Abstract
Purpose
Hachimijiogan (HJG, Rehmannia Eight Formula), a kidney‐replenishing Kampo formula, is clinically known to be effective in the treatment of male infertility with oligozoospermia. The purpose of this study was to evaluate the effect of HJG on the epididymal sperm characteristics and related serum hormone changes in rats in an attempt to determine its mechanism.
Methods
Male Wistar–Imamichi rats (233.4 ± 5.2 g, nine weeks old) were assigned randomly to four groups (n = 6 for each group). Apart from one control group treated with distilled water, the other groups were administered HJG consecutively for 9–11 days with doses of 250, 500 and 1,000 mg/kg. After the last administration the caude epididymides were quickly removed under anesthesia for assessing sperm characteristics. Additionally, the testes, seminal vesicles, prostate and adrenal glands were removed surgically and their wet weights measured.
Results
Results showed that HJG increased sperm numbers and motility as well as the weights of seminal vesicles and adrenal glands at lower doses. Moreover, HJG decreased serum levels of testosterone and luteinizing hormone while increasing follicle‐stimulating hormone levels.
Conclusions
Our findings may support the conclusion that a lower dosage of HJG has an effect on improving local spermatogenous environments by activating adrenal functions and/or promoting local androgen activity.
Keywords: Hachimijiogan, Kampo medicine, Kidney‐replenishing, Male infertility, Sperm characteristics
Introduction
Based on the latest population statistical data of the Japanese government, Japan's population has been decreasing naturally for the sixth consecutive year and the number of people over 65 years topped 30 million for the first time in 2013 [1] and the population younger than 14 has decreased to a minimum of 16.6 million. Thus, Japan's “low fertility and aging society,” or shoshi kōreika shakayi, means Japan has a serious social issue that will affect all Japanese social structures and economic development in the near future. As such, it is critical the Japanese government not only address its aging population and associated burdensome medical and welfare expenses but also the difficulty of ensuring a labor force.
The background of very lower fertility in Japan is an issue complicated by factors such as low economic growth and changes in family values among young Japanese. Consequently, increasing infertility in women and men is considered to be one of the main reasons the public media refer to Japan as an “infertility society,” or funin no shakai. In an attempt to address this problem the Japanese and local governments have in recent years taken various measures such as increasing nurseries, introducing a childcare leave system and, in particular, subsidizing infertility treatment.
Unlike female infertility, the recognition and treatment of male infertility has not attracted attention until recently due to cultural and social Japanese customs. In fact, approximately one third of infertility problems are due to female infertility and one third are attributable to male infertility. Infertility in the remaining cases affects both partners or the cause of infertility is unclear [2]. Male infertility can be caused by a variety of disorders, including anatomical problems, hormonal imbalances, genetic defects and psychological or behavioral problems. However, the most common cause of male infertility is due to sperm production abnormalities such as a low sperm count and/or poor sperm quality [2]. Interestingly, in a recent cross‐sectional population study Iwamoto et al. [3] reported that semen quality of young Japanese people is lower than that of a reference population of fertile men.
Treatment of male infertility depends upon the underlying cause. Testicular sperm extraction and drug therapy for hormone disorders are the usual treatments, in addition to surgery. On the other hand, traditional Chinese–Japanese medicine (Kampo medicine) is applied widely due to its efficacy and few side effects. Hachimijiogan (HJG, Rehmannia Eight Formula) is a representative Kampo formula used to treat idiopathic male infertility (efficacy rate of 45–60% [4]) and oligozoospermia [5, 6, 7, 8]; it is also combined with other supplemental Kampo formulae such as ninjinto [9, 10].
The formula consists of Rehmannia root, Cornus fruit, Dioscorea rhizome, Alsima rhizome, Poria sclerotium, Moutan bark, Cinnamomi bark and processed Aconite root. The formula is a famous ancient kidney‐replenishing formula that reactivates degenerated kidney function in attempts at alleviating severe fatigue and lassitude, dysuria or polyuria and senility [11, 12]. In light of Chinese–Japanese medicinal theory, the kidney is a critical reproductive organ the qi (energy flow) of which is the material basis of body growth, development and reproduction [13].
Despite HJG being known as effective at improving male fertility, its pharmacological mechanism is still relatively unclear. Therefore, the purpose of this study was to evaluate the effect of HJG on the epididymal sperm characteristics and related serum hormone changes in healthy male rats, thereby potentially determining its mechanism.
Materials and methods
Animals
Male Wistar–Imamichi rats (eight weeks old) were obtained from the Institute for Animal Reproduction (Ibaraki, Japan). They were reared in an air‐conditioned animal housing facility at the Laboratory of Comparative and Behavioral Medicine, Nippon Veterinary and Life Science University (Musano, Japan). The rats were housed in sterilized polypropylene cages (one rat/cage) and provided laboratory pellet chow (Labo MR Stock, Nosan Corporation, Japan) and water ad libitum. The rats were allowed to acclimate to the room for one week before commencing the experimental procedures. This experiment was performed in accordance with the Guidance of Ethical Committee for Research on Laboratory Animals of Nippon Veterinary and Life Science University.
Preparation of Hachimijiogan and experimental design
A crude powder of Hachimijiogan (Table 1) was manufactured at the GMP pharmaceutical factory of Kracie Pharma Ltd. (Takaoka, Japan) by mixing the powders of Rokumijiogan (Lot No. QH2116S), Cinnamomi bark (Lot No. 11100523) and processed Aconite root (Lot No. 11112907), each of which were prepared via special processes, including a cryogenic crushing method. Rokumijiogan is composed of Rehmannia root, Cornus fruit, Dioscorea rhizome, Alsima rhizome, Poria sclerotium and Moutan bark. The crude powder of Hachimijiogan was suspended in distilled water just before administration.
Table 1.
Composition (daily dose) of Kampo formula Hachimijiogan (HJG) powdered crude drugs
| Ingredients | Contents (mg) | |
|---|---|---|
| English name | Latin name | |
| Rehmannia root | Rehmaniae radix | 1,072 |
| Cornus fruit | Corni fructus | 536 |
| Dioscorea rhizome | Dioscorea rhizoma | 536 |
| Alisma rhizome | Alisma rhizoma | 402 |
| Poria sclerotium | Poria | 402 |
| Moutan bark | Motan cortex | 402 |
| Cinnamomi bark | Cinnamomi cortex | 134 |
| Processed aconite root | Processi aconiti radix | 134 |
HJG powdered crude drugs were prepared at the GMP‐standardized factory of Kracie Pharma, Ltd. (Japan)
Rats were assigned randomly to four groups on the basis of their average body weights (233.4 ± 5.2 g). Apart from a control group treated with distilled water, the others were consecutively administered HJG with low, medium and high dose rates (250, 500, 1,000 mg/kg; p.o.) for 9–11 days. The middle dose was determined based on the daily clinical dose (3,618 mg/d). After the last administration blood collection from the ventral vena cava and organ removal (testes, seminal vesicles, prostate gland and adrenal glands) were immediately carried out in each animal under pentobarbital anesthesia (somnopentyl®, 150 mg/kg, i.p); the rats were then sacrificed by cervical dislocation. Serum samples were prepared by centrifugation at 3,000 rpm for 15 min and stored at −20 °C until the assay.
Cauda epididymal sperm collection and assessment of sperm characteristics
The caude epididymides were quickly removed from the male rats and cut into small pieces allowing the spermatozoa to disperse into 3 ml of a pre‐warmed medium at 37 °C (Modified HTF medium, Human Tubal Fluid HEPES buffered with Gentamicin, Irvine Scientific, Lot No. 90126130603). The sperm suspension was placed in an incubator at 37 °C for 15 min prior to assessing sperm motility, abnormalities and count as described below.
Sperm motility
Sperm motility was assigned three grades on the basis of the nature and strength of sperm movement(i.e., + (active forward movement); +/− (slow forward movement and rotation); − (no movement). A 2‐μl aliquot of the sperm suspension was further diluted 10 times in a warm medium, placed on thin cover glass and observed under a light microscope (×100 magnification). In order to make a statistical comparison, motility was expressed as the percentage of motile sperm to the total number of sperm.
Sperm abnormality
The same smear prepared above was used. Sperm abnormality was tabulated by noting the percentage of abnormal sperm heads, mid‐sections and tails.
Sperm count
The epididymal sperm count was determined by haemocytometry (an Erma improved Neubauer counting chamber, Erma Inc., Japan) by counting 25 × 16 squares (1 × 1 × 0.1 mm) under a light microscope (200× magnification). A 10‐μl aliquot of sperm suspension was diluted 100 times with a Formalin‐Saline solution (Paraformaldehyde, Merk KGaA 64271 Darmstadt, Germany), loaded in the counting chamber and the sperm count determined on the basis of the formula: sperm number = total number of sperm in squares × 104 (sperm in 1 ml) × 102 (diluted times) × volume of medium (3 ml).
Measurement of testosterone (T), follicle stimulating hormone (FSH) and luteinizing hormone (LH)
Total serum levels of testosterone (Lot No. 308769, R&D Systems, USA), LH (Lot No. 110513, Endocrine technologies, Inc., USA) and FSH (Lot No. 140129622, Cloud‐Clone Corp., USA) were measured with ELISA test kits according to the attached protocols. ELISA kits were purchased from Hirano Pure Chemical Co. Ltd. (Fukui, Japan). All of the samples were run at the same time to avoid inter‐assay variation.
Statistical analysis
Experimental data are expressed as mean ±SEM. Statistical differences between groups were analyzed by One Way Analysis of Variance (ANOVA) followed by a Dunnett's test. Values of p less than 0.05 were accepted as statistically significant.
Results
Effect on body weight gain
The mean body weight gain for each group is shown in Fig. 1. Treatment with HJG for 9–11 days increased body weights in a dose‐dependent manner, although there were no significant differences compared to the control.
Figure 1.
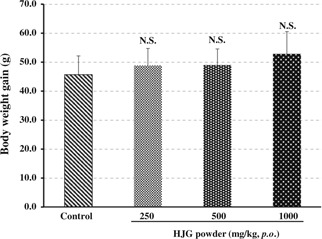
Effect of the HJG crude powder on body weight gain at different doses. Each column represents the mean ±SE (n = 6). NS, p > 0.05 versus control (Dunnett's test)
Effect on the weight of testes, seminal vesicle, prostate gland and adrenal glands
The mean absolute and relative weight of testes, seminal vesicles, prostate glands and adrenal glands are tabulated in Table 2. Compared to the control group, approximately 3.6 to 4.7% or 4.5 to 5.0% of absolute or relative testes weight decreases were observed in each group treated with different doses of HJG. And the prostate glands were decreased by HJG both in their absolute and relative testes weight by approximately 7.2 to 19.2% or 7.9 to 20.1%; the medium dose (250 mg/kg) was particularly significant. On the other hand, HJG increased the weight of the seminal vesicles as well as adrenal glands in the order of low > medium > high dose rate in comparison to the control group both in their absolute (10.0% > 6.9% > 5.9%, and 8.8% > 5.3% > 1.5%, respectively) and relative weights (10.4% > 5.4% > 4.7%, and 12.5% > 6.3% > 0.0%, respectively).
Table 2.
Effects of HJG powdered crude drugs on the weight of testes, seminal vesicles, prostate and adrenal glands
| Groups | Organs absolute weights, mg/BW g (relative weights, mg/BW g) | |||
|---|---|---|---|---|
| Testes | Prostate gland | Seminal vesicles | Adrenal glands | |
| Control | 2,617.2 ± 51.2 (9.34 ± 0.17) | 389.3 ± 24.9 (1.39 ± 0.08) | 838.7 ± 59.3 (2.99 ± 0.21) | 45.6 ± 1.2 (0.16 ± 0.006) |
| Low‐HJG | 2494.5 ± 37.1 (8.92 ± 0.20) | 359.3 ± 17.5 (1.28 ± 0.06) | 922.2 ± 36.1 (3.30 ± 0.14) | 49.6 ± 3.8 (0.18 ± 0.012) |
| Medium‐HJG | 2524.2 ± 41.0 (8.89 ± 0.13) | 314.5 ± 13.5 (1.11 ± 0.06) | 896.7 ± 49.1 (3.15 ± 0.16) | 48.0 ± 1.5 (0.17 ± 0.006) |
| High‐HJG | 2521.3 ± 61.7 (8.87 ± 0.33) | 361.2 ± 34.9 (1.27 ± 0.13) | 888.5 ± 32.2 (3.13 ± 0.17) | 46.3 ± 1.8 (0.16 ± 0.006) |
Mean ± SEM (n = 6)
Effect on epididymal sperm characteristics (sperm count, motility and abnormality)
The mean total sperm number and motility grade of sperm treated with distilled water (0 mg/kg, control) and HJG (250, 500, 1,000 mg/kg) are shown Table 3. In comparison with the control, HJG increased sperm numbers in the order of: medium (81.8%) > low (35.5%) > high (27.3%) dose rate. Sperm motility with grade (+) was enhanced in the order of: low (35.7%) > medium (23.7%) > high (7.1%) dose rates; while no significant sperm morphological abnormalities (head, mid‐piece and tail) were observed in any group, although HJG slightly decreased tail defects compared to the control.
Table 3.
Effects of HJG powdered crude drugs on sperm characteristics in healthy male rats
| Groups | Total sperm numbers (×106) | Motility grades (%) | Abnormality (%) | ||||
|---|---|---|---|---|---|---|---|
| + | +/− | − | Head | Midpiece | Tail | ||
| Control | 33.0 ± 4.96 | 35.0 ± 4.83 | 40.8 ± 5.07 | 24.2 ± 2.71 | 0.0 ± 0.00 | 0.4 ± 0.19 | 3.4 ± 0.91 |
| Low‐HJG | 44.7 ± 7.80 | 47.5 ± 6.80 | 31.7 ± 6.28 | 20.8 ± 3.00 | 0.1 ± 0.05 | 0.2 ± 0.10 | 2.8 ± 0.67 |
| Medium‐HJG | 60.0 ± 13.5 | 43.3 ± 7.82 | 35.8 ± 8.98 | 20.8 ± 2.01 | 0.1 ± 0.05 | 0.3 ± 0.05 | 2.0 ± 0.35 |
| High‐HJG | 42.0 ± 10.3 | 37.5 ± 4.96 | 40.0 ± 4.83 | 22.5 ± 1.12 | 0.0 ± 0.00 | 0.2 ± 0.07 | 2.8 ± 0.58 |
Sperm motility grades: + (active forward movement); +/− (slow forward movement and rotation); −(no movement)
Mean ± SEM (n = 6)
Effect on serum testosterone, LH and FSH levels
As presented in Table 4, HJG decreased serum testosterone levels in a non‐dose dependent manner as well as serum LH levels. On the other hand, HJG showed a tendency to decrease serum FSH levels, particularly at low doses as compared to the control.
Table 4.
Effects of HJG powdered crude drugs on serum testosterone, LH and FSH levels
| Group | Testosterone (ng/ml) | LH (ng/ml) | FSH (ng/ml) |
|---|---|---|---|
| Control | 16.6 ± 3.07 | 3.39 ± 0.34 | 31.9 ± 3.51 |
| Low‐HJG | 6.70 ± 0.728 | 2.25 ± 0.37 | 37.9 ± 1.69 |
| Medium‐HJG | 14.3 ± 3.89 | 2.54 ± 0.43 | 34.7 ± 2.35 |
| High‐HJG | 12.7 ± 3.45 | 1.90 ± 0.28* | 31.3 ± 1.02 |
*Versus control, p < 0.05 (Dunnett's test); Mean ±SEM (n = 6)
Discussion
Kampo medicine (traditional Chinese‐Japanese medicine) has been widely used in the modern healthcare system of Japan for approximately 40 years along with Western medicine or modern medicine. In particular, Kampo medicine is preferred in the treatment of chronic disease such as allergies, dementia, obesity and infertility, and often as a first choice to treat male infertility in order to avoid the adverse effects of drug therapy or the inconvenience of surgery.
The most common cause of male infertility is sperm production abnormalities such as low sperm counts and/or poor sperm quality [2]. Kampo medicine offers a different perspective from modern medicine in understanding spermatogenesis, namely, kidney qi (essence, energy) which is the material basis of human body growth, development and reproduction [13]. In other words, low sperm counts and/or poor sperm quality, including sexual dysfunction, is due to the losing of kidney qi. Thus, a famous ancient kidney‐replenishing formula, HJG is designed to reactivate the functions of kidneys, adrenals and reproductive organs [12], and HJG has been widely applied in the treatment of male infertility. Outstanding achievements have been obtained [5, 6, 7, 8, 9, 10]. This study aimed to evaluate the effect HJG on the sperm quality of adult rats during 9–11 days of treatment by means of the cauda epididymis; only sperm from the cauda epididymis are suitable for in vitro fertilization [14].
HJG increased total sperm numbers and sperm motility while decreasing tail defects in a non‐dose dependent manner. Treatment of HJG at low and medium doses showed stronger effects than that of high doses (Table 3). Furthermore, the levels of serum testosterone in HJG treated rats decreased as did levels of LH. On the other hand, levels of serum FSH increased greatlyly in the mice treated with HJG at low and medium doses. Results seem to suggest that lower doses of HJG (250, 500 mg/kg) increase epididymal sperm counts by stimulating FSH release. This is apparently because FSH plays a key role in spermatogenesis in Sertoli cells [15] and decreases LH levels, which may in turn induce serum testosterone decline, resulting in weight loss of the prostate gland because this organ is considered to be testosterone‐dependent (Table 2). On the contrary, HJG interestingly increased both absolute and relative weights of seminal vesicles, although that also is a testosterone‐dependent organ, suggesting HJG may have local androgenic activity. Early studies reported that HJG produces testosterone in adult rat testes [16] and increases adrenal corticosteroids [17], but has no androgenic activity via the hypothalamic‐pituitary–testicular system [18]. In fact, we also found that HJG did not enhance serum testosterone levels in castrated mice or rats in our previous study (data not shown). Furthermore, Yoshimura et al. [19] reported that low‐dose HJG significantly improves dysuria of patients with benign prostatic hyperplasia and is safe without side effects other than epigastric discomfort. These findings suggest an optimal dosage of HJG may exist and compel pharmacological action. Other Kampo formulae, such as saikokaryukotsuboreito, reportedly induce a similar dose–response pattern in serum testosterone levels in mice [20] and monoamine‐related substances of the mouse brain [21].
It is notable that the body weights of rats treated with HJG increased in a dose‐dependent manner as comparison to the control (Fig. 1). This indicates HJG should have anabolic properties that may benefit germ cell development and spermatogenesis. In addition, Dioscorea rhizome (from Dioscorea batatas), one of components in HJG, has been reported to induce release of growth hormones in vitro and in vivo [22], suggesting it may partly contribute to the anabolic properties of HJG. Moreover, Usuki verified that HJG enhances deoxyribonucleic acid alpha‐nucleotidyltransferase activity in relationship to DNA synthesis by ovarian follicles via a cyclic AMP system [23].
Furthermore, HJG increased the weight adrenal glands at a lower dose, though they were not significant compared to the control (Table 2). Spermatogenesis is dependent on a dual control: local production of pituitary hormone FSH and androgens in response to LH has been known; however, the detailed mechanism of these hormone functions during spermatogenesis is yet to be fully understood. On the other hand, Kampo medicine offers a unique recognition, namely the kidney qi plays a crucial role in spermatogenesis [13]. In fact, the relationship between the adrenal glands and the gonads has been observed and documented since the 19th century. The notion that adrenal gland hormones, such as corticosteroids, exert a metabolic action on spermatogenesis rather than act directly on the pituitary‐gonad system is plausible [24].
Taken together these findings suggested that HJG may, in a sense, locally improve spermatogenous environments by activating or enhancing adrenal functions. This is consistent with the concept of “kidney‐replenishing” because the term “kidney” in Kampo theory not only refers to kidney organ, but also includes the adrenal glands and related meridian [13]. Therefore, four kinds of crude drugs, Rehmannia root, Cornus fruit, Dioscorea rhizome and processed Aconite root with “kidney‐replenishing” and/or “kidney‐warming” actions, are used in HJG [12]. In fact, Cornus fruit has been verified to enhance motility of human sperm in vitro [25], and mesaconitine, one of the alkaloids from Aconite root, may have an effect on sperm release by inducing contraction of the vas deferens [26]. Mesaconitine is known as a major toxic alkaloid in Aconite root and, therefore, further study is necessary to clarify the role of Aconite root, as well as Cornus fruit and other crude dugs, as to whether they contribute to the pharmacological actions of the HJG formula. In the meantime, it also suggests that using this mixed medicine, namely, a crude multi‐drug HJG formula, is necessary in clinical application rather than a single crude drug.
In summary, results could support the clinical findings that lower doses of HJG has an effect on improving local spermatogenous environments by activating adrenal functions and/or possessing local androgen activity. In addition, further study on the effects of HJG in aging and/or “kidney‐vacuity” rats is under investigation and will report elsewhere.
Acknowledgments
The authors would like to thank Prof. Kawakami Eiichi (Department of Reproduction, Nippon Veterinary and Life Science University) for his technical assistance with the sperm characteristics assessment.
Conflict of interest
Toru R. Saito has received research grants from Kracie Pharma, Ltd. Yuying Wang, Chiaki Murayama, Seiwa Michihara and Hisayoshi Norimoto declare that they have no conflict of interest.
Animal studies
All institutional and national guidelines for the care and use of laboratory animals were followed.
Human rights statements and informed consent
This article does not contain any studies with human subjects performed by any of the authors.
References
- 1.Statistics Bureau, Ministry of Internal Affairs and Communications, Japan [Internet]. Current Population Estimates as of October 1, 2013. http://www.stat.go.jp/data/jinsui/. Accessed 15 Jun 2014.
- 2.World Health Organization. WHO laboratory manual for the examination of human semen and sperm‐cervical muscus interaction. Cambridge University Press; 1999.
- 3. Iwamoto T, Nozawa S, Mieno MN, Yamakawa K, Baba K, Yoshiike M, Namiki M, Koh E, Kanaya J, Okuyama A, Matsumiya K, Tsujimura A, Kanetake H, Eguchi J, Skakkebaek NE, Vierula M, Toppari J, Jørgensen N. Semen quality of 1559 young men from four cities in Japan: a cross‐sectional population‐based study. BMJ Open, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Miyakawa Y, Matsumiya K, Okuyama A. Alteration of spermatogenesis (article in Japanese). Sannfujinkachiryo, 2002, 85, 543–546 [Google Scholar]
- 5. Miura K, Matsuhashi M, Maki A, Takanami M, Fujio K, Nakayama K, Shirai M, Ando K. Clinical experience of Hachimijiogan for male infertility patients (article in Japanese). Hinyokika Kiyo., 1984, 30, 97–102 [PubMed] [Google Scholar]
- 6. Fuse H, Iwasaki M. Effectiveness of the treatment with traditional Chinese medicine for idiopathic male infertility (article in Japanese). Pharma Medica, 2000, 18, 93–98 [Google Scholar]
- 7. Watanabe M, Yoshida H. Kampo prescription in male infertility (article in Japanese). HInyoki gekka., 1997, 10, 1091–1093 [Google Scholar]
- 8. Naitoh Y, Yoshida H, Imamura K. Clinical effects and hormonal changes on the treatment with Chinese herb medicine (HACHIMI‐JIOU‐GAN) to infertile men (article in Japanese). Jap J Fert, 1985, 30, 156–162 [Google Scholar]
- 9. Nishizawa Y. The effect of Chinese drug therapy on the patients with male infertility. 1) Concomitant administration of ninjinto and hachimijiogan on patients with male infertility (article in Japanese). Hinyokika Kiyo., 1984, 30, 265–273 [PubMed] [Google Scholar]
- 10. Shiina M, Sumi Y, Toshimura S, Oda T, Ohno T. Clinical experience of ninjinto and hachimijiogan for male infertility patients—Especially regarding to the cases combined with AIH (article in Japanese). Jap J Fert Ster, 1985, 30, 303–307 [Google Scholar]
- 11.The Japanese Pharmacopoeia (JP XV) English version The Ministry of Health, Labor and Welfare. Japan; 2006. p. 1656–1659.
- 12. Hsu HY, Hsu CS Commonly used Chinese herb formulas with illustrations, 1980. Irvine: Ohai Press; 250–252 [Google Scholar]
- 13. Zhang EQ. Basic theory of traditional Chinese medicine (I). In a practical English–Chinese library, 1999. Shanghai: Publishing House of Shanghai University of Traditional Chinese Medicine; 100–105 [Google Scholar]
- 14. Susan M, Martin HA Marten HH. Jan D. In vitro Fertilization/Cryopreservation. Transgenic Mouse Methods and protocols, 2002. New York: Humana Press; 35–50 [Google Scholar]
- 15. O'shaughnessy PJ. Hormonal control of germ cell development and spermatogenesis. Semin Cell Dev Biol, 2014. [DOI] [PubMed] [Google Scholar]
- 16. Utsuki S. Hachimijiogan produces testosterone in adult rat testes. Am J Chin Med, 1988, 16, 93–105 10.1142/S0192415X88000169 [DOI] [PubMed] [Google Scholar]
- 17. Itoh T, Tanaka N, Shibahara N, Kita T, Hashiba M, Shimada Y, Kobayashi Y, Terasawa K. Effect of Hachimi‐jio‐gan on adrenal corticosteroids. J Trad Med, 1998, 15, 155–160 [Google Scholar]
- 18. Utsugi T, Igarashi M, Yazaki C, Hasegawa Y, Miyamoto K, Taniguchi Y, Nomura S, Shinkawa T. Effects of Hachimijiogan on hypothalamo‐pituitary‐testicular system (article in Japanese). Nihon Sanka Fujinka Gakkai Zasshi., 1983, 35, 2305–2310 [PubMed] [Google Scholar]
- 19. Yoshimura K, Terai A, Arai Y. Two‐week administration of low‐dose Hachimi‐jio‐gan (Ba‐Wei Di‐Huang‐Wan) for patients with benign prostatic hyperplasia (article in Japanese). Hinyokika Kiyo., 2003, 49, 509–514 [PubMed] [Google Scholar]
- 20. Michihara S, Shin N, Watanabe S, Morimoto Y, Okubo T, Norimoto H. A Kampo formula, saikokaryukotsuboreito, improves serum testosterone levels of castrated mice and its possible mechanism. Aging Male., 2013, 16, 17–21 10.3109/13685538.2012.755507 [DOI] [PubMed] [Google Scholar]
- 21. Ito T, Murai S, Saito H, Ito M, Odashima J, Michijiri S, Hashimoto N. Effect of Saiko‐ka‐ryukotsu‐borei‐to on the monoamine‐related substances in several regions of mouse brain. Nihon Toyo Igaku Zasshi (Jap J Orient Med)., 1994, 45, 97–106 10.3937/kampomed.45.97 [Google Scholar]
- 22. Lee HY, Jung DY, Ha H, Son KH, Jeon SJ, Kim C. Induction of growth hormone release by dioscin from Dioscorea batatas DECNE. J Biochem Mol Biol, 2007, 40, 1016–1020 10.5483/BMBRep.2007.40.6.1016 [DOI] [PubMed] [Google Scholar]
- 23. Usuki S. Hachimijiogan and Tokishakuyakusan enhance deoxyribonucleic acid alpha‐nucleotidyltransferase activity in relationship to DNA synthesis by ovarian follicles via a cyclic AMP system. Am J Chin Med, 1988, 16, 37–46 10.1142/S0192415X88000078 [DOI] [PubMed] [Google Scholar]
- 24. Kuyama M. Cytological studies on the rat testis after total adrenalectomy (article in Japanese). J Tokyo W Med Univ, 1965, 35, 695–705 [Google Scholar]
- 25. Jeng H, Wu CM, Su SJ, Chang WC. A substance isolated from Cornus officinalis enhances the motility of human sperm. Am J Chin Med, 1997, 25, 301–306 10.1142/S0192415X97000330 [DOI] [PubMed] [Google Scholar]
- 26. Sato H, Ohizumi Y, Hikino H. Mechanism of mesaconitine‐induced contractile response in guinea pig vas deferens. Eur J Pharmacol, 1979, 55, 83–92 10.1016/0014‐2999(79)90150‐X [DOI] [PubMed] [Google Scholar]


