Abstract
The periocular area may be affected by infectious or noninfectious diseases such as inflammatory dermatoses, systemic disease, drug reactions, benign and malignant lesions, traumatic lesions, and esthetic complications. We present a review of the most common periocular dermatoses.
Introduction
The functional purpose of the periocular area stands out among all other purposes. The main structure must be preserved to maintain the sight function and the eyelids are responsible to physically protect the eyeball, acting as a barrier to foreign objects and trauma. The lubrication of the cornea by the lacrimal film is another essential role, which is fulfilled by making the palpebral anatomy suitable through thin and flexible skin that covers the deeper structures (Sand et al., 2016).
The eyelashes originate in the free palpebral border and their main function is the protection of the eye by closing with reflex stimulation. The upper eyelashes curve upward and the lower ones downward so they do not interfere with each other. Individuals of all races have them with variations in length and thickness, but they are always present; thus, their absence is pathologic (Vij and Bergfeld, 2015).
The periocular area is also a very relevant aesthetic unit of the face and is one of the first to show signs of aging. For this reason, this area is frequently treated with cosmetic intentions (Neimkin and Holds, 2016).
The periocular area may be affected by infectious or noninfectious diseases such as inflammatory dermatoses, systemic disease, drug reactions, benign and malignant lesions, traumatic lesions, and esthetic complications.
Infections
Bacteria, mycobacteria, fungi, virus, and ectoparasites can be responsible for periocular infections. Some of these have particular clinical characteristics or incidence, depending on the particular location. Among the common infections are those caused by bacteria of normal skin flora such as coagulase negative Staphylococcus, Staphylococcus aureus, and Propionibacterium acnes. They are frequently encountered as contributors to blepharitis and although their presence cannot always be considered pathologic, they can participate in the meibomian gland dysfunction (Hossain and Konstantopoulos, 2015).
Other frequent findings are Demodex folliculorum and Demodex brevis, which are two species of the commensal mite that human beings host. Demodex folliculorum is located in the follicular infundibulum and Demodex brevis in the sebaceous and Meibomian glands. The infection is not related to immunosuppression, but when the number of mites increases, they cause symptoms such as itching, burning, foreign body sensation, crusting and redness on the eyelid margin, blurred vision, and chronic blepharitis (Fig. 1; Kosik-Bogacka et al., 2013; Tenorio-Abreu et al., 2016; Yun et al., 2013).
Fig. 1.

Demodecidosis that causes chronic blepharitis.
The most common and quite ominous viral infection is the one caused by the reactivation of the sensory ganglia of the varicella zoster virus (VZV), particularly when cell-mediated immunity declines (Fig. 2, Fig. 3). This disease has become more common for unknown reasons, and its identified risk factors are a personal and familial history of herpes zoster (HZ), stress, sleep disturbances, depression, and weight loss (Marin et al., 2016). The trigeminal nerve is the third most frequently affected area (13%) after the thoracic and lumbar areas. The first division of the trigeminal nerve is 20 times more commonly involved, thus affecting the ocular/periocular area (Bandeira et al., 2016; Ganesan et al., 2016); although rare, it may present severe complications such as blindness, nerve palsies, or intraocular involvement such as retinitis. The herpes simplex virus also can affect the periocular area.
Fig. 2.
Herpes zoster.
Fig. 3.

Severe necrosis and crusting originated by herpes zoster.
More common complications include bacterial infections, scabs and scarring, and postinflammatory hyperpigmentation. As with HIV, infected individuals have a higher risk of presenting with HZ. An Indian study reported that 37.7% of cases with HZ also had HIV. HIV testing is suggested for patients younger than 50 years of age or those who present with more than one dermatomal involvement (Bhandage et al., 2016).
The poxvirus that is responsible for molluscum contagiosum is also frequently seen in the periocular area, particularly in the two main affected groups—children (Fig. 4) and young adults—although the HIV-infected population probably will be added in the near future. The main affected areas in children are the trunk, extremities, and face. In young adults, the predominant corporal surface is the genital area because the poxvirus is primarily transmitted sexually (Gonnering and Kronish, 1988). In patients who live with HIV/AIDS, these lesions are frequently found on the face, particularly in the beard and periocular areas. The lesions tend to be more recurrent and larger in size, which sometimes complicates treatment because topical treatments can cause severe damage when in contact with the eye structures. Warts also can affect the periocular area (Fig. 5).
Fig. 4.
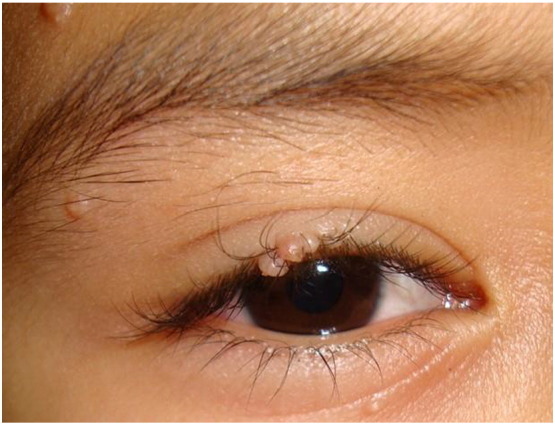
Molluscum contagiosum in the eyelash area.
Fig. 5.
Viral warts.
Fungal infections may be systemic, subcutaneous, or superficial, and the most benign forms are the latter ones. Periocular tineas are rare and frequently misdiagnosed, particularly those that clinically show an important inflammatory response. The most probable complication is the development of tinea incognita secondary to the topical administration of steroid medications because of a misdiagnosis of the disease, which further distorts the clinical picture and delays an adequate diagnosis. The key features to a correct diagnosis are the scale in the lesion, loss of eyelashes or eyebrows, and a history of exacerbation with the administration of steroid medications (Finger Basak et al., 2011). Subcutaneous mycosis such as micetoma, chromoblastomycosis, and sporotrichosis (Fig. 6) are rare in this location but have been reported, such as a case of sporotrichosis with eyelid involvement after a traumatic injury with a subsequent development of nodular subcutaneous lesions with lymphangitis dissemination (Iyengar et al., 2010).
Fig. 6.

Sporotrichosis.
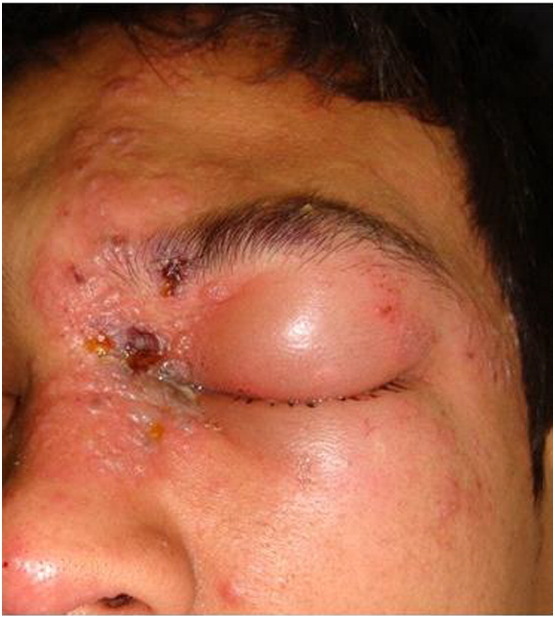
The most severe infections are mucormycosis and aspergillosis. The first is most commonly caused by Rhizopus (Mukherjee et al., 2016). Mucormycosis is an opportunistic infection with an increasing incidence in patients who are immunosuppressed or those with metabolic acidosis. The rhino orbital cerebral presentation is the most common form, consisting of 40% of the cases. As the fungus invades the blood vessels, it causes thrombosis, emboli, and ischemia that rapidly evolve into the necrotic areas. Initially, the most common signs are nasal obstruction or discharge, edema, unilateral ptosis, exophthalmos, and affected necrotic areas. A prompt approach to diagnosis is made by a direct potassium hydroxide mount that must be confirmed by the results of a culture, histopathology, and imaging such as magnetic resonance imaging scans because this is a life-threatening infection that can leave severe sequels. Treatment may include surgical debridement, which can result in severe disfigurement, and systemic antifungal therapy. The patient’s prognosis for recovery relies on a prompt diagnosis and adequate treatment (Jiang et al., 2016). The main differential diagnosis is made with aspergillosis, which may have a slightly better prognosis. Histoplasma capsulatum rarely affects the periocular area (Fig. 7; Carlisle and Digiovanni, 2015; Tambe et al., 2012).
Fig. 7.
Histoplasmosis.
Exposed areas of the skin such as the face are common sites of involvement for anthrax, which is caused by Bacillus anthracis. Three main clinical forms exist including gastrointestinal, cutaneous, and inhalational anthrax, and the skin is the most common place of presentation (95%). The eyelids are a frequent site of involvement, and adequate and prompt treatment is required to prevent complications such as scarring that can lead to ectropion and corneal scars. Anthrax infection begins as an erythematous patch that enlarges and becomes a papule with fine tight shiny yellow or pink vesicles accompanied by edema and eventually progresses to necrosis. Prior contact with animals is an important piece of information to help formulate the diagnosis (Gelaw and Asaminew, 2013). The diagnosis is clinical and supported by Gram stains from an imprint smear and culture. The main differential diagnosis is made with necrotizing fasciitis and the early stages of mucormycosis.
Other rare and exceptional infections have been reported, including bacillary angiomatosis, which is an infection caused by Bartonella (B. quintana and B. henselae) and predominantly found in patients who are immune-compromised. This was also the first description of an HIV-positive patient. Since the evolution of combined antiretroviral therapy (cART), incidence rates have been significantly reduced, and it is now a rare finding. However, it is important to remember that the main differential diagnoses are common dermatoses such as chalazion and hemangioma. The final diagnosis is made with dermatopathology, where vascular proliferation with histiocytic infiltrate predominate and the etiological agent is made evident with a Warthin Starry stain. A diagnosis on the basis of a polymerase chain reaction is another option. A full resolution is achieved with macrolides or tetracycline (Mcelroy et al., 2013; Murray et al., 2010). In the case of Chagas disease, Romaña’s sign can be observed as painless periorbital swelling during the acute phase of the infection (Romaña, 1935).
As part of the clinical picture of lepromatous leprosy, patients show skin adnexa involvement that is seen as alopecia of the eyebrows and eyelashes. Patients with the lepromatous leprosy form of the infection can also present with corneal nerve thickening and nodules (Jurado et al., 2015). Isolated cases of Nocardia infection have been documented. The triad of local trauma to the site, multiple discharging sinuses, and bone involvement with a characteristic moth-eaten appearance suggests the diagnosis (Rath et al., 2012). Infestations of Phthirus pubis (palpebral pediculosis) are not as rare as expected, and the treatment includes oral ivermectin and physical removal of the parasite (Oguz and Kilic, 2006).
Dermatological diseases
Urticaria and angioedema are highly prevalent diseases that affect between 0.3% and 11.3% of the world population. Twenty percent of the population will experience at least one episode during their lifetime that affects only skin or involves mucosal tissues such as with angioedema. With regard to the etiology, most patients run an idiopathic course. Only a few patients can identify the triggering factor, which most commonly is for physical urticaria. It is generally difficult to treat because the triggering factor is difficult to identify and patients are often frustrated with their lower quality of life. Urticaria is more common in female adults, and autoimmune alterations are detected in 40% to 45% of patients with chronic spontaneous urticarial, which is the same rate as the associated angioedema; only 10% of patients present with isolated angioedema. Periocular disease manifests as angioedema alone or in association with hives (Fig. 8) and runs the same course as other body areas that are affected, although the cosmetic appearance and vision impairment are extremely relevant for the treatment options (Sánchez-Borges et al., 2012; Wu et al., 2016).
Fig. 8.

Urticarial and angioedema.
Vitiligo is a hypo-pigmentary disease that affects 1% of the population with 30% of familial cases. This acquired disease is characterized by progressive depigmentation that very commonly affects the face (80%) and thus the periocular area (Fig. 9) Vitiligo runs an unpredictable course; however, facial lesions are known to respond better to treatment when compared with other body areas. Although most patients develop the disease before the age of 25 years, a study reported that new lesions in women mostly occurred on the face in the perioral and periocular areas, but the reasons are not fully elucidated. Apparently, the most important differences are related to local trauma and the Koebner phenomenon. Treatment with pimecrolimus 1% twice daily has proven effective with eyelid involvement (Speeckaert and van Geel, 2014; Souza Leite and Craveiro Leite, 2007).
Fig. 9.
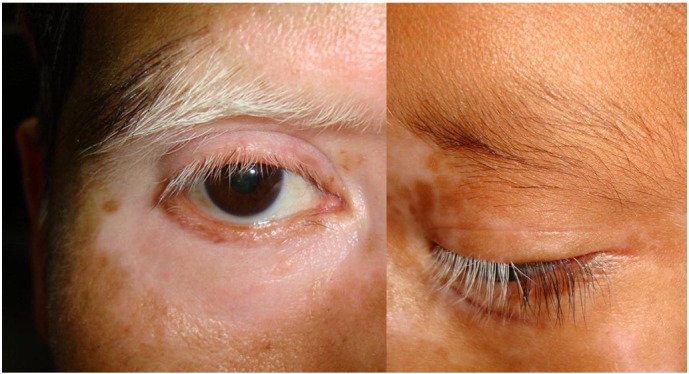
Vitiligo.
A particular characteristic of patients with atopic disease is the presence of Dennie-Morgan fold in the lower eyelids, which currently is considered a minor criterion for atopic dermatitis and present in up to 84% of cases. Atopic disease may also be associated with dark circles under the eyes. The physiopathology is not fully understood, but when clinically observed, the diagnosis of atopic dermatitis with or without allergic rhinitis should be suspected (Fig. 10; Blanc et al., 2015).
Fig. 10.
Atopic dermatitis.
Rosacea is a chronic inflammatory disease with relapses that affects the facial skin and may involve the eyes, in which case it is known as oculorosacea. Its etiology is poorly understood, but identification involves factors such as ultraviolet (UV) exposure, vascular hyperreactivity, and vasodilation. Ocular affection may or may not be associated with facial skin disease, and it is similar to chronic blepharitis with chronic low-grade conjunctivitis and hyperemia. Severe cases show peripheral corneal vascularization, thinning, and ulceration (Rambhatla et al., 2015).
Periocular dermatitis can be observed as a manifestation of periorificial dermatitis where eczema, erythema papules, and pustules are seen in varying degrees and the absence of comedones helps differentiate from acne. The dermatitis is frequently associated with the use of fluorinated steroid medications that are administered topically or systemically such as the inhaled forms of the treatment.
Contac dermatitis is a common finding in the periocular area because of environmental allergens but mostly secondary to cosmetic applications and the use of eye drops. The eyelids are particularly exposed to this ailment because of their anatomy, which is semi-occlusive in the upper eyelid to anything applied to that area. Also, this skin is the thinnest of the entire body surface and is in constant contact with the hands, which transport allergens very effectively. This can be an occupational disease with a high economic burden (Rojo-España et al., 2011).
Systemic diseases
Almost all connective tissues and autoimmune diseases can present periocular manifestations. For instance, discoid lupus erythematosus, which is a cutaneous variant of the autoimmune disease, affects sun-exposed areas that in 6% of cases includes the eyelids and eyebrows. Discoid lupus erythematosus presents as raised erythematous scaly lesions; when present only in the periocular area, diagnoses can include blepharon-conjunctivitis, allergic dermatitis, psoriasis, lichen planus, and even sebaceous or basal cell carcinoma (Gupta et al., 2012). Another autoimmune disease, dermatomyositis, frequently presents with a characteristic periocular rash (heliotrope rash) that is present in 88% of cases (Fig. 11) and part of the Bohan and Peter diagnostic criteria. This disease presents mainly with skin and muscle involvement, although the joints and organs such as esophagus, lungs, and heart may be involved (Troyanov et al., 2014).
Fig. 11.

Dermatomyositis with the periocular rash (heliotrope rash) characteristic.
For amyloidosis, the most common clinical presentation of skin involvement is the presence of petechiae, purpura, and/or ecchymoses. The other forms are rarer, skin-colored macules, papules, or nodules with a predilection for flexural areas such as the eyelids (Fig. 12) and the axillae, inframammary, inguinal, and anogenital areas. The diagnosis is made on the basis of histopathologic test results (Kumar et al., 2013).
Fig. 12.

Amyloidosis with petechiae.
Idiopathic orbital inflammatory syndrome is a nonspecific inflammation of the ocular region and is considered an exclusion diagnosis for other inflammatory diseases, such as systemic lupus erythematosus, that manifest as keratoconjunctivitis sicca, periocular skin lesions and inflammation, retinal hemorrhages and vasculitis, and inflammation of any of the eye structures. The variation of lupus that involves the adipose tissue (lupus erythematosus profundus) can also involve the periocular structures (Ohsie et al., 2012; Qureshi et al., 2015). Photoinduced dermatosis can affect the eyes and periorbital area because of their photo-exposed location.
Actinic prurigo is a dermatosis that is induced by sunlight. This dermatosis presents during childhood and can resolve by the time the patient reaches adolescence. It affects exposed skin, the lips, and conjunctiva. Actinic prurigo has a higher prevalence in mestizos and a strong association to human leukocyte antigen DR4 (gene products DRB1*0407), which suggests genetic susceptibility. Erythematous papules and nodules appear in sun-exposed areas of the body, hemorrhagic crusts, or lichenification and heal with scarring. Cheilitis is also very common.
Chronic actinic dermatitis is an uncommon form of chronic eczematous dermatitis with predominantly photodistribution. Its pathophysiology includes induction by UV radiation and is rarely visible by light. It is probably a delayed type of hypersensitivity against photoinduced cutaneous antigens similar to what is observed in allergic contact dermatitis. Clinically, lichenified lesions are seen in older men and, as with most of the photodermatoses, it spares the upper eyelids, nasolabial folds, retroauricular areas, and submental areas, which are generally not exposed to UV radiation. The main differential diagnosis is drug-induced photosensitivity and T cell lymphoma (Rambhatla et al., 2015).
Hydroa vacciniforme is a rare, pediatric form of photodermatosis. Children with this dermatosis present with clustered pruritic erythematous macules on photo-exposed skin, which may occur as quickly as after a few hours of exposure. The skin lesions progress to vesicles and leave pock-like scars. Solar urticarial is associated to UV B, UV A, or visible light range. Although the main sites affected are photo-exposed skin, some reports mention associated snowflake corneal dystrophy. This disease occurs predominately in female patients during the fourth and fifth decades of life and is thought to be induced by an immunoglobulin E-mediated response to a photoinduced allergen (Rambhatla et al., 2015).
Photo allergy is a delayed type of hypersensitivity that presents in previously sensitized individuals as a response to a photoallergen that is applied to the skin or ingested. Photoprotected sites (e.g., upper eyelids) are generally spared unless the reaction is very strong. These dermatoses are best diagnosed by photo-patch testing (Rambhatla et al., 2015).
Contrary to a photo allergy, phototoxicity does not require previous sensitization because it causes direct tissue and cellular injury after UV radiation-induced activation of any phototoxic agent. This can occur in any individual; in these patients, the upper eyelids are usually spared, but the lower ones are not because these are typically sun-exposed. Patients who are treated with 200 mg doxycycline per day commonly present with this reaction (Rambhatla et al., 2015).
Genodermatoses are inherited skin diseases often associated with disorders in multiple organs and many involve the periocular area (Aravindha Babu et al., 2015). Xeroderma pigmentosum is an autosomal, recessive genodermatosis that is characterized by intense photosensitivity during early childhood and manifests with sunburns and freckling on sun-exposed areas of the skin. These children have a high risk of developing skin cancer before adolescence because of the defective DNA repair system. With regard to the eyes, up to 40% of these pediatric patients show marked light sensitivity and blepharospasm. Other findings are madarosis, ectropion, symblepharon, ankyloblepharon, corneal opacification and neovascularization, pterygia, keratopathy, melanoma, and eyelid malignant lesions such as squamous cell carcinoma (Rambhatla et al., 2015).
Congenital erythropoietic porphyria is rare autosomal recessive disease that is characterized by decreased catalytic activity of the uroporphyrinogen III synthase. Dermatosis onset is early life with severe photosensitivity that is initially seen as vesicles, erosions, and ulcerations accompanied by pruritus and a burning sensation. These lesions cause mutilation, especially on the hands and face, with severe scarring. The eyebrows and eyelashes are commonly involved with conjunctival and corneal manifestations that parallel those of exposed skin (Rambhatla et al., 2015).
Lipoid proteinosis or Urbach-Wiethe syndrome is an autosomal, recessive genodermatosis due to an abnormal lipid protein complex deposition in the skin and in mucous membranes of the respiratory tract with pathognomonic moniliform blepharosis that is mainly diagnosed by ophthalmologists (Kamath et al., 2015).
Rothmund-Thomson syndrome is another rare, autosomal recessive disease that is characterized by an increased susceptibility to malignancies related to sun exposure. Skeletal and dental abnormalities can be observed as well as ocular alterations (Rambhatla et al., 2015). Goltz syndrome (focal dermal hypoplasia) is another X-linked dominant genodermatosis with multiple cutaneous features that are related to mesodermal and ectodermal tissues. Up to 40% of patients with Goltz syndrome will have ocular involvement (Rambhatla et al., 2015).
Drug reactions
The spectrum of fixed drug eruption (Fig. 13, Fig. 14), Stevens Johnson syndrome (Fig. 15), and toxic epidermal necrolysis (TEN; Fig. 16) are immune-mediated mucocutaneous drug reactions. The first drug reaction is more common; TEN is the rarest form but also the most severe and life threatening. Reactions with ocular involvement are the most feared because of postinflammatory sequalae that include scarring and corneal blindness, and up to 79% of affected individuals who survive will live with significant ocular disease (Saeed and Chodosh, 2016).
Fig. 13.

Fixed drug eruption to acetaminophen.
Fig. 14.
Stevens Johnson syndrome to albendazole.
Fig. 15.

Stevens Johnson syndrome to allopurinol.
Fig. 16.

Toxic epidermal necrolysis to nonsteroidal anti-inflammatory drugs.
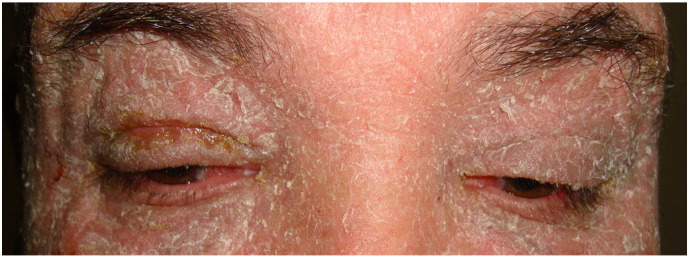
Erythroderma is a generalized skin reaction to the exacerbation of certain skin conditions or an adverse drug reaction. Erythroderma is desquamative with variable exudate, affects the temperature regulation, and has high protein loss. Because it affects the entire skin surface, the periocular area is frequently involved (Fig. 17; Lemmenmeier et al., 2016; Rener-Prmec and Balkovec, 2014).
Fig. 17.
Erythroderma.
Benign lesions
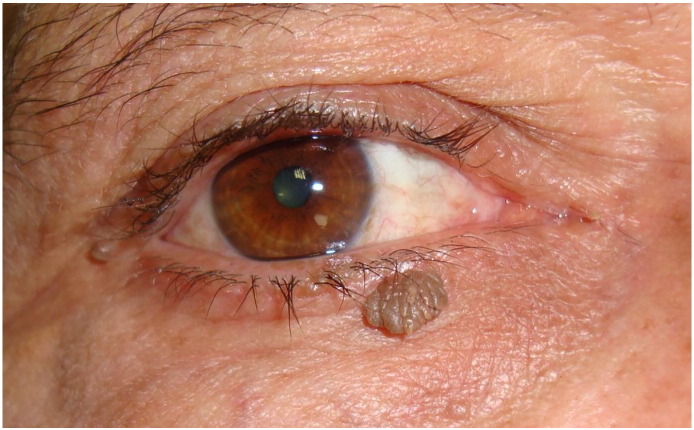
Most of the periocular neoplasias are benign lesions but must always be evaluated to rule out malignant forms. One study reported that almost 60% of eyelid lesions are benign; of these, 18% were histologically reported as cysts, 13% as seborrheic keratosis, and 13% as nevi. Hemangiomas accounted for 4% of the lesions. The benign lesions are diagnosed typically in younger patients compared with malignant lesions, and they show no preference for upper or lower eyelid involvement (Asproudis et al., 2015). Acrochordons, or skin tags, are extremely common benign neoplasms that are located in areas with thin, flexible skin such as the axillae, neck, groin, and eyelids (Fig. 18). Clinically, skin tags are pedunculated skin colored or light-to-dark brown color depending on the patient’s skin tone. As patients get older, skin tags can also be related to metabolic syndrome and pregnancy. The main differential diagnoses are neurofibromas, seborrheic keratosis, and pedunculated nevi (Higgins et al., 2015).
Fig. 18.
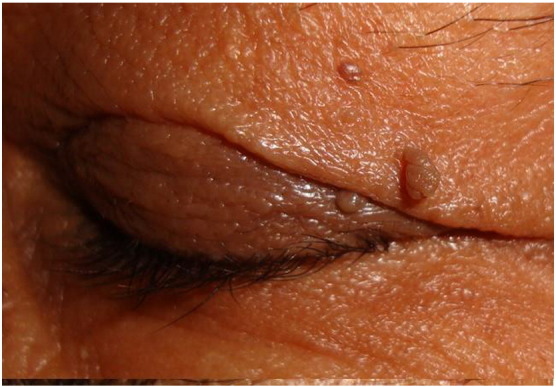
Acrochordons.
Some of the most commonly encountered benign adnexal tumors are syringomas, which derive from the eccrine glands. The classic clinical presentation affects mostly the eyelids (Fig. 19) of women with multiple 1 to 3 mm sessile, skin-colored neoplasias, bilateral, and asymptomatic (Ghanadan and Khosravi, 2013). Eccrine or apocrine hidrocystomas are another type of benign adnexal tumor that is mostly found on the eyelids (Fig. 20). Derived from the sweat glands, they mostly affect middle-aged women and clinically appear as translucent papules with a bluish discoloration that are a few millimeters in size, either solitary or multiple. Eccrine-derived tumors are more common in the periocular area. Although they are asymptomatic and benign, they may resemble basal cell carcinoma or other malignant tumors for which resection is required to obtain a histological confirmation for the diagnosis because the malignant counterpart has a high morbidity rate (Al-Faky et al., 2009; Jabbar et al., 2013).
Fig. 19.
Syringomas.
Fig. 20.
Hidrocystomas.
For the pediatric population, hemangiomas are the most common type of facial tumors. Almost all are detectable by the first month of life and will continue with rapid tumor development until the third or fourth month. From this point, a stable phase starts followed by involution that leaves varying degrees of sequels depending on the size, evolution, location, and treatment received if any. Periocular hemangiomas require treatment because the patient can present up to 73% of amblyopia (lazy eye) or refractive errors by the mass effect of the tumor (Gontijo, 2014). Ulceration is also a frequent complication and sometimes related to involution.
Capillary vascular tumors are less common in adults than in children. In adults, cavernous hemangiomas are the most common benign orbital tumor. This vascular malformation does not show spontaneous regression and has important differential diagnoses such as Kaposi sarcoma, low-grade angiosarcoma, Kaposiform hemangioendothelioma, and even pyogenic granuloma (Stagner and Jakobiec, 2016; Tambe et al., 2009).
Milia are millimetric keratinous cysts that can be classified as primary or secondary cysts (Fig. 21). The primary cysts occur spontaneously and the secondary ones are generally related to other pathologies such as pseudoxanthoma elasticum, discoid lupus erythematosus, lichen planus, trauma, and scars. They most commonly appear on the face; thus, the periocular region is involved. Although their etiology is not defined, they are believed to be derived from the infundibular portions of villous hair follicles. These cysts are asymptomatic and do not require treatment other than for cosmetic reasons (Terui et al., 2016). Seborrheic keratoses are extremely common in older adults and present as epidermal benign tumors that may mimic skin cancer. They are hyperpigmented from light brown to black, waxy, scaly, and with papular appearance and are most frequently seen on the trunk and the face. They can be solitary but habitually present as multiple lesions that measure 2 mm to 15 mm. The periocular area is frequently involved, and patients seek care for cosmetic reasons or to rule out malignant disease (Fig. 22).
Fig. 21.

Milia cysts.
Fig. 22.
Seborrheic keratosis.
Xanthelasma is a common skin disease that affects middle-aged women and clinically appears as symmetrical, soft, yellowish papules and plaques on the upper eyelid (62%) or both (38%) (Fig. 23). Although hormonal factors are involved, its pathogenesis is not fully understood, Despite the fact that it is mostly a cosmetic problem and the majority of patients present with normal lipid profiles, cholesterol-to-high-density lipoprotein ratios were significantly different between patients and controls. Therefore, xanthelasma may be considered a cutaneous sign for screening subclinical atherosclerosis (Kavoussi et al., 2016).
Fig. 23.
Xanthelasma.
Nevus of Ota is a congenital or acquired pigmentary disorder that affects the skin and mucous membranes innervated by the first and second branches of the trigeminal nerve, so periocular skin and sclera are common sites of involvement. Nevus of Ota is more common in female patients of Asian race, unilateral (95%), and has psychological and cosmetic consequences. Laser treatments are available with various degrees of success (Liu et al., 2016; Yang and Jiang, 2016).
Among the less frequent types of lesions are those of granuloma annulare, which are normally located on the trunk and the upper extremities. However, some cases have been identified as periocular lesions, which makes the diagnosis a challenge (Abalo-Lojo et al., 2008; DeBecker et al., 2010; Zloto et al., 2015).
Subepidermal calcified nodules have been described as appearing on the eyelids and are frequently misdiagnosed as warts, pilomatrixomas, molluscum contagiosum, or sebaceous cysts. The nodules are seen in male patients of preadolescent age, usually appear on the upper eyelid, and are generally asymptomatic. They are usually not related to any systemic disorder, although rheumatologic conditions must be ruled out (Shields et al., 2016).
Malignant tumors
In comparison with benign tumors, malignant ones are less frequent, affect primarily the lower eyelid, and are typically observed in the older population. Basal cell carcinoma (BCC), which is a non-melanoma form of skin cancer, is the most common malignant periocular tumor and is observed in 85% of cases (Belaid et al., 2016). In second place is squamous cell carcinoma (SCC). Both are more prevalent and aggressive in patients who are immunosuppressed, particularly in those patients with a solid organ transplant, which carries a 250-fold increased risk for SCC and 10-fold increased risk for BCC. This risk increases with UV exposure, a first episode of non-melanoma skin cancer, genetic variations, human papilloma virus or human herpes virus infection, and tobacco and alcohol use.
Malignant tumors require aggressive treatment and surveillance because these malignancies may cause globe exposure, nerve damage, vision loss, or even death and have important cosmetic complications (Perry et al., 2016). BCC is the most common form of skin cancer in Caucasians over the age of 50 years with a very high percentage of periocular malignancies (90%) distributed as follows: lower eyelid (43%), medial canthus (26%), upper eyelid (12%), and lateral canthus (8%; Fig. 24). The golden standard for diagnosis is by histopathologic testing although some new noninvasive methods are being evaluated such as optical coherence tomography (Pelosini et al., 2015).
Fig. 24.

Basal cell carcinoma.
The first treatment option is surgery, either conventional or with Mohs technique (Nikose et al., 2016). Alternate or adjunct therapies include intralesional bleomycin for the selected eyelid and periocular and orbital tumor with satisfactory results Meyer and Gooding, 2015. The rest of the malignancies have a much lower incidence, including SCC (Fig. 25). Periocular melanoma clinically presents as lentigo maligna melanoma in 85% of cases and 14% correspond to the superficial spreading type (Demirici et al., 2008).
Fig. 25.
Squamous cell carcinoma.
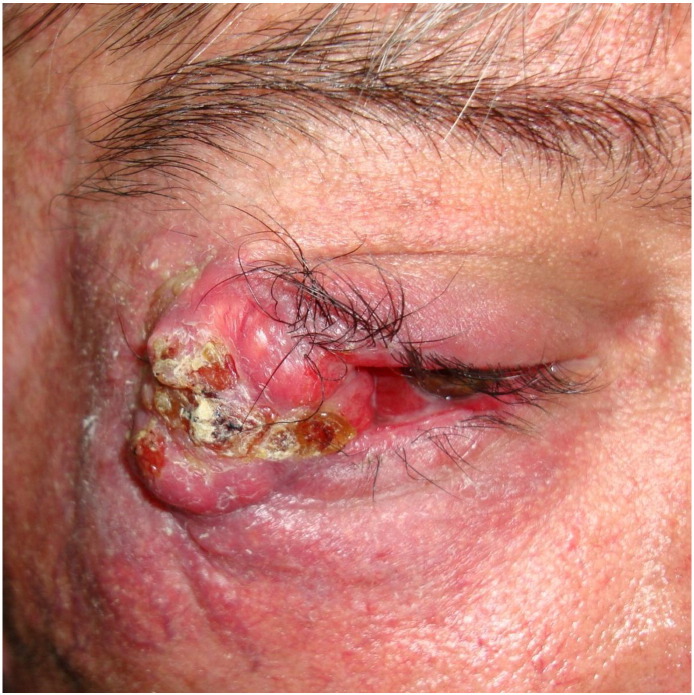
Eyelid metastases present in advanced disease and are not extremely common. In adults, eyelid metastases occur in less than 1% of malignant eyelid lesions. Up to 50% of cases are breast cancer-derived but also from cancer of the stomach, esophagus, lungs, and other organs. In 8% to 11% of cases, the primary cancer is from unknown origin (Goel et al., 2015). Orbit metastases are infrequent also but must always be considered as a differential diagnosis in any patient with cancer with visual alterations (Tabai et al., 2016). Sebaceous gland carcinomas (Fig. 26) are third in incidence after BCC and SCC. They are rare, slow-growing, skin adnexal tumors that are commonly periocular, which corresponds to less than 5% of ocular malignancies. Sebaceous gland carcinoma has its origin in the Meibomian glands, Zeis, or glands from the caruncle. The malignancy primarily affects the upper lids of elderly women and two forms have been described: nodular and spreading. Sebaceous gland carcinomas have a multifocal origin, present with local recurrence (30%), pagetoid spread and distant metastasis (41%), or are either lymphatic or hematogenous with a reported mortality of 6% to 11%.
Fig. 26.

Sebaceous gland carcinoma.
The diagnosis is usually delayed, particularly in diffuse cases where it may be confused with chronic blepharoconjunctivitis or other benign conditions. Treatment involves surgery with wide margins and with or without neck dissection and orbital exenteration. Radiotherapy is used as a palliative treatment. Poor prognostic factors involve the upper lid or both eyelids, a tumor > 10 mm, poorly differentiated or anaplastic tumors, metastasis, orbital extension, multicentricity, previous irradiation to the head and neck, and pagetoid spread. Tumors < 6 mm and an origin in the gland Zeis are more favorable (Dasgupta et al., 2009; Mahipathy et al., 2016).
Cutaneous T cell lymphomas (CTCLs) are non-Hodgkin lymphomas with skin involvement. Several subtypes have been described, and the most commonly encountered are mycosis fungoides (44%-62%; Fig. 27), Sézary syndrome, and primary cutaneous peripheral T cell lymphoma. Sometimes, the periocular area is involved (Bagherani and Smoller, 2016). B cell lymphomas can present as primary cutaneous malignancies and also as CTCLs because they are extranodal non-Hodgkin lymphomas. They account for 25% of these malignancies and have been classified by the World Health Organization and the European Organization for Research and Treatment of Cancer (2008) as primary cutaneous follicle-center lymphoma, primary cutaneous diffuse large cell lymphoma, leg type, and primary cutaneous marginal zone lymphoma. The malignancy affects white male adults who are over 50 years old more commonly (Wilcox, 2016).
Fig. 27.

Mycosis fungoides.
An even more unusual presentation is the Muir Torre syndrome, which is an autosomal dominant cancer syndrome that presents as sebaceous adenomas or carcinomas or multiple keratoacanthomas and visceral malignancies. Sebaceous neoplasms precede visceral malignant disease with 22% to 60% (Mintsoulis and Beecker, 2016).
Merkel cell tumor is a solitary, rare, primary malignancy that appears in sun-exposed areas. It is difficult to diagnose, recurrent (33% within the first year), and metastatic (66%) and can invade the bone, cartilage, and skeletal muscle. The main differential diagnosis is BCC, SCC, sweat gland carcinoma, metastatic bronchogenic oat cell carcinoma, lymphoma, leukemia, carcinoid tumor, neuroblastoma, and melanoma. Treatment is surgery with a 5-mm, tumor-free margin and radiotherapy in conjunction, most of the time with a sentinel lymph node biopsy. Distant metastases are more difficult to treat and respond only temporarily to chemotherapy, so it is mainly palliative. The first two years carry the highest risk for metastasis, and these may occur simultaneously with other lid carcinomas (Sniegowski et al., 2014; Thakur et al., 2008).
Trichilemmal carcinoma is another rare malignant adnexal tumor with origin in the external hair sheath. It presents on the face and other sun-exposed areas in hair-bearing areas of elderly patients and has no gender predilection. The clinical appearance is polymorphic, and the malignancy may include plaques, papules, nodules, ulcerated or crusts, can be unique or multiple, and show fast growth. It is commonly misdiagnosed as cutaneous horn, SCC, CBC, keratoacanthoma, or nodular melanoma. This tumor is locally invasive with high-grade mitotic activity. However, with surgery and a good margin, no adjuvant therapy is necessary, and only rare cases of recurrence or metastasis have been reported (Sajin et al., 2014). Cutaneous angiosarcoma is a highly malignant neoplasia that is derived from the endothelium that rarely presents in the periocular area. The tumor may appear flattened or present with nodular lesions, solitary or numerous, with an important surrounding edema and bluish-red to skin tones. It is frequently misdiagnosed as a benign lesion, but its rapid growth raises suspicion. Chronic lymphedema and radiotherapy are well-known risk factors for 10% of cases (Wiwatwongwana et al., 2010).
Among other extremely rare periocular malignancies, we find the primary mucinous carcinoma of the skin. The main differential diagnosis is metastasis of visceral adenocarcinoma, particularly from the breast; thus, it can be stained for estrogen and progesterone receptors and may appear histologically identical. Primary mucinous carcinoma has a low mortality rate but a high rate of local recurrence. Surgery is the best therapeutic approach even with recurrences (Burris et al., 2013). Pilomatrix carcinoma is rare and arises from the hair follicle matrix. It is more common in the head and neck region but rarely in the eyebrow or on the eyelid. It is frequently misdiagnosed as a sebaceous cyst but it is a low-rade malignant tumor with occasional distant metastasis that is mostly found in middle-aged men. There are approximately 80 cases reported in the literature (Pauly et al., 2014).
Traumatic lesions
Hematomas (Fig. 28) and edema are consequences of trauma, whether accidental or surgical, and both resolve within days. However, particularly with hematomas, patients should follow certain instructions to avoid further bleeding and complications. Such indications are to maintain normal and stable blood pressure, avoid Valsalva maneuvers, and keep the head upright most of the time (Klapper and Patrineloy, 2007).
Fig. 28.

Hematoma.
Scarring is the natural process for injury repair. In the periocular area, cosmetic procedures and other types of surgery are required frequently, and because it is an important, sun-exposed area, sun-related malignancies are commonly removed and repaired with the subsequent risk of ill scarring. Fortunately, the eyelids are not particularly affected by keloid or hypertrophic scar formation. The most common scarring complication is ectropion by skin contraction, which leaves the cornea exposed.
Cosmetic complications
Cosmetic applications for the eye area are used every day by many women worldwide. Conjunctival product migration has been widely studied and proven to occur after the application of products in the periocular area (Ng et al., 2015). This may be insignificant unless an allergy develops or a foreign body sensation causes discomfort.
However, some more serious cosmetic complications have been documented. For example, the everyday, more common practice of facial filler injections has some well-identified complications such as hypersensitivity reactions, infections, foreign body reaction, or—in more severe cases—ischemia and necrosis by intravascular embolization of permanent or semi-permanent fillers that may lead to very severe scarring and even visual loss if ocular irrigation is compromised (Sung et al., 2010). Some of these complications are not acute but sometimes present months or even years after infiltration so differential diagnoses such as neoplastic lesion are often worrisome (Nathoo et al., 2014).
The periocular skin is a frequent target for facial rejuvenation treatments. The most widely used lasers for this purpose are carbon dioxide and erbium:yttrium-aluminum-garnet. Recurring complications include sustained erythema, hypo-/hyperpigmentation, and scarring. Bacterial infections and herpes have also been reported (Blanco et al., 2007). Body dysmorphic syndrome can be focused on the periocular area with devastating cosmetic and psychological results because 81% of patients will be unsatisfied with the results. The main association with this disease is depression. In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, this disease is now classified as part of the obsessive compulsive and related disorders chapter. Physicians must be aware of this pathology to avoid overtreating these patients (McConnell et al., 2015).
Accidental burns affect the eyelids in 15% to 20% of cases; these can be mild or vision-threatening, so immediate evaluation and therapy are required (Pargament et al., 2015). Periocular scarring of any origin can lead to ectropion formation that causes corneal exposure and its consequent ulceration and loss of vision (Yesiloğlu et al., 2014).
Miscellaneous
Dark circles under the eye are a common complaint among patients. Despite its high prevalence, its physiopathology is still not fully understood. The most important factors are the increase of melanin deposition in the dermis, vasculature status, and the structural characteristics of each patient, which leaves aside the popular belief that lack of sleep worsens these cases (Fig. 29; Matsui et al., 2015).
Fig. 29.
Dark circles under the eye.
Although multifactorial, the main treatment options must be directed to the most probable cause of the malignancy. After cosmetic and cosmeceuticals, one must always try with the least invasive method such as intense pulsed light or superficial peelings (Vrcek et al., 2016). Permanent eyelid tattoos (Fig. 30) are frequent among middle-aged women with several advantages, such as a time saving when applying makeup and higher self-esteem. However, it is not a risk-free procedure, and the most common complications include fanning, fading, scarring, granulomatous reactions, contact dermatitis, and infections. Some are easy to correct, such as bacterial infections and fanning, but many others pose a serious challenge to the physician. Lasers are the first option to correct pigmentary defects and have variable results (Goldman and Wollina, 2014). Another lesser-known complication of eyelid tattooing is Meibomian gland dysfunction, which alters the tear film stability for several reasons. The first and most obvious is mechanical damage to the glands but also pigment toxicity, inflammation, and allergic reactions (Lee et al., 2015).
Fig. 30.
Cosmetic tattoo.
Footnotes
Conflicts of interest: The authors declare that they have no conflict of interest.
Funding sources: None.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijwd.2017.08.001.
Appendix A. Supplementary data
The following are the Supplementary data related this article.
Supplementary video
References
- Abalo-Lojo J.M., Cameselle-Teijeiro J., González F. Pilomatrixoma: Late onset in two periocular cases. Ophthal Plast Reconstr Surg. 2008;24:60–62. doi: 10.1097/IOP.0b013e318160681d. [DOI] [PubMed] [Google Scholar]
- Al-Faky Y.H., Al-Mosallam A.R., Al-Sohaibani M.O. Periocular hidradenoma papilliferum. Saudi J Ophthalmol. 2009;23:211–213. doi: 10.1016/j.sjopt.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aravindha Babu N., Rajesh E., Krupaa J., Gnananandar G. Genodermatoses. J Pharm Bioallied Sci. 2015;7:s203–6. doi: 10.4103/0975-7406.155903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asproudis I., Sotiropoulos G., Gartzios C.H., Raggos V., Papoudou-Bai A., Ntountas I. Eyelid tumors at the University Eye Clinic of Ioannina, Greece: A 30-year retrospective study. Middle East Afr J Ophthalmol. 2015;22:230–232. doi: 10.4103/0974-9233.151881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagherani N., Smoller B.R. An overview of cutaneous T cell lymphomas. F1000Res. 2016;28:5. doi: 10.12688/f1000research.8829.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandeira F., Roizenblatt M., Levi G.C., de Freitas D., Belfort R. Herpes zoster ophthalmicus and varicella zoster virus vasculopathy. Arq Bras Oftalmol. 2016;79:126–129. doi: 10.5935/0004-2749.20160038. [DOI] [PubMed] [Google Scholar]
- Belaid A., Nasr C., Benna M., Cherif A., Jmour O., Bouguila H. Radiation therapy for primary eyelid cancers in Tunisia. Asian Pac J Cancer Prev. 2016;17:3643–3646. [PubMed] [Google Scholar]
- Bhandage S., Kurki M., Hosur V., Sukhija P., Bajoria A. A little known relationship between immune recovery syndrome and herpes zoster. J Korean Assoc Oral Maxillofac Surg. 2016;42:169–172. doi: 10.5125/jkaoms.2016.42.3.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanc S., Bourrier T., Albertini M., Chiaverini C., Giovannini-Chami L. Dennie Morgan fold plus dark circles: Suspect atopy at first sight. J Pediatr. 2015;166:1541. doi: 10.1016/j.jpeds.2015.03.033. [DOI] [PubMed] [Google Scholar]
- Blanco G., Clavero A., Soparkar C.N., Patrinely J.R. Periocular laser complications. Semin Plast Surg. 2007;21:74–79. doi: 10.1055/s-2007-967752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burris C.K., Rajan K.D., Iliff N.T. Primary mucinous carcinoma of the periocular region: Successful management with local resections over 30 years. BMJ Case Rep. 2013 doi: 10.1136/bcr-2012-007972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlisle R.T., Digiovanni J. Differential diagnosis of the swollen red eyelid. Am Fam Physician. 2015;92:106–112. [PubMed] [Google Scholar]
- Dasgupta T., Wilson L.D., Yu J.B. A retrospective review of 1349 cases of sebaceous carcinoma. Cancer. 2009;115:158–165. doi: 10.1002/cncr.23952. [DOI] [PubMed] [Google Scholar]
- DeBecker I., Summers C.G., Kaye V., Traboulsi E.I., Schoenfield L., Markowitz G. Periocular granuloma annulare in four children. Am Assoc Pediatr Ophthalmol Strabismus. 2010;14:280–282. doi: 10.1016/j.jaapos.2010.02.004. [DOI] [PubMed] [Google Scholar]
- Demirici H., Johnson T.M., Frueh B.R., Musch D.C., Fullen D.R., Nelson C.C. Management of periocular cutaneous melanoma with a staged excision technique and permanent sections. The square procedure. Ophthalmology. 2008;115:2295–2300. doi: 10.1016/j.ophtha.2008.06.011. [DOI] [PubMed] [Google Scholar]
- Finger Basak S.A., Berk D.R., Lueder G.T., Bayliss S.J. Common features of periocular tinea. Arch Ophthalmol. 2011;129:306–309. doi: 10.1001/archophthalmol.2011.14. [DOI] [PubMed] [Google Scholar]
- Ganesan V., Bandyopadhyay D., Sankar Kar S., Choudhury C., Choudhary V. Herpes zoster infection involving mandibular division of trigeminal nerve and Ramsay Hunt syndrome with meningitis in an immunocompetent patient: A rare association. J Clin Diagn Res. 2016;10:5–7. doi: 10.7860/JCDR/2016/19862.7935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelaw Y., Asaminew T. Periocular cutaneous anthrax in Jimma Zone, Southwest Ethiopia: A case series. BMC Res Notes. 2013;6:313. doi: 10.1186/1756-0500-6-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghanadan A., Khosravi M. Cutaneous syringoma: A clinicopathologic study of 34 new cases and review of the literature. Indian J Dermatol. 2013;58:326. doi: 10.4103/0019-5154.113956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel S., Mittal D.K., Sharma P., Grover R.K. An unusual case of eyelid metastasis from a rectal primary. J Can Res Ther. 2015;11:1032. doi: 10.4103/0973-1482.147383. [DOI] [PubMed] [Google Scholar]
- Goldman A., Wollina U. Severe unexpected adverse effects after permanent eye makeup and their management by Q-switched Nd:YAG laser. Clin Invest Aging. 2014;9:1305–1309. doi: 10.2147/CIA.S67167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonnering R.S., Kronish J.W. Treatment of periorbital molluscum contagiosum by incision and curetaje. Ophthalmic Surg. 1988;19:325–327. [PubMed] [Google Scholar]
- Gontijo B. Complications of infantile hemangiomas. Clin Dermatol. 2014;32:471–476. doi: 10.1016/j.clindermatol.2014.02.002. [DOI] [PubMed] [Google Scholar]
- Gupta T., Beaconsfield M., Rose G.E., Verity D.H. Discoid lupus erythematosus of the periorbita: Clinical dilemmas, diagnostic delays. Eye. 2012;26:609–612. doi: 10.1038/eye.2011.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.C., Maher M.H., Douglas M.S. Diagnosing common benign skin tumors. Am Fam Physician. 2015;92:601–607. [PubMed] [Google Scholar]
- Hossain P., Konstantopoulos A. Blepharitis: Remains a diagnostic enigma. A role for tea tree oil shampoo? Eye. 2015;29:1520–1521. doi: 10.1038/eye.2015.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyengar S.S., Khan J.A., Brusco M., FitzSimmons C.J. Cutaneous Sporothrix schenckii of the human eyelid. Ophthal Plast Reconstr Surg. 2010;26:305–306. doi: 10.1097/IOP.0b013e3181c15c1f. [DOI] [PubMed] [Google Scholar]
- Jabbar A.S., Matinpour K., Orengo I., Rodríguez-Waitkus P.M., Diwan A.H., Motaparthi K. Eccrine hidrocystomas presenting as multiple papules on the cheeks. Dermatol Online J. 2013;19:19269. [PubMed] [Google Scholar]
- Jiang N., Zhao G., Yang S., Lin J., Hu L., Che C. A retrospective analysis of eleven cases of invasive rhino-orbito-cerebral mucormycosis presented with orbital apex syndrome initially. BMC Ophthalmol. 2016;16:10. doi: 10.1186/s12886-016-0189-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jurado F., Rodriguez O., Novales J., Navarrete G., Rodríguez M. Lucio’s leprosy: A clinical and therapeutic Challenger. Clin Dermatol. 2015;33:66–78. doi: 10.1016/j.clindermatol.2014.07.004. [DOI] [PubMed] [Google Scholar]
- Kamath S.J., Marthala H., Manapragada B. Ocular manifestations in lipoid proteinosis: A rare clinical entity. Indian J Ophthalmol. 2015;63:793–795. doi: 10.4103/0301-4738.171517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavoussi H., Rezaei M., Najafi B., Ebrahimi A., Ramezani M., Kavoussi R. Serum lipid profile and clinical characteristics of patients with xanthelasma palpebrarum. Ann Bras Dermatol. 2016;91:468–471. doi: 10.1590/abd1806-4841.20164607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klapper S.R., Patrineloy J.R. Management of cosmetic eyelid surgery complications. Semin Plast Surg. 2007;21:80–93. doi: 10.1055/s-2007-967753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosik-Bogacka D.I., Lanocha N., Lanocha A., Czepita D., Grobelny A., Zdziarska B. Demodex folliculorum and Demodex brevis in healthy and immunocompromised patients. Ophthalmic Epidemiol. 2013;20:159–163. doi: 10.3109/09286586.2013.789532. [DOI] [PubMed] [Google Scholar]
- Kumar S., Sengupta R.S., Kakkar N., Sharma A., Singh S., Varma S. Skin involvement in primary systemic amyloidosis. Mediterr J Hematol Infect Dis. 2013;5:e2013005. doi: 10.4084/MJHID.2013.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y.B., Kim J.J., Hyon J.H., Wee W.R., Shin Y.J. Eyelid tattooing induces Meibomian gland loss and tear firm instability. Cornea. 2015;34:750–755. doi: 10.1097/ICO.0000000000000452. [DOI] [PubMed] [Google Scholar]
- Lemmenmeier E., Gaus B., Schmid P., Hoffmann M. A case of erythrodermia from exacerbated psoriasis vulgaris due to treatment of acute hepatitis C. BMC Dermatol. 2016;16:5. doi: 10.1186/s12895-016-0042-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Zeng W., Geng S. A retrospective study on the characteristics of treating nevus of Ota by 1064-nm Q-switched neodymiun-doped yttrium aluminum garnet laser. Indian J Dermatol. 2016;61:347. doi: 10.4103/0019-5154.182470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahipathy S.R., Durairaj A.R., Kothandaraman K., Rajamanohar V.C., Prabakaran A. Sebaceous gland carcinoma of the lower eyelid reconstructed with a composite flap: A case report. J Clin Diagn Res. 2016;6:16–18. doi: 10.7860/JCDR/2016/20003.8017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin M., Harpaz R., Zhang J., Wollan P.C., Bialek S.R., Yawn B.P. Risk factor for herpes zoster among adults. Open Forum Infect Dis. 2016;3:119. doi: 10.1093/ofid/ofw119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsui M.S., Schalka S., Vanderover G., Fthenakis C.G., Christopher J., Bombarda P.C. Physiological and lifestyle factors contributing to risk and severity of peri-orbital dark circles in the Brazilian population. Ann Bras Dermatol. 2015;90:494–503. doi: 10.1590/abd1806-4841.20153520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnell L.K., Lee W.W., Black D.W., Shriver E.M. Beauty is in the eye of the beholder: Body dysmorphic disorder in ophthalmic plastic and reconstructive surgery. Ophthal Plast Reconstr Surg. 2015;31:e3–e6. doi: 10.1097/IOP.0000000000000019. [DOI] [PubMed] [Google Scholar]
- McElroy A.K., Hilinski J.A., Abramowsky C.R., Jaffe R., Park S.I., Shehata B.M. Bacillary angiomatosis in patients with cancer: A pediatric case and a review of the literature. J Pediatr Infect Dis Soc. 2013;2:175–178. doi: 10.1093/jpids/pis085. [DOI] [PubMed] [Google Scholar]
- Meyer D., Gooding C. Intralesional bleomycin as an adjunct theraopeutic modality in eyelid and extraocular malignancies and tumors. Middle East Afr J Ophthalmol. 2015;22:410–414. doi: 10.4103/0974-9233.167822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mintsoulis D., Beecker J. Muir-Torre syndrome. CMAJ. 2016;15:e95. doi: 10.1503/cmaj.150171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee B., Rajchura N.D., Alam M.S. Fungal infections of the orbit. Indian J Ophthalmol. 2016;64:337–345. doi: 10.4103/0301-4738.185588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray M.A., Zamecki K.J., Paskowski J., Lelli G.J., Jr. Ocular bacillary angiomatosis in an immunocompromised man. Ophthal Plast Reconstr Surg. 2010;26:371–372. doi: 10.1097/IOP.0b013e3181cff605. [DOI] [PubMed] [Google Scholar]
- Nathoo N.A., Rasmussen S., Dolman P.J., Rossman D.W. Periocular mass lesions secondary to dermatologic fillers: Report of 3 cases. Can J Ophthalmol. 2014;49:468–472. doi: 10.1016/j.jcjo.2014.07.004. [DOI] [PubMed] [Google Scholar]
- Neimkin M.G., Holds J.B. Evaluation of eyelid function and aesthetics. Facial Plast Surg Clin N Am. 2016;24:97–106. doi: 10.1016/j.fsc.2015.12.002. [DOI] [PubMed] [Google Scholar]
- Ng A., Evans K., North R.V., Purslow C.H. Migration of cosmetic products into the tear film. Eye Contact Lens. 2015;41:304–309. doi: 10.1097/ICL.0000000000000124. [DOI] [PubMed] [Google Scholar]
- Nikose A.S., Laddha P.M., Bisen R.R. Periocular basal cell carcinoma in a young school teacher. Int J Appl Basic Med Res. 2016;6:143–145. doi: 10.4103/2229-516X.179021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oguz H., Kilic A. Eyelid infection. Ophthalmology. 2006;113:1891.e1–1891.e3. doi: 10.1016/j.ophtha.2006.02.011. [DOI] [PubMed] [Google Scholar]
- Ohsie L.H., Murchison A.P., Wojno T.H. Lupus erythematosus profundus masquerading as idiopathic orbital inflammatory syndrome. Orbit. 2012;31:3,181–3. doi: 10.3109/01676830.2011.648813. [DOI] [PubMed] [Google Scholar]
- Pargament J.M., Armenia J., Nerad J.A. Physical and chemical injuries to eyes and eyelids. Clin Dermatol. 2015;33:234–237. doi: 10.1016/j.clindermatol.2014.10.015. [DOI] [PubMed] [Google Scholar]
- Pauly M., Subramanian K., Anantharaman G., Anthony E. Pilomatrix carcinoma of the eyebrow. Ophthal Plast Reconstr Surg. 2014;31:e9–10. doi: 10.1097/IOP.0000000000000021. [DOI] [PubMed] [Google Scholar]
- Pelosini L., Smith H.B., Schofield J.B., Meeckings A., Dithal A., Khandwala M. A novel imaging approach to periocular basal cell carcinoma: in vivo optical coherence tomography and histological correlates. Eye. 2015;29:1092–1098. doi: 10.1038/eye.2015.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry J.D., Polito S.C., Chundury R.V., Singh A.D., Fritz M.A., Vidimos A.T. Periocular skin cancer in solid organ transplant recipients. Opthalmology. 2016;123:203–208. doi: 10.1016/j.ophtha.2015.09.030. [DOI] [PubMed] [Google Scholar]
- Qureshi F., Dharmasena A., Leatherbarrow B. Periocular scleromyxedema. Ophthal Plast Reconstr Surg. 2015;31:e119–20. doi: 10.1097/IOP.0000000000000144. [DOI] [PubMed] [Google Scholar]
- Rambhatla P.V., Brescoll J., Hwang F., Juzych M., Lim H.W. Photosensitive disorders of the skin with ocular involvement. Clin Dermatol. 2015;33:238–246. doi: 10.1016/j.clindermatol.2014.10.016. [DOI] [PubMed] [Google Scholar]
- Rath S., Sharma S., Mophatra S., Roy A., Vemuganti G.K., Balne P. Mixed Nocardia cyriacigeorgica and Staphylococcus aureus infection in the periocular skin and orbit in an immunocompetent adult. Orbit. 2012;31:428–430. doi: 10.3109/01676830.2012.694556. [DOI] [PubMed] [Google Scholar]
- Rener-Prmec Z., Balkovec V. Valproate-related erythrodermia with reversible encephalopathy: A rare but serious adverse reaction, case report. Acta Dermatovenererol Alp Pannonica Adriat. 2014;23:35–38. doi: 10.15570/actaapa.2014.9. [DOI] [PubMed] [Google Scholar]
- Rojo-España R., Tomas-Mallebrera L., Gimeno-Clemente N., Marquina-Vila A., Morales-Suárez Varela M. Epidemiological study of periocular dermatitis in a specialized hospital department. Iran J Allergy Asthma Immunol. 2011;10:195–205. [PubMed] [Google Scholar]
- Romaña C. La conjuntivitis schizotripanosómica unilateral (hipótesis sobre la puerta de entrada conjuntival de la enfermedad) Vol. 22. 1935. Acerca de un síntoma inicial de valor para el diagnóstico de la forma aguda de la enfermedad de Chagas; pp. 16–25. (Mision de Estudios de Patologia Regional Argentina (MEPRA)). (in Portugese) [Google Scholar]
- Saeed H.N., Chodosh J. Ocular manifestations of Stevens-Johnson syndrome and their management. Ophthalmology. 2016;27:1–8. doi: 10.1097/ICU.0000000000000312. [DOI] [PubMed] [Google Scholar]
- Sajin M., Luchian M.C., Hodorogea A.P., Dumitru A., Patrascu O.M., Costache D. Trichilemmal carcinoma - rare cutaneous malignancy: Report of two cases. Romanian J Morphol Embryol. 2014;55:687–691. [PubMed] [Google Scholar]
- Sánchez-Borges M., Asero R., Ansotegui I.J., Baiardini I., Bernstein J.A., Canonica G.W. Diagnosis and treatment of urticarial and angioedema: A worldwide perspective. WAO J. 2012;5:125–147. doi: 10.1097/WOX.0b013e3182758d6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sand J.P., Zhu B.Z., Desai S.C. Surgical anatomy of the eyelids. Facial Plast Surg Clin N Am. 2016;24:89–95. doi: 10.1016/j.fsc.2015.12.001. [DOI] [PubMed] [Google Scholar]
- Shields C.L., Marous M.R., Casey M.G., Douglass A.M., Khoo C.T., Bilyk J.R. Ophthalmology. 2016;123:671–672. doi: 10.1016/j.ophtha.2015.10.015. [DOI] [PubMed] [Google Scholar]
- Sniegowski M.C., Warneke C.L., Morrison W.H., Nasser Q.J., Frank S.J., Pfeiffer M.L. Correlation of American Joint Committee on cancer T category for eyelid carcinoma with outcomes in patients with periocular Merkel cell carcinoma. Ophthal Plast Reconstr Surg. 2014;30:480–485. doi: 10.1097/IOP.0000000000000153. [DOI] [PubMed] [Google Scholar]
- Souza Leite R.M., Craveiro Leite A.A. Two therapeutic challenges: Periocular and genital vitiligo in children successfully treated with pimecrolimus cream. Int J Dermatol. 2007;46:986–989. doi: 10.1111/j.1365-4632.2007.03282.x. [DOI] [PubMed] [Google Scholar]
- Speeckaert R., van Geel N. Distribution patterns in generalized vitiligo. J Eur Acad Dermatol Venereol. 2014;28:755–762. doi: 10.1111/jdv.12171. [DOI] [PubMed] [Google Scholar]
- Stagner A.M., Jakobiec F.A. A critical analysis of eleven periocular lobular capillary hemangiomas in adults. Am J Ophthalmol. 2016;165:164–173. doi: 10.1016/j.ajo.2016.03.010. [DOI] [PubMed] [Google Scholar]
- Sung M.S., Kim H.G., Woo K.I., Kim Y.D. Ocular ischemia and ischemic oculomotor nerve palsy after vascular embolization of injectable calcium hydroxylapatite filler. Ophthal Plast Reconstr Surg. 2010;26:289–291. doi: 10.1097/IOP.0b013e3181bd4341. [DOI] [PubMed] [Google Scholar]
- Tabai M., Hazboun I.M., Sakuma E.T., Sampaio M.H., Sakano E. Orbital metastasis of breast cancer mimicking invasive fungal rhinosinusitis. Case Rep Otolaryngol. 2016;2016:2913241. doi: 10.1155/2016/2913241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tambe K., Munshi V., Dewsbery C., Ainsworth J.R., Willshaw H., Parulekar M.V. Relationship of infantile periocular hemangioma depth to growth and regression pattern. J AAPOS. 2009;13:567–570. doi: 10.1016/j.jaapos.2009.09.014. [DOI] [PubMed] [Google Scholar]
- Tambe K., Tripathi A., Burns J., Sampath R. Multidisciplinary management of periocular necrotizing fasciitis: A series of 11 patients. Eye. 2012;26:463–467. doi: 10.1038/eye.2011.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenorio-Abreu A., Sánchez-España J.C., Naranjo-González L.E., González-Gallego M.C., Hidalgo-Grass C., Ruíz-Frutos C. Development of a PCR for the detection and quantification of parasitism by Demodex folliculorum infestation in biopsies of skin neoplasms periocular area. Rev Esp Quimioter. 2016;29:220–223. [PubMed] [Google Scholar]
- Terui H., Hashimoto A., Yamasaki K., Aiba S. Milia en plaque as a distinct folicular hamartoma with cystic trichoepitheliomatous features. Am J Dermatopathol. 2016;38:212–217. doi: 10.1097/DAD.0000000000000445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakur S., Chalioulias K., Hayes M., While A. Bilateral primary Merkel cell carcinoma of the upper lid misdiagnosed as basal cell carcinoma. Orbit. 2008;27:139–141. doi: 10.1080/01676830701556715. [DOI] [PubMed] [Google Scholar]
- Troyanov Y., Targoff I.N., Payette M.P., Raynauld J.P., Chartier S., Goulet J.R. Redefining dermatomyositis. A description of new diagnostic criteria that differentiate pure dermatomyositis form overlap myositis with dermatomyositis features. Medicine. 2014;93:318–332. doi: 10.1097/MD.0000000000000222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vij A., Bergfeld W.F. Madarosis, milphosis, eyelash trichomegaly, and dermatochalasis. Clin Dermatol. 2015;33:217–226. doi: 10.1016/j.clindermatol.2014.10.013. [DOI] [PubMed] [Google Scholar]
- Vrcek I., Ozgur O., Nakra T. Infraorbital dark circles: A review of the pathogenesis, evaluation and treatment. J Cutan Aesthet Surg. 2016;9:65–72. doi: 10.4103/0974-2077.184046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox R.A. Cutaneous B-cell lymphomas: 2016 update on diagnosis, risk stratification, and management. Am J Hematol. 2016;91:1052–1055. doi: 10.1002/ajh.24462. [DOI] [PubMed] [Google Scholar]
- Wiwatwongwana D., White V.A., Dolman P.J. Two cases of periocular cutaneous angiosarcoma. Ophthal Plast Reconstr Surg. 2010;5:365–366. doi: 10.1097/IOP.0b013e3181c0e180. [DOI] [PubMed] [Google Scholar]
- Wu M.A., Perego F., Zanichelli A., Cicardi M. Angioedema phenotypes: disease expression and classification. Clin Rev Allergy Immunol. 2016;51:162–169. doi: 10.1007/s12016-016-8541-z. [DOI] [PubMed] [Google Scholar]
- Yang T., Jiang X. Three cases of symmetrical nevus of Ota. Int J Dermatol. 2016;55:e404–e406. doi: 10.1111/ijd.13087. [DOI] [PubMed] [Google Scholar]
- Yesiloğlu N., Sirinoğlu H., Sarici M., Temiz G., Güvercin E. A simple method for the treatment of cicatricial ectropion and eyelid contraction in patients with periocular burn: Vertical V-Y advancement of the eyelid. Burns. 2014;40:1820–1821. doi: 10.1016/j.burns.2014.08.024. [DOI] [PubMed] [Google Scholar]
- Yun S.H., Levin F., Servat J. Demodex folliculitis presenting as periocular vesiculopustular rash. Orbit. 2013;32:370–371. doi: 10.3109/01676830.2013.812124. [DOI] [PubMed] [Google Scholar]
- Zloto O., Fabian I.D., Vishnevskia V., Simon G.J.B., Rosner M. Periocular pilomatrixoma: A retrospective analysis of 16 cases. Ophthal Plast Reconstr Surg. 2015;31:19–22. doi: 10.1097/IOP.0000000000000164. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary video