Abstract
Introduction
Palliative radiotherapy is effective in reducing symptom burden and improving quality of life in patients with symptomatic metastatic cancer and should be delivered in a timely manner. The aim of this study was to determine whether referring patients directly to a Palliative Advanced Practice Radiation Therapist (APRT) improves access to palliative radiotherapy and reduces time from referral to treatment.
Methods
At Radiation Oncology Mater Center (ROMC) in Brisbane, Australia a new referral pathway was developed which involved patients requiring palliative radiotherapy, being referred directly to the APRT from a single external hospital medical oncology and palliative care departments. Over a 5 months period, patient demographics and time in working days from referral to treatment were compared for consecutive palliative patients seen within our department. Patients were stratified by method of referral i.e. via the new referral pathway (NP) or via standard referral pathway (SP).
Results
Between October 2014 and March 2015, a total of 150 patients were referred for palliative radiotherapy. Of these patients, 48 were referred and processed via the NP. There was a significant reduction in the number of days from referral to treatment for patients referred through the NP. Patients referred through the NP via the APRT had a mean and median wait time of 3.5 and 3 days respectively compared with 8.1 and 5 days for patients referred through the SP (P = <0.001). Patients were also more likely to have the treatment completed with less visits to the hospital (P < 0.001).
Conclusions
The new referral pathway utilising a dedicated palliative APRT decreased waiting times for patients receiving palliative radiotherapy and improved timely access to the radiotherapy service for both referrers and patients.
Keywords: Advanced practice, quality improvement, radiation therapist, referral, waiting lists
Introduction
Radiotherapy plays a significant role in the palliation of symptoms in patients with cancer1, 2 and has been proven to be both cost effective and well tolerated.2, 3 Waiting for palliative radiotherapy may cause distress, unnecessary symptom burden, and under certain circumstances compromise survival outcomes for patients with metastatic cancer. Long waiting lists and difficult access may discourage patients and referrers from utilising palliative radiotherapy.4 Anxiety caused by the financial burden associated with travel to and from appointments and fatigue caused by long delays associated with ambulance transport5 can be reduced by minimising the number of visits to the hospital between referral and the patients first radiotherapy treatment.
Advanced practice in palliative radiation therapy is an established concept in the UK and Canada but is still finding its way in Australia.6, 7, 8 A framework for the scope of practice of advanced practice for radiation therapy and a pathway to achieve accreditation in Australia was developed by the Australian Institute of Radiography (AIR) now Australian Society of Medical Imaging and Radiation Therapy (ASMIRT) in 2014. With this framework in mind, the fact that 35% of patients in the department were treated with palliative intent and that there was an established rapid response palliative clinic (RRPC) in the department, a palliative APRT role was developed in 2013 at ROMC Brisbane, Australia. One of the aims of developing this position was to expedite and individualise the treatment and follow up for palliative patients seen outside of the RRPC. The role has continued to develop over the 4 years since inception and the APRT's responsibilities have expanded as the role has evolved.
Multidisciplinary RRPC have shown to expedite patient's palliative radiotherapy both nationally and internationally.2, 9, 10 An assessment of the established RRPC at ROMC in 2005, showed patients referred to the RRPC waited less time to receive palliative radiotherapy compared with patients seen outside the RRPC.2 Although the RRPC at ROMC was running successfully 1 day a week with the APRT as part of the multidisciplinary team, the majority of palliative patients were still referred through the department's standard pathway and seen in individual consultant non‐rapid response clinics. It was not felt feasible to extend the RRPC so an alternative solution was sought to improve the waiting times for palliative patients referred to the department.
To facilitate reducing the time from referral to treatment, a new referral pathway was proposed whereby external hospital palliative referrals from the medical oncology and palliative care departments, where possible, would be made directly to the APRT.
The aim of this study was to determine whether, by establishing a new referral pathway where consultants referred palliative patients directly to a palliative APRT, it would reduce time from referral to treatment and improve access to palliative radiotherapy for patients.
Establishment of APRT referral pathway
As a significant proportion of ROMC palliative radiotherapy referrals came from a single external hospital's medical oncology and palliative care department which is in close proximity geographically to ROMC, we introduced the concept for the new referral pathway at a weekly multidisciplinary meeting at the external hospital. This meeting was attended by the palliative APRT, medical oncologists, palliative care consultants, palliative and medical oncology registrars and palliative nursing staff. Laminated promotional flyers clearly labelled with the APRT contact phone number were put up in all the external hospital's palliative care and medical oncology clinic rooms and on the oncology ward.
Referral pathways
The standard referral pathway (SP) (Fig. 1) involved any referral that was either faxed or phoned to any of the department's Radiation Oncologists (RO) via the administration staff. This referral pathway typically involved handovers between administration staff, ROs and a radiation therapist coordinator.
Figure 1.
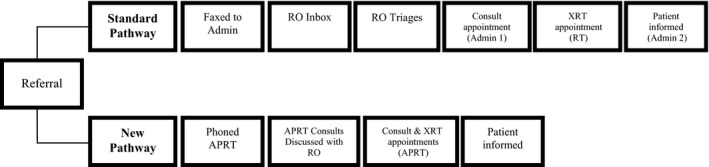
Flow chart of referral pathways. Admin, administration; APRT, advanced practice radiation therapist; RO, radiation oncologist; RT, radiation therapist; Consult, consultation; XRT, radiation therapy.
The new referral pathway (NP) (Fig. 1) involved palliative patients referred directly to the APRT via a phone call, then a paper referral by consultants or registrars from the one external hospital medical oncology and palliative care departments. The following information was requested at point of referral: the patient's site of disease, symptoms, recent imaging and current chemotherapy. Where possible on the day of referral, the APRT would review the patient in the referrer's outpatient clinic or on the ward to further assess prior radiation treatment details, patient symptoms, performance status and social situation. Alternatively, the APRT assessed the patient by phone. For patients new to the department the APRT triaged them to an appropriate RO according to primary site of disease and availability of the RO. Returning patients were allocated to the previous treating RO providing this was not going to delay the patient's treatment. Following a discussion with the RO regarding the patients imaging, history and current condition, consult, planning and treatment appointments were coordinated by the APRT and where possible the patient was seen by the RO and planned on the day of referral.
Referral to the NP was totally at the discretion of the referrer. As this was a new service some consultants used the service regularly while others used the standard pathway as it was familiar. On occasions, the referrer felt it was required to discuss a patient directly with a consultant or a registrar, so these patients were processed through the SP. Palliative patients referred and seen by the departments ROs in offsite clinics at other community hospitals were processed through the SP as they had been referred directly to the RO.
Material and Methods
Prospective evaluation of new referral pathway
Ethics approval for this project was obtained through Princess Alexandra Hospital Metro South Hospital and Health Services. (HREC/13/QPAH/713).
Over a 5‐month period, 150 consecutive palliative patients having 10 fractions or less were seen at ROMC. All patients had their planning using CT scans which were imported into the 3D volume based planning system. Treatment fields were delineated on digital reconstructed radiographs.
The time from referral date until the commencement of their first radiotherapy treatment was recorded in working days. This data was then separated into time from referral to consult, time from referral to planning and time from referral to treatment for each individual patient. The following data was also collected for all patients in both pathways: age, gender, primary histological diagnosis, site/s of disease treated, the number of visits made to the department between referral and first radiotherapy treatment, referral pathway and priority status. Priority status 1 included patients with spinal cord compression, bronchial obstruction with lobar collapse, superior vena cava obstruction or major haemorrhage. Priority 2 status included all other patients (Table 1). Departmental policy dictates that all priority 1 patients are planned and treated on the same day and all priority 2 patients, whose treatment is planned using treatment fields delineated on digital reconstructed radiographs, are offered the next available treatment appointment from planning, workload permitting.
Table 1.
Demographics, disease characteristics, site of treatment and priority of patients
| Characteristic | New pathway | Standard pathway |
|---|---|---|
| N = 48 | N = 102 | |
| Gender–no. (%) | ||
| Male | 22 (46) | 56 (56) |
| Female | 26 (54) | 46 (46) |
| Age–year no. (%) | ||
| Median (range) | 66 (37–91) | 66 (33–94) |
| ≤55 | 6 (12) | 20 (20) |
| 55–75 | 33 (69) | 56 (55) |
| ≥75 | 9 (19) | 26 (25) |
| Primary diagnosis–no. (%) | ||
| Bladder | 2 (4) | 3 (3) |
| Prostate | 8 (17) | 25 (25) |
| Colorectal | 2 (4) | 2 (2) |
| Lung | 13 (27) | 30 (29) |
| Breast | 18 (38) | 16 (16) |
| Gynae | 2 (4) | 6 (6) |
| Renal | 1 (2) | 6 (6) |
| Other | 2 (4) | 14 (15) |
| Site of treatment–no. (%) | ||
| Brain | 5 (10) | 14 (14) |
| Spine | 13 (27) | 28 (26) |
| Chest | 10 (21) | 17 (17) |
| Limb | 6 (13) | 21 (21) |
| Pelvis/Abdomen | 14 (29) | 22 (22) |
| Priority–% | ||
| 1 emergency | 14.5 | 6 |
| 2 non‐emergency | 85.5 | 94 |
Guidelines from the Royal Australian and New Zealand College of Radiologists (RANZCR) states that the standard of good practice for palliative radiotherapy is that non‐urgent treatment should commence between 2 and 14 working days from the time of referral.11 With this in mind we compared the percentage of patients in both groups that were treated within 2 days of referral and those that waited longer than 14 days to receive treatment.
Statistical analysis
Comparisons of time from referral to consult, referral to planning and referral to treatment were analysed with a Wilcoxon rank sum test using R version 3.1.3 statistical software. A median (±Inter Quartile range) and mean (±SD) have been reported. The relationship between the RANZCR guidelines (between 2 and 14 days) and the different pathways was performed using a Fisher's exact test. The relationship between number of visits and the different pathways was performed using a chi‐square test.
Results
Between October 2014 and March 2015, the target enrolment of 150 consecutive palliative patients receiving 10 fractions or less was achieved. Of the 150 palliative patients, 48 were referred directly to the APRT and processed through the NP. The remainder were referred through the department's SP. Patient demographics for all patients are represented in Table 1. There were a greater percentage of patients referred through the NP with a breast cancer primary. More priority 1 patients were referred through the NP. There were a greater number of patients with a prostate primary and other primary referred through the SP.
There was a statistically significant reduction in the number of days from referral to planning and from referral to treatment for patients referred through the NP (Table 2). Patients referred through the NP via the APRT had a mean and median wait time of 1.6 and 1 days from referral to planning respectively compared to 5.3 and 3 days for patients referred through the SP (P = <0.001). Mean and median wait time from referral to treatment for patients through the NP were 3.5 and 3 days respectively compared with 8.1 and 5 days for patients referred through the SP (P = <0.001).
Table 2.
Time interval in working days for all patients
| New pathway | Standard pathway | P | |||
|---|---|---|---|---|---|
| n = 48 | n = 102 | ||||
| Median (Range) | Mean (±SD) | Median (Range) | Mean (±SD) | ||
| Referral to Consult | 1 (0–5) | 1.4 (±1.3) | 1 (0–29) | 3.2 (±4.8) | 0.065 |
| Referral to Planning | 1 (0–9) | 1.6 (±1.7) | 3 (0–29) | 5.3 (±6.0) | <0.001 |
| Referral to Treatment | 3 (0–13) | 3.5 (±2.5) | 5 (1–31) | 8.1 (±7.1) | <0.001 |
When priority 1 patients were excluded from the analysis the differences seen in times between referral to planning and referral to treatment between the two groups remained statistically significant (Table 3). Patients referred through the NP via the APRT had a mean and median wait time 1.7 and 1 day from referral to planning respectively compared with 5.5 and 3 days for patients referred through the SP (P = <0.001). Mean and median wait time from referral to treatment for patients through the NP were 3.9 and 4 days respectively compared with 8.4 and 6 days for patients referred through the SP (P = <0.001).
Table 3.
Time interval in working days for priority 2 patients
| New pathway | Standard pathway | P | |||
|---|---|---|---|---|---|
| n = 41 | n = 96 | ||||
| Median (Range) | Mean (±SD) | Median (Range) | Mean (±SD) | ||
| Referral to consult | 1 (0–5) | 1.4 (±1.4) | 1 (0–29) | 3.2 (±4.9) | 0.097 |
| Referral to planning | 1 (0–5) | 1.7 (±1.8) | 3 (0–29) | 5.5 (±6.4) | <0.001 |
| Referral to treatment | 4 (1–13) | 3.9 (±2.5) | 6 (1–31) | 8.4 (±7.2) | <0.001 |
Through the NP, 39% of patients were treated within 2 days of referral compared with 17% of patients referred through the SP. No patients referred through the NP waited more than 14 days from referral to treatment with 93% of patients treated within 6 days of referral. Through the SP, 61% of patients were treated within 6 days of referral with 20% waited longer than 14 days to receive radiotherapy. There is a statistically significant relationship (P < 0.001) between the pathway and the independent time categories. (Table 4)
Table 4.
Time from referral to treatment: No (%) of patients
| <2 days | 2–6 days | 6–14 days | >14 days | |
|---|---|---|---|---|
| New pathway | 18 (39) | 25 (54) | 3 (7) | 0 (0) |
| Standard pathway | 17 (17) | 46 (44) | 19 (19) | 20 (20) |
Of patients referred through the NP, 31% were consulted, planned and treated on the same day compared with 9% of patients referred through the SP and 33% planned and treated on the same day compared with 15% for patients referred through the SP.
When analysed for number of visits, patients referred through the NP made fewer visits to the department for their consult, planning and first treatment appointments than those patients referred through the SP. This comparison was found to be statistically significant (P < 0.001) (Table 5).
Table 5.
Number of visits: No (%) of patients
| 1 | 2 | 3 | |
|---|---|---|---|
| New pathway | 15 (31) | 30 (63) | 3 (6) |
| Standard pathway | 7 (7) | 44 (43) | 51 (50) |
Discussion
Palliative radiation treatment plays an important role in the management of patients with metastatic and locally advanced disease. The aim should always be to deliver palliative radiotherapy in a timely fashion, minimising delays from referral to treatment delivery. In some cases delays in receiving treatment can impact survival.4 Increased anxiety in patients by any delay in treatment from referral can occur and should be minimised if possible.12 In our department, in 2005, a dedicated RRPC was successfully established to improve waiting times for palliative patients.2 However, this clinic was staffed by one radiation oncologist, one day per week and so the majority of palliative patients were still being managed outside of this dedicated palliative clinic. The aim of establishing a palliative APRT role was to improve waiting times for patients seen outside of the RRPC. It was predicted that having the APRT as a single point of contact for palliative referrers from the one external hospital medical oncology and palliative care departments, where a significant proportion of the department's palliative referrals come from, it would streamline the process and minimise treatment delays. Our results have shown that this new referral process has been successful in optimising the time from referral to palliative radiotherapy delivery.
There were a larger number of patients with a breast cancer primary referred through the NP potentially due to the referring medical oncology department having a large breast cancer practice. Discrepancies in other disease primaries between the two pathways cannot be explained.
There were a greater proportion of priority 1 patients referred to the APRT. This may have biased the referral to treatment times but, as shown in the results, when the priority 1 patients were taken out of the mix statistical significance remained. It could be anticipated that referrers, seeing their priority 2 patients in need of more urgent treatment, might contact the APRT assuming they would be fast tracked. As mentioned earlier all priority 2 patients whose treatment is planned using treatment fields delineated on digital reconstructed radiographs are offered the next available treatment appointment from planning. The APRT and all Radiation Oncologists had equal access to the booking of consult, planning and treatment appointments.
There were a variety of unavoidable external factors identified for a minority of patients in the NP and the SP that delayed time from referral to treatment. Examples of delays included department waiting lists, waiting on restaging results, chemotherapy schedules, patient request, cardiac assessments and treatments becoming more complex due to previous radiotherapy. Through the SP 4.7% of patients referred had their treatment delayed due to an unavoidable external factor compared to 6.3% of patients referred through the NP. Two patients from both groups had their planning to treatment time affected by department waiting lists.
In an assessment of the RRPC at ROMC in 2005 it was shown that patients referred through the clinic had a reduced waiting time to receive palliative radiotherapy compared with patients seen outside the RRPC.2 An overall improvement in the time it takes for a patient to receive palliative radiotherapy from referral has been shown in the NP in this study, compared with the patients processed through the RRPC in 2005. When comparing the mean number of days from referral to consultation for patients referred through the NP to those from the RRPC data published in 2005, a decrease was seen (1.38 vs. 3). However, waiting times from consult to treatment were equivalent.
In this study, patients referred through the SP had improved overall waiting times compared to those patients seen via the same pathway in the non‐RRPC in 2005. Although referral to consult mean time interval was similar between these two data groups, consult to treatment times showed an improvement with the number of patients waiting >5 days at 55.6% non‐RRPC (2005) versus 30% SP (current study) which suggests that having a RRPC established for 10 years in our department has influenced the other clinicians in the department into treating palliative patients more promptly.2
Non‐emergency patients referred through the NP and those seen in the RRPC in 2005 were given the option of having their treatment on the same day as their planning appointment. An explanation was given to the patients that this could involve a wait of up to 4 h in the department. Thirty three per cent of the patients through the NP elected to be planned and treated on the same day compared with 74% of patients seen in the RRPC. It is noteworthy that 30% of the NP patients had a medical oncology and or a palliative care appointment on the same day they were referred and consulted and planned for radiotherapy. As they had already spent a considerable amount of time in the hospital, the burden of waiting to receive treatment was greater than returning on another day to receive their first fraction.
The standard of good practice for palliative treatments as set by the RANZCR 11 was met by 100% of patients referred through the NP compared to 80% of patients referred to the RRPC in 2005.
The results from our study of the new APRT referral pathway compare favourably with rapid response clinics internationally. A New Zealand rapid access palliative clinic (RAPC) assessed wait times for 261 patients with metastatic bone pain.13 All patients in the RAPC were seen within a week of referral. This compares with 96% of patients referred through the NP in this study seen within 3 days with the remaining 4% seen within 5 days. In the New Zealand RAPC 63% of patients were planned and treated on the same day compared with 33% in the current studies NP. Consult to first treatment was quicker for patients through the NP in this study compared with patients from the RAPC with 98% treated within 10 days for NP versus 36% for RAPC.
For over 10 years similar clinics in Canada have shown consistent improvement in wait times for palliative patients to receive radiotherapy. Between 2008 and 2012 the Rapid Response Radiotherapy Program at the Odette Cancer Centre evaluated wait times from referral to consultation for 2742 patients.14 Although the number of patients in the study was dramatically larger, the percentages of various sites treated were comparable with patients in this study. Once again there was a reduction in the mean number of days from referral to consult in patients referred through the NP compared to the Canadian clinic (1.38 vs. 3). The wait times from consult to treatment were similar with 96% of patients through the NP being treated within 7 days compared to 93% in the Canadian clinic.
Understandably the results from this study are from a single centre, a single APRT and one point of external referral and perhaps do not provide a robust conclusion on the benefits of the APRT but at the time this paper was written the APRT was the only RT to be accredited as an advanced practitioner in palliative radiotherapy in Australia. The APRT role in palliative radiotherapy at ROMC is unique nationally, although there are RTs working within multidisciplinary RRPC in Australia. With the development of advanced practice in radiation therapy in Australia and New Zealand, this new referral pathway model may prove to be a concept to be considered in departments where a rapid response clinic is not available or viable which may provide opportunities to collect more robust data to consolidate the benefits of an APRT in palliative radiotherapy. This study is also part of a larger project in which we evaluate the APRT role in our department with regards to wait times to receive radiotherapy, ability of the APRT to define palliative treatment fields and patient satisfaction. The results of the larger study are being prepared for publication.
It is important to consider a replacement when the APRT is not available i.e. planned and unplanned leave. This has been addressed by educating a small group of radiation therapists to step into the role for planned absences of greater than 5 days with support from ROs and registrars. For short absences the on call registrar accesses the APRT phone so referrals can be received and rapid treatment facilitated.
In this study only a third of patients during the timeframe of the study were referred through the new referral pathway. This was due to a number of factors including the fact that our centre treats a significant number of private patients and these referrals tend to be from consultant to consultant. These patients would be referred directly to the RO therefore be processed through the SP. For this study the new referral pathway was only introduced to the one external hospital medical oncology and palliative care departments to pilot the NP which also limited patient numbers referred through the NP. As it showed a reduction in the time it takes for palliative patients to receive radiotherapy from referral, the NP has been introduced to other external palliative care facilities and public health networks to provide ‘fast track’ radiotherapy for palliative patients. The departments ROs visiting other community hospitals with offsite clinics processed their palliative patients through the SP as these patients also would be referred directly to the RO. The plan for the future is for radiation oncologists in the department to utilise the APRT to fast track these offsite referrals. Although these factors affected the number of referrals received by the APRT in this study and the fact that there will always be situations where consultant to consultant referral is preferred and appropriate, it is felt with education of the benefits of the NP to more external referrers the number of patients referred directly to the APRT will increase.
Conclusion
National and international literature shows a decrease in waiting times for patients to receive palliative radiotherapy when referred to dedicated Rapid Response Palliative clinics.2, 15, 16 However, these clinics do not exist in the majority of Australian and New Zealand radiation centres. In this study utilising a dedicated palliative APRT to manage palliative patients has shown to be comparable to, and in some cases better than, established national and international rapid response palliative clinics in terms of reducing waiting times from referral to treatment. It has also reduced the number of visits patients receiving palliative radiotherapy are required to make in order to receive treatment.
Further evaluation of the palliative APRT role and the impact the role has on planning room workflow, reducing the workload of radiation oncologists and patient and referrer satisfaction is required to justify the cost of the role to the department and these aspects will form the basis of further research and publications.
Conflict of Interest
The authors declare no conflict of interest.
J Med Radiat Sci 64 (2017) 274–280
References
- 1. Bedard G. Handbook of Bone Metastases For Healthcare Professionals, 2nd edn. Odette Cancer Centre, Sunnybrook Health Sciences Centre, Toronto, 2014. [Google Scholar]
- 2. Holt TR, Yau VKY. Innovative program for palliative radiotherapy in Australia. J Med Imaging Radiat Oncol 2009; 54: 76–81. [DOI] [PubMed] [Google Scholar]
- 3. Janjan N. Palliative radiation therapy: Utilization of advanced technologies Fairchild AM. (ed). Vol 1, Nova Science Publishers, New York, 2015. [Google Scholar]
- 4. Nieder C, Spanne O, Haukland E, Dalhaug A. Does time between imaging diagnosis and initiation of radiotherapy impact survival after whole‐brain radiotherapy for brain metastases? ISRN Oncol 2013; 2013: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hubbard G, Maguire R, Kidd L, Kearney N, Hilliam A. Patient views of transport for cancer treatment. Eur J Oncol Nurs 2006; 10: 391–5. [DOI] [PubMed] [Google Scholar]
- 6. Bolderston A. Advanced practice perspectives in radiation therapy. J Radiother Pract 2004; 4: 57–65. [Google Scholar]
- 7. Ford P. The role of the consultant radiographer – Experience of appointees. Radiography 2010; 16: 189–97. [Google Scholar]
- 8. Forsyth LJ, Maehle V. Consultant radiographers: Profile of the first generation. Radiography 2010; 16: 279–85. [Google Scholar]
- 9. Fairchild A, Pituskin E, Rose B, et al. The rapid access palliative radiotherapy program: Blueprint for initiation of a one‐stop multidisciplinary bone metastases clinic. Support Care Cancer 2009; 17: 163–70. [DOI] [PubMed] [Google Scholar]
- 10. Chow E, Wong R, Connolly R, Hruby G, Franssen E, et al. Prospective assessment of symptom palliation for patients attending a rapid response radiotherapy program: Feasibility of telephone follow‐up. J Pain Symptom Manage 2001; 22: 649–56. [DOI] [PubMed] [Google Scholar]
- 11. Committee TT . Tripartite Radiation Oncology Practice Standards – The Royal Australian and New Zealand College of Radiologists 2011. Available from: http://www.ranzcr.edu.au/quality-a-safety/radiation-oncology/tripartite-radiation-oncology-practice-standards.
- 12. Robinson D, Massey T, Davies E, Jack RH, Sehgal A, Møller H. Waiting times for radiotherapy: Variation over time and between cancer networks in southeast England. Br J Cancer 2005; 92: 1201–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Casson C, Johnson J. Implementation and evaluation of a rapid access palliative clinic in a New Zealand cancer centre. J Med Radiat Sci 2014; 61: 217–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Thavarajah N, Wong K, Zhang L, et al. Continued success in providing timely palliative radiation therapy at the Rapid Response Radiotherapy Program: A review of 2008–2012. Curr Oncol 2013; 20: e206–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. De Sa E, Sinclair E, Mitera G, et al. Continued success of the rapid response radiotherapy program: A review of 2004–2008. Support Care Cancer 2009; 17: 757–62. [DOI] [PubMed] [Google Scholar]
- 16. Danjoux C, Chow E, Drossos A, et al. An innovative rapid response radiotherapy program to reduce waiting time for palliative radiotherapy. Support Care Cancer 2006; 14: 38–43. [DOI] [PubMed] [Google Scholar]


