Abstract
BACKGROUND
Heart failure (HF) symptoms such as dyspnea are common and may precipitate hospitalization. Medication nonadherence is presumed to be associated with symptom exacerbations, yet how HF symptoms, medication adherence, and hospitalization/death are related remains unclear.
OBJECTIVE
To explore the relationships among HF symptoms, medication adherence, and cardiac event-free survival in patients with HF.
METHODS
At baseline, patients’ demographic, clinical data, and HF symptoms were collected in 219 patients with HF. Medication adherence was monitored using the Medication Event Monitoring System. Patients were followed for up to 3½ years to collect hospitalization and survival data. Logistic regression and survival analyses were used for analyses.
RESULTS
Patients reporting dyspnea or ankle swelling were more likely to have poor medication adherence (p=.05). Poor medication adherence was associated with worse cardiac event-free survival (p=.006). In Cox regression, patients with HF symptoms had 2 times greater risk for a cardiac event than patients without HF symptoms (p=.042). HF symptoms were not a significant predictor of cardiac event-free survival after entering medication adherence in the model (p=.091), indicating mediation.
CONCLUSION
Medication adherence was associated with fewer HF symptoms and lower rates of hospitalization and death. It is important to develop interventions to improve medication adherence that may reduce HF symptoms and high hospitalization and mortality in patients with HF.
Keywords: symptoms, medication adherence, heart failure, outcomes, mediator
INTRODUCTION
Heart failure (HF) is a chronic and costly condition with high morbidity and mortality.1 Approximately 6 million Americans have heart failure (HF), and it is estimated that more than 8 million Americans may be living with this condition by 2030.1, 2 Patients with chronic HF have symptoms of congestion, such as dyspnea and ankle swelling, and symptoms commonly worsen and lead to hospitalizations.3–5
Poor medication adherence is associated with worse health outcomes, including higher rates of hospitalizations and death in patients with HF.6–10 In Riegel’s original and recently revised Self-care of Heart Failure Model, relationships among self-care maintenance (including medication adherence), symptom monitoring, symptom recognition, self-care management and outcomes are described. Specifically, treatment adherence (e.g., medication adherence) is important to maintaining patient’s physiologic stability.11 Better adherence to self-care should lead to better health-related quality of life and reduce hospitalizations/death.11–15 Poor medication adherence is presumed to be associated with greater HF symptom burden.11, 13, 16 To our knowledge, the relationship between medication adherence and presence of HF symptoms has not been established in the current literature.16
It is not clear how HF symptoms, medication adherence, and hospitalization are related. Thus, the purposes of this study were to examine the relationship between medication adherence and HF symptoms and further explore the relationships among HF symptoms, medication adherence, and cardiac event-free survival in patients with HF. We tested whether the association between HF symptoms and the composite endpoint of event-free survival (i.e., time to cardiac-related hospitalizations or cardiac-related mortality) could be explained by medication adherence.
METHODS
Study Design
This was a secondary data analysis of two prospective studies in which medication adherence was measured objectively using the Medication Event Monitoring System (MEMS) and cardiac event-free survival was followed for up to 3 ½ years in patients with HF (both studies had similar mean follow-up days of 390+ days).9, 17 Both studies were designed to examine the relationships among demographic, psychosocial, and clinical factors, medication adherence, and health outcomes.8, 9, 17–23 The inclusion and exclusion criteria were identical in both studies. The data were collected between 2004–2007 for the first study and 2007–2009 for the second study. The attrition rate over time was low with less than 10% for each study. In the current study, we examined the relationships among HF symptoms, medication adherence, and cardiac event-free survival in patients with HF.
Samples and Setting
Detailed eligibility criteria and recruitment methods have been published previously.9, 17 Briefly, patients were recruited from either outpatient cardiology clinics or inpatient cardiology units. Patients who had a confirmed diagnosis of chronic HF and were on stable doses of HF medications were included. Patients were excluded if they had obvious cognitive impairment or a co-existing terminal illness.
Measurement of Variables
Heart Failure symptoms
HF symptoms were assessed using a single item from the Self-Care of Heart Failure Index (SCHFI). All participants were asked “In the past three months, have you had trouble breathing and/or ankle swelling? (Yes/No)” The SCHFI is a reliable, valid, and the most widely used instrument to measure self-care behaviors in patients with HF.24
Medication adherence
Medication adherence was assessed using the MEMS (AARDEX®-USA, Union City, CA). The MEMS data were collected for 3 months for the first study and 1 month for the second study. We used MEMS data to compute medication adherence. The MEMS has been used extensively in many patient populations (including patients with HF) and is a valid, objective, and sensitive method of determining medication adherence.25 The MEMS is the most commonly used electronic monitoring system and is considered the gold standard in measuring medication adherence.25, 26 The MEMS data were collected from one HF medication for each patient. We chose the medication to monitor based on the following criteria. First, we chose a medication that was taken twice a day. If all medications were taken twice or only once per day, then we chose the beta-adrenergic blocking agent unless the patient was not prescribed one. In those cases, the angiotension-converting-enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB) was used. If no beta-blocker or ACEI/ARB was prescribed, a diuretic (fixed dose, not as needed or adjustable one) was used in the MEMS device.
In this study, medication adherence was calculated as number of days the correct number of doses were taken (i.e., number of days the correct number of doses were taken during the monitoring period/total days during the monitoring period * 100%).8, 27, 28 Patients who took the correct number of doses ≥ 88% of days were defined as medication adherent, while those who took < 88% were as defined as medication nonadherent. This cutpoint was chosen based on a study demonstrating that adherence at or above 88% predicted better event-free survival.9
Cardiac event-free survival
We calculated time from baseline to the first cardiac event (a cardiac hospitalization or cardiac death which came first) as the outcome variable. Outcome data were collected monthly by patient phone calls, hospital record review, and review of death certificates. To determine whether an event was cardiac-related, a trained research assistant reviewed data from patient interviews, medical records and/or death certificates to determine if the event was cardiac-related. Any uncertain events were adjudicated by the principal investigators (JRW and DKM). The RA and the PIs were blinded to participants’ demographic and clinical data.
Other variables of interest
To completely describe the sample, compare differences in characteristics by groups, and obtain data on potential confounding variables, the following sociodemographic, clinical, and psychological data were collected.
Sociodemographics
Age, gender, marital status, race, and education level were collected from patient interview.
Clinical variables
Left ventricular ejection fraction (LVEF), etiology of HF, comorbidity (hypertension or diabetes), body mass index (BMI), and prescribed medications (ACEI/ARB and beta-blocker) were collected from the medical record and patient interview.
Procedure
Both studies were approved by the appropriate Institutional Review Boards. All patients provided informed, signed consent. Patients’ sociodemographic and clinical characteristics were collected by interview and medical record review at baseline. After completion of the baseline assessment, patients were given instructions on use of the MEMS bottle. Patients started to use the MEMS bottle at baseline. Patients returned the MEMS bottle after one or three months of continuous use. Patients were contacted monthly by phone to collect data regarding hospitalizations and death.
Data Management and Analysis
A significance level of ≤ .05 was chosen to indicate statistical significance. Study variables were summarized descriptively, including means and standard deviations or frequency distributions and quartiles, as appropriate to the level of measurement. We examined differences between adherent and nonadherent groups and between presence or absence HF symptom groups using independent t-tests and chi-square tests. Data analyses were performed using SPSS (IBM, Armonk, NY), version 23.0.
Kaplan-Meier and log-rank tests were used to compare the time to first cardiac event between patients in adherent and nonadherent groups, and in presence or absence of HF symptom groups. Cox proportional hazards regression modeling was used to assess the cardiac event-free survival between those who did and did not report HF symptom with and without adjusting for the following potential confounding variables: age, body mass index (BMI), and ACEI use (as these variables were different between groups, please see Table 1). We also controlled for gender, left ventricular ejection fraction (LVEF), etiology of HF, and diabetes as these factors might impact cardiac event-free survival.29–31 To account for differences between the two studies, we also controlled for study group (i.e., study 1 or study 2) in the final Cox regression models. We followed Baron and Kenny’s steps to test for mediation by conducting a series of logistic and Cox regression models (Figure 1).32
Table 1.
Sample Characteristics
| Characteristics | Without HF symptoms (n = 75) Mean ± SD or n (%) |
With HF symptoms (n = 144) Mean ± SD or n (%) |
p |
|---|---|---|---|
| Age | 63±11 | 59±12 | .018 |
| Female | 21 (28) | 56 (38.9) | .136 |
| White | 64 (85.3) | 122 (84.7) | 1.00 |
| Education: < high school | 16 (21) | 29 (20) | .372 |
| Marital status: married | 51 (68) | 82 (56.9) | .145 |
| LVEF, % | 37±14.9 | 35±13.9 | .426 |
| Body mass index | 30.6±6.9 | 33.1±7.8 | .021 |
| Heart attack | 41 (56.2) | 75 (53.2) | .772 |
| Diabetes | 28 (38.4) | 69 (47.9) | .196 |
| Taking ACEI | 63 (84) | 91 (63.6) | .002 |
| Taking beta-blocker | 70 (93.3) | 130 (90.3) | .614 |
| Study group: Study 1 Study 2 |
46 (61.3) 29 (38.7) |
90 (62.5) 54 (37.5) |
.884 |
| Intervention assignment: Intervention group |
20 (71.4) |
34 (64.2) |
.623 |
ACEI =angiotensin-converting-enzyme inhibitor; LVEF =left ventricular ejection fraction
Figure 1.
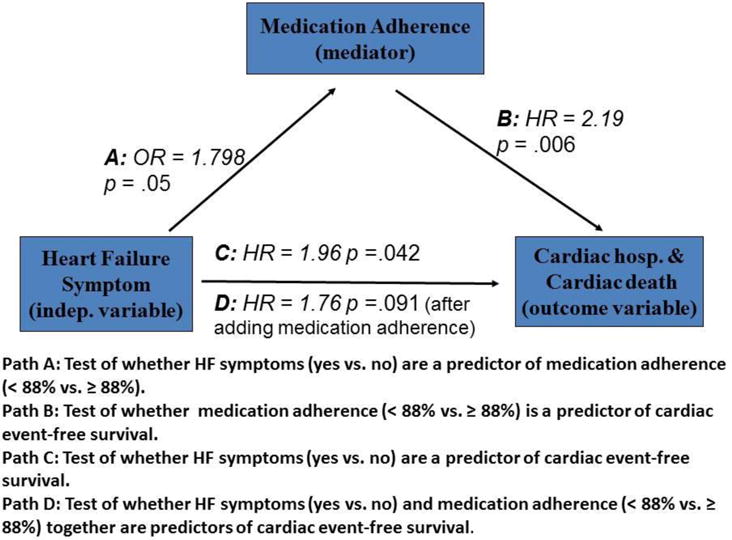
Testing the hypothesis that medication adherence is a mediator of the relationship between heart failure symptoms and cardiac event-free survival
RESULTS
Patient characteristics
Data from a total of 219 patients with HF were used in this study. The mean age of patients in the sample was 60 ± 12 years. About two thirds of patients were male. Fifteen percent of patients were African Americans. The average LVEF reflected enrollment of patients with and without systolic dysfunction: more than two fifths of the participants (42%) had HF with preserved systolic function (HFpEF, LVEF≥40%). The most common cause of HF was ischemic heart disease (50.2%). About one-fifth of the patients did not complete high school (21%). Most patients were unemployed (82%). There were 136 HF patients from study 1 and 83 HF patients from study 2. No demographic and clinical differences were found between subjects who participated from each study.
HF symptoms
About two thirds of the patients reported trouble breathing or ankle swelling (65.8%). Patients who reported HF symptoms were younger, had higher BMI, and were less likely to take ACE inhibitors compared with those who did not report HF symptoms. Age, BMI, and ACEI use were different between the two symptom groups. There were no differences between the two symptom groups in gender, race, education, marital status, LVEF, heart attack comorbidity, beta-blocker use, or study group (Table 1).
Medication adherence
Overall, 90 out of the 219 patients were categorized as nonadherent to prescribed HF medications (41%). A total of 46% of patients with HF symptoms were nonadherent to medication compared with 32% of patients without HF symptoms. In the unadjusted logistic regression model, patients with HF symptoms were 1.8 times more likely to be non-adherent compared with those without HF symptoms (odds ratio [OR] = 1.8, 95% CI: 1.00–3.23, p = .05).
HF symptoms and cardiac event-free survival
There were 50 cardiac events (4 cardiac deaths and 46 cardiac hospitalizations) during the follow-up period, with 38 events in patients who reported having HF symptoms in the last 3 months and 12 events in those who reported no HF symptoms. No difference in the prevalence of cardiac mortality between HF symptom groups was found (2.1% vs. 1.3% p =1.00). There was a significant difference in the composite end-point of cardiac hospitalizations or cardiac mortality between HF symptom groups (26.4% vs. 16%, p=.036). Kaplan-Meier plots and log-rank tests demonstrated that cardiac event-free survival was significantly worse in patients who had HF symptoms (p =. 039) (Figure 2).
Figure 2.
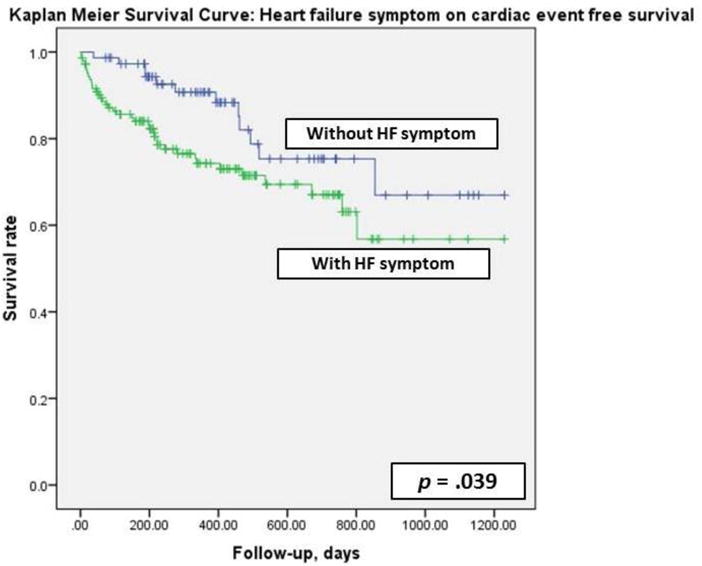
Heart failure symptoms and cardiac event-free survival
Mediation analysis
The first step of testing for mediation (Path A, Figure 1) explored whether HF symptoms were associated with medication adherence. There was an association between HF symptoms and medication adherence. Patients who reported HF symptoms were 80% more likely to be nonadherent to medication compared with those who did not report HF symptoms. In the second step (Path B), patients with medication nonadherence had a higher risk of experiencing a cardiac event. In the third mediation model (Path C), HF symptoms were associated with higher risk of experiencing a cardiac event. In the final model (Path D) that included both HF symptoms and medication adherence, HF symptoms were no longer a significant predictor of cardiac event-free survival with and without adjustment for all covariates (Table 2); this indicates complete mediation of the relationship between HF symptoms and cardiac event-free survival by medication adherence.
Table 2.
Cox Regression: Heart Failure Symptom and Medication Adherence§ on Cardiac Event-free Survival (N = 219)
| Variable | Hazard Ratio | 95% CI | Significance |
|---|---|---|---|
|
| |||
| Without covariate adjustment | |||
| *Step 1 | |||
| With HF symptoms | 1.961 | 1.023–3.758 | .042 |
| **Step 2 | |||
| With HF symptoms | 1.759 | .913–3.390 | .091 |
| Poor medication adherence | 2.035 | 1.157–3.578 | .014 |
|
| |||
| With covariate adjustment | |||
| †Step 1 | |||
| With HF symptoms | 2.053 | 1.022–4.124 | .043 |
| ‡Step 2 | |||
| With HF symptoms | 1.947 | .964–3.935 | .063 |
| Age | 1.00 | .974–1.027 | .988 |
| Female | 1.354 | .721–2.543 | .347 |
| Etiology of HF, non-ischemic | .610 | .310–1.200 | .152 |
| Left ventricular ejection fraction (%) | .985 | .961–1.009 | .211 |
| Body mass index | .966 | .925–1.009 | .120 |
| ACEI user | .992 | .491–2.003 | .982 |
| Diabetes | 1.193 | .645–2.208 | .574 |
| Study 1 | 1.148 | .620–2.218 | .660 |
| Poor medication adherence | 2.009 | 1.122–3.597 | .019 |
CI =confidence interval; ACEI =angiotensin-converting-enzyme inhibitor; NYHA =New York Heart Association
χ2 =4.274, p = .039;
χ2 = 10.775, p =.005;
χ2 = 13.105, p =.158;
χ2 = 18.618, p = .006
In the adjusted model with all covariates, none of the covariates were associated with cardiac event-free survival. In each adjusted regression model, all variance inflation factors were < 1.4, suggesting no parameter distortion due to multicollinearity.
DISCUSSION
In this study we explored the relationships among HF symptoms, medication adherence, and cardiac event-free survival in patients with HF and examined the mediating role of medication adherence in the relationship between HF symptoms and health outcomes. The most striking finding from this study was that medication adherence mediated the relationship between HF symptoms and cardiac event-free survival. Based on Riegel’s Self-care of Heart Failure Model, self-care maintenance behaviors, such as medication adherence in this study are essential to maintain a patient’s physiologic stability,11, 13 therefore, reduce HF symptoms, delay the progression of HF, and improve health-related outcomes such as rehospitalizations.12, 33–36
In our prior studies, we have found that medication adherence mediated the relationships between African-American race and worse outcomes,20 between depressive symptoms and worse outcomes,21 and between single marital status and worse outcomes.19 To our knowledge, this is the first study to provide evidence to support the important mediating role of medication adherence in the relationship between HF symptoms and worse outcomes. Thus, it is essential to develop effective interventions to improve medication adherence in patients with HF to improve a variety of health outcomes.
Our study confirms the hypothesis that better medication adherence, one of the major self-care maintenance behaviors, is associated with fewer HF symptoms. Lee proposed that effective self-care maintenance behaviors lead to better health outcomes through cardioprotective mechanisms, such as neurohormonal deactivation.16 For example, if patients with HF adhere to prescribed neurohormonal blockers (e.g., beta-blockers or angiotensin-converting-enzyme inhibitors), medication adherence will help minimize the cardiocirculatory burden from increased neurohormone levels (e.g., norepinephrine and angiotensin II).16
In the current literature on drug studies, use of neurohormonal blockers is associated with better functional capacity and health-related quality of life (HRQOL), lower symptom burden, and lower hospitalization and death rates.37–41 Yet, medication adherence was rarely evaluated, or had not been reported in these studies, so we are not sure whether positive health outcomes (better functional capacity and HRQOL, fewer HF symptoms and hospitalizations) can be attributed to adherence to neurohormonal blockers or to other causes such as better monitoring seen in clinical trials. Interestingly, in a trial to test the effect of a beta-blocker on mortality, investigators randomized 2,175 patients with myocardial infarction to receive propranolol or placebo, and found poor adherers were 2.6 times more likely than good adherers to die within a year of follow-up.42 Poor adherers had an increased risk of death whether they were on propranolol or placebo. Our findings provide evidence that better medication adherence is indeed related to lower symptom burden.
As expected, patients with HF symptoms in the past 3 months had a greater risk of experiencing a cardiac event than those without HF symptoms. In prior studies, HF symptoms such as shortness of breath and ankle swelling were indicators of acute HF exacerbation and the most common causes patients were admitted to the hospital.3–5, 43 In line with prior studies, poor medication adherence was one of the most common preventable precipitating factors for acute HF exacerbation.44, 45 Therefore, reducing HF symptoms can be an incentive to encourage patients with HF to improve/maintain medication adherence.
Our study has several limitations. First, the concept of HF symptoms is complex and multifaceted. It includes multiple elements (e.g., numbers, frequency, duration, and severity of HF symptoms, how much patients are distressed by their HF symptoms).46, 47 We measured presence of HF symptoms only one time (baseline) using a single item, yes/no question from the Self-Care of Heart Failure Index that might not capture the full spectrum of HF symptoms. However, our findings, which demonstrate a significant relationship between HF symptoms and medication adherence and between HF symptoms and outcomes, suggest that the concept of HF symptoms were accurately reflected by the self-report measure in this study. Nevertheless, given that patients have difficulty with symptom recognition, and HF patients’ symptoms might change in duration or severity over time;13, 43, 46–48 future studies of this phenomenon should use a scale to capture multi-dimensional HF symptoms longitudinally so that the complex dynamics surrounding HF symptoms, medication adherence and outcomes can be better illuminated. The single item question measure of HF symptoms may be insensitive to reflect HF symptoms and may produce unstable results that need to be verified in a future longitudinal study. Thus our findings should be considered exploratory and the need for replication emphasized.
Second, patients in our study were relatively younger than patients with HF in general. The difference might have resulted from recruiting most patients in this study in the outpatient settings and not the in-hospital settings. Third, we only monitored one HF medication in the MEMS as it is costly and burdensome to the patients for using multiple MEMS for multiple medications. However, previous investigators have demonstrated that monitoring one medication is sufficient to capture overall medication adherence.49, 50 Moreover, data were from 2 prospective studies collected in different time periods might introduce potential bias. Therefore, we controlled for original study group membership (Study 1 or 2) to account for potential differences between studies. Finally, although we included LVEF, etiology of HF, and diabetes as covariates in the statistical analysis, we acknowledge that patients with HF might have other concurrent conditions that may impact health outcomes that were not collected and controlled in our study.
CONCLUSION
We observed that patients with better medication adherence had fewer HF symptoms and that medication adherence mediated the relationship between HF symptoms and cardiac event-free survival. Therefore, it is imperative that clinicians educate/emphasize the importance of medication adherence to their HF patients to reduce HF symptoms and high hospitalization and mortality rates. Due to the importance of medication adherence and current low medication adherence rate, it is important to develop effective interventions to improve/sustain medication adherence to achieve better health outcomes in patients with HF.
Acknowledgments
FUNDING SOURCES
This study was supported by funding from the National Institute of Nursing Research (NINR): K23NR014489 (J. Wu, PI).
Footnotes
DISCLOSURES
None.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB, American Heart Association Statistics C, Stroke Statistics S Heart disease and stroke statistics–2015 update: A report from the american heart association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Pina IL, Trogdon JG, American Heart Association Advocacy Coordinating C, Council on Arteriosclerosis T, Vascular B, Council on Cardiovascular R, Intervention, Council on Clinical C, Council on E, Prevention, Stroke C Forecasting the impact of heart failure in the united states: A policy statement from the american heart association. Circulation. Heart failure. 2013;6:606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedman MM, Quinn JR. Heart failure patients’ time, symptoms, and actions before a hospital admission. The Journal of cardiovascular nursing. 2008;23:506–512. doi: 10.1097/01.JCN.0000338928.51093.40. [DOI] [PubMed] [Google Scholar]
- 4.Schiff GD, Fung S, Speroff T, McNutt RA. Decompensated heart failure: Symptoms, patterns of onset, and contributing factors. Am J Med. 2003;114:625–630. doi: 10.1016/s0002-9343(03)00132-3. [DOI] [PubMed] [Google Scholar]
- 5.Friedman MM. Older adults’ symptoms and their duration before hospitalization for heart failure. Heart & lung : the journal of critical care. 1997;26:169–176. doi: 10.1016/s0147-9563(97)90053-4. [DOI] [PubMed] [Google Scholar]
- 6.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008:Cd000011. doi: 10.1002/14651858.CD000011.pub3. [DOI] [PubMed] [Google Scholar]
- 7.Riegel B, Moser DK, Anker SD, Appel LJ, Dunbar SB, Grady KL, Gurvitz MZ, Havranek EP, Lee CS, Lindenfeld J, Peterson PN, Pressler SJ, Schocken DD, Whellan DJ. State of the science: Promoting self-care in persons with heart failure: A scientific statement from the american heart association. Circulation. 2009;120:1141–1163. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- 8.Wu JR, Moser DK, Chung ML, Lennie TA. Objectively measured, but not self-reported, medication adherence independently predicts event-free survival in patients with heart failure. Journal of cardiac failure. 2008;14:203–210. doi: 10.1016/j.cardfail.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu JR, Moser DK, De Jong MJ, Rayens MK, Chung ML, Riegel B, Lennie TA. Defining an evidence-based cutpoint for medication adherence in heart failure. American heart journal. 2009;157:285–291. doi: 10.1016/j.ahj.2008.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riegel B, Knafl GJ. Electronically monitored medication adherence predicts hospitalization in heart failure patients. Patient Prefer Adherence. 2013;8:1–13. doi: 10.2147/PPA.S54520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riegel B, Dickson VV. A situation-specific theory of heart failure self-care. The Journal of cardiovascular nursing. 2008;23:190–196. doi: 10.1097/01.JCN.0000305091.35259.85. [DOI] [PubMed] [Google Scholar]
- 12.Buck HG, Lee CS, Moser DK, Albert NM, Lennie T, Bentley B, Worrall-Carter L, Riegel B. Relationship between self-care and health-related quality of life in older adults with moderate to advanced heart failure. The Journal of cardiovascular nursing. 2012;27:8–15. doi: 10.1097/JCN.0b013e3182106299. [DOI] [PubMed] [Google Scholar]
- 13.Riegel B, Dickson VV, Faulkner KM. The situation-specific theory of heart failure self-care: Revised and updated. The Journal of cardiovascular nursing. 2015 doi: 10.1097/JCN.0000000000000244. [DOI] [PubMed] [Google Scholar]
- 14.Bennett SJ, Huster GA, Baker SL, Milgrom LB, Kirchgassner A, Birt J, Pressler ML. Characterization of the precipitants of hospitalization for heart failure decompensation. Am J Crit Care. 1998;7:168–174. [PubMed] [Google Scholar]
- 15.Lee CS, Moser DK, Lennie TA, Riegel B. Event-free survival in adults with heart failure who engage in self-care management. Heart & lung : the journal of critical care. 2011;40:12–20. doi: 10.1016/j.hrtlng.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee CS, Tkacs NC, Riegel B. The influence of heart failure self-care on health outcomes: Hypothetical cardioprotective mechanisms. The Journal of cardiovascular nursing. 2009;24:179–187. doi: 10.1097/JCN.0b013e31819b5419. quiz 188–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu JR, Corley DJ, Lennie TA, Moser DK. Effect of a medication-taking behavior feedback theory-based intervention on outcomes in patients with heart failure. Journal of cardiac failure. 2012;18:1–9. doi: 10.1016/j.cardfail.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu JR, Frazier SK, Rayens MK, Lennie TA, Chung ML, Moser DK. Medication adherence, social support, and event-free survival in patients with heart failure. Health Psychol. 2013;32:637–646. doi: 10.1037/a0028527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu JR, Lennie TA, Chung ML, Frazier SK, Dekker RL, Biddle MJ, Moser DK. Medication adherence mediates the relationship between marital status and cardiac event-free survival in patients with heart failure. Heart & lung : the journal of critical care. 2012;41:107–114. doi: 10.1016/j.hrtlng.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu JR, Lennie TA, De Jong MJ, Frazier SK, Heo S, Chung ML, Moser DK. Medication adherence is a mediator of the relationship between ethnicity and event-free survival in patients with heart failure. Journal of cardiac failure. 2010;16:142–149. doi: 10.1016/j.cardfail.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu JR, Lennie TA, Dekker RL, Biddle MJ, Moser DK. Medication adherence, depressive symptoms, and cardiac event-free survival in patients with heart failure. Journal of cardiac failure. 2013;19:317–324. doi: 10.1016/j.cardfail.2013.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu JR, Moser DK. Type d personality predicts poor medication adherence in patients with heart failure in the USA. Int J Behav Med. 2014;21:833–842. doi: 10.1007/s12529-013-9366-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu JR, Moser DK, Chung ML, Lennie TA. Predictors of medication adherence using a multidimensional adherence model in patients with heart failure. Journal of cardiac failure. 2008;14:603–614. doi: 10.1016/j.cardfail.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riegel B, Carlson B, Moser DK, Sebern M, Hicks FD, Roland V. Psychometric testing of the self-care of heart failure index. Journal of cardiac failure. 2004;10:350–360. doi: 10.1016/j.cardfail.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 25.Farmer KC. Methods for measuring and monitoring medication regimen adherence in clinical trials and clinical practice. Clin Ther. 1999;21:1074–1090. doi: 10.1016/S0149-2918(99)80026-5. discussion 1073. [DOI] [PubMed] [Google Scholar]
- 26.Cramer JA. Microelectronic systems for monitoring and enhancing patient compliance with medication regimens. Drugs. 1995;49:321–327. doi: 10.2165/00003495-199549030-00001. [DOI] [PubMed] [Google Scholar]
- 27.Cheng CW, Woo KS, Chan JC, Tomlinson B, You JH. Association between adherence to statin therapy and lipid control in hong kong chinese patients at high risk of coronary heart disease. Br J Clin Pharmacol. 2004;58:528–535. doi: 10.1111/j.1365-2125.2004.02202.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dobbels F, De Geest S, van Cleemput J, Droogne W, Vanhaecke J. Effect of late medication non-compliance on outcome after heart transplantation: A 5-year follow-up. J Heart Lung Transplant. 2004;23:1245–1251. doi: 10.1016/j.healun.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 29.Mullens W, Abrahams Z, Sokos G, Francis GS, Starling RC, Young JB, Taylor DO, Wilson Tang WH. Gender differences in patients admitted with advanced decompensated heart failure. The American journal of cardiology. 2008;102:454–458. doi: 10.1016/j.amjcard.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 30.Senni M, Gavazzi A, Oliva F, Mortara A, Urso R, Pozzoli M, Metra M, Lucci D, Gonzini L, Cirrincione V, Montagna L, Di Lenarda A, Maggioni AP, Tavazzi L. In-hospital and 1-year outcomes of acute heart failure patients according to presentation (de novo vs. Worsening) and ejection fraction. Results from in-hf outcome registry. Int J Cardiol. 2014;173:163–169. doi: 10.1016/j.ijcard.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 31.Bourassa MG, Gurne O, Bangdiwala SI, Ghali JK, Young JB, Rousseau M, Johnstone DE, Yusuf S. Natural history and patterns of current practice in heart failure. The studies of left ventricular dysfunction (solvd) investigators. Journal of the American College of Cardiology. 1993;22:14A–19A. doi: 10.1016/0735-1097(93)90456-b. [DOI] [PubMed] [Google Scholar]
- 32.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 33.Hauptman PJ. Medication adherence in heart failure. Heart Fail Rev. 2008;13:99–106. doi: 10.1007/s10741-007-9020-7. [DOI] [PubMed] [Google Scholar]
- 34.Heo S, Doering LV, Widener J, Moser DK. Predictors and effect of physical symptom status on health-related quality of life in patients with heart failure. Am J Crit Care. 2008;17:124–132. [PubMed] [Google Scholar]
- 35.Zambroski CH, Moser DK, Bhat G, Ziegler C. Impact of symptom prevalence and symptom burden on quality of life in patients with heart failure. European journal of cardiovascular nursing : journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology. 2005;4:198–206. doi: 10.1016/j.ejcnurse.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 36.Moser DK, Yamokoski L, Sun JL, Conway GA, Hartman KA, Graziano JA, Binanay C, Stevenson LW. Improvement in health-related quality of life after hospitalization predicts event-free survival in patients with advanced heart failure. Journal of cardiac failure. 2009;15:763–769. doi: 10.1016/j.cardfail.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL. 2013 accf/aha guideline for the management of heart failure: Executive summary: A report of the american college of cardiology foundation/american heart association task force on practice guidelines. Circulation. 2013;128:1810–1852. doi: 10.1161/CIR.0b013e31829e8807. [DOI] [PubMed] [Google Scholar]
- 38.Armstrong PW, Moe GW. Medical advances in the treatment of congestive heart failure. Circulation. 1993;88:2941–2952. doi: 10.1161/01.cir.88.6.2941. [DOI] [PubMed] [Google Scholar]
- 39.Fonarow GC, Abraham WT, Albert NM, Stough WG, Gheorghiade M, Greenberg BH, O’Connor CM, Sun JL, Yancy C, Young JB. Carvedilol use at discharge in patients hospitalized for heart failure is associated with improved survival: An analysis from organized program to initiate lifesaving treatment in hospitalized patients with heart failure (optimize-hf) American heart journal. 2007;153:82 e81–11. doi: 10.1016/j.ahj.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 40.Ghali JK, Tam SW, Ferdinand KC, Lindenfeld J, Sabolinski ML, Taylor AL, Worcel M, Curry CL, Cohn JN. Effects of ace inhibitors or beta-blockers in patients treated with the fixed-dose combination of isosorbide dinitrate/hydralazine in the african-american heart failure trial. Am J Cardiovasc Drugs. 2007;7:373–380. doi: 10.2165/00129784-200707050-00007. [DOI] [PubMed] [Google Scholar]
- 41.Bouzamondo A, Hulot JS, Sanchez P, Cucherat M, Lechat P. Beta-blocker treatment in heart failure. Fundam Clin Pharmacol. 2001;15:95–109. doi: 10.1046/j.1472-8206.2001.00019.x. [DOI] [PubMed] [Google Scholar]
- 42.Horwitz RI, Viscoli CM, Berkman L, Donaldson RM, Horwitz SM, Murray CJ, Ransohoff DF, Sindelar J. Treatment adherence and risk of death after a myocardial infarction. Lancet. 1990;336:542–545. doi: 10.1016/0140-6736(90)92095-y. [DOI] [PubMed] [Google Scholar]
- 43.Sethares KA, Chin E, Jurgens CY. Predictors of delay in heart failure patients and consequences for outcomes. Curr Heart Fail Rep. 2015;12:94–105. doi: 10.1007/s11897-014-0241-5. [DOI] [PubMed] [Google Scholar]
- 44.Michalsen A, Konig G, Thimme W. Preventable causative factors leading to hospital admission with decompensated heart failure. Heart. 1998;80:437–441. doi: 10.1136/hrt.80.5.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Opasich C, Rapezzi C, Lucci D, Gorini M, Pozzar F, Zanelli E, Tavazzi L, Maggioni AP. Precipitating factors and decision-making processes of short-term worsening heart failure despite “optimal” treatment (from the in-chf registry) The American journal of cardiology. 2001;88:382–387. doi: 10.1016/s0002-9149(01)01683-6. [DOI] [PubMed] [Google Scholar]
- 46.Jurgens CY. Somatic awareness, uncertainty, and delay in care-seeking in acute heart failure. Res Nurs Health. 2006;29:74–86. doi: 10.1002/nur.20118. [DOI] [PubMed] [Google Scholar]
- 47.Jurgens CY, Hoke L, Byrnes J, Riegel B. Why do elders delay responding to heart failure symptoms? Nurs Res. 2009;58:274–282. doi: 10.1097/NNR.0b013e3181ac1581. [DOI] [PubMed] [Google Scholar]
- 48.Riegel B, Dickson VV, Cameron J, Johnson JC, Bunker S, Page K, Worrall-Carter L. Symptom recognition in elders with heart failure. J Nurs Scholarsh. 2010;42:92–100. doi: 10.1111/j.1547-5069.2010.01333.x. [DOI] [PubMed] [Google Scholar]
- 49.Bouvy ML, Heerdink ER, Urquhart J, Grobbee DE, Hoes AW, Leufkens HG. Effect of a pharmacist-led intervention on diuretic compliance in heart failure patients: A randomized controlled study. Journal of cardiac failure. 2003;9:404–411. doi: 10.1054/s1071-9164(03)00130-1. [DOI] [PubMed] [Google Scholar]
- 50.Dunbar-Jacob J, Bohachick P, Mortimer MK, Sereika SM, Foley SM. Medication adherence in persons with cardiovascular disease. The Journal of cardiovascular nursing. 2003;18:209–218. doi: 10.1097/00005082-200307000-00006. [DOI] [PubMed] [Google Scholar]


