Abstract
Head and neck cancers together (oral cavity, pharynx and larynx) are sixth commonest worldwide and are the commonest cancers in developing countries. The Cancer Project was started in Kheda/Anand, Gujarat, a harvest land of tobacco. The objective of this programme was to indoctrinate the most vulnerable and the least tended upon; the basics of head and neck cancers via the medium of their own kins. Voluntary village health workers were educated and trained to pick up the early signs of head and neck cancers. Oral self examination was taught to them and they went to peripheral villages to screen the population. They would refer suspicious cases to tertiary healthcare centre. The population was enlightened upon the basics of preventable measures, treatment options and rehabilitation facilities for head and neck cancer patients. Knowledge, attitude and practice analysis was done in the population which showed widespread disbelief and false practices. A population of 26,10,432 was surveyed in 1862 villages of which 10,522 (1.1%) individuals successfully quit the habit. The minimally educated workers referred 3309 suspicious individuals to higher centre of which 1890 (57.11%) tested positive for cancer. A lot of resource is put in research and development of rapid diagnosis and complete cure; however such a minimally costing program may help the most in primordial, primary and secondary level of prevention. Such programs should be advocated on the global platform on lines of Breast Self Examination.
Keywords: Prevention of head and neck cancers, Oral self examination, Village health workers, Cancer project
Introduction
Head and neck cancers together (oral cavity, pharynx and larynx) are sixth commonest worldwide and are the commonest cancers in developing countries [1–3]. Tobacco kills nearly 6 million people a year, nearly 80% of the world’s one billion smokers live in low- and middle income countries. 1 person dies every 6 s due to tobacco related cancer death [4]. 1 in 10 adult deaths is attributable to tobacco use. By 2030, more than 80% of tobacco deaths will be in developing countries [5]. Cancer is treatable if detected early. In India, 44.85% adults (57% males and 32.7% females) are addicted to some form of tobacco [5]. Worldwide 47% men and 12% women are habituated to tobacco smoking [6]. Only two cases of tobacco unrelated head and neck cancer have been observed in the last 3 years in our institute. Tobacco is the major crop in our region, which makes its availability easy and cheap that contributes to the rampant habit of tobacco abuse here, finally culminating to high prevalence rates of head and neck cancers in this region. However, the pattern of disease has changed in the recent few years.
The previous decades showed male predominance more so in the upper middle age group.
There is now a paradigm shift in which incidence amongst young individuals has quadrupled.
This suggests that the current measures are inadequate in curbing the disease. The average age of initiation of tobacco abuse in India is as low as 17.8 years [7]. More often head and neck cancers are diagnosed when the tumor is locoregionally advanced [8]. The prognosis at this stage is grim as the primary tends to advance into the deeper tissue planes till then.
It came to our notice that it is the sheer lack of fundamental cognizance that is to be blamed for the current situation. The worldwide propaganda of breast self-examination has revolutionized the detection rates of breast lumps [9]. Widespread demonstration of breast self-examination from the most developed to the least developed countries deserves credit for the same. Thus, the program—“Cancer Project” was initiated with the same ideals.
Aims
The prime objective of the program was a simple triad chain—Creating Awareness ≫ Early Detection ≫ Rapid Diagnosis.
This triad would promote prior treatment eventually steering to the ultimate goal of curing cancer. The crux is simple—the minimally educated can create awareness and make a major impact.
Methodology
Knowledge, attitude and practice (KTP) assessment was done in the target population to understand their perception towards tobacco addiction and its relation to head and neck cancer. Also their behaviour towards the disease, their knowledge on the natural history, available treatment options and prognosis was noted (Fig. 1).
Fig. 1.

An elderly man with a fungating growth believing that a black thread around his neck is more likely to relieve his miseries than a qualified doctor
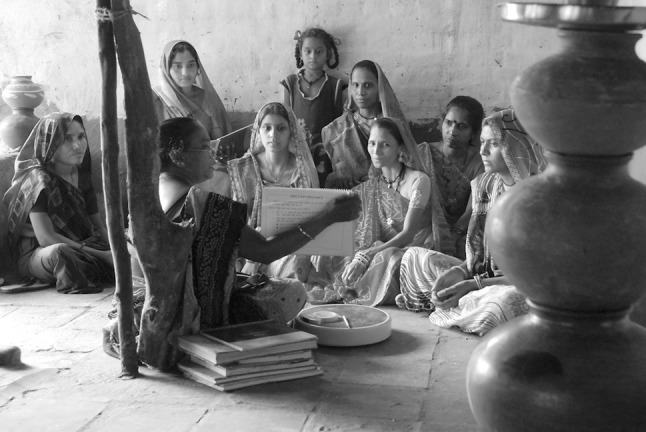
Next voluntary individuals from the native population with village health workers were invited for training. Some of these health workers were those working under the Maternal and Child Health Program running under the Government of India. Others were voluntary individuals from the population. These health workers were trained by specialised health professionals in the basics of head and neck cancers, their common presentations, the flag signs and the warning signs (Table 1). The mean education level of these workers was eighth or ninth grade, hence they were trained accordingly. The observations from the KAP analysis were kept in mind while educating these workers. Certain sessions were held in the community such as local schools or village assembly. At times the workers were transported to the home institute where they would be taught by the expert faculty.
Table 1.
Early signs of head and neck cancer
| Flag signs |
|---|
| Change of voice > 15 days |
| Non-healing red/white patch in oral cavity |
| Trismus |
| Difficulty in swallowing > 15 days |
| Neck or cheek swelling > 7 days |
| Oral/throat/nose bleed |
| Breathing difficulty/noisy breathing |
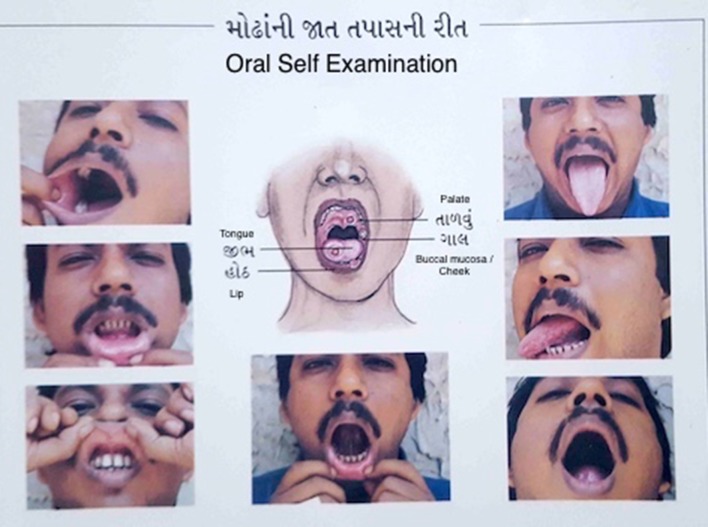
Oral self examination (OSE)—the heart of this program was inculcated in the minds of the workers. The simplicity of performing this checkup was emphasised. Every volunteer was given a Health Education Manual/Booklet which contained all the particulars on the telltales of head and neck cancers regarding the causative factors, early and late clinical features with treatment modalities and preventive measures along with a descriptive portrayal of performing OSE (Fig. 2).
Fig. 2.
A page from the health information book showing ways to perform oral self examination (OSE)
The health workers were entitled with specific villages. They assessed the prevalence of tobacco addiction in the population and coaxed the addicts to quit. Next, the workers evaluated their basic oral, throat and neck examination and looked for any of the aforementioned flag signs. The individuals were enlightened with the kernel of this program—OSE. OSE comprises of a variety of manoeuvres by which different parts of the oral cavity and neck can be evaluated. These simple tasks were demonstrated by the health workers and performed by the villagers (Fig. 3).
Fig. 3.
A page from the health information booklet showing the simple way to self examine the oral cavity using a mirror
In this survey, the workers came across suspicious cases which they referred to tertiary health care centres for further workup. The population was enlightened upon the basics of preventable measures, treatment options and rehabilitation facilities for head and neck cancer patients. The workers helped the villagers to overlook their disbeliefs. Motivating these individuals to seek expert medical care was probably the most demanding task of all.
The program was carried out for 3 years. The health workers would go every 6 months to evaluate the population. Those who did not consume tobacco for 6 months were labeled as free of addiction. In the follow-up surveys they also ensured that the individuals who were diagnosed positive for malignancy initiated, continued and completed the full treatment. Treatment defaulters were rigorously followed up and coaxed to complete the treatment.
Results
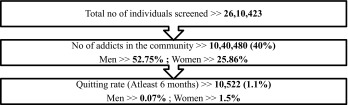
Over a period of 3 years, 1862 villages were surveyed. A total of 5214 village health workers were trained. These health workers came in direct contact with 5,64,202 households residing a population of 26,10,423 individuals. Thus, 2.8 workers were assigned to one village and each worker screened 500 individuals. In their survey, they came across 10,40,480 (39.89%) individuals who were addicted to some form of tobacco. Prevalence of addiction amongst men was 52.75% and that in women was 25.86%. We were successful in 10,522 (1.1%) individuals to quit the habit. Amongst women the quitting rate was 1.5% (5018), whereas in men, it was 0.07% (5504) (Table 2).
Table 2.
Addiction profile of the target population
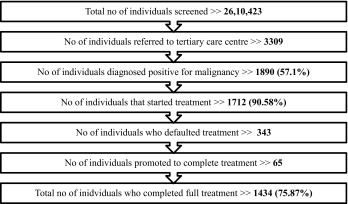
3309 suspicious individuals were referred to tertiary care institute. 1890 (57.1%) of them were diagnosed positive for malignancy. 1712 (90.58%) started treatment. However, 343 were treatment defaulters. The health workers went to the villages to promote them to resume the treatment. 65 restarted treatment. So finally, 1434 (75.87%) completed the entire treatment (Table 3).
Table 3.
Gist of results of the entire program
Discussion
The KAP analysis showed that the level of awareness in our rural population was very low. A major section made a direct relation of cancer to death. They believed that cancer is incurable and that no treatment in any form is effective. Various absurd hypotheses existed amongst the population in which one said that cancer is a curse by the Gods for their sins. Alternate forms of medicine with falsified superstitions were being practiced rampantly (Image 1). The delusion existed that though tobacco caused cancer in others, it would exclusively spare them.
A study in Britain showed that only 33.4% individuals recognised white patches in the oral cavity as a sign [10]. Over 75% individuals know that their addictive habit is likely to cause cancer [11]. Elango et al. have noted that the awareness of oral cancer was satisfactory, though certain gaps exist, pointing to a need for targeted health education and risk factor cessation counselling [12].
This program not only evaluated the level of awareness in the community, it also promoted them to quit tobacco, educated them upon the early signs of cancer and pushed them to attend a cancer clinic at the earliest. Never before has a study been conducted that covered such a large population. Various studies have been done on a limited scale which show that such projects are feasible and should be implemented on a wider platform [12, 13].
Inspite of diagnostics and management of head and neck cancer advancing rapidly, detection rates continue to lag. As the time for malignancy confirmation gets delayed, staging tends to advance. Higher the staging, the options for treatment modalities narrow down. For example, a tongue cancer diagnosed in Stage I would undergo a simpler operative requiring a wide excision with primary closure along with a suitable neck dissection; in comparison, the same patient presenting in Stage IV would advocate a complex surgery involving excision part of the mandible along with a reconstructive procedure which would lead to high post-op morbidity and poor quality of life. The cost for the same patient rises to almost four to five folds. Invariably, higher staging at presentation has an adverse effect on the final clinical outcome, disease prognosis and economic burden.
Historically death rate associated with head and neck cancers is particularly high due to the cancer being discovered late in its development. It is usual for patients to avoid or ignore the disease in the early stages. An American study has concluded that screening programs could be a reason for improvement in survival in head and neck cancer patients [14]. This program mainly focuses on picking up such cases in their early stages.
In case an educated health care professional was to undertake this project, the personnel would not have been able to penetrate the masses. He would be looked upon as a foreigner who has come to cheat them. College students have also undertaken this task [15]. In contrast expertise imparted by their own brethren would get easily digested, absorbed as well as assimilated.
It is seen here how the minimally educated can make a difference. Out of the suspicious cases referred by the workers, almost 58% were diagnosed positive for malignancy, a figure that should be reckoned with, especially considering their level of education, comprehension and understanding. In another study by Elango et al., the concordance rate for trained health workers was 72%, but compliance to seek treatment was merely 32%, as compared to our study in which 75.87% [16]. Continuous follow-up at six monthly intervals could be the reason of our satisfactory compliance rate.
Oral self examination taught to the villagers is the central core of the program.
Individuals enlightened with this pioneering practice would bring about continual progressive change. OSE would promote them to seek early intervention. The sensitivity of OSE has been reported as 33% and the specificity as 54% [17]. We do not have data on this from our study, and more research should be done on the same.
Head and neck cancers are known as lifestyle disorders. Thus, changing life trends in terms of Tobacco de-addiction is another area which was addressed. With increase in this habit worldwide, radical measures are warranted. National tobacco quitting rates have been in the range of 4.8–5.3%, which were higher than ours [7]. This could be due to regional variation.
Conclusion
Towards the end of the Cancer Project, there were still 25% malignant individuals who did not initiate or complete the entire treatment. This program directs to such individuals and all those susceptible in the entire world. The cases diagnosed should be perceived as the tip of the iceberg. The ultimate goal of healthful living can be achieved only by innate participation of the population. We strongly recommend all Health Professionals to institute the basics of OSE in their patients. This could help us improve the mortality and morbidity indicators in head and neck cancers.
A lot of energy and resource is put in research and development of rapid diagnosis and complete cure; however such a minimally costing program may help the most in primordial, primary and secondary level of prevention. A recent news release in aetiology of Cancer in John Hopkins Medicine showed that the only treatment of cancer is early detection, when they can be managed by surgery [18]—this line holds greatest significance in head and neck cancers. This program’s success is an example that could be used as a pilot in various countries specifically developing countries like ours.
Acknowledgements
Humble thanks to The Tribhuvandas Foundation, Anand, Gujarat, India for their generous contribution.
Compliance with Ethical Standards
Conflict of interest
The authors declare they have no conflict of interest.
Research Involving Human Participants and/or Animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research and ethics committee and with the 1964 Helsinki declaration and its later amendments.”
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.International Agency for Research on Cancer. World Health Organization (WHO). GLOBOCAN 2012 (2012) Estimated cancer incidence, mortality & prevalence worldwide. http://globocan.iarc.fr/Pages/fact_sheets_population.aspx. Accessed 26 Jan 2017
- 2.Parkin DM, Stjernsward J, Muir CS. Estimates of the worldwide frequency of twelve major cancers. Bull WHO. 1984;62:163–182. [PMC free article] [PubMed] [Google Scholar]
- 3.Joshi P, Dutta S, et al. Head and neck cancers in developing countries. Rambam Maimonides Med J. 2014;5(2):e0009. doi: 10.5041/RMMJ.10143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO (2017) Media centre; tobacco. http://www.who.int/mediacentre/factsheets/fs339/en/. Accessed 17 June 2017
- 5.WHO Report on Global Tobacco Epidemic (2008). http://www.who.int/tobacco/mpower/mpower_report_full_2008.pdf. Accessed 17 June 2017
- 6.The Oral Cancer Foundation, WHO (1999). http://www.oralcancerfoundation.org/tobacco/. Accessed 17 June 2017
- 7.Ministry of Health & Family Welfare, Government of India, World Health Organization (WHO). Global Tobacco Surveillance System (GTSS). Centre for Disease Control & Prevention (CDC). Global Adult Tobacco Survey (GATS). Fact Sheet India 2009–2010. http://www.who.int/tobacco/surveillance/en_tfi_india_gats_fact_sheet.pdf. Accessed 17 June 2017)
- 8.Cleveland Clinic (2010) Centre for continuing education. Disease management: head and neck cancer (published August 2010). http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/hematologyoncology/head-and-neck-cancer/Default.htm. Accessed 17 June 2017
- 9.Mena M, Wiafe-Addai B, Sauvaget C, Ali IA, Wiafe SA, Dabis F, Anderson BO, Malvy D, Sasco AJ. Evaluation of the impact of a breast cancer awareness program in rural Ghana: a cross-sectional survey. Int J Cancer. 2014;134:913–924. doi: 10.1002/ijc.28412. [DOI] [PubMed] [Google Scholar]
- 10.West R, Alkhatib MN, McNeill A, Bedi R. Awareness of mouth cancer in Great Britain. Br Dent J. 2006;200:167–169. doi: 10.1038/sj.bdj.4813197. [DOI] [PubMed] [Google Scholar]
- 11.Mehta FS, Gupta PC, Bhonsle RB, Murti PR, Daftary DK, Pindborg JJ. Detection of oral cancer using basic health workers in an area of high oral cancer incidence in India. Cancer Detect Prev. 1986;9(3–4):219–225. [PubMed] [Google Scholar]
- 12.Elango JK, et al. Factors affecting oral cancer awareness in a high-risk population in India. Asian Pac J Cancer Prev. 2009;9(4):627–630. [PubMed] [Google Scholar]
- 13.Gupta PC, Pindborg JJ, et al. Intervention study for primary prevention of oral cancer among 36 000 Indian tobacco users. The Lancet. 1986;327(8492):1235–1239. doi: 10.1016/S0140-6736(86)91386-3. [DOI] [PubMed] [Google Scholar]
- 14.Carvalho AL, Nishimoto IN, Califano JA, et al. Trends in incidence and prognosis for head and neck cancer in the United States: a site-specific analysis of the SEER database. Int J Cancer. 2005;114:806–816. doi: 10.1002/ijc.20740. [DOI] [PubMed] [Google Scholar]
- 15.Mathew B, Sankaranarayanan R, Wesley R, Nair MK. Evaluation of mouth self examination in the control of oral cancer. Br J Cancer. 1995;71(2):397–399. doi: 10.1038/bjc.1995.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elango KJ, Anandkrishnan N, Suresh A, Iyer SK, Ramaiyer SK, Kuriakose MA. Mouth self-examination to improve oral cancer awareness and early detection in a high-risk population. Oral Oncol. 2011;47(7):620–624. doi: 10.1016/j.oraloncology.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Scott SE, Rizvi K, Grunfeld EA, McGurk M. Pilot study to estimate the accuracy of mouth self-examination in an at-risk group. Head Neck. 2010;32(10):1393–1401. doi: 10.1002/hed.21341. [DOI] [PubMed] [Google Scholar]
- 18.John Hopkins Medicine. The John Hopkins University (2015) Bad luck of random mutations plays predominant role in cancer, study shows. Last updated January 07, 2016. http://www.hopkinsmedicine.org/news/media/releases/bad_luck_of_random_mutations_plays_predominant_role_in_cancer_study_shows. Accessed 17 June 2017)