Abstract
Objective
The aims of the study were to investigate psychological distress in pneumothorax patients.
Methods
A cohort study was performed in 101 patients with spontaneous pneumothorax. They were divided into three groups: (A) under 19 years old, (B) those of an intermediate age, and (C) over 45 years old. General well-being [Psychological Wellbeing Index-Short Form (PWI-SF)], traumatic event [Impact of Event Scale (IES)], and resilience [Life Orientation Test-Revised (LOT-R)] were assessed.
Results
There were 35 patients in Group A, 51 in B, and 15 in C. The mean length of hospital stay was five days in all patients. The overall recurrence rate after surgery was 8%. All patients were under severe stress and reported an average PWI-SF score of 39. The IES score was 27, which did not meet the criteria for post-traumatic stress disorder but was higher in Group C than in the other groups (p=0.02). Age and operation were significant factors for a high IES, but age was the only significant factor according to multivariate analysis.
Conclusion
Pneumothorax patients may be at high risk for severe stress. Moreover, post-traumatic stress was higher in elderly patients. Actions to reduce the psychological problems in these patients are required.
Keywords: Pneumothorax, Distress, Well-being, Resilience
INTRODUCTION
Pneumothorax is an irritating disorder that presents with a variable spectrum. It may develop in young and healthy people (primary, spontaneous pneumothorax) or as a complication of an underlying lung disorder (secondary pneumothorax).1 Moreover, its treatment options are also variable. Observation, air aspiration, and chest tube insertion are generally recommended for the first episode of pneumothorax, while chemical pleurodesis, video-assisted thoracic surgery (VATS) and thoracotomy may be useful for recurrent or persistent pneumothorax.2 Despite newer treatments that use VATS, the recurrence rate is still reported to be from 1.8–4% to 9% in cases of secondary pneumothorax.3,4,5,6 In other words, patients in all age groups suffer not only from pneumothorax and its related symptoms but also from a fear of the condition's recurrence. Few reports have documented psychopathological abnormalities in patients with pneumothorax.7,8,9 One study investigated the etiology of primary spontaneous pneumothorax and suggested an association between anger and primary spontaneous pneumothorax.7 Other studies also investigated psychological factors, including depression, anxiety, and anger in patients with pneumothorax compared with normal individuals but the result is not consistent.8,9
The fear and pain associated with a pneumothorax contribute to the overall stress level of these patients and include the initial pain, the emergency department (ED) experience, the diagnosis and follow-up appointments, chest tube insertions, and corrective surgery. Few studies have evaluated psychological distress in pneumothorax patients. The prevalence rate of post-traumatic stress disorder (PTSD) varies from 1–32%.10,11 A substantial number of pneumothorax patients do not fulfill the diagnostic criteria for PTSD but may still exhibit clinically relevant psychological symptoms. In this study, we evaluated the current level of distress and related symptoms among a sample of spontaneous pneumothorax patients using the Impact of Events Scale (IES). To identify factors that influenced psychological distress, we assessed the relationships between demographic factors (e.g., age), clinical factors (e.g., length of hospital stay and management methods) and IES scores. Post-traumatic stress symptoms decrease over time, and resilience plays an important role in producing transient and low levels of symptoms soon after the event as well as maintaining a low incidence during the follow-up period.12 Few studies have investigated the health-related quality of life, stress, or psychological problems experienced by pneumothorax patients. In this study, we used a revised version of the Life Orientation Test (LOT)13 because it is widely used to investigate the relationship between exposure to traumatic events and resilience to trauma. In addition, the IES intrusion and avoidance subscales were evaluated to understand which factors that affect psychological distress may be best suited to identify those patients at risk for distress.
The aims of the study were as follows: 1) to investigate psy-chological distress in pneumothorax patients awaiting discharge and 2) to study possible contributory background variables, including age, management of pneumothorax-related predic-tors of psychological distress, and resilience.
METHODS
Study design and population
This was a retrospective cohort study that used the medical records and questionnaires of 101 patients who received pneumothorax management between August 2013 and October 2015 at a university-based tertiary hospital in Cheongju, South Korea. The follow-up period lasted until March 25, 2016. Patient eligibility criteria included the following: 1) patients who were diagnosed with spontaneous pneumothorax by thoracic surgery specialists (DK, SK, and JH); 2) those who agreed with the study and questionnaire; and 3) participants whose pneumothorax management was performed using the same policy as this hospital. The exclusion criteria were as follows: 1) patients with traumatic or iatrogenic pneumothorax; 2) participants who were admitted to the intensive care unit or who had poor general conditions that may confound clinical outcomes or psychologic measures; 3) patients less than one year of age whose disease entity was different from that of general pneumothorax patients.
The participants were divided into three groups: A) under 19 years, B) of intermediate age, and C) over 45 years. The possible causes of secondary pneumothorax are chronic bronchitis and emphysematous lung disease, and they were relevant in the population greater than 45 years old.14 Demographics including gender, age, body mass index (BMI), height, history of smoking, reason for pneumothorax development and occupations were investigated. Details of the procedures used, including the type of approach (VATS or thoracotomy) and the usage of polyglycolic acid (PGA) felt (Neoveil™, Gunze Ltd, Kyoto, Japan), were collected. Clinical outcomes were evaluated along with information about the patients' hospital stay (duration from the time of admission to discharge) and recurrence rate after surgery. Questionnaires dealing with resilience, stress, and post-traumatic stress were completed by the patients one day before their discharge. All the data were collected and compared among the three groups. This study was reviewed and approved by the Institutional Review Board (IRB) of Chungbuk National University Hospital (IRB No. 2016-01-008). All participants agreed and signed the informed consent prepared by the researchers.
Management of pneumothorax
All patients in our study who had pneumothorax primarily received chest tube insertion and chest computed tomography. A 12 French chest tube was usually selected, but a larger one (24 or 28 French) was chosen if the patients were suspected to be suffering from chemical pleurodesis. If the air leakage stopped after chest tube insertion, then the patient can be discharged after the tube has been removed. However, another management strategy was considered in the following situations: 1) prolonged air leakage for more than three days; 2) a second attack of pneumothorax; and 3) large or multiple bullae discovered in the chest following computed tomography (CT). Consecutive management attempts included wedge resection of the lung parenchyma or chemical pleurodesis.
Psychometric measures
All patients who agreed to take part in the study completed a questionnaire one day before discharge. This questionnaire consisted of three sections that assessed optimism [10 questions, Life Orientation Test-Revised (LOT-R)], distress (15, IES), and general stress [18, Psychological Wellbeing Index-Short Form (PWI-SF)].
Life Orientation Test-Revised (LOT-R)
The LOT was developed to assess individual differences in generalized optimism versus pessimism.15 Although the LOT has been widely used, its items do not all focus as explicitly on expectations for the future as theory dictated. To overcome this weak point, the LOT-R was developed.13 The LOT-R is a 10-item measure of optimism versus pessimism. Of the 10 items, 3 measure optimism, 3 assess pessimism, and 4 serve as fillers. The respondent options for each item on a 4-point scale were as follows: 0=strongly disagree, 1=disagree, 2=neutral, 3=agree, and 4=strongly agree. Dispositional optimism is defined as a generalized expectancy of positive future outcomes.16 It positively affects health outcomes17 and health-related behaviors.18
Impact of the Event Scale (IES)
The IES is a simple but powerful self-report measure for assessing the magnitude of symptomatic response to a specific traumatic life event.19 The IES scale consists of 15 items, 7 of which measure intrusive symptoms (intrusive thoughts, nightmares, intrusive feelings, and imagery) and 8 top avoidance symptoms (numbing of responsiveness, avoidance of feelings, situations, ideas); when combined, the two provide a total subjective stress score. The respondents were also asked to rate the items on a 4-point scale according to how often each had occurred in the past 7 days. The 4 points on the scale were as follows: 0=not at all, 1=rarely, 3=sometimes, and 5=often. An IES score of >20 has been suggested as a clinical case level,20 while a cut-off score ≥ 35 has been suggested to indicate PTSD.21
Psychological Wellbeing Index-Short Form (PWI-SF)
The PWI-SF is a stress questionnaire based on the General Health Questionnaire.22 It has been adapted to Korea with proven feasibility in selecting groups for the treatment of psychiatric disorders, such as depression and anxiety disorder.23 The 18 questions on the PWI-SF form can be answered and are assigned 0, 1, 2, or 3 points, which produces a total score; the higher the score, the more severe the stress patient's level. As suggested by the developer of the PWI-SF, the participants of this study were divided into a healthy group with less than 8 points, a potentially stressed group with 9–26 points, and a high-risk group with 27 points or higher.
Statistical analysis
Descriptive statistics were used to summarize the patient characteristics and outcomes; differences in baseline clinical characteristics, operative information, and surgical outcomes were compared by age-groups using χ2 tests. Fisher's exact test was used when the data contained fewer than five for categorical variables and t-tests were used for continuous variables. T-tests and Mann-Whitney-Wilcoxon tests were employed depending on the outcome distribution. In the linear regression analyses, two steps were conducted; the first was a univariate analysis of independent variables. Secondly, the in-dependent variables were entered as multivariables using backwards elimination methods. All statistical tests were two-sided with a significance level set at 0.05 and were performed using Stata software version 10.0 (Stata, College Station, TX, USA).
RESULTS
Characteristics of the study population
This study included 101 patients. There were 87 males, and the mean age was 29 years. The mean height and weight were 172 cm and 58 kg, respectively. The average BMI was 19.5. About one-third of the patients (32%) had a history of smoking. Most patients (90%) experienced symptoms related with pneumothorax when they were conducting their daily activities of getting up, walking, studying, or eating. Others reported that these symptoms began during moderate-intensity exercise, such as soccer, running, or golf. Regarding participant occupation, 62 were students, 17 were businessmen, and the remaining 22 held other jobs. Some patients experienced a repeated admission due to pneumothorax; 26 were admitted twice, 3 had a third episode, and 4 experienced fourth pneumothorax-related hospital admissions. Surgery was performed in 65 (65%) patients. Most of them (n=64, 98%) were carried out using VATS, and PGA felt was applied to prevent recurrence.
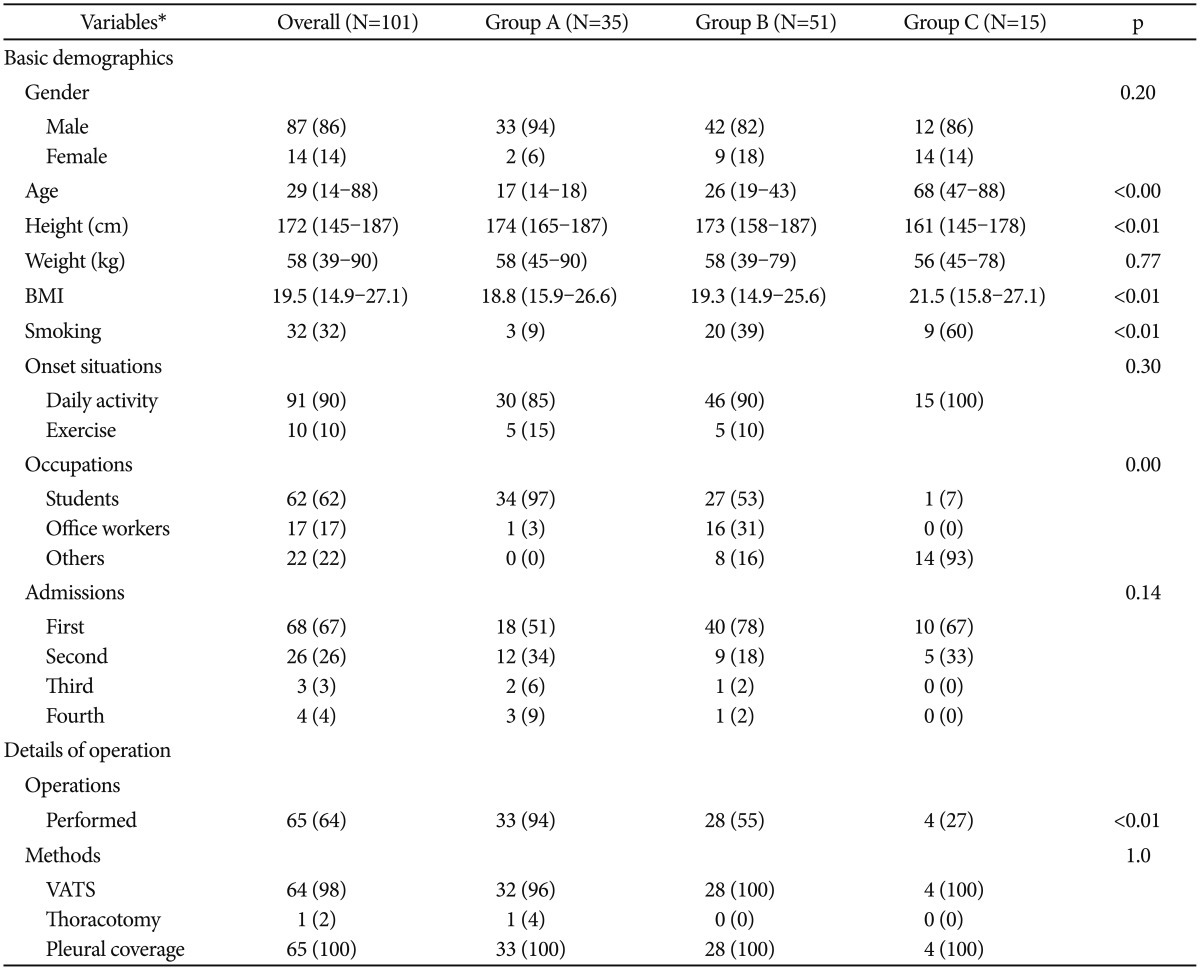
Group A contained 35 patients (<19 years); there were 51 in Group B (19–44) and 15 in Group C (>45). The gender proportion and weight were not different among groups (p=0.20, 0.77). However, Group C was smaller (161 cm) than Group A (174 cm) or Group B (173 cm) (p<0.01). The proportion of smokers (A: 9%, B: 39%, and C: 60%) increased with aging (p<0.01). All patients in Group C experienced pneumothorax during their daily activities. However, other patients (15% in Group A and 10% in Group B) reported pneumothorax during exercise; this difference was not statistically significant (p=0.30). A repeated admission history was prominent in Group A (two admissions in 34%, three in 6%, and four in 9%) but was not statistically different among groups (p=0.14). All patients who underwent a wedge resection in Groups B and C were treated using VATS. One patient (4%) in Group A had a mini-thoracotomy. Details about the patient demographics are shown in Table 1.
Table 1. Basic demographics of the pneumothorax patients.
*continuous variables are presented as the mean (range) and categoric variables as number (%). BMI: body mass index, VAT: video-assisted thoracic
Clinical outcomes
Surgical results
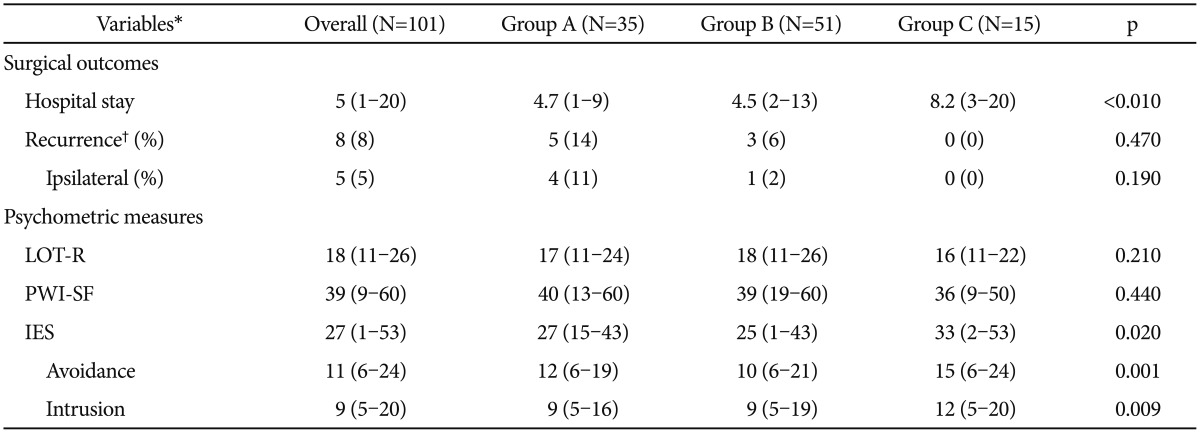
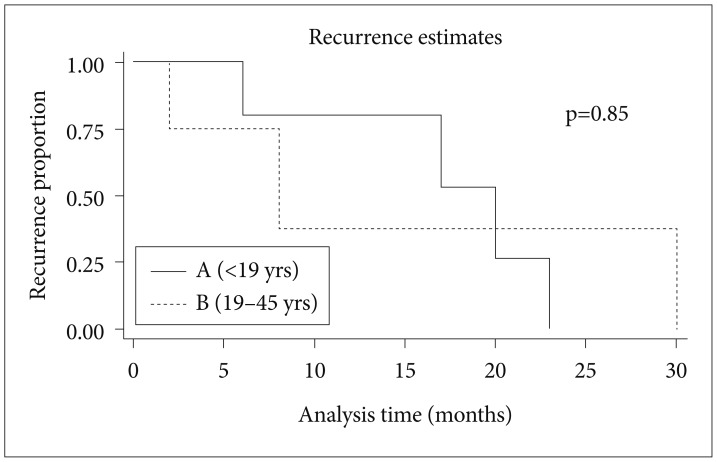
The mean hospital stay was five days. This length of stay was an average of four days in Groups A and B but only about eight days in Group C (p<0.01). No complications or requirements for repeat surgery arose during the initial hospital stay. The mean follow-up duration was 20 months. Overall, the recurrence rate after surgery was 8% (5% on the ipsilateral and 3% on the contralateral sides). Recurrence was more common in Group A (14%) than in Groups B (6%) or C (0%). However, the difference between Groups A and B was not statistically different (p=0.85). Details are shown in Table 2 and Figure 1.
Table 2. Clinical outcomes with surgical and psychometric measures.
*continuous variables are presented as the mean (range) and categoric variables as number (%), †recurrence means recurred pneumothorax after surgical managements. LOT-R: Life Orientation Test-Revised, PWI-SF: Psychological Wellbeing Index-Short Form, IES: Impact of Event Scale
Figure 1. Recurrence pattern of pneumothorax after surgical treatment in different age groups.
Psychometric analysis
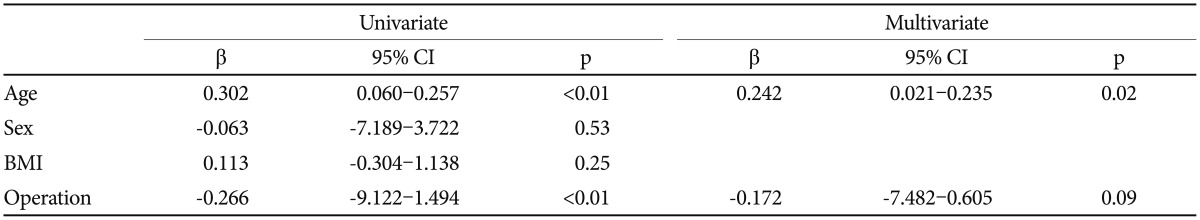
The overall mean of the PWI-SF scores was 39, which suggests a high-risk group with severe stress; however, there were no significant differences in LOT-R and PWI-SF scores among the three groups. The mean of the IES scores was 27, which suggests a clinical case level but was not enough for a diagnosis of PTSD. However, the IES scores were significantly different in Group C (33) compared to Groups A (27) and B (25) (p=0.02) (Table 2). Avoidance and Intrusion, which are subscales of the IES, were also significantly increased in Group C compared to Groups A and B (p=0.001, 0.009 respectively) (Table 2). In addition, age and operation were significantly associat-ed with the IES scores upon univariate analysis, but age was the only significant factor (p=0.02) according to the multivariate analysis (Table 3).
Table 3. Predictors of psychological distress in pneumothorax patients.
CI: confidence interval, BMI: body mass index
DISCUSSION
Pneumothorax patients may be included in a high-risk group of severe stress, particularly elderly patients, who can be more fragile and therefore more at risk from a pneumothorax or its related treatment. Pneumothorax is an irritating disease with a high recurrence rate that may require frequent ED visits. However, the cause of this “irritation” has traditionally been regarded as a focus of doctors, not patients. Therefore, frustration, depression, or unhappiness reported by pneumothorax patients has not been sufficiently studied. In this investigation, it was confirmed that the stress levels of pneumothorax patients were severe, so appropriate measures are required to reduce their distress. Some type of treatment may be urgent for Group C or any elderly pneumothorax patients because their post-traumatic stress level is higher than those of the other groups. These patients have several features in common: they are elderly and usually had a secondary pneumothorax, a longer hospital stay, and a lower rate of surgical management. Although age was the only significant factor that affected the IES score in this research, further large-scale studies will be required to identify other clinical factors that determine psychological distress in pneumothorax patients.
Older adults tended to respond to traumatic events by re-experiencing emotional numbing, behavioral avoidance, and increased physiological arousal. Because aging is negatively associated with the ability to respond to stress, older adults should be considered a high-risk group following a specific stressful event, such as a pneumothorax. According to Horowitz's model of emotional processing following a trauma,24 until the traumatic experiences are psychologically assimilated, the individual will alternate between the experience of intrusive thoughts and feelings in one moment and avoidance strategies in the next. Intrusion means repeated thoughts about the trauma, while avoidance is when the patient makes an effort to avoid situations that serve as reminders of the trauma.
Remarkable findings have been reported about the management of pneumothorax. First, the condition usually arises when patients are going about their regular daily activities. In another report, more than 87% reported being inactive when their symptoms began.25 These observations were similar in our report and were especially prominent in Group C. Therefore, avoiding exercise to prevent another collapsed lung may be useless. Second, smoking was regarded as a risk factor for pneumothorax.26 However, this may not be true in young patients because their smoking rates are lower than others in this report. Nevertheless, smoking should be avoided because young pneumothorax patients may be hidden smokers.27 Third, the surgical management of pneumothorax in elderly patients should not a reason for hesitation; the post-surgical recurrence rate in our reports was 0%. Given that patients may be carefully selected for surgery, surgical management should not be denied because it can present a good option in some elderly, secondary pneumothorax patients.
There are some limitations to this report. First, this study was a retrospective study. Therefore, the numbers of patients were uneven among groups. Moreover, the psychological questionnaire was only administered once during the study period. Further study should include repeated measures of psychologic questionnaires to identify any changes and related factors. Second, we included both primary and secondary pneumothorax patients. In contrast with primary spontaneous pneumothorax, secondary spontaneous pneumothorax is more a dangerous condition and the peak incidence can occur later in life. However, our study aim was to elucidate not the pathophysiology of pneumothorax but the health-related quality of life, stress, or psychological problems experienced by overall spontaneous pneumothorax patients. Third, we conducted a cross-sectional examination of the characteristics of patients with pneumothorax and a brief self-report without the need for intensive interviews. Despite these limitations, this study is unique and worth reading because it analyzed psychological distress in patients with pneumothorax, an irritating and annoying disease, from the patients' point of view.
In conclusion, pneumothorax patients may be included in a high-risk group that experiences severe stress. Moreover, post-traumatic stress is prominent in elderly sufferers. Actions to reduce psychological problems in these patients are required and may be particularly urgent in the elderly. At the same time, further large-scale studies to determine any potential causes of the stress are also required.
Acknowledgments
This work was supported by the intramural research grant of Chungbuk National University in 2015.
This study was supported by a grant of the Korean Mental Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HM15C1058).
References
- 1.Massard G, Thomas P, Wihlm JM. Minimally invasive management for first and recurrent pneumothorax. Ann Thorac Surg. 1998;66:592–599. [PubMed] [Google Scholar]
- 2.de Vos B, Hendriks J, Van Schil P, Van Hee R, Hendrickx L. Long-term results after video-assisted thoracic surgery for spontaneous pneumothorax. Acta Chir Belg. 2002;102:439–444. doi: 10.1080/00015458.2002.11679348. [DOI] [PubMed] [Google Scholar]
- 3.Isaka M, Asai K, Urabe N. Surgery for secondary spontaneous pneumothorax: risk factors for recurrence and morbidity. Interact Cardiovasc Thorac Surg. 2013;17:247–252. doi: 10.1093/icvts/ivt221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yamazaki K, Haratake N, Shikada Y, Mori R, Kouso H, Shoji F, et al. Initial experience of single-incision thoracoscopic surgery for 100 patients with primary spontaneous pneumothorax. Ann Thorac Cardiovasc Surg. 2015;21:513–516. doi: 10.5761/atcs.oa.15-00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Delpy JP, Pages PB, Mordant P, Falcoz PE, Thomas P, Le Pimpec-Barthes F, et al. Surgical management of spontaneous pneumothorax: are there any prognostic factors influencing postoperative complications? Eur J Cardiothorac Surg. 2016;49:862–867. doi: 10.1093/ejcts/ezv195. [DOI] [PubMed] [Google Scholar]
- 6.Herrmann D, Klapdor B, Ewig S, Hecker E. Initial management of primary spontaneous pneumothorax with video-assisted thoracoscopic surgery: a 10-year experience. Eur J Cardiothorac Surg. 2016;49:854–859. doi: 10.1093/ejcts/ezv206. [DOI] [PubMed] [Google Scholar]
- 7.Lee SH, Choi H, Kim S, Choi TK, Lee S, Kim B, et al. Association between anger and first-onset primary spontaneous pneumothorax. Gen Hosp Psychiatry. 2008;30:331–336. doi: 10.1016/j.genhosppsych.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 8.Eryigit H, Ozkorumak E, Unaldi M, Ozdemir A, Cardak ME, Ozer KB. Are there any psychological factors in male patients with primary spontaneous pneumothorax? Int J Clin Exp Med. 2014;15:1105–1109. [PMC free article] [PubMed] [Google Scholar]
- 9.Lim HK, Yoon SH, Oh CH, Choo SH, Kim TH. The impact of primary spontaneous pneumothorax on multiphasic personal inventory test results in young South Korean males. Yonsei Med J. 2012;53:901–905. doi: 10.3349/ymj.2012.53.5.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones RC, Chung MC, Berger Z, Campbell JL. Prevalence of post-traumatic stress disorder in patients with previous myocardial infarction consulting in general practice. Br J Gen Pract. 2007;57:808–810. [PMC free article] [PubMed] [Google Scholar]
- 11.Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26:537–547. doi: 10.1002/jts.21848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- 13.Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev. 2010;30:879–889. doi: 10.1016/j.cpr.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Lung Association Epidemiology and Statistics Unit Research and Health Education Division. Trends in copd (chronic bronchitis and emphysema): Morbidity and Mortality. Chicago: American Lung Association; 2013. [Google Scholar]
- 15.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the life orientation test. J Pers Soc Psychol. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 16.Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol. 1985;4:219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 17.Cozzarelli C. Personality and self-efficacy as predictors of coping with abortion. J Pers Soc Psychol. 1993;65:1224–1236. doi: 10.1037//0022-3514.65.6.1224. [DOI] [PubMed] [Google Scholar]
- 18.Yarcheski TJ, Mahon NE, Yarcheski A. Depression, optimism, and positive health practices in young adolescents. Psychol Rep. 2004;95:932–934. doi: 10.2466/pr0.95.3.932-934. [DOI] [PubMed] [Google Scholar]
- 19.Horowitz M, Wilner N, Alvarez W. Impact of event scale: a measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Friedman M, Keane T, Resick P. Handbook of PTSD, Science and Practice. New York: The Guilford Press; 2007. [Google Scholar]
- 21.Wohlfarth TD, van den Brink W, Winkel FW, ter Smitten M. Screening for posttraumatic stress disorder: an evaluation of two self-report scales among crime victims. Psychol Assess. 2003;15:101–109. doi: 10.1037/1040-3590.15.1.101. [DOI] [PubMed] [Google Scholar]
- 22.Goldberg DP, Hillier VF. A scaled version of the general health questionnaire. Psychol Med. 1979;9:139–145. doi: 10.1017/s0033291700021644. [DOI] [PubMed] [Google Scholar]
- 23.Jang S. Stress. In: Jang S, editor. Collection of Health Statistics and Standardization of Measurement. Seoul: Gaechook Press; 2000. pp. 92–132. [Google Scholar]
- 24.Horowitz M. Stress response syndromes. Character style and dynamic psychotherapy. Arch Gen Psychiatry. 1974;31:768–781. doi: 10.1001/archpsyc.1974.01760180012002. [DOI] [PubMed] [Google Scholar]
- 25.Bense L, Wiman LG, Hedenstierna G. Onset of symptoms in spontaneous pneumothorax: correlations to physical activity. Eur J Respir Dis. 1987;71:181–186. [PubMed] [Google Scholar]
- 26.Noppen M. Spontaneous pneumothorax: epidemiology, pathophysiology and cause. Eur Respir Rev. 2010;19:217–219. doi: 10.1183/09059180.00005310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cheng YL, Huang TW, Lin CK, Lee SC, Tzao C, Chen JC, et al. The impact of smoking in primary spontaneous pneumothorax. J Thorac Cardiovasc Surg. 2009;138:192–195. doi: 10.1016/j.jtcvs.2008.12.019. [DOI] [PubMed] [Google Scholar]