial correlation coefficient and coefficient of determination for multivariate normal repeated data. Journal of the Royal Statistical Society Series D – The Statistician. 2001;50:87–95. [Google Scholar]
- Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. Canadian Medical Association Journal. 2012;184(3):E191–E196. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalak J, Heidenreich T, Meibert P, Schulte D. Mindfulness predicts relapse/recurrence in major depressive disorder after mindfulness-based cognitive therapy. Journal of Nervous and Mental Disease. 2008;196(8):630–633. doi: 10.1097/NMD.0b013e31817d0546. [DOI] [PubMed] [Google Scholar]
- Michalak J, Hölz A, Teismann T. Rumination as a predictor of relapse in mindfulness-based cognitive therapy for depression. Psychology and Psychotherapy: Theory, Research and Practice. 2011;84(2):230–236. doi: 10.1348/147608310X520166. [DOI] [PubMed] [Google Scholar]
- Nierenberg A, Husain M, Trivedi M, Fava M, Warden D, Wisniewski S, Rush A. Residual symptoms after remission of major depressive disorder with citalopram and risk of relapse: a STAR* D report. Psychological Medicine. 2010;40(01):41–50. doi: 10.1017/S0033291709006011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow J. A prospective-study of depression and posttraumatic stress symptoms after a natural disaster - the 1989 Loma-Prieta earthquake. Journal of Personality and Social Psychology. 1991;61(1):115–121. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- Patten SB, Meadows GM. Population-Based Service Planning for Implementation of MBCT: Linking Epidemiologic Data to Practice. Psychiatric Services. 2009;60(11):1540–1542. doi: 10.1176/ps.2009.60.11.1540. [DOI] [PubMed] [Google Scholar]
- Paykel E. Partial remission, residual symptoms, and relapse in depression. Dialogues in clinical neuroscience. 2008;10(4):431. doi: 10.31887/DCNS.2008.10.4/espaykel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards D, Richardson T. Computer-based psychological treatments for depression: A systematic review and meta-analysis. Clinical Psychology Review. 2012;32(4):329–342. doi: 10.1016/j.cpr.2012.02.004. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Liu XF. Effects of study duration, frequency of observation, and sample size on power in studies of group differences in polynomial change. Psychological Methods. 2001:387–401. [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DB. Reducing Bias in Observational Studies Using Subclassification on the Propensity Score. Journal of the American Statistical Association. 1984;79(387):516–524. [Google Scholar]
- Rush A, Trivedi M, Wisniewski S, Nierenberg A, Stewart J, Warden D, Lebowitz B. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR* D report. American Journal of Psychiatry. 2006;163(11):1905–1917. doi: 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Bieling P, Young T, MacQueen G, Cooke R, Martin L, Levitan RD. Antidepressant Monotherapy vs Sequential Pharmacotherapy and Mindfulness-Based Cognitive Therapy, or Placebo, for Relapse Prophylaxis in Recurrent Depression. Archives of General Psychiatry. 2010;67(12):1256–1264. doi: 10.1001/archgenpsychiatry.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahar B, Britton WB, Sbarra DA, Figueredo AJ, Bootzin RR. Mechanisms of change in mindfulness-based cognitive therapy for depression: Preliminary evidence from a randomized controlled trial. International Journal of Cognitive Therapy. 2010;3(4):402–418. [Google Scholar]
- Strauss C, Cavanagh K, Oliver A, Pettman D. Mindfulness-based interventions for people idagnosed with a current episode of an anxiety or depressive disorder: A meta-analysis of randomised controlled trials. PLOS One. 2014;9(4) doi: 10.1371/journal.pone.0096110. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, Williams JMG, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology. 2000;68(4):615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- Unutzer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, Lin EH. Collaborative care management of late-life depression in the primary care setting. JAMA: the journal of the American Medical Association. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- Unutzer J, Katon WJ, Fan M-Y, Schoenbaum MC, Lin EH, Della Penna RD, Powers D. Long-term Cost Effects of Collaborative Care for Late-life Depression-Page 2. American Journal of Managed Care. 2008;14:95–100. [PMC free article] [PubMed] [Google Scholar]
- Zajecka J, Kornstein SG, Blier P. Residual symptoms in major depressive disorder: prevalence, effects, and management. Journal of Clinical Psychiatry. 2013;74(4):407–414. doi: 10.4088/JCP.12059ah1. [DOI] [PubMed] [Google Scholar]