Abstract
Migraine related vertigo (MRV) is largely accepted in the vestibular community and probably represents the second most common cause of vertigo after benign positional vertigo by far exceeding Meniere’s disease. The data on vestibular migraine management is still relatively poor, despite its enormous importance in daily practice. A 55-year old male presented with history of giddiness, imbalance, sweating and sensation of nausea with severe pulsating headache of one day duration. Ear, Nose and Throat examination was normal. Neurological tests were negative. Audiogram and Electronystagmography were within normal limits. Nystagmus was positive on turning his head to left side. By reviewing the available literature on MRV, the report aims to outline a protocol for future management. The patient and caretakers were thoroughly counseled and educated, started on Flunarizine 10 mg and Dimenhydrinate 50 mg; advice healthy life style, necessary precautions, compliance to treatment. Patient was reportedly followed up and was symptom free over a period of 9 years. There is a call for proper diagnosis to address the complaint and manage of symptoms in acute attack and prophylaxis. In addition, this case highlight the ongoing need for proper systematic evaluation, therapeutic management, follow up by ensuring compliance to medication, necessary precautions and life style modification.
Keywords: Vertigo, Meniere’s disease, Migraine, Migraine-associated vertigo
Introduction
Vestibular migraine is largely accepted in the vestibular community and probably represents the second most common cause of vertigo after benign positional vertigo [1] by far exceeding Meniere’s disease. The quality of the data on vestibular migraine management is still relatively poor, despite its enormous importance in daily practice.
Recent reports have focused on a possible association between migraine and Meniere’s disease; suggested symptoms of migraine and recurrent cochleovestibular disorders.
Migraine is one of the most debilitating chronic disorders, almost as prevalent as hypertension and is more common than asthma and diabetes mellitus. Migraine strikes people between ages 20 and 40 for most women, with a slightly higher age range for men. It is estimated that approximately 50% of migraineurs go undiagnosed or mismanaged to this day. Many self-treat, or are treated inappropriately for sinus or other non-migrainous types of headache [2].
Case Report
55 years old Gentlemen presented to our clinic on 20 May 2007 with a history of giddiness, imbalance, sweating and sensation of nausea with severe pulsating headache of one day duration. Though he had headache and mild dizziness on and off since 2 months, it was the first time he noticed this severity. There is no history of unconsciousness or chest pain. There were no associated medical comorbidities. He was a railway PSI (Power Supply Installation) having stress factors due to some family problems and heavy duty, skips meals on and off otherwise a nonsmoker and does not consume alcohol.
Ear, Nose and Throat examination was normal. Neurological tests were negative. Nystagmus was positive on turning his head to left side. Audiogram and ENG (Electronystagmography) were within normal limits. He was non diabetic and non-hypertensive. Physician opinion and cardiac parameters were within normal limits.
Patient was put on Flunarizine 10 mg and or cinnarizine 20 mg + dimenhydrinate 50 mg for long period. He has been followed up till date yearly up to 2016, now he has retired, has solved his stress and family problems, cultivated regular food habits and is free from giddiness and headache.
Discussion
Migraine is periodic, severe, one sided pulsating headache lasting for more than couple of hours often accompanied by neurological/autonomic/gastrointestinal problems preceded by an aura. Migraine is sometimes associated with vertigo than it is known as migraine related vertigo. More than 50% of migraine patients have some form of balance disorder and is most common cause of spontaneous episodic vertigo [2].
Vertigo of migraine patients may precede the attack of headache and be a part of migrainous aura. It is difficult to understand wether vertigo and migraine are different manifestations of same pathophysiology.
Migraine May be Classified
-
Common migraine (Migraine without aura)
The headache is unilateral pulsating and aggravated by physical activity. It has high sensitivity to light (photophobia) and sound (Phonophobia). Neurological test are negative.
-
Classical migraine (Migraine with aura)
Patients must have had 2 or 3 attacks of headache which must be preceded by reversible CNS dysfunction- ataxia, diplopia, dysarthria, unilateral numbness/weakness, tinnitus vertigo. This phase is called aura. Neurological tests after attacks are normal.
-
Basilar migraine (variant of classical migraine)
Features of basilar and vertebral artery spasm. Symptoms of brain stem hypoxia like vertigo tinnitus, deafness, dysarthria, diplopia, decreased level of consciousness, numbness or weakness of limb. Attacks last for few minutes to hours. Headaches originating in the occipital and cervical regions.
-
Vestibular migraine
Only vestibular symptoms and no headache possibly due to vestibulo-cochlear artery spasm may turn into classical migraine.
-
Complicated migraine (migrainous infraction)
It’s a classical migraine but neurological symptoms are not reversible within 7 days. MRI shows zone of ischemic infraction of brain (Fig. 1).
Fig. 1.
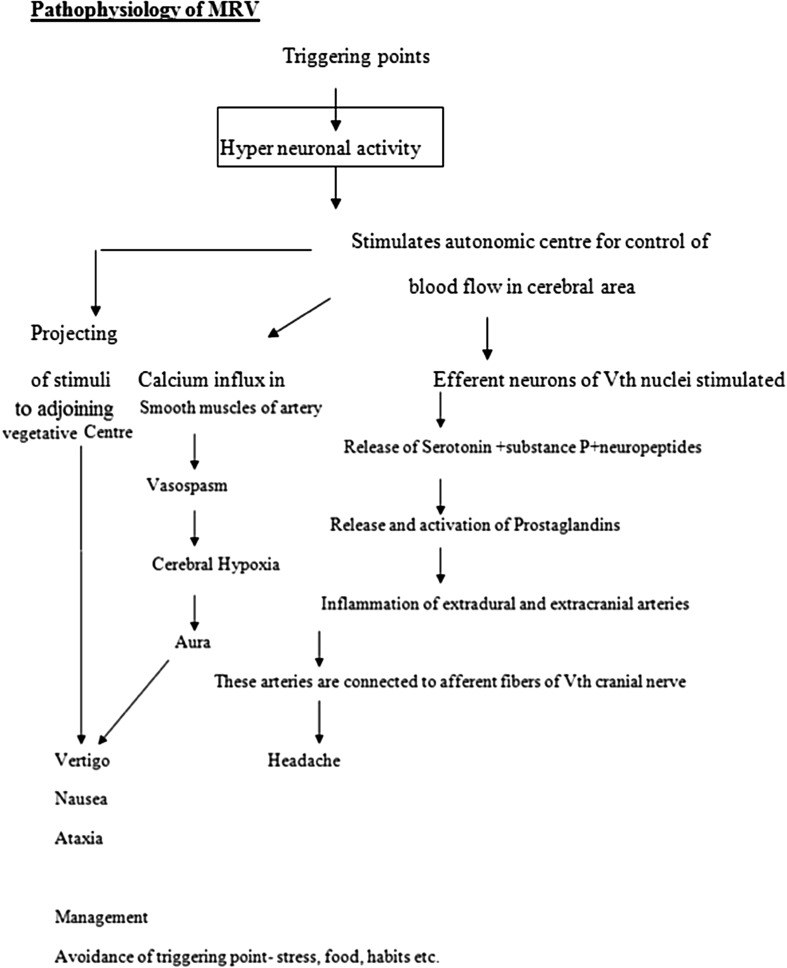
Pathophysiology of Migraine Related Vertigo
Fundamental to the pathophysiology of migraine is the trigeminovascular reflex. This is a parasympathetic reflex that can produce vasodilation of large cranial vessels. The vasodilation of large cranial vessels is a consequence of activation mediated by the trigeminal nucleus caudalis (Vc) and C1-C2 dorsal horn neurones [3, 4]. In addition to the parasympathetic effects of the trigeminovascular reflex, vasodilation may be induced or augmented by direct vasodilator effects of neurokinin A (NKA), calcitonin gene related peptide (CGRP), and substance P (SP) release from trigeminal sensory terminals [3].
Vestibular pathways can contribute to both central and peripheral migraine mechanisms [5]. Two possible mechanisms may be related to vertigo as a migraine aura. Short duration vertigo symptoms have been suggested to be a “brainstem aura” that may be accompanied by changes in blood flow [6]. Alternatively, direct connections from the posterior parietal cortex to the vestibular nuclei may provide a direct access for cortical mechanisms underlying migraine aura to reach areas important for vestibular information processing and reflex performance.
The vestibular periphery may also influence migraine pathways. Vass et al. [7] have demonstrated that there is a significant trigeminal sensory innervation of the stria vascularis, spiral modiolar blood vessels, and dark cell region of the cristae ampularis. They have shown also that electrical stimulation of the trigeminal ganglion produces extravasation from the basilar, anterior inferior cerebellar, and cochlear arteries of albino guinea pigs, and that round window application of capsaicin produces extravasation in the former two sites [8]. The powerful vasodilators SP and NKA are present in the eighth nerve afferent terminals in the organ of Corti and vestibular sensory epithelia [9]. SP and NKA may be released during nerve activation in the same manner as vasodilatory peptides are released by peripheral trigeminal nerve terminals as a neurogenic mechanism in migraine. As CGRP is present in efferent projections to cochlear and vestibular epithelia [10, 11], release is expected during efferent activation. Thus, it is possible that released SP, NKA, and CGRP from trigeminal and eighth nerve fibres could contribute to migraine related dizziness via hormone-like actions on neural and vascular elements.
Clinical Features
Imbalance, episodic spinning or rotating sensation or giddiness or light headedness from few seconds to hours or to Days. Hearing loss is not a feature of common and classical migraine, but 80% of basilar migraine have Sensorineural loss and or tinnitus mimicking the meniere’s syndrome. Severe episodic pulsating headache present. During aura spontaneous and positional nystagmus can be produced, patient may not have any neurological deficiencies.
The family history of headache is present. Triggering points such as stress, physical, mental, menstrual period, contraceptive pills, smoking, exposure to sound and light, loss of sleep, fasting habit and certain foods.
Clinical Tests
Routine and Otoneurological investigations including Complete blood count (CBC), Erythrocyte sedimentation rate (ESR), C Reactive Protein (CRP), Pure tone audiometry, Brainstem audiometry evoked response, Electronystagmography and Magnetic Resonance Imaging (MRI) brain.
Differential Diagnosis
Central
Transient ischemic accident.
Vestibulo-basilar artery insufficiency.
Multiple sclerosis.
Neurodegenerative disorders.
Familial ataxic syndrome.
Peripheral
Meniere’s disease.
Vestibular neuronitis.
BPPV (Benign Paroxysmal Positional Vertigo).
Perilymph fistula.
Therapy
Approach to the treatment of vertigo is symptomatic.
Anticholinergics.
Anticonvulsant (Topiramate, Valproic acid, Lamotrigine).
Antihistamines.
Calcium channel Antagonists (verapamil and flunarizine).
Tricyclic antidepressants (nortriptyline, amitriptyline).
Beta blockers (atenolol, propranolol).
Histamine analogues.
Antiemetics.
Benzodiazeipines (clonazepam).
Corticosteriods.
Serotonin Reuptake Inhibitor (venlafaxine) (Table 1).
Table 1.
Migraine Related Vertigo (MRV) most closely overlaps the presentation of Meniere’s disease
| Difference | Meniere’s disease | MRV |
|---|---|---|
| Headache | −ve | +ve |
| Sensation of blockage | + | − |
| Family history of headache | − | + |
| Duration of vertigo | Less | More than 24 h |
| Phonophobia and photophobia | − | + |
| Hearing loss | + | − |
| Tinnitus | + | − |
| Antimigraine drugs | − | Good response |
Combination Therapy
-
A.
Cinnarizine 20 mg + diminehydronate 40 mg + flunarizine 10 mg.
Cinnarizine and flunarizine are calcium channel blockers which inhibit vestibular hair cells stimuli and regulate their afferent transmission.
Dimenhydrinate is a H1 blocker which acts on central vestibular nuclei and adjacent vegetative centre in brain stem.
Both of these drugs have synergitic effect.
Prophylactic Therapy
-
B.
More than 3 attacks in 2 months = Flunarizine + Diminehydrate + Cinnarizine + Beta blockers.
Key to Better Management
Schedule your day well.
Have a set time for sleeping and wake up.
Eat well balanced regular meal.
Keep a record of possible triggering factors.
You must take the prescribed medicine every day even when you’re not having migraine attack.
These medicines may take time to show benefits.
Hence stay on therapy as prescribed.
Stopping the medicine can worsen the condition.
Preventive therapy when taken for recommended period reduces the frequency severity of migraine attacks.
Conclusion
There is a call for proper diagnosis to address the complaint and manage of symptoms in acute attack and prophylaxis. In addition, this case highlight the ongoing need for proper systematic evaluation, therapeutic management, follow up by ensuring compliance to medication, necessary precautions and life style modification.
Compliance with Ethical Standards
Conflict of interest
None.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Contributor Information
Vithal D. Udagatti, Email: drvithal.du@gmail.com
Rajendran Dinesh Kumar, Email: dinuraj1186@gmail.com.
References
- 1.Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and vestibular vertigo. J Neurol. 2009;256:333338. doi: 10.1007/s00415-009-0149-2. [DOI] [PubMed] [Google Scholar]
- 2.Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States; data from the American Migraine Study II. Headache. 2001;41:646–657. doi: 10.1046/j.1526-4610.2001.041007646.x. [DOI] [PubMed] [Google Scholar]
- 3.May A, Goadsby PJ. The trigeminovascular system in humans: pathophysiologic implications for primary headache syndromes of the neural influences on the cerebral circulation. J Cereb Blood Flow Metab. 1999;19:115–127. doi: 10.1097/00004647-199902000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Goadsby PJ, Lipton RB, Ferrari MD. Migraine—current understanding and treatment. N Engl J Med. 2002;346:257–270. doi: 10.1056/NEJMra010917. [DOI] [PubMed] [Google Scholar]
- 5.Furman JM, Marcus DA, Balaban CD. Migrainous vertigo: development of a pathogenetic model and structured diagnostic interview. Curr Opin Neurol. 2003;16:5–13. doi: 10.1097/00019052-200302000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Dieterich M, Brandt T. Episodic vertigo related to migraine (90 cases): vestibular migraine? J Neurol. 1999;246:883–892. doi: 10.1007/s004150050478. [DOI] [PubMed] [Google Scholar]
- 7.Vass Z, Shore SE, Nuttall AL, et al. Direct evidence of trigeminal innervation of the cochlear blood vessels. Neuroscience. 1998;84:559–567. doi: 10.1016/S0306-4522(97)00503-4. [DOI] [PubMed] [Google Scholar]
- 8.Vass Z, Steyger PS, Hordichok AJ, et al. Capsaicin stimulation of the cochlea and electric stimulation of the trigeminal ganglion mediate vascular permeability in cochlear and vertebro-basilar arteries: a potential cause of inner ear dysfunction in headache. Neuroscience. 2001;103:189–201. doi: 10.1016/S0306-4522(00)00521-2. [DOI] [PubMed] [Google Scholar]
- 9.Scarfone E, Ulfendahl M, Lundeberg T. The cellular localization of the neuropeptides substance P, neurokinin A, calcitonin gene-related peptide and neuropeptide Y in guinea-pig vestibular sensory organs: a high-resolution confocal microscopy study. Neuroscience. 1996;75:587–600. doi: 10.1016/0306-4522(96)00243-6. [DOI] [PubMed] [Google Scholar]
- 10.Marco RA, Hoffman LF, Wackym PA, et al. Distribution of calcitonin gene-related peptide immunoreactivity in vestibular efferent neurons of the chinchilla. Hear Res. 1996;97:95–101. doi: 10.1016/S0378-5955(96)80011-6. [DOI] [PubMed] [Google Scholar]
- 11.Kong WJ, Scholtz AW, Kammen-Jolly K, et al. Ultrastructural evaluation of calcitonin gene-related peptide immunoreactivity in the human cochlea and vestibular endorgans. Eur J Neurosci. 2002;15:487–497. doi: 10.1046/j.0953-816x.2001.01880.x. [DOI] [PubMed] [Google Scholar]