Abstract
Background:
Dilated cardiomyopathy (DCM) is revealed with the left ventricular dilatation and systolic dysfunction.
Objective:
This study was performed to determine the level of calcitonin gene-related peptide (CGRP) and brain natriuretic peptide (BNP) in children with DCM and controls and comparison of these two biomarkers in patients.
Materials and Methods:
This study was performed from April 2014 to March 2015 on patients with DCM. The levels of BNP and CGRP were measured by ELISA, and final amounts of biomarkers were compared with the echocardiographic finding.
Results:
In this study, the mean age was 10.567 ± 5.50 and 12.135 ± 4.626 years for controls and cases, respectively (P = 0.321). The majority of echocardiographic indices in the left and right heart had different means in cases and controls (P < 0.05). Means of BNP were 213.814 ± 309.601 and 2.76 ± 1.013 for case and control, respectively (P < 0.001). Means of CGRP were 2.278 ± 1.586 and 1.488 ± 0.501 for cases and controls, respectively, (P = 0.001). In the patients group, however, no significant relationship was observed between CGRP level and Ross classification but observed a direct relationship of Ross classification with BNP (χ2 = 15.845, P < 0.05).
Conclusions:
The present research was performed on DCM patients and showed that most echocardiographic parameters, mean of CGRP and mean of BNP increased in patients compared to healthy children. The severity of illness based on the Ross classification showed significant and positive correlation with BNP level but not with CGRP. Probably, it could be concluded that BNP would be a better biomarker in DCM patients.
Key words: Brain natriuretic peptide, calcitonin gene-related peptide, children, dilated cardiomyopathy
INTRODUCTION
Dilated cardiomyopathy (DCM) is identified with systolic dysfunction and dilatation of left ventricle that may cause ventricular arrhythmia, atrioventricular block, syncope, and finally sudden death. Yearly incidence is 0.57 per 100 000 with the distribution of 0.66 and 0.47 for males and females in children. This term is ranged from 4 to 40 in infants that are much higher than in children.1 Calcitonin gene-related peptide (CGRP) neurotransmitter peptide 37 is an amino acid that extracted from calcitonin gene and commonly increases in nervous and cardiovascular systems. A positive inotropic and chronotropic effect of calcitonin has been observed on the heart, and it is the strongest endogen vasodilator peptide that has been known so far.2 Inconsistent results reported about CGRP levels in congestive heart failure (CHF) with low information regarding regulation of CGRP function.3,4,5 Cardiac sensory nerves play a defensive role in the heart through the expulsion of CGRP and nitric oxide. CGRP plays a protective role in myocardial injuries, including ischemia recirculation and cardiotoxic agent doxorubicin. CGRP in addition of having great power in vasodilator, it also has beneficial effects on the heart by local downregulation of tumor necrosis factor-alpha and upregulation of insulin-like growth factor.6 Brain-type natriuretic peptide (BNP) is a natriuretic hormone secreted from the cardiac ventricular myocytes in response to an increase in ventricular wall stretch and filling pressures. Natriuretic peptides are useful markers in a variety of cardiac diseases in children and adolescents.7 These peptides may be useful for screening of asymptomatic high-risk patients such as aged persons, hypertensive, diabetics, and coronary artery disease.8 The cutoff point of BNP in children is higher than adults and is a reliable test for diagnosis of functional and structural disorders of the cardiovascular system.9 These peptides are used to diagnose the CHF and may have advantages in screening of asymptomatic high-risk patients. BNP is a reliable test for diagnosis of functional and structural disorders of coronary heart disease (CHD).10 It resulted that CGRP constituted potential therapeutic for the treatment of cardiomyopathy on diabetic rats in long-term.11 Moreover, it pointed that CGRP measures are related to the overload pulmonary volume in children with CHD, and it can be a cause of CHF and increases with severity.3 The most common cause of CHF is CHD with pulmonary volume overload in infants and children. It also plays an important role in CHF pathogenesis secondary to CHD. Pulmonary volume overload may have a strong role in the regulation of CGRP in children with CHF.3,5 In CHF patients, it has been concluded that an increase in BNP level is associated with blood volume increase. Therefore, high secretion of BNP is due to pulmonary hypertension and cyanosis. BNP levels are increased in most types of CHD with both volume and pressure overload of left or right ventricle.12 Accordance with a variety in DCM studies and this fact that most of them are about the role of BNP and CGRP in the diagnosis, we decided to perform a study with the aim of using BNP and CGRP to diagnose DCM in children to specify the diagnostic value of these two biomarkers with comparison of control group.
MATERIALS AND METHODS
This study was performed on 37 DCM patients from February 2014 for1 year. Thirty healthy children were matched in age and weight with patients. Hemoglobin <10 g/dl, endocrine, metabolic, valvular disorders, dysrhythmia, and heart block were exclusion criteria. For the control participants, if echocardiography diagnosed any type of heart diseases, they were excluded from the study and replaced with new one based on conditions. Participants aged from 1 to 18 years. Children over 2 years measured weight using RASA mark made in Iran by an error of 100 g, and for children under 2 years, MIKA mark recumbent weighting scale made in Japan with error of 10 g was applied. Height of patients was measured in the recumbent position using a calibrated and flat wooden table while that of the children above 2 years old was measured in the standing position with a scale ruler. Heart failure stratification was performed by modified Ross classification. Patients were normal in respect to Na, K, Ca, blood urea nitrogen, and creatinine. Three milliliters of blood was drawn from the patients in fasting at 8 am. Samples were centrifuged at 5°C with a round of 3000 g for 10 min. The separated serum was kept in −80°C refrigerator. The levels of BNP and CGRP were measured by ELISA kits. Echocardiography findings were measured by MyLab 60 made in Italy. Data analysis was performed by SPSS 20.0 (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.) using test of normality at first with Kolmogorov–Smirnov. In the case of normality, independent t-test and one-way ANOVA were used, otherwise same nonparametric tests applied. For the relationship between variables, Pearson correlation was used. In all tests, the significant level considered <0.05.
RESULTS
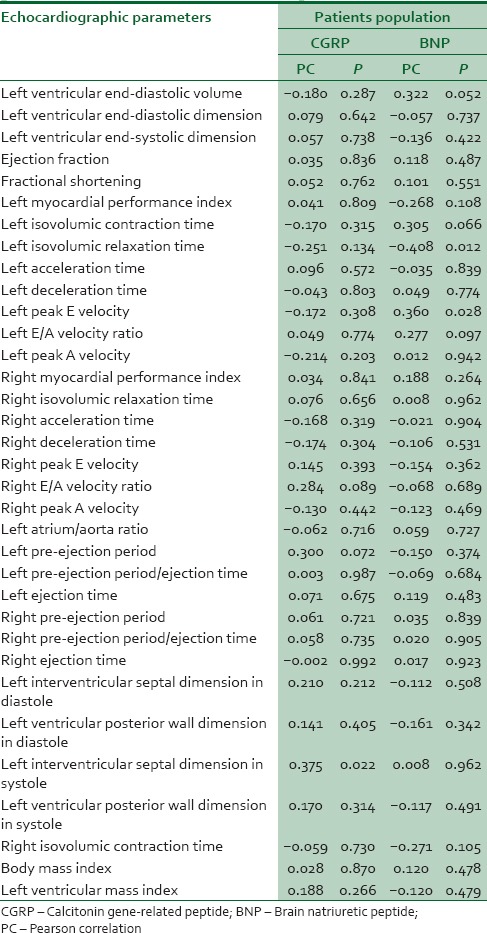
In this study, 67 children were recruited in case (37) and control (30). The age range was from 1 to 18 years. The mean age was 11.933 ± 7.625 and 13.568 ± 6.517 years for control and case, respectively, in which t-test results nonsignificant difference (t = 0.946, P = 0.348). The mean weight was 35.133 ± 18.471 and 28.7 02 ± 10.553 kg in control and case groups, respectively (t = −1.79, P = 0.078). The mean height was 128.700 ± 29.200 and 127.405 ± 18.712 cm in control and case groups, respectively (t = −0.22, P = 0.827). Since the sample size is larger than 50, we use the Kolmogorov–Smirnov normality test for variables in the study. The null hypothesis for the test of normality stated that the actual distribution of the variable is equal to the expected distribution, i.e. the variable is normally distributed. Since the probability associated with the test of normality for all variables except weight, left ventricular end-diastolic volume (LVEDV), fractional shortening (FS), left peak E velocity, body mass index, and right isovolumic contraction time (ICT) is less than or equal to the level of significance (0.05), we reject the null hypothesis and conclude that these variables are normally distributed. Therefore, for these variables, all applied tests would be parametric. Table 1 shows the results of independent t-test to compare the means of normal distributed echocardiographic parameters of left and right heart in case and control groups. The results showed that mean LVEDV for case and control groups was 66.108 ± 22.129 and 39.279 ± 14.782 with significant level in different (t = −5.687, P < 0.001) and same trends for means of case and control for left peak E velocity with 85.974 ± 17.759 and 101.558 ± 19.648, respectively (t = −3.406, P = 0.001). An examination of the findings in Tables 2 and 3 shows that the results of the nonparametric Mann–Whitney U-test applied to the variables in left and right in the case and control groups revealed a statistically significant difference at the level in some of them. The rank average of the left ventricular end-diastolic dimension (LVEDD) of the case group was 42.568, while the participants in the control group had an LVEDD score rank average of 23.433 with the P < 0.001, which shows statistically significant different [Table 4]. The mean ranks of the right E/A velocity ratio were 33.216 and 34.967 in the case and control groups, respectively, with the P = 0.714, in which not enough power to reject equality of mean ranks [Table 5]. Note that the test statistic is corrected for the existence of ties in the ranks of the BNP (χ2 = 15.845, P < 0.05) and CGRP (χ2 = 297, P < 0.05) data; there exists enough evidence to result that there is a difference in the Mann–Whitney test scores. Table 4 shows Ross classification impact on BNP and CGRP in patients. CGRP with mean ranks of 20.95, 20.56, 18.25, and 15.75 for severity of classes 1, 2, 3, and 4 in the order given shows no significant relationship with Ross classification. However, according to Table 4, BNP shows that influenced by the level of disease's severity significantly (χ2 = 15.8453 and P = 0.001). Table 5 shows that with BNP increasing, CGRP decreases but not significantly in bout patients and all population. LVEDV has appositive and significant correlation (r = 0.447, P < 0.001) with BNP in the case of considering all population but not with CGRP. It is observed that there is no significant correlation in the case of patients, except a few parameters. In patients, it is observed that just interventricular septal dimension in systole (IVSDS) has a correlation with CGRP. At the end of the analysis, from 10 patients in Group 1, two patients died due to disease progression. All nine participants in the second groups survived until the end of follow-up. In Group 3, one patient died and one had heart transplantation (from 10 patients). And finally, for the fourth group, from eight patients, two received heart transplantation, one with three chambers peacemaker (died), and two individuals withdraw the study.
Table 1.
Echocardiographic parameters of the left and right heart
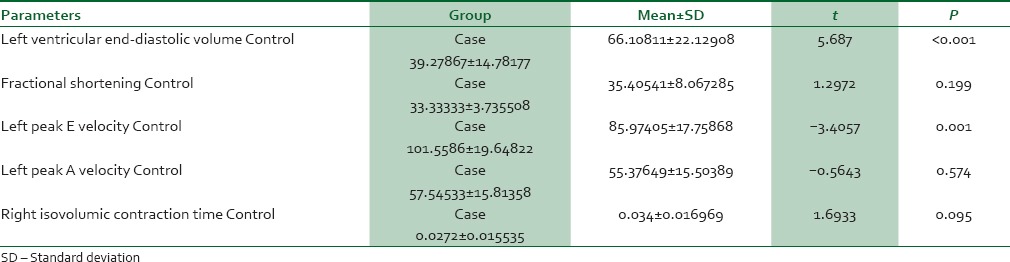
Table 2.
Results of the Mann-Whitney U-test to compare the groups’ values of the left heart parameters
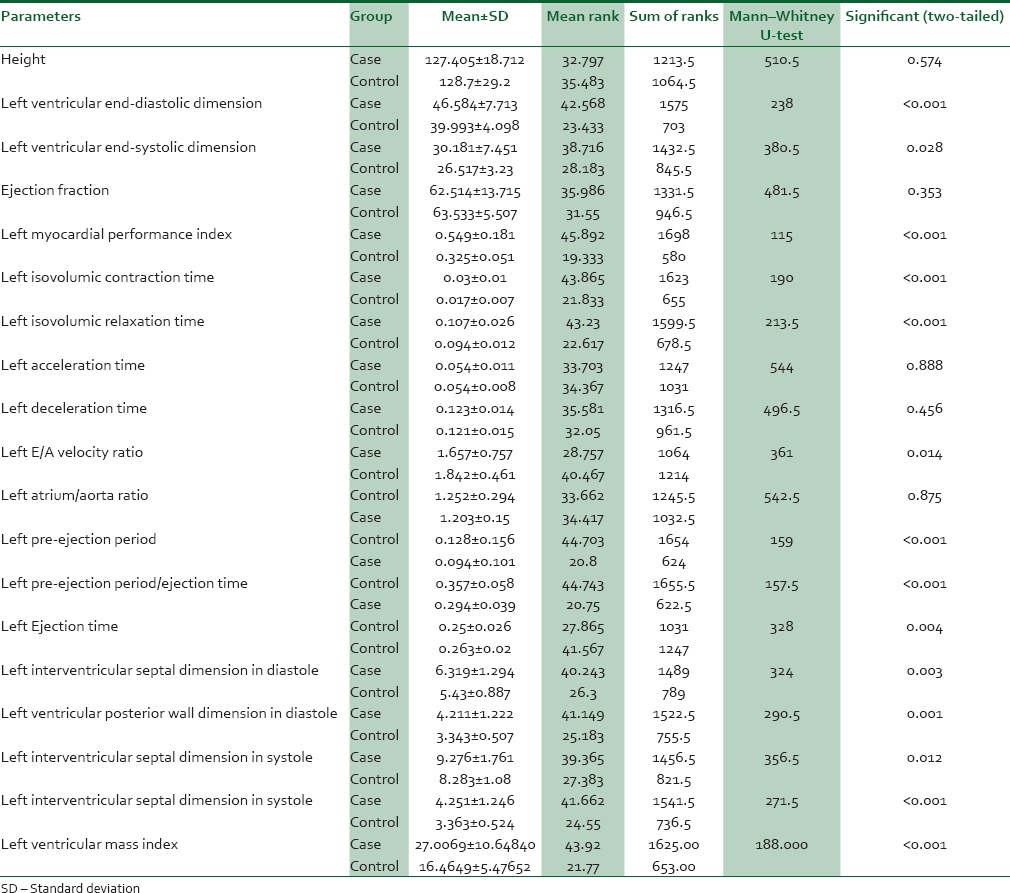
Table 3.
Results of the Mann-Whitney U-test to compare the groups’ values of right heart parameters and biomarkers
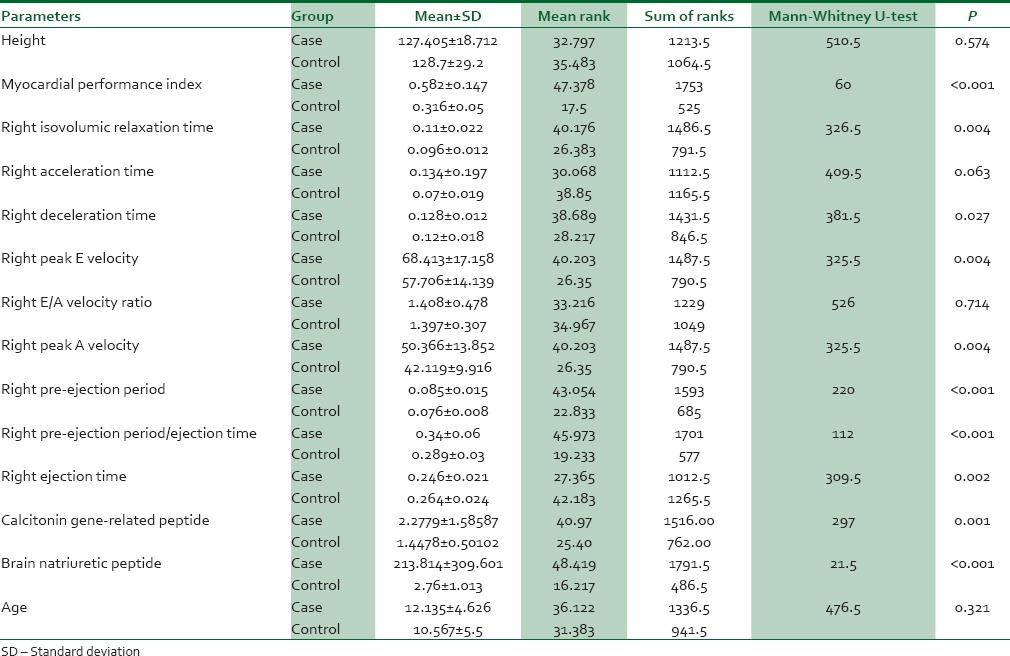
Table 4.
Ross classification impact on age and biomarkers in patients
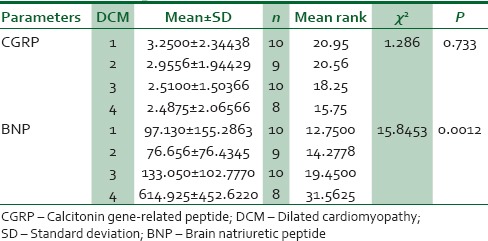
Table 5.
Correlation of echocardiographic parameters and biomarkers in patients
DISCUSSION
The current study provided that LVEDD, left ventricular end-systolic dimension (LVESD), ICT, LVEDV, myocardial performance index (MPI), ICT, IRT, IVSDS, peak E velocity, pre-ejection period/ejection time (PEP/ET), ET, interventricular septal dimension in diastole, left ventricular posterior wall dimension in diastole (LVPWDD), and left ventricular posterior wall dimension in systole (LVPWDS) in the left heart and MPI, IRT, deceleration time (DT), E, A (peak A velocity), PEP/ET, PEP, and ET in the right heart were significantly different between two case and control groups. The results showed that CGRP level and BNP were higher among patients, but it was very stronger significant in BNP. Increased BNP may approve the presence of DCM due to diastolic dysfunction and probably systolic dysfunction as well but without differentiation power between systolic and diastolic types. Noori in a study concluded a significant difference in the levels of IRT, DT, PEP, ET, PEP/ET, and MPI of the right heart between case and control groups. For the other echocardiography parameters such as ICT, E, A, and E/A, nonsignificant difference was observed, which is similar with the present findings in all echocardiography parameters, except peak E velocity and peak A velocity in the left heart. In our study, we resulted that the findings comparatively is similar with the Noori's outcomes.13 In the years 2012 and 2013, Noori carried out studies on the cardiac and pulmonary dysfunction in asymptomatic beta-thalassemia major patients. In the study, the right and left side heart functions compared in patients with thalassemia major, patients with thalassemia intermedia, and control groups resulted that MPI in both right and left heart was significantly higher in patients than controls, which was similar with our finding in this specific situation. PEP/ET ratio was different in case and controls significantly with similar outcome of the present study. Ejection fraction, in both studies, showed a significant difference that was similar with the present study. For acceleration time in left and right heart, there was not reported a significant difference. Mean of ICT as a parameter of left heart was different in case and control comparison significantly which was similar with our findings. Isovolumic relaxation time (IRT) was significantly different in both studies. In the present study, we received to the conclusion of a significant difference in both left and right heart. DT had significant difference in two case and control groups in Noori studies that agree with right heart. In brief, these two studies by Noori show similar patterns with the results of the present study.14,15 Left ventricular mass index (LVMI) as a left heart parameter had significant different values in case and control groups.16,15 The results of the late studies were similar with the present study findings. Noori reported that echocardiographic parameters of left ventricle such as ICT, MPI, ET, PEP/ET, DT, AT, IRT, LVEDD, LVESD, and EF in patients and control groups were significantly different. However, in the present study, the results were a little dissimilar. It means that for all the mentioned parameters, we found same results except DT, AT, and EF. Echocardiographic parameters of right ventricle such as MPI (higher in patient), peak A velocity (higher in patient), PEP (higher in patient), and ET (higher in case) in patients were statistically different compared with controls, which was similar with our findings. However, for the E/A (higher in case) parameter, we found disagreement with the Noori study which was not significantly different in case and controls.17 Jefferies and Towbin reported that DCM is characterized with left ventricular dilatation and is accompanied with systolic dysfunction. However, diastolic dysfunction may also be seen and both ventricles may develop insufficiency, and also there is mortality risk due to ventricular arrhythmia, atrioventricular block, syncope, and sudden death.1 In our patients, we received to the conclusion that BNP had strong relationship with three of echocardiographic parameters and severity of illness, which was consisted with Jefferies' results. NT-pro-BNP could be introduced for continuous left ventricle dysfunction in children with cardiomyopathy or myocarditis. However, the normal level in improved children may not demonstrate any residual heart disease.9 This result was similar to our findings comparatively when we used BNP instead of NT-pro-BNP. Consequently, to diagnose the heart failure, BNP has been approved by FDA. Similarly, we found an association between BNP and MPI that showed systolic and diastolic dysfunction.18 Koch et al. demonstrated that in children with congenital heart disease, the plasma level of BNP was associated with ventricular function and reflects the ventricular overload injury. Hence, the normal BNP may show compensatory phase.19 Our results were similar with Koch when we assessed children with DCM. In both studies, the major problem was due to volume overload. Mariano-Goulart et al. reported that an increase in BNP level in patients with systolic ventricular dysfunction would be considered as a risk factor for right ventricular dysfunction.20 According to our finding, the BNP level was higher in high severity level of disease based on Ross classification. Kremastinos et al. said in their report “plasma level of BNP and NT-Pro-BNP is increased in major thalassemia patients and when left ventricular dysfunction is developing the predictive value of NT-pro-BNP would be better than BNP for diagnosis of latent left ventricular diastolic dysfunction.” Moreover, in the related study by Kremastinos et al., they were also proposed that NT-pro-BNP was increasing by age.21,22 In our study, a significant difference in mean age and BNP level was observed in the various severity of disease such that in higher severity, the mean age and the mean BNP were higher. Niedner found a relationship between BNP and severity of congenital heart disease;23 however, in our study, we resulted that increasing of BNP was correlated with severity of DCM. The results of various studies on CGRP have reported that CGRP infusion had meaningful positive clinical impacts on patients with heart failure during multiple mechanisms. These results proposed that heart failure would be treated by CGRP. The findings of the present study showed a significant positive correlation between CGRP and left ventricular dilatation dysfunction (LVDD), LVESD, LVPWDD, and LVPWDS, which was comparable with the results of the study conducted by Jianping in animal model.24 Marangoni et al. conducted an animal model study on rats and resulted that FS, E/A, IVRT, LVDD, left ventricular systolic dysfunction (LVSD), intraventricular septum in diastole (IVSD), intraventricular septum in systole (IVSS), and DT were higher in the cases compared with controls. In the current study, similar results were obtained regarding IVDD, IVSD, LVSD, IVSS, and IVRT while the two groups were not significantly different in respect to FS, E/A, IVRT, and DT.25 Hsu JH expressed that CGRP level was related to pulmonary artery systolic pressure. Hsu et al. reported an association between CGRP and heart failure due to CHD and pulmonary artery pressure. Hsu et al. also pointed CGRP was related to the severity of the disease.3 A study was carried out on CHD patients who had left to right shunt by Zhang et al. The research was different with ours in terms of cardiomyopathy improvement. They measured CGRP and endothelin plasma levels in CHD patients with pulmonary hypertension. They resulted that the level of CGRP increased in patients with pulmonary hypertension. These results were comparable with our findings for showing higher CGRP levels in the patients with DCM.26 Xin et al. studied the relationship between right heart echocardiographic findings and CGRP in major thalassemia patients and reported that CGRP was inversely correlated with right ventricle MPI and pulmonary hypertension; however, in another study resulted that there were no correlations between CGRP and pulmonary hypertension in CHD patients.27,28 Nonetheless, the current study results showed significant positive correlations in both left and right hearts. Besides, no significant relationship was found between CGRP and MPI in the case group, and there was a direct correlation between IVSS and CGRP level in the left heart.
CONCLUSIONS
The present research was performed on DCM patients and showed that the majority echocardiographic parameters, mean of CGRP and mean of BNP increased in patients compared to healthy children. The severity of illness based on the Ross classification showed significant and positive correlation with BNP level but not with CGRP. Probably could be concluded that BNP would be a better biomarker in DCM patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to show their warm gratitude to all parents for the participation, especially control groups. The authors also thank nursing staff from hospitals for data gathering.
REFERENCES
- 1.Jefferies JL, Towbin JA. Dilated cardiomyopathy. Lancet. 2010;375:752–62. doi: 10.1016/S0140-6736(09)62023-7. [DOI] [PubMed] [Google Scholar]
- 2.Noori N, Shahramian I, Mahjoobifar M, Teymoori A, Shahraki Z. Comparison of calcitonin gene related peptide level between children with dilated cardiomyopathy and control group. Int Cardiovasc Res J. 2015;9:100–5. [Google Scholar]
- 3.Hsu JH, Yeh JL, Dai ZK, Chen IJ, Wu JR. Increased circulating calcitonin gene-related peptide in congestive heart failure caused by congenital heart disease. Int Heart J. 2005;46:867–75. doi: 10.1536/ihj.46.867. [DOI] [PubMed] [Google Scholar]
- 4.Spinarova L, Vitovec J. Neurohumoral changes in chronic heart failure. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2007;151:201–7. doi: 10.5507/bp.2007.035. [DOI] [PubMed] [Google Scholar]
- 5.Hasbak P, Saetrum Opgaard O, Eskesen K, Schifter S, Arendrup H, Longmore J, et al. Investigation of CGRP receptors and peptide pharmacology in human coronary arteries. Characterization with a nonpeptide antagonist. J Pharmacol Exp Ther. 2003;304:326–33. doi: 10.1124/jpet.102.037754. [DOI] [PubMed] [Google Scholar]
- 6.Boerma M, Hauer-Jensen M. Preclinical research into basic mechanisms of radiation-induced heart disease. Cardiol Res Pract 2010. 2011:pii: 858262. doi: 10.4061/2011/858262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lechner E, Wiesinger-Eidenberger G, Wagner O, Weissensteiner M, Schreier-Lechner E, Leibetseder D, et al. Amino terminal pro B-type natriuretic peptide levels are elevated in the cord blood of neonates with congenital heart defect. Pediatr Res. 2009;66:466–9. doi: 10.1203/PDR.0b013e3181b3aee4. [DOI] [PubMed] [Google Scholar]
- 8.Braunwald E. Biomarkers in heart failure. N Engl J Med. 2008;358:2148–59. doi: 10.1056/NEJMra0800239. [DOI] [PubMed] [Google Scholar]
- 9.Law YM, Hoyer AW, Reller MD, Silberbach M. Accuracy of plasma B-type natriuretic peptide to diagnose significant cardiovascular disease in children: The better not pout children! study. J Am Coll Cardiol. 2009;54:1467–75. doi: 10.1016/j.jacc.2009.06.020. [DOI] [PubMed] [Google Scholar]
- 10.Noori NM, Mahjoubifard M, Shahramian I, Teimouri A, Jahangirifard A. Comparison between procalcitonin, brain natriuretic peptide, and uric acid in children with cardiomyopathy and controls. Biomed Res Int. 2015;2015:510450. doi: 10.1155/2015/510450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dvorakova MC, Kruzliak P, Rabkin SW. Role of neuropeptides in cardiomyopathies. Peptides. 2014;61:1–6. doi: 10.1016/j.peptides.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Trojnarska O, Gwizdala A, Katarzynski S, Katarzynska A, Szyszka A, Lanocha M, et al. Evaluation of exercise capacity with cardiopulmonary exercise test and B-type natriuretic peptide in adults with congenital heart disease. Cardiol J. 2009;16:133–41. [PubMed] [Google Scholar]
- 13.Noori NM, Rajaei S. Serum uric acid correlation with echocardiographic indices in children with dilated cardiomyopathy. J Tehran Univ Heart Cent. 2009;4:230–3. [Google Scholar]
- 14.Noori NM, Keshavarz K, Shahriar M. Cardiac and pulmonary dysfunction in asymptomatic beta-thalassanemia major. Asian Cardiovasc Thorac Ann. 2012;20:555–9. doi: 10.1177/0218492312439706. [DOI] [PubMed] [Google Scholar]
- 15.Noori N, Mohamadi M, Keshavarz K, Alavi SM, Mahjoubifard M, Mirmesdagh Y. Comparison of right and left side heart functions in patients with thalassemia major, patients with thalassemia intermedia, and control group. J Tehran Univ Heart Cent. 2013;8:35–41. [PMC free article] [PubMed] [Google Scholar]
- 16.Noori NM, Mahjoubifard M, Mohammadi M, Jahangiri Fard A, Abassi A, Farzanegan B. Comparison of QT dispersion with left ventricular mass index in early diagnosis of cardiac dysfunction in patients with ß-thalassemia major. Iran Red Crescent Med J. 2014;16:e11698. doi: 10.5812/ircmj.11698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Noori NM, Mehralizadeh S. Echocardiographic evaluation of systolic and diastolic heart function in patients suffering from beta-thalassemia major aged 5-10 years at the Zahedan Research Center for children and adolescent health. Anadolu Kardiyol Derg. 2010;10:150–3. doi: 10.5152/akd.2010.041. [DOI] [PubMed] [Google Scholar]
- 18.Bhatia V, Nayyar P, Dhindsa S. Brain natriuretic peptide in diagnosis and treatment of heart failure. J Postgrad Med. 2003;49:182–5. [PubMed] [Google Scholar]
- 19.Koch A, Zink S, Singer H. B-type natriuretic peptide in paediatric patients with congenital heart disease. Eur Heart J. 2006;27:861–6. doi: 10.1093/eurheartj/ehi773. [DOI] [PubMed] [Google Scholar]
- 20.Mariano-Goulart D, Eberlé MC, Boudousq V, Hejazi-Moughari A, Piot C, Caderas de Kerleau C, et al. Major increase in brain natriuretic peptide indicates right ventricular systolic dysfunction in patients with heart failure. Eur J Heart Fail. 2003;5:481–8. doi: 10.1016/s1388-9842(03)00041-2. [DOI] [PubMed] [Google Scholar]
- 21.Kremastinos DT, Hamodraka E, Parissis J, Tsiapras D, Dima K, Maisel A. Predictive value of B-type natriuretic peptides in detecting latent left ventricular diastolic dysfunction in beta-thalassemia major. Am Heart J. 2010;159:68–74. doi: 10.1016/j.ahj.2009.10.025. [DOI] [PubMed] [Google Scholar]
- 22.Kremastinos DT, Tsiapras DP, Kostopoulou AG, Hamodraka ES, Chaidaroglou AS, Kapsali ED. NT-proBNP levels and diastolic dysfunction in beta-thalassaemia major patients. Eur J Heart Fail. 2007;9:531–6. doi: 10.1016/j.ejheart.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Niedner MF, Foley JL, Riffenburgh RH, Bichell DP, Peterson BM, Rodarte A. B-type natriuretic peptide: Perioperative patterns in congenital heart disease. Congenit Heart Dis. 2010;5:243–55. doi: 10.1111/j.1747-0803.2010.00396.x. [DOI] [PubMed] [Google Scholar]
- 24.Li J, Levick SP, DiPette DJ, Janicki JS, Supowit SC. Alpha-calcitonin gene-related peptide is protective against pressure overload-induced heart failure. Regul Pept. 2013;185:20–8. doi: 10.1016/j.regpep.2013.06.008. [DOI] [PubMed] [Google Scholar]
- 25.Marangoni MN, Brady ST, Chowdhury SA, Piano MR. The co-occurrence of myocardial dysfunction and peripheral insensate neuropathy in a streptozotocin-induced rat model of diabetes. Cardiovasc Diabetol. 2014;13:11. doi: 10.1186/1475-2840-13-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang ZW, Lin R, Li JH, Hu J, Wang X. Perioperative changes in plasma endothelin and calcitonin gene-related peptide in congenital heart disease with pulmonary hypertension. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2003;32:212–4. doi: 10.3785/j.issn.1008-9292.2003.03.010. [DOI] [PubMed] [Google Scholar]
- 27.Xin P, Sun M, Sun G, Ding H, Zhu W, Wu Z, et al. The relationship of the calcitonin gene-related peptide and the right ventricular function in patients with pulmonary hypertension. J Youjiang Med Coll Natly. 2005;1:1. [Google Scholar]
- 28.Fang W, Chen H, Huang J, Luo Z, Huang J. Clinical observation of significance of urotensin II, calcitonin gene related peptide and endothelin in patients with congenital heart disease complicated with secondary pulmonary hypertension. Chin J Extracorpor Circ. 2008;3:11. [Google Scholar]


