Abstract
Gambling problems impact 0.2%-4.0% of the population, and research related to treating gambling has burgeoned in the last decades. This paper reviews trials for psychosocial treatments of gambling problems. Using Preferred Reporting Items for Systematic reviews and Meta-Analyses standards, we identified 21 randomized trials. Eleven studies evaluated interventions delivered via multi-session, in-person therapy: cognitive therapies, cognitive-behavioral (CB) therapies, and motivational interventions (MI) alone or with CB therapies. An additional ten studies used approaches that involved one or fewer in-person sessions; these included workbooks with CB exercises alone or in combination with MI and brief feedback or advice interventions. Although most studies found some benefits of CB therapy (alone or combined with MI) and brief feedback or advice relative to the control condition in the short term, only a handful of studies demonstrated any long-term benefits. Nearly half the studies used waitlist controls, precluding an understanding of long-term efficacy, and standardized outcomes measures are also lacking. Populations also differ markedly across studies, from non-treatment seeking persons who screened positive for gambling problems to those with severe gambling disorder, and these discrepant populations may require different interventions. Although problem gamblers with less pronounced symptoms may benefit from very minimal interventions, therapist contact generally improved outcomes relative to entirely self-directed interventions, and at least some therapist contact may be necessary for patients with more severe gambling pathology to benefit from CB interventions. As treatment services for gambling continue to grow, this review provides timely information on best practices for gambling treatment.
Keywords: gambling, treatment, psychotherapy, review
Gambling problems have impacted most all cultures since the beginning of recorded history. In the United States (US) and elsewhere throughout the world, the past few decades have witnessed a rapid acceleration in gambling opportunities. Perhaps in parallel with these societal changes, scientific understanding of this condition and its treatment has advanced markedly.
Gambling disorder is characterized by financial, psychological, employment, and relationship difficulties related to excessive wagering (American Psychiatric Association, 2013). In extreme cases, it can lead to legal problems as well. In a large meta-analysis of prevalence studies from around the world, between 0.2% and 2.1% of the population develops gambling disorder (Stucki & Rihs-Middel, 2007). An even larger proportion (0.5% to 4.0%) experiences some degree of difficulties with gambling, but not as severe as those classified by gambling disorder (Stucki & Rihs-Middel, 2007). In college students, the rates appear to be even higher. Nowak and Aloe (2014) conducted a meta-analysis of college student surveys and found an estimated 10% have gambling problems. Throughout this paper, “problem gamblers” or “problem gambling” will refer to a heterogeneous group of persons or conditions encompassing gambling disorder and its subthreshold symptoms.
Few people seek treatment for gambling. Of those with gambling disorder, less than 15% receive treatment (Slutske, 2006), and almost none with less severe problems do (Petry, 2005). In part, low participation in treatment relates to limited availability of services as well as a lack of insurance coverage for gambling treatment, at least in the US. Most professional treatment, in the US and throughout the world, occurs in specialized gambling treatment clinics. The types of treatments these clinics provide are usually eclectic and varied in nature, boding the question of whether they should adapt theoretically or evidence-based treatments, to the extent they exist.
Now that gambling disorder is classified alongside substance use disorders in the fifth revision of the Diagnostic and Statistical Manual for Mental Disorders (DSM; American Psychiatric Association, 2013), interest in and demand for treatment may increase (Petry et al., 2014). Substance abuse treatment providers as well as other mental health clinicians may begin screening for gambling problems and providing treatment when indicated. Due to the high comorbidities of substance use and gambling disorders (Kessler et al., 2008; Petry, Stinson, & Grant, 2005), many cases of gambling problems are likely to be identified. Choice of treatments should be guided by an understanding of efficacious, or at least potentially effective, interventions.
A meta-analysis of gambling treatments was published over a decade ago (Pallesen, Mitsem, Kvale, Johnsen, & Molde, 2005), along with a Cochrane review (Cowlishaw et al., 2012). In addition, theoretical (Rash & Petry, 2014; Stea & Hodgins, 2011) and specific reviews exist for motivational interviewing (Yakovenko, Quigley, Hemmelgarn, Hodgins, Ronksley, 2015) and the treatment of dual diagnosis gamblers (Dowling, Merkouris, & Lorains, 2016). These reviews generally conclude there appears some evidence of efficacy, at least in the short term, for cognitive-behavioral and motivational interventions. However, many identified studies suffered from limitations in design, as well as measurement and analyses of outcomes. Since the comprehensive Cochrane review, which is now over five years old, additional treatment studies have been conducted.
To guide treatment and research for gambling problems, this paper provides an up-to-date narrative review of interventions that have been studied empirically. Following the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA; Moher, Liberati, Tetzlaff, Altman, & PRISMA Group, 2009) standards, we summarize types of treatments from randomized trials, as well as the designs and results from these studies. Based on this review, the paper outlines recommendations for future research in treating gambling problems.
Methods
We conducted a systematic search using the PRISMA guidelines (Moher et al., 2009), initially on Pubmed Central for studies published through September 2016. A combination of MESH terms, wildcards and key words were included: (gambling OR gamble*) AND (therapy OR treatment OR intervention) AND random*. We performed additional searches for non-overlapping publications on other databases such as EBSCOhost, PsychInfo, and PsychArticles. We manually searched reference sections from articles and gambling specific journals not indexed in these databases.
Inclusion criteria for this review were: administration of any psychological intervention (e.g., individual, group, workbook, Internet/computerized, or self-help) for gambling problems (defined as meeting diagnostic criteria or based on responses to a questionnaire designed to assess sub-diagnostic threshold gambling problems); random assignment to two or more conditions; at least 25 participants per condition (Chambless & Hollon, 1998); and published in the English language. Studies that presented long-term follow-up data from a randomized trial and that met these criteria were also included.
Studies were excluded if they involved pharmacotherapy as a study treatment condition (because medication may exert effects on gambling independent of psychotherapies), but we did not exclude studies that recruited patients who were taking medications clinically (i.e., on their own and not part of the research study). We also excluded studies that did not provide treatment directly to individuals experiencing gambling problems (i.e., those treating significant others of gamblers, prevention interventions delivered to individuals who have not yet experienced problems related to gambling). A comprehensive listing of full text studies reviewed and excluded for specific reasons is available upon request from the authors.
Data extraction and synthesis
For included studies, we present information about the specific type of treatment(s) for gambling along with the control or comparator conditions. We present data for numbers randomized, expected number of sessions and duration of treatment and follow-up, along with proportions of patients completing multi-session interventions, and the significance and direction of results on primary gambling outcome measures. A second author independently coded a randomly selected third of the studies, and the overall inter-rater agreement was 96%. Discussions resolved any discrepancies, with only one or two each related to: population/study inclusion criteria, treatment duration, and initial results.
Effects of experimental interventions relative to control or other active conditions on gambling outcomes focus on indices of clinically significant improvements (Jacobson & Truax, 1991). We describe intent-to-treat analyses when possible, presuming that participants who did not complete follow-ups continued gambling problematically. We also review other indices of gambling behaviors (e.g., expenditure or frequency of gambling) or gambling symptom severity (e.g., global assessments of gambling harms from questionnaires). Outcomes are detailed for the post-treatment assessment (or the initial assessments following randomization for single session interventions) and for the most distal follow-up.
Indices of gambling outcomes varied across studies, and studies did not use parallel definitions of clinically significant improvements (i.e., no longer meeting DSM criteria, or substantial reductions in gambling along one or more domains, which differed across studies). Further, some studies relied upon single item responses (i.e., for cravings or urges) or assessment tools with limited information on psychometric properties. Amount gambled is a commonly reported metric, but it can reflect money risked, lost, or both (or undefined), and it is non-normally distributed and influenced by income as well as severity of problems. Days gambled is also often non-normally distributed, and a person who buys one lottery ticket per day, for example, will have a high value on this index, but not necessarily experience gambling difficulties. Because types, measurement and presentation of outcomes differed markedly across studies and in some cases were clearly biased (e.g., only significant differences reported, or only treatment or follow-up completers included), a meta-analysis of specific outcomes would likely provide misleading conclusions (Higgins & Green, 2011). Compounding these concerns, the populations studied ranged from patients meeting diagnostic criteria and explicitly seeking gambling treatment to persons identified with relatively mild gambling problems via study specific screening procedures such as South Oaks Gambling Screen (Lesieur & Blume, 1987) scores. Therefore, this review is narrative and focuses on global issues related to the study designs and outcomes.
Results and Discussion
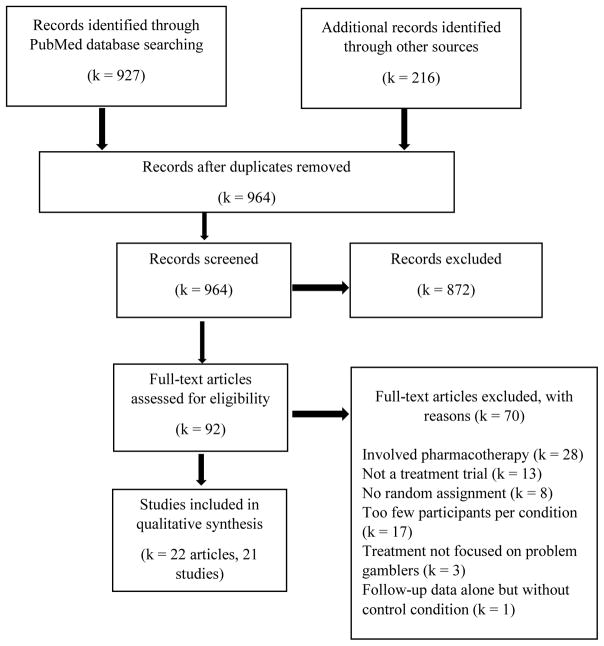
A total of 22 trials met inclusion and not exclusion criteria (Figure 1). Most described primary outcomes, and one provided follow-up data from two conditions to which patients in one of the primary trials were randomized. Table 1 lists studies that evaluated interventions that involved more than one in-person session with a therapist. Table 2 outlines studies that focused primarily on brief, single session interventions (with some also providing written materials) or those involving no in-person contact with a therapist.
Figure 1.
Records identified and reviewed.
Table 1.
Studies evaluating interventions that included more than one in-person session.
| First author year | Treatments | N | Treatment duration (sessions) | % Completed treatment | Significant effects post treatment relative to control or other active | Follow-up (wks) | Long term outcomes |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Cognitive | |||||||
| Ladouceur 2001 | Waitlist | 29 | -- | -- | Benefits on % Improved , $, Days, and DSM criteria | -- | -- |
| Cognitive therapy | 59 | 12 wks (≤20) | ~ 50% | ||||
|
| |||||||
| Ladouceur 2003 | Waitlist | 25 | -- | -- | Benefits on % Improved and DSM criteria | -- | -- |
| Cognitive therapy (group) | 46 | 10 wks (10) | 74% | ||||
|
| |||||||
| Smith 2015 | Exposure therapy | 43 | 12 wks (12) | 49% | No differences on % Improved or VGS. | 26 | No differences. |
| Cognitive therapy | 44 | 12 wks (12) | 68% | ||||
|
| |||||||
| Cognitive-behavioral | |||||||
|
| |||||||
| Petry 2006 | GA referral | 63 | -- (1) | -- | Benefits of CB therapy on % Im- proved and $. Benefits of both CB types on SOGS, ASI-G, and Days. | 52 | Benefits of CB (workbook or therapy) on ASI-G and SOGS but not other indices. |
| CB workbook | 84 | 8 wks (8) | 37% | ||||
| CB therapy | 84 | 8 wks (8) | 61% | ||||
|
| |||||||
| Campos 2013 | CB workbook | 40 | 20 wks (6) | ~50% | Benefits on % Abstinent and G- SAS but not $. | 52 | No differences. |
| CB workbook + support | 47 | 20 wks (6) | |||||
|
| |||||||
| Oei 2010 | Waitlist | 28 | -- | 68% | No differences on % Improved, $, or Days. | 26 | No differences. |
| CB therapy (group) | 37 | 6 wks (6) | 78% | ||||
| CB therapy (individual) | 37 | 6 wks (6) | 95% | ||||
|
| |||||||
| Motivational | |||||||
|
| |||||||
| Grant 2009 | GA referral | 35 | -- (1) | -- | Benefits on % Abstinent and PG- YBOCS. | na | -- |
| MI + CB therapy | 33 | 8 wks (6) | 76% | ||||
|
| |||||||
| Larimer 2012 | Assessment | 51 | -- | -- | Benefits of Personal Feedback on frequency, and of both interventions on DSM. No differences on $. | na | -- |
| MI + Personal feedback | 52 | 1 (1) | 88% | ||||
| CB therapy (group) | 44 | 6 wks (4-6) | <41% | ||||
|
| |||||||
| Carlbring 2010 | Waitlist | 46 | -- | -- | Both treatments equally reduced NODS. | 52 | No differences. |
| MI | 54 | 8 wks (4) | ~43% | ||||
| CB therapy (group) | 50 | 8 wks (8) | ~29% | ||||
|
| |||||||
| Petry 2008 | Assessment | 48 | -- | -- | Benefits of Brief Advice on % Improved, $ and ASI-G. | 39 | Benefits of Brief Advice on % Improved, and of MI + CB Therapy on ASI-G. No effects on $. |
| Brief advice | 37 | 1 (1) | 100% | ||||
| MI | 55 | 1(1) | 94% | ||||
| MI + CB therapy | 40 | 4 wks (4) | 33% | ||||
|
| |||||||
| Petry 2016 | Brief education | 69 | 1 (1) | 100% | Benefits of Brief Advice on Days. Benefits of MI + CB Therapy vs Brief Advice on % Improved, $, and SOGS. | 104 | Benefits of MI + CB Therapy vs Brief Advice on % Improved and $, but not Days or SOGS. |
| Brief advice | 66 | 1 (1) | 100% | ||||
| MI + CB therapy | 82 | 4 wks (4) | 28% | ||||
Notes: CB = Cognitive Behavioral; GA = Gamblers Anonymous; MI = Motivational Interviewing; DSM = Diagnostics and Statistical Manual of Mental Disorders (4th ed.) criteria for pathological gambling; VGS = Victorian Gambling Screen harm to self scale; SOGS = South Oaks Gambling Screen; ASI-G = Addiction Severity Index- Gambling scale; G-SAS = Gambling Symptom Assessment Scale; PG-YBOCS: Yale-Brown Obsessive-Compulsive Scale for Pathological Gambling; NODS = National Opinion Research Center DSM-IV Screen for Gambling Problems; na = not applicable;
Table 2.
Studies evaluating interventions that involved no or one in-person sessions.
| First author, year | Treatments | N | Treatment duration (sessions) | % Comp- lete | Significant effects post treatment relative to control or other active conditions | Follow up (wks) | Long term outcomes relative to non- waitlist condition |
|---|---|---|---|---|---|---|---|
|
| |||||||
| CB workbook | |||||||
|
| |||||||
| Hodgins 2001 | Waitlist | 35 | 4 wks | -- | Benefits of CB workbook + MI call on % Improved, $ and Days. | 104 | Benefits on % Improved, $, Days and SOGS (Hodgins, 2004). |
| CB workbook | 35 | 4 wks | 56% | ||||
| CB workbook + MI call | 32 | 4 wks (1) | overall | ||||
|
| |||||||
| Hodgins 2009 | Waitlist | 65 | 6 wks | Not reported | Benefits of CB workbook + both call conditions on $, Days, and G- SAS but not % Improved. | 52 | No differences. |
| CB workbook | 82 | 6 wks | |||||
| CB workbook + MI call | 83 | 6 wks (1) | |||||
| CB workbook + MI calls | 84 | 36 wks (7) | |||||
|
| |||||||
| LaBrie 2012 | Waitlist | 102 | 12 wks | Not reported | No differences on % Abstinent, $ or Days. | 13 | No differences. |
| MI/CB workbook | 108 | 12 wks | |||||
| MI/CB workbook + call | 105 | 12 wks (1) | |||||
|
| |||||||
| Diskin 2009 | CB workbook + control interview | 39 | 1 (1) | 50% | .. | 52 | Benefits on $ but not Days or % Improved. |
| CB workbook + MI | 42 | 1 (1) | 64% | ||||
|
| |||||||
| Hodgins 2007 | CB workbook | 85 | 1 | 63% | No differences on % Improved, $ or Days. | 52 | No differences. |
| CB workbook multiple mailings | 84 | 44 wks (8) | overall | ||||
|
| |||||||
| Carlbring 2008 | Waitlist | 32 | -- | -- | Benefits on NODS. | na | -- |
| Internet CB + support | 34 | 8 wks | 50% | ||||
|
| |||||||
| Luquiens 2016 | Waitlist | 264 | 6 wks | -- | No differences on PGSI. | 12 | No differences. |
| 293 | 22% | ||||||
| Email + CB workbook | 264 | 17% | |||||
| Email, CB workbook & guidance | 301 | 5% | |||||
|
| |||||||
| Feedback | |||||||
|
| |||||||
| Cunningham 2012 | Waitlist | 69 | -- | -- | No differences on $ or Days. | 53 | Benefits of MI partial vs full feedback on Days, but not $. |
| Partial feedback | 70 | 1 (1) | 100% | ||||
| Full feedback | 70 | 1 (1) | 100% | ||||
|
| |||||||
| Neighbors 2015 | Attention control | 128 | 1 (1) | 100% | Benefits on $ and SOGS but not Days. | 26 | Benefits on $ but not Days or SOGS. |
| Feedback via computer | 124 | 1 (1) | 100% | ||||
|
| |||||||
| Martens 2015 | Assessment | 109 | -- | Not reported | Benefits of Personalized Feedback on $ and CPGI but not Days. No differences Education vs Personalized feedback. | na | -- |
| Education | 113 | 1 (1) | |||||
| Personalized feedback | 111 | 1 (1) | |||||
Notes: CB = Cognitive Behavioral; MI = Motivational Interviewing; G-SAS = Gambling Symptom Assessment Scale; NODS = National Opinion Research Center DSM-IV Screen for Gambling Problems; PGSI = Problem Gambling Severity Index; SOGS = South Oaks Gambling Screen CPGI = Canadian Problem Gambling Inventory; na = not applicable.
Table 1 lists studies based on treatment type. It presents studies on cognitive therapies first, followed by cognitive-behavioral therapies. Other studies evaluated these interventions in conjunction with or in comparison to motivational interventions (MI), and section 3 outlines these studies. Initially, we briefly describe rationales for the therapies and then outcomes from studies examining them.
1. Cognitive therapies
Cognitive distortions, or erroneous beliefs that one can control or predict outcomes of chance events, are common (Fortune & Goodie, 2012), and cognitive therapies attempt to alter these thoughts in problem gamblers. In one of the first studies to examine cognitive therapy for gambling problems, Ladouceur et al. (2001) in Canada randomized 59 patients with gambling disorder to a waitlist control or cognitive therapy. About half of those assigned to cognitive therapy completed treatment, which involved up to 20 sessions or until gambling ceased. After adjusting for an intent-to-treat analysis including all patients randomly assigned and assuming those who did not finish treatment or assessments were gambling problematically, 32% of those assigned to cognitive therapy had clinically significant improvements in gambling on a global index versus only 7% of those assigned to the waitlist condition. Those who completed the full course of cognitive therapy also decreased amounts spent and days gambled relative to those in the waitlist condition, but these analyses did not adjust for treatment non completion or missing data.
A subsequent study in Canada applied this same cognitive therapy in a group format. Ladouceur et al. (2003) randomized 71 patients with gambling disorder to a waitlist control or cognitive therapy delivered in a group format. Of those in the cognitive therapy condition, 74% completed all ten sessions. In applying an intent-to-treat analysis, 43% of those who received cognitive therapy substantially reduced gambling versus 8% in the waitlist condition. Benefits were also reported on DSM-based gambling criteria, but these results included only treatment completers.
In Australia, Smith, Battersby, Harvey, Pols and Ladouceur (2015) compared this cognitive therapy to a behavioral treatment, exposure therapy, in which patients encountered gambling situations without wagering. They randomized 87 patients to one of the two conditions. Both groups reduced gambling as assessed by the Victorian Gambling Screen (VGS) at a 3-month follow-up, with no differences between conditions. At the 6-month follow-up, 79% of cognitive therapy and 83% of exposure therapy participants were improved using VGS scores, and these rates again did not differ.
Across these three randomized trials evaluating cognitive therapy, between a quarter and half of patients offered it did not engage in or complete it. Nevertheless, cognitive therapy appears to have some short-term benefits compared to a waitlist control. Waitlist conditions are appropriate for initially evaluating new treatments, but they cannot address long-term effects because these participants are offered the therapy after the waiting period is over. Additionally, waitlist conditions cannot control for general therapy effects, or expectations of patients who seek, and are hoping to receive, an intervention. To date, there are no available data suggesting long-term efficacy of cognitive therapy for treating gambling disorder, and relative to an active control condition (exposure therapy), cognitive therapy had no benefits in the short or long term.
2. Cognitive-behavioral therapy
Cognitive-behavioral (CB) therapy integrates aspects of cognitive therapy along with behavioral interventions. Typically, it involves identifying external triggers for gambling, practicing alternative responses to cues or triggers, and promoting alternatives to gambling (see Petry, 2005). In the US, Petry et al. (2006) randomized 231 participants with gambling disorder to one of three conditions: referral to Gamblers Anonymous (GA), referral to GA along with a CB workbook, or referral to GA plus CB therapy, comprised of the same CB exercises as the workbook but a therapist delivered them in individual therapy sessions. This study did not employ a waitlist condition and therefore could evaluate long-term efficacy relative to GA referral, the standard of care in the US. Participation in GA was similar across all conditions, but only 37% of those assigned to the CB workbook condition completed 6 or more chapters while 61% of those receiving CB therapy attended at least 6 sessions. At the end of treatment, significantly more participants in the individual CB therapy condition no longer met DSM criteria for gambling disorder (69%) than in the other conditions: 51% for the CB workbook and 47% for the GA referral alone condition. Using an intent-to-treat analysis, those assigned to either CB condition (workbook or individual therapy) evidenced significantly greater improvements than those assigned to GA referral alone on days gambled, as measured by South Oaks Gambling Screen (SOGS; Lesieur & Blume, 1987) scores and Addiction Severity Index-Gambling (ASI-G; Petry, 2003) scores. Those in the CB therapy group also wagered lower amounts than those in the CB workbook group. At the 12-month follow-up, about 60% overall had clinically significant improvements in gambling, which did not differ by group. Groups also did not differ in terms of days or dollars wagered, but significant benefits of CB treatment remained for decreasing severity of gambling problems long-term on two indices of gambling problems: SOGS and ASI-G scores.
In the US, Campos et al. (2015) examined whether therapist guidance improved outcomes in persons receiving a CB workbook. In this study, 87 problem gamblers received a CB workbook, with half randomized to meet with a therapist for support and review of materials in 5 sessions. The other half received brief check-ins with a research assistant about workbook completion at the same frequency. Although benefits of therapist support were reported on proportion abstinent and a global index of gambling problems at the post treatment assessment, half or more of the patients failed to complete follow-ups. No differences were noted between groups on dollars wagered in the short term and there were no long-term differences between groups.
Oei, Raylu and Casey (2010) randomized 102 patients in Australia with gambling disorder to a waitlist condition, CB therapy delivered in an individual format, or CB therapy delivered in a group format. There were no significant differences across groups on any index, including dollars and days gambled or gambling urges or cognitions. The proportions considered improved post treatment relative to pre-treatment were 68%–93% across groups and did not differ by treatment assignment.
To summarize, one study of CB treatment (Petry et al., 2006) found some benefits for reducing gambling over the short- and long-term relative to a referral to GA control condition. Another study (Campos et al., 2015) also reported potential short-term benefits of therapist support when combined with CB treatment relative to the CB workbook alone. A third study found no differences between CB therapy when delivered in an individual or group format compared to a waitlist control condition. Although only these three studies have evaluated in-person delivery of CB treatment as a standalone intervention, many others have combined CB approaches with another form of treatment, motivational interventions.
3. Motivational interventions with or without CB treatment
In the above studies, up to two-thirds of participants who sought treatment and were randomized to cognitive or CB therapy did not become actively engaged in or complete it. Motivational interventions (MI) are designed to enhance engagement in treatment and address ambivalence while guiding patients toward healthy behavioural choices. They can be standalone interventions or included alongside CB treatments.
In the US, Grant et al. (2009) added MI to Petry’s (2005) CB therapy, and they also included a specific module on imaginal desensitization. They randomized 68 patients to referral to GA or MI + CB therapy. Two months later, patients in MI + CB therapy were more likely to have achieved a month of gambling abstinence (64%) than those in GA referral (17%), and significant differences were noted on composite indices of gambling. After the post-treatment period, those in the GA referral condition received MI + CB therapy, so long-term efficacy could not be examined.
In another study from the US, Larimer et al. (2012) also used the CB content from Petry (2005) and applied it in group format. They randomly assigned 147 college student problem gamblers to an assessment only control, a single MI session that included personalized feedback about gambling, or 4-6 sessions of CB therapy delivered in groups. Both the MI feedback and CB therapy conditions decreased DSM gambling symptoms versus the control, with only the MI feedback condition reducing frequency of gambling.
Carlbring, Jonsson, Josephson and Forsberg (2010) randomized 150 problem gamblers from Sweden to a waitlist control, four individual sessions of MI, or eight sessions of CB therapy delivered in group format. Both MI and CB therapies resulted in improvements on an index of DSM gambling criteria relative to the waitlist, with no differences between the two active treatments in the short- or long-term.
Petry, Weinstock, Ledgerwood and Morasco (2008) screened US patients at medical and substance abuse treatment clinics for gambling problems. A total of 180 patients identified with problem gambling were randomly assigned to: assessment only, 10 minutes of Brief Advice about ways to reduce gambling problems, a single MI session, or an MI session plus three sessions of CB therapy, modeled after that in Petry (2005). Six weeks after randomization, proportions clinically improved were higher in the Brief Advice (66%) than control condition (47%), with intermediary effects in the other conditions (50-54%). Those receiving Brief Advice also reduced amounts wagered and ASI-G scores compared to the control condition at the initial post-intervention assessment. Brief Advice was the only intervention that yielded significant benefits relative to the control condition on proportions improved nine months later, with 71% improved versus 48% in the control condition, and 59% in the other conditions. The MI + CB therapy condition had significant effects on ASI-G scores compared to the assessment control throughout the 9-month follow-up period. No intervention reduced amounts wagered relative to the control condition in the long-term, and none of the active interventions differed significantly from one another.
In a subsequent study involving an active control for Brief Advice, Petry, Rash and Alessi (2016) randomly assigned 217 US substance abuse treatment patients who screened positive for problem gambling to: Brief Psychoeducation about gambling, Brief Advice, or one session of MI plus 3 sessions of CB therapy. Although few in MI + CB therapy completed it, this condition resulted in the best short-and long-term outcomes. Five months after randomization, 46% of patients assigned to MI + CB therapy had clinically significant reductions in gambling versus 34% in Brief Psychoeducation and 28% in Brief Advice. Significant improvements in the short term were noted for Brief Advice relative to Brief Psychoeducation in terms of days wagered, while MI + CB led to improvements compared to Brief Advice on dollars wagered and SOGS scores. Compared to Brief Advice, MI + CB continued to yield benefits for dollars wagered throughout a two-year follow-up. Patients in this condition also had a higher rate of clinically significant reductions in gambling; at the 2-year follow-up, proportions improved were 77%, 64%, and 69% in MI + CB therapy, Brief Psychoeducation, and Brief Advice conditions, respectively.
As Table 1 shows, only two studies evaluated MI on its own. One found effects on gambling (Carlbring et al., 2010) while the other did not (Petry et al., 2008), and in both studies MI had similar outcomes to a CB therapy. A combined MI + CB therapy approach yielded some benefits in all studies in which it was assessed (Grant et al., 2009; Petry et al., 2008, 2016), although it is unclear if integrating MI improves professionally delivered CB therapy because no studies used a dismantling design. Treatment completion rates were low in most studies, and especially for non-treatment seeking gamblers such as college students and substance abuse treatment patients.
4. Self-directed cognitive-behavioral interventions
Perhaps in part because of the low rate of completion of in-person therapies for gambling, clinicians and researchers developed self-directed treatments. Most involve written materials, provided in a workbook or Internet format, based upon CB principles. Table 1 included two studies that evaluated self-directed interventions as one of the conditions to which in-person interventions were compared (Campos et al., 2015; Petry et al., 2006). Table 2 contains studies of entirely self-directed interventions.
In Canada, Hodgins and colleagues (2001) randomized 102 problem gamblers to: a waitlist control, a CB workbook, or the same CB workbook plus an MI phone call. Compared to the waitlist, the CB workbook yielded no benefits one month later. However, the MI phone call plus CB workbook condition resulted in a larger proportion of patients (74%) classified as improved relative to the waitlist condition (44%) with intermediary effects in the CB workbook alone condition (61%). Decreases in dollars and days gambling were also greater in the CB workbook + MI condition compared to the waitlist condition. Longer term assessments, among only those who received the workbooks, found benefits of the MI were maintained throughout the next two years with respect to days and dollars wagered and SOGS scores (Hodgins, Currie, el-Guebaly, & Diskin, 2004), and rates of improvement were 62% in CB workbook alone condition and 89% in the condition that also included MI.
In a replication and extension study again in Canada, Hodgins et al. (2009) compared a single MI call from a therapist to multiple MI calls. They randomized 314 problem gamblers to four conditions, the first three of which were identical to the above study (Hodgins, Currie, & el-Guebaly, 2001), and the fourth included 7 MI calls over 9 months. Compared to the waitlist and CB workbook alone conditions, conditions that included MI calls resulted in higher proportions of patients clinically improved. The respective proportions were 59%, 64%, 74%, and 73% for the waitlist, CB workbook, CB workbook + 1 MI call, and CB workbook + 7 MI calls conditions. The two MI call conditions also yielded improvements in days and dollars gambled versus those without MI calls in the short-term. However, there were no differences between conditions on any index in the one year follow-up.
Using a similar design but integrating motivational content within the workbook, LaBrie et al. (2012) from the US randomized 315 problem gamblers to a waitlist control, an MI/CB workbook, or the same workbook with a phone call instructing about use of the workbook. There were no differences across conditions for days gambled or proportions of patients able to achieve 7-day periods of abstinence at the one month assessment or the three month follow-up, with about 41%–66% achieving brief periods of abstinence across groups and time periods.
Other studies attempted to enhance the impact of MI by delivering it in person rather than over the phone. Diskin and Hodgins (2009) provided a CB workbook to 81 problem gamblers from Canada and randomized them to a control condition consisting of a structured psychiatric interview or a single in-person MI session. Compared to the control, those who received the MI session spent less money gambling at the first post-treatment evaluation, but there were no group by time differences in days gambled, and no differences in clinically significant changes in gambling, with 55% overall having reductions in SOGS scores at a one year follow-up.
In another Canadian study, Hodgins, Currie, el-Guebaly and Diskin (2007) mailed the CB workbook right after participants enrolled in the study, or they mailed the CB workbook initially, along with seven additional mailings over a one-year period. Regardless of the condition to which they were assigned, there were no differences on proportions improved one year later, with 54% overall continuing to meet diagnostic criteria for gambling disorder. Dollars and days gambled also did not differ between groups.
Although most studies provided CB in a workbook, it can also be delivered over the Internet. Carlbring and Smit (2008) randomized 66 persons in Sweden with gambling disorder to a waitlist control or 8 weeks of CB treatment delivered over the Internet along with therapist emails and weekly 15-minute phone calls reviewing materials and providing support. The CB treatment reduced DSM gambling criteria relative to the waitlist condition at the post-treatment evaluation, but long-term efficacy could not be evaluated.
Another study, originating from France, also evaluated therapist facilitation of CB treatment delivered over the Internet. Luquiens et al. (2016) recruited 1122 problem gambling players on an online poker website and randomized them to one of four conditions: a waitlist control, a single email providing them normalized feedback related to their gambling, an email containing a self-help book to be downloaded with a CB treatment program, or the same CB treatment program emailed weekly by a therapist who also provided personalized guidance about its content. There were no differences in gambling outcomes across conditions in the short- or long-term.
Across these studies, self-directed CB interventions led to some short-term benefits in reducing gambling, and generally, although not always, outcomes appear to be improved when a therapist provided MI or support along with the CB materials. However, only one study (Hodgins et al., 2004) found long-term benefits of a CB workbook provided with an MI call. Another (Diskin & Hodgins, 2009) found long-term improvements of MI added to a CB workbook relative to a control interview on one outcome measure but not others, and the four other studies that examined long-term effects (Hodgins et al., 2007, 2009; LaBrie et al., 2012; Lunquins et al., 2016) found no evidence of extended efficacy.
5. Brief feedback interventions
Brief Advice and MI with personalized feedback improved outcomes in studies using in-person administration of these interventions. As shown in Table 1, Petry et al. (2008, 2016) found some benefits of Brief Advice relative to assessment only or psychoeducational control. In US college students, Larimer et al. (2012) found an MI session integrating personalized feedback had some benefits compared to assessment only control. Three additional studies (Table 2) evaluated effects of MI and feedback, without involving any direct contact with therapists.
In Canada, Cunningham, Hodgins, Toneatto and Murphy (2012) randomized 209 problem gamblers to a waitlist or one of two feedback conditions. One provided personalized feedback about gambling along with population norms. The other applied similar feedback about the participant’s gambling, but without the norms. There were no differences across groups at the initial 3-month assessment. At a one-year follow-up, reductions in days gambled, but not amounts wagered, occurred among those assigned to the partial relative to full feedback conditions, contrary to expectations.
Neighbors et al. (2015) randomly assigned 252 US college student problem gamblers to an attention control condition in which they received information about proportions of students living on campus, exercising, etc. or one in which they received a summary of their gambling along with that of student norms. Three months later, students who had received the gambling normative feedback reported lower gambling symptoms and dollars lost, with no difference on days gambled. At a 6-month follow-up, the personalized feedback condition continued to have benefits on money lost, but there were no differences in gambling days or problem scores.
Martens, Arterberry, Takamatsu, Maters and Dude (2015) also evaluated a personalized feedback condition in US college students. They randomized 333 problem gamblers to assessment only control, general information about college student gambling, or personalized feedback. Relative to assessment only, those in the personalized feedback condition gambled less money, but not days, and reported lower gambling symptoms at a 3-month follow-up. The gambling education and personalized feedback conditions did not differ on any outcome variable.
These findings provide some support for brief feedback interventions. However, as in most studies, treatment effects were not consistent across domains or time periods of assessment. When compared to other active interventions such as brief education (Martens et al., 2015), effects of gambling-specific feedback interventions appear to be relatively modest. Although computerized feedback about gambling is inexpensive to deliver on a large-scale basis, it does not appear to have pronounced benefits in improving outcomes in studies conducted to date.
Overall summary and recommendations
Randomized trials have evaluated cognitive, CB, MI, and feedback treatments for problem gambling. Formats ranged from entirely self-directed (workbooks or Internet) to those with a brief phone call or a single in-person session, to in-person therapy ranging from one to up to 20 sessions. Twenty-one moderate to large studies examined these interventions, but no consistent, or persistent, changes in gambling are noted with any specific treatment.
Although no treatment is empirically validated for problem gambling, CB interventions have the greatest evidence of efficacy. Most trials included CB interventions in one or more arms, and most found at least some benefits. These treatments can be delivered on an individual or group basis in 4–8 sessions or via a workbook or the Internet. When CB treatments are self-directed, including a MI phone call along with the materials may improve outcomes relative to providing materials without instructions or support (Diskin & Hodgins, 2009; Hodgins, 2001, 2009). On the other hand, only two of the studies evaluated MI as a stand-alone intervention (Carlbring et al., 2010; Petry et al., 2008), and they provide little evidence that MI is beneficial for reducing gambling when not combined with CB treatments.
Providing brief personalized feedback or advice about gambling has also resulted in some benefits (Cunningham et al., 2012; Larimer et al., 2012; Martens et al., 2015; Neighbors et al., 2015; Petry et al., 2008, 2016), but these brief interventions generally did not outperform other control conditions or CB treatments. Very brief treatments are also only well suited for persons not seeking gambling treatment and are typically applied to college students and others who screen positive for gambling problems, but not those actively looking for gambling treatment.
As clinical care and research advances, it is important to consider the empirical evidence related to these interventions, along with the designs of the studies from which data are drawn. Six issues of importance in designing studies, interpreting their results, and determining practice are described.
Patient population. Although some populations may accept and benefit from brief interventions, people seeking treatment for gambling are more likely to expect in-person therapy or at least some contact with therapists. Thus, subsequent studies in gambling treatment-seeking populations should move beyond waitlist control conditions, as they cannot control for general therapy effects and do not allow for long-term evaluation of efficacy.
Long-term effects. Studies that involved comparator conditions that were not waitlist controls are relatively limited in number, but a few found benefits of CB treatment alone or combined with MI for up to 9-24 months (e.g., Diskin & Hodgins, 2009; Petry et al., 2006, 2008, 2016). Epidemiological research notes that 50% or more of people with lifetime gambling disorder do not meet criteria for gambling disorder in the past year (Hodgins, Wynne, & Makarchuk, 1999; Petry et al., 2005; Slutske, 2006), so future research needs to establish whether gambling specific interventions improve upon natural recovery rates over long periods.
Outcomes. Measures to assess gambling outcomes vary complicating cross study comparisons, and even within studies, effects of interventions generally were noted for some but not all gambling indices. This paper attempts to focus on clinically significant changes, but the field has yet to agree on a single or composite index of improved outcomes (Walker et al., 2006). Objective indices are also important, and studies should collect data from sources beyond the gambler (e.g., Diskin & Hodgins, 2009; Hodgins et al., 2001, 2009; Petry et al., 2006, 2008, 2016).
Goals. Most treatments directed toward persons with gambling disorder encourage abstinence, but few achieve it. Controlled or minimal gambling may be appropriate for some, especially those with less severe problems (e.g., Dowling & Smith, 2007; Dowling, Smith, & Thomas, 2009; Ladouceur, 2005; Ladouceur, Lachance, & Fournier, 2009; Slutske, Piasecki, Blaszczynski, & Martin, 2010). Motivational approaches, as well as CB therapy, allow for personalized goals including reductions in gambling, and therapists, as well as outcomes from treatment studies, should include goals in determining outcomes.
-
Comparisons between interventions. Studies comparing active interventions rarely found differences between them. Demonstrating superiority between interventions requires far more participants than detecting differences between an intervention and a no treatment control condition (Kazdin & Bass, 1989; Luborsky et al., 2002; Wampold, 1997).
Further, psychotherapies, including cognitive, CB, and MI therapies and personalized feedback, are based on theoretical models, and understanding mechanisms of action may improve outcomes (Rounsaville, Carroll, & Onken, 2001). Few gambling studies evaluated whether the therapies are exerting benefits in the intended manner. Petry, Litt, Kadden and Ledgerwood (2007) demonstrated that CB therapy enhanced acquisition of coping skills, which mediated some reductions in gambling. Larimer et al. (2012) found that MI + personalized feedback changed perceptions about gambling norms, which mediated effects on the frequency of gambling. Hodgins, Ching and McEwin (2009) rated audiotapes from MI sessions and found that patients who expressed stronger commitment to change their gambling reduced wagering to a greater extent over 12 months than did patients with weaker or no commitment to change their gambling behavior, but readiness to change, desire, ability, needs and reasons for change were not associated with outcomes. Additional research should evaluate mechanisms through which interventions promote change.
Other symptoms and dually diagnosed gamblers. Gambling disorder often occurs with other psychiatric conditions, including substance use disorders and depression (Kessler et al., 2008; Petry et al., 2005). When gambling decreases, other psychological symptoms also subside. Relative to control conditions, Petry et al. (2006) and Carlbring et al. (2008), for example, found reductions in depression and other psychological symptoms with CB therapy for gambling, suggesting that treating gambling is likely to have generalized effects. However, more research in larger or perhaps more homogeneous comorbid populations is needed to understand how these symptoms are related and impacted by interventions.
Conclusions
Results from this review recommend a 6-8 session or chapter CB treatment, that integrates MI if the CB treatment is entirely self-directed, for individuals seeking gambling treatment. For persons with less severe gambling problems and perhaps even those with gambling problems but who are not desiring traditional in-person multi-session interventions, minimal interventions involving feedback related to one’s gambling may also suffice. Although more research must inform best practices and empirically validate existing or novel interventions for gambling, the studies from the past decades provide a guide for clinicians and a benchmark for expectations regarding outcomes. By comprehensively reviewing and integrating results across published studies, research and clinical practice may advance over time, with the ultimate goal of assisting those suffering from gambling problems.
Acknowledgments
Preparation of this report was supported in part by NIH grants P50-DA09241 and P60-AA03510. Dr. Petry has served as a consultant to the Responsible Gambling Trust.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®) Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Campos MD, Rosenthal RJ, Chen Q, Moghaddam J, Fong TW. A self-help manual for problem gamblers: The impact of minimal therapist guidance on outcome. International Journal of Mental Health and Addiction. 2015;14(4):579–596. [Google Scholar]
- Carlbring P, Jonsson J, Josephson H, Forsberg L. Motivational interviewing versus cognitive behavioral group therapy in the treatment of problem and pathological gambling: A randomized controlled trial. Cognitive Behaviour Therapy. 2010;39(2):92–103. doi: 10.1080/16506070903190245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlbring P, Smit F. Randomized trial of internet-delivered self-help with telephone support for pathological gamblers. Journal of Consulting and Clinical Psychology. 2008;76(6):1090–1094. doi: 10.1037/a0013603. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Hollon SD. Defining empirically supported therapies. Journal of Consulting and Clinical Psychology. 1998;66(1):7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- Cowlishaw S, Merkouris S, Dowling N, Anderson C, Jackson A, Thomas S. Psychological therapies for pathological and problem gambling. The Cochrane Database of Systematic Reviews. 2012;11:CD008937. doi: 10.1002/14651858.CD008937.pub2. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Hodgins DC, Toneatto T, Murphy M. A randomized controlled trial of a personalized feedback intervention for problem gamblers. PloS One. 2012;7(2):e31586. doi: 10.1371/journal.pone.0031586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diskin KM, Hodgins DC. A randomized controlled trial of a single session motivational intervention for concerned gamblers. Behaviour Research and Therapy. 2009;47(5):382–388. doi: 10.1016/j.brat.2009.01.018. [DOI] [PubMed] [Google Scholar]
- Dowling NA, Merkouris SS, Lorains FK. Interventions for comorbid problem gambling and psychiatric disorders: Advancing a developing field of research. Addictive Behaviors. 2016;58:21–30. doi: 10.1016/j.addbeh.2016.02.012. [DOI] [PubMed] [Google Scholar]
- Dowling N, Smith D. Treatment goal selection for female pathological gambling: A comparison of abstinence and controlled gambling. Journal of Gambling Studies. 2007;23(3):335–345. doi: 10.1007/s10899-007-9064-6. [DOI] [PubMed] [Google Scholar]
- Dowling N, Smith D, Thomas T. A preliminary investigation of abstinence and controlled gambling as self-selected goals of treatment for female pathological gambling. Journal of Gambling Studies. 2009;25(2):201–214. doi: 10.1007/s10899-009-9116-1. [DOI] [PubMed] [Google Scholar]
- Fortune EE, Goodie AS. Cognitive distortions as a component and treatment focus of pathological gambling: A review. Psychology of Addictive Behaviors. 2012;26(2):298–310. doi: 10.1037/a0026422. [DOI] [PubMed] [Google Scholar]
- Grant JE, Donahue CB, Odlaug BL, Kim SW, Miller MJ, Petry NM. Imaginal desensitisation plus motivational interviewing for pathological gambling: Randomised controlled trial. The British Journal of Psychiatry. 2009;195(3):266–267. doi: 10.1192/bjp.bp.108.062414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins PT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. 2011 http://handbook.cochrane.org/front_page.htm.
- Hodgins DC, Ching LE, McEwen J. Strength of commitment language in motivational interviewing and gambling outcomes. Psychology of Addictive Behaviors. 2009;23(1):122–130. doi: 10.1037/a0013010. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Currie SR, Currie G, Fick GH. Randomized trial of brief motivational treatments for pathological gamblers: More is not necessarily better. Journal of Consulting and Clinical Psychology. 2009;77(5):950–960. doi: 10.1037/a0016318. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Currie SR, el-Guebaly N. Motivational enhancement and self-help treatments for problem gambling. Journal of Consulting and Clinical Psychology. 2001;69(1):50–57. doi: 10.1037//0022-006x.69.1.50. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Currie SR, el-Guebaly N, Diskin KM. Does providing extended relapse prevention bibliotherapy to problem gamblers improve outcome? Journal of Gambling Studies. 2007;23(1):41–54. doi: 10.1007/s10899-006-9045-1. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Currie S, el-Guebaly N, Peden N. Brief motivational treatment for problem gambling: A 24-month follow-up. Psychology of Addictive Behaviors. 2004;18(3):293–296. doi: 10.1037/0893-164X.18.3.293. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, Wynne H, Makarchuk K. Pathways to recovery from gambling problems: Follow-up from a general population survey. Journal of Gambling Studies. 1999;15(2):93–104. [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Bass D. Power to detect differences between alternative treatments in comparative psychotherapy outcome research. Journal of Consulting and Clinical Psychology. 1989;57(1):138–147. doi: 10.1037//0022-006x.57.1.138. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Hwang I, LaBrie R, Petukhova M, Sampson NA, Winters KC, Shaffer HJ. DSM-IV pathological gambling in the National Comorbidity Survey Replication. Psychological Medicine. 2008;38(9):1351–1360. doi: 10.1017/S0033291708002900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie RA, Peller AJ, LaPlante DA, Bernhard B, Harper A, Schrier T, Shaffer HJ. A brief Self-Help toolkit intervention for gambling problems: A randomized multisite trial. American Journal of Orthopsychiatry. 2012;82(2):278–289. doi: 10.1111/j.1939-0025.2012.01157.x. [DOI] [PubMed] [Google Scholar]
- Ladouceur R. Controlled gambling for pathological gamblers. Journal of Gambling Studies. 2005;21(1):49–59. doi: 10.1007/s10899-004-1923-9. [DOI] [PubMed] [Google Scholar]
- Ladouceur R, Lachance S, Fournier PM. Is control a viable goal in the treatment of pathological gambling? Behaviour Research and Therapy. 2009;47(3):189–197. doi: 10.1016/j.brat.2008.11.004. [DOI] [PubMed] [Google Scholar]
- Ladouceur R, Sylvain C, Boutin C, Lachance S, Doucet C, Leblond J. Group therapy for pathological gamblers: A cognitive approach. Behaviour Research and Therapy. 2003;41(5):587–596. doi: 10.1016/s0005-7967(02)00036-0. [DOI] [PubMed] [Google Scholar]
- Ladouceur R, Sylvain C, Boutin C, Lachance S, Doucet C, Leblond J, Jacques C. Cognitive treatment of pathological gambling. The Journal of Nervous and Mental Disease. 2001;189(11):774–780. doi: 10.1097/00005053-200111000-00007. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Neighbors C, Lostutter TW, Whiteside U, Cronce JM, Kaysen D, Walker DD. Brief motivational feedback and cognitive behavioral interventions for prevention of disordered gambling: A randomized clinical trial. Addiction. 2012;107(6):1148–1158. doi: 10.1111/j.1360-0443.2011.03776.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesieur HR, Blume SB. The South Oaks Gambling Screen (SOGS): A new instrument for the identification of pathological gamblers. The American Journal of Psychiatry. 1987;144(9):1184–1188. doi: 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- Luborsky L, Rosenthal R, Diguer L, Andrusyna TP, Berman JS, Levitt JT, … Krause ED. The dodo bird verdict is alive and well—mostly. Clinical Psychology: Science and Practice. 2002;9(1):2–12. [Google Scholar]
- Luquiens A, Tanguy ML, Lagadec M, Benyamina A, Aubin HJ, Reynaud M. The efficacy of three modalities of internet-based psychotherapy for non-treatment-seeking online problem gamblers: A randomized controlled trial. Journal of Medical Internet Research. 2016;18(2):e36. doi: 10.2196/jmir.4752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Arterberry BJ, Takamatsu SK, Masters J, Dude K. The efficacy of a personalized feedback-only intervention for at-risk college gamblers. Journal of Consulting and Clinical Psychology. 2015;83(3):494–499. doi: 10.1037/a0038843. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Journal of Clinical Epidemiology. 2009;62(10):1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Rodriguez LM, Rinker DV, Gonzales RG, Agana M, Tackett JL, Foster DW. Efficacy of personalized normative feedback as a brief intervention for college student gambling: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2015;83(3):500–511. doi: 10.1037/a0039125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowak DE, Aloe AM. The prevalence of pathological gambling among college students: A meta-analytic synthesis, 2005–2013. Journal of Gambling Studies. 2014;30(4):819–843. doi: 10.1007/s10899-013-9399-0. [DOI] [PubMed] [Google Scholar]
- Oei TP, Raylu N, Casey LM. Effectiveness of group and individual formats of a combined motivational interviewing and cognitive behavioral treatment program for problem gambling: A randomized controlled trial. Behavioural and Cognitive Psychotherapy. 2010;38(2):233–238. doi: 10.1017/S1352465809990701. [DOI] [PubMed] [Google Scholar]
- Pallesen S, Mitsem M, Kvale G, Johnsen BH, Molde H. Outcome of psychological treatments of pathological gambling: A review and meta-analysis. Addiction. 2005;100(10):1412–1422. doi: 10.1111/j.1360-0443.2005.01204.x. [DOI] [PubMed] [Google Scholar]
- Petry NM. Validity of a gambling scale for the Addiction Severity Index. The Journal of Nervous and Mental Disease. 2003;191(6):399–407. doi: 10.1097/01.NMD.0000071589.20829.DB. [DOI] [PubMed] [Google Scholar]
- Petry NM. Pathological gambling: Etiology, comorbidity, and treatment. Washington, DC: American Psychological Association; 2005. [Google Scholar]
- Petry NM, Ammerman Y, Bohl J, Doersch A, Gay H, Kadden R, … Steinberg K. Cognitive-behavioral therapy for pathological gamblers. Journal of Consulting and Clinical Psychology. 2006;74(3):555–567. doi: 10.1037/0022-006X.74.3.555. [DOI] [PubMed] [Google Scholar]
- Petry NM, Blanco C, Auriacombe M, Borges G, Bucholz K, Crowley TJ, … O'Brien C. An overview of and rationale for changes proposed for pathological gambling in DSM-5. Journal of Gambling Studies. 2014;30:493–502. doi: 10.1007/s10899-013-9370-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Litt MD, Kadden R, Ledgerwood DM. Do coping skills mediate the relationship between cognitive-behavioral therapy and reductions in gambling in pathological gamblers? Addiction. 2007;102(8):1280–1291. doi: 10.1111/j.1360-0443.2007.01907.x. [DOI] [PubMed] [Google Scholar]
- Petry NM, Rash CJ, Alessi SM. A randomized controlled trial of brief interventions for problem gambling in substance abuse treatment patients. Journal of Consulting and Clinical Psychology. 2016;84(10):874–886. doi: 10.1037/ccp0000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Stinson FS, Grant BF. Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry. 2005;66(5):564–574. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- Petry NM, Weinstock J, Ledgerwood DM, Morasco B. A randomized trial of brief interventions for problem and pathological gamblers. Journal of Consulting and Clinical Psychology. 2008;76(2):318–328. doi: 10.1037/0022-006X.76.2.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rash CJ, Petry NM. Psychological treatments for gambling disorder. Psychology Research and Behavioral Management. 2014;7:285–295. doi: 10.2147/PRBM.S40883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology: Science and Practice. 2001;8(2):133–142. [Google Scholar]
- Slutske WS. Natural recovery and treatment-seeking in pathological gambling: Results of two U.S. national surveys. The American Journal of Psychiatry. 2006;163(2):297–302. doi: 10.1176/appi.ajp.163.2.297. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Piasecki TM, Blaszczynski A, Martin NG. Pathological gambling recovery in the absence of abstinence. Addiction. 2010;105(12):2169–2175. doi: 10.1111/j.1360-0443.2010.03080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DP, Battersby MW, Harvey PW, Pols RG, Ladouceur R. Cognitive versus exposure therapy for problem gambling: Randomised controlled trial. Behaviour Research and Therapy. 2015;69:100–110. doi: 10.1016/j.brat.2015.04.008. [DOI] [PubMed] [Google Scholar]
- Stea JN, Hodgins DC. A critical review of treatment approaches for gambling disorders. Current Drug Abuse Reviews. 2011;4(2):67–80. doi: 10.2174/1874473711104020067. Review. [DOI] [PubMed] [Google Scholar]
- Stucki S, Rihs-Middel M. Prevalence of adult problem and pathological gambling between 2000 and 2005: An update. Journal of Gambling Studies. 2007;23(3):245–257. doi: 10.1007/s10899-006-9031-7. [DOI] [PubMed] [Google Scholar]
- Walker M, Toneatto T, Potenza MN, Petry N, Ladouceur R, Hodgins DC, … Blaszczynski A. A framework for reporting outcomes in problem gambling treatment research: The Banff, Alberta consensus. Addiction. 2006;101(4):504–511. doi: 10.1111/j.1360-0443.2005.01341.x. [DOI] [PubMed] [Google Scholar]
- Wampold B. Methodological problems in identifying efficacious psychotherapies. Psychotherapy Research. 1997;7(1):21–43. [Google Scholar]
- Yakovenko I, Quigley L, Hemmelgarn BR, Hodgins DC, Ronksley P. The efficacy of motivational interviewing for disordered gambling: Systematic review and meta-analysis. Addictive Behaviors. 2015;43:72–82. doi: 10.1016/j.addbeh.2014.12.011. [DOI] [PubMed] [Google Scholar]