Abstract
Patient: Male, 81
Final Diagnosis: Bochdalex hernia
Symptoms: Chest pain • vomiting
Medication: —
Clinical Procedure: Laparoscopic repair of both diaphragmatic hernias
Specialty: Surgery
Objective:
Rare co-existance of disease or pathology
Background:
A Bochdalek hernia (BH) is a rare congenital condition consisting of a posterolateral defect in the diaphragm. A para-esophageal hernia (PEH) is a rare variant of hiatus hernia. BH and PEH may present with gastric volvulus or incarceration, requiring emergency treatment. Minimally invasive surgery is the preferred treatment, particularly for elderly patients and patients with comorbidities. The occurrence of BH with concomitant PEH is a very rare event. We describe a case of an octogenarian patient with BH and concomitant PEH treated laparoscopically.
Case Report:
An 81-year-old male patient, without significant comorbidities, presented with a two-month history of severe chest pain and vomiting after eating. Cardiological investigations ruled out cardiac ischemia, infarction, or other cardiovascular abnormalities. Chest and abdominal computed tomography (CT) imaging demonstrated a large diaphragmatic hernia, with the entire stomach in the left thorax. Laboratory results showed mild anemia and a low iron level. The patient underwent simultaneous laparoscopic repair of a BH and a PEH with mesh reinforcement without antireflux fundoplication. The patient’s postoperative recovery was uneventful.
Conclusions:
We have presented a rare case of BH with concomitant PEH in an octogenarian that was successfully treated with laparoscopic surgery. Although these two forms of hernia are a very rare association, this case report illustrates that the surgical approach should be individualized in each patient’s case to ensure a successful surgical outcome. In this case, the decision was made to suture the diaphragmatic crura and reinforce the diaphragm repair with mesh, rather than by fundoplication.
MeSH Keywords: Hernia, Diaphragmatic; Herniorrhaphy; Laparoscopy
Background
A Bochdalek hernia (BH) is a rare congenital condition consisting of a posterolateral defect in the diaphragm, first described in 1848 by the Czech anatomist, Vicente Bochdalek who studied diaphragmatic hernia in newborns [1,2]. The BH occurs through a posterolateral defect in the diaphragm [3,4]. Since Bochdalek’s description of the diaphragmatic defect, for many years, no satisfactory approach to the surgical repair of BH was developed, particularly for newborn infants, who undergo respiratory compromise due to herniation of the stomach and other organs into the thorax, and the mortality rate in newborns remains high [5,6]. The first successful surgical repair of BH was performed in 1901 [7]. The incidence of BH is reported as 1 in 3,000 live births, and usually occurs on the left side in between 80–90% of cases; right-sided BH is less common because the right side of the diaphragm develops earlier than the left side in embryogenesis [8]. However, a congenital diaphragmatic hernia can go unnoticed during childhood, and individuals can reach adulthood without symptoms, but BH is rare in adults and accounts for between 0.17–6% of all diaphragmatic hernias [9].
In 1926, Akerlund was the first to describe repair of a paraesophageal hernia (PEH) [10]. The incidence of PEH is between 3.5–5% of all hiatal hernias [11,12]. Furthermore, advanced age, vertebral deformity, and concomitant diseases are common risk factors that frequently occur in patients with PEH [13]. PEH may present with sudden chest pain or abdominal pain, dysphagia, vomiting, or anemia and gastric volvulus or incarceration may occur, requiring emergency surgical treatment [13]. Patients who have PEH may be poor operative candidates, and minimally invasive surgery is the preferred treatment, particularly for elderly patients and for patients with comorbidities [14].
The occurrence of BH with concomitant PEH is a very rare event. We present a rare case of an octogenarian patient suffering from a BH with concomitant PEH who was treated laparoscopically.
Case Report
An 81-year-old man, with known significant past medical history, suffered for the previous two months from severe chest pain and vomiting after eating. He was admitted to the emergency room several times for investigation of these symptoms. On the first hospital visit, clinical findings were as follows: blood pressure, 135/76 mm Hg; pulse rate, 94/min; his body temperature, 36.3°C; and oxygen saturation, 94%. Repeated electrocardiogram (ECG) showed no ischemic changes, and serum troponin levels were less than 0.01 ng/mL on two separate occasions, excluding the possibility of an ischemic cardiac event. After feeling better, he was discharged from the emergency room.
On his second admission to the emergency room, an ischemic cardiac event was again ruled out. Laboratory tests showed a mild microcytic anemia with a hemoglobin level of 11.5 gm/dl and a serum ferric level of 25 μg/dL, normal ECG, and a chest X-ray that showed a left lung that was compressed by the presence of the stomach in the chest. Computed tomography (CT) imaging of the thorax and abdomen were performed that showed that the patient’s stomach was in the mediastinum, and a mesenteric-axial volvulus was present (Figure 1).
Figure 1.
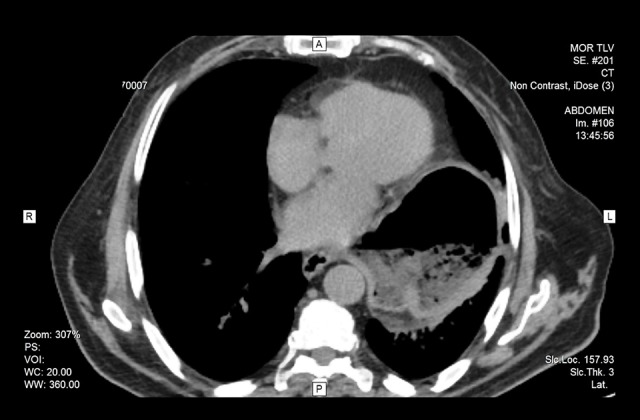
Computed tomography (CT) axial view of the abdomen. The image shows the whole stomach in the left mediastinum, full of food and air. There is a mesenteric-axial volvulus.
The patient was treated with a nasogastric tube (34 Fr), intravenous fluid, and electrolyte replacement, and was referred to our surgical institution where, without further studies, he was scheduled for surgery. Under general anesthesia in the Fowler position, with the surgeon standing between the patient’s legs, a laparoscopic approach was achieved. The stomach was reduced from the BH to the abdomen using atraumatic graspers (Figure 2). The hiatus was dissected, the hernia sac was completely reduced, and the esophagus was released from the soft adhesions in the lower mediastinum, ensuring that the lower esophagus was at least 3 cm in length in the abdominal cavity (Figure 3). The stomach was disconnected from the diaphragm by cutting the gastrophrenic ligament, ensuring the complete release of the stomach and the esophagus from the diaphragm (Figure 4). The vagus nerves were recognized and preserved.
Figure 2.
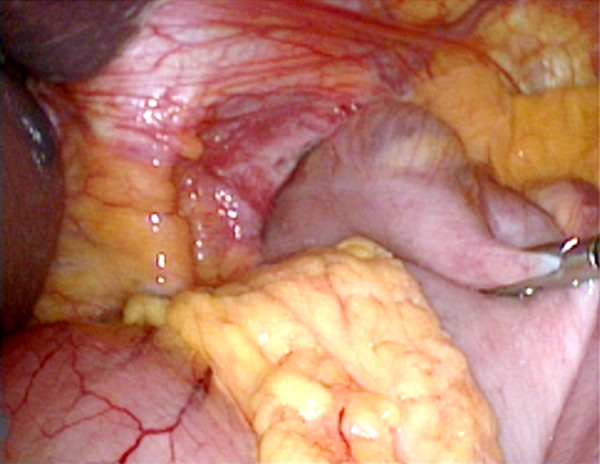
Laparoscopic surgical treatment of a Bochdalek hernia (BH). The image shows that a laparoscopic approach reduced the stomach from the Bochdalek hernia (BH) from the left chest to the abdominal cavity, following the use of atraumatic graspers.
Figure 3.
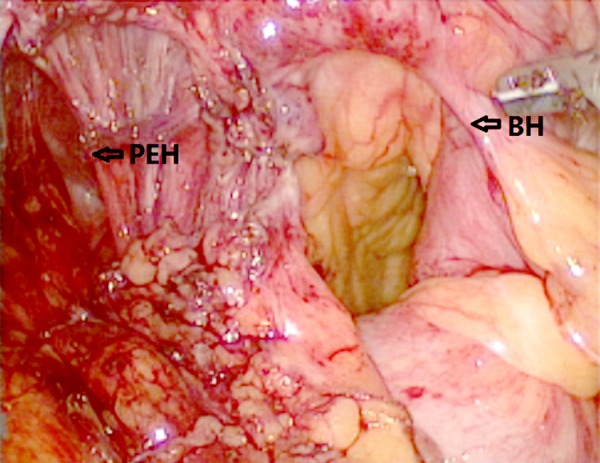
Laparoscopic surgical treatment of a Bochdalek hernia (BH). The image shows that the size of the stomach was reduced allowing views the Bochdalek hernia (BH) and the para-esophageal hernia (PEH). The hernia sac was completely reduced and the esophagus released from the soft adhesions in the lower mediastinum to ensure that there is a 3 cm length of lower esophagus in the abdominal cavity.
Figure 4.
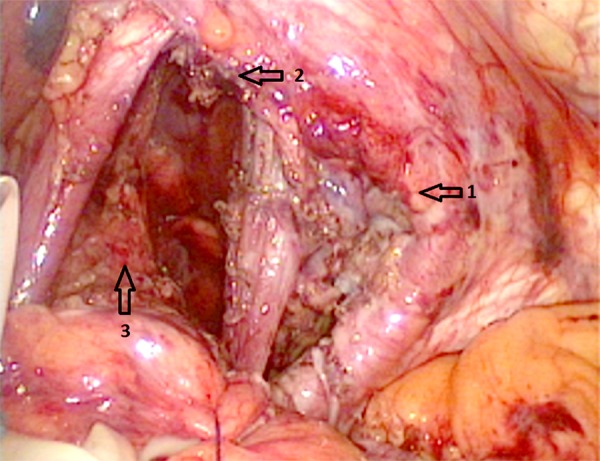
Laparoscopic surgical treatment of a Bochdalek hernia (BH). This image was taken following dissection and complete release of the stomach and esophagus, which were disconnected from the diaphragm by cutting the gastrophrenic ligament. The arrows show: 1) the Bochdalek hernia (BH); 2) the para-esophageal hernia (PEH), and 3) the esophagus.
The Bochdalek foramen was sutured in an anteroposterior direction with non-absorbable barbed sutures in a continuous fashion. The diaphragmatic crura were closed posterior to the esophagus in the same way. The repair was reinforced with a 12 cm ‘O’-shaped mesh, fastened to the diaphragm with absorbable tackers and sutures, taking special care to avoid damage to the pericardium (Figure 5). No antireflux procedures were performed.
Figure 5.
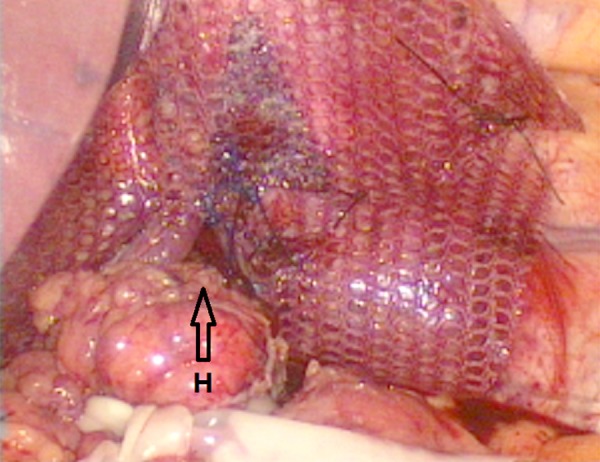
Laparoscopic surgical treatment of a Bochdalek hernia (BH). The image is taken following the suture of the Bochdalek hernia (BH) and the para-esophageal hernia (PEH) using a composite mesh to reinforce the repair, fastened to the diaphragm with absorbable tackers and sutures. H – hiatus. The Bochdalek foramen was sutured in an anteroposterior direction; the crura were closed posterior to the esophagus in the same way.
During the first postoperative day, an upper gastrointestinal fluoroscopic examination was performed showing a good esophageal passage of the contrast medium, the stomach in the correct anatomical site and adequate duodenojejunal passage (Figure 6). Postoperatively, the patient made an uneventful recovery, allowing liquid feeding on the first postoperative day and advancing to soft food on the fourth day after surgery.
Figure 6.
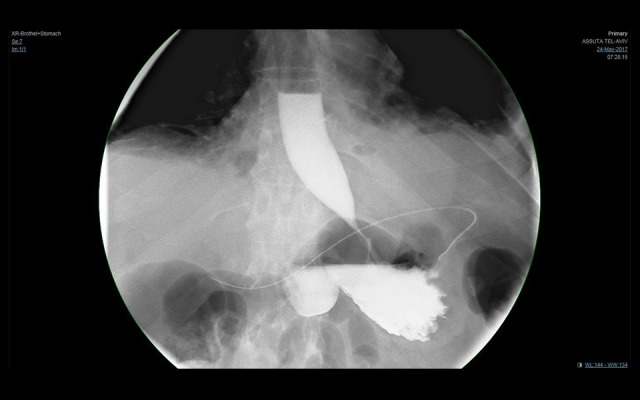
Upper gastrointestinal fluoroscopy performed 24 hours after the operation. On the first postoperative day, an upper gastrointestinal fluoroscopic examination shows a good esophageal passage of the contrast medium, the stomach in place, and there is an adequate duodenojejunal passage.
He was then discharged from the hospital, and medicated with proton pump inhibitors. The patient was subsequently seen at postoperative day 10 and one month after surgery with no reported dysphagia, tolerating all kinds of food well and without heartburn or symptoms related to reflux. The scars were normal, and he had no pain (Figure 7).
Figure 7.

The minimally-invasive laparoscopic surgical procedure. The minimally invasive surgery performed through five ports: one port measures 11 mm and four of the ports measure 5 mm. The patient was seen at postoperative day 10 and also at one month after surgery, with no reported symptoms related to reflux, with good healing, and no pain.
Discussion
The aim of this case report was to emphasize the importance of early diagnosis of the potentially life-threatening condition of a diaphragmatic hernia and to demonstrate that even congenital abnormalities of the gastrointestinal tract may be asymptomatic until late in life. In this case, although a rare association of a Bochdalek hernia (BH) with a concomitant para-esophageal hernia (PEH) was present, for patients with chest pain who have normal cardiac function tests a simple chest X-ray could have made the diagnosis on the first admission to hospital, preventing a delay in treatment.
This case report was also unusual because of the combination of BH with a concomitant PEH in an octogenarian. A review of the medical literature has not found a similar previously reported case. Congenital diaphragmatic hernias are rare in adults, and most of them are diagnosed in childhood, probably because they are small without causing symptoms and without other congenital conditions [15].
Mullins and colleagues have reported an incidence of BH in adults of 0.17%, in a large series of patients that underwent CT imaging, with a mean age of 66.6 years [16]. Rodriguez and colleagues have reported that the adult incidence of the congenital form of diaphragmatic hernia of Morgagni-Larrey is also low [17].
In this case report, the patient went to the emergency room with an incarceration of the BH. Placing a nasogastric tube and evacuating the gastric content is the treatment of choice in acute cases of diaphragmatic hernia, which can achieve reduction of the stomach [18]. However, if conservative treatment does not work in the first hours, an emergency operation must be carried out, as the clinical outcome for patient s who have delayed treatment is worse. In a study published by Synder and Greaney, they showed that in patients who had surgery during the first 72 hours following hospital admission, there was no mortality; after 72 hours, patient mortality rose to 50% [18].
In the management of this case, we choose the laparoscopic approach from the abdomen, as this is our normal approach and we use it routinely. While laparotomy is the most widely used surgical approach (38%), minimally invasive surgical techniques have gained popularity since their first report in 1995 [19]. Laparoscopic repair can be performed with a low complication rate (7%) and short hospital stay (4 days) [19]. In 2016, Machado demonstrated that the thoracotomy approach had twice the mortality rate when compared with laparotomy (4% and 2%, respectively) for repair of diaphragmatic hernia [20]. However, the outcomes were similar when treatment was by minimally invasive surgery, either by thoracos-copy or laparoscopy [20].
A new technological surgical development is the use of the barbed suture used to suture the diaphragm, which saves time and does not require knotting, this reducing the risk of suture failure [21,22]. The use of mesh in diaphragmatic repair remains controversial, and the concept of the use of this tension-free repair approach is not always applicable, has been shown for inguinal hernia repair [23]. Elderly patients may have thinner and weakened diaphragmatic muscle, and so the type of mesh to use is important as there are many available surgical meshes on the market, as follows: non-absorbable prosthetic; absorbable biosynthetic; and composite mesh [24]. Until recently, it has not been possible to demonstrate pre-clinically, or clinically, the superiority of one type of mesh over another [24]. As the biological meshes are costly and do not have any major advantages over the synthetic meshes, we chose to use synthetic mesh [25–27].
Another important aspect in the repair of diaphragmatic hernias is to perform antireflux fundoplication. However, patients with abnormal motility of the esophagus may suffer from dysphagia in the early postoperative period following fundoplication, and sometimes this can be irreversible [28]. Therefore, we do not use fundoplication routinely, but use it selectively, depending on the motility of the esophagus and on the patient’s clinical condition before the surgery [29–31]. It is also important to decide what type of antireflux mechanism to use, whether Nissen-Rosetti, Toupet, or Dor (anterior partial fundoplication) [29–31].
Laparoscopic surgery offers the best treatment outcome for patients with a diaphragmatic hernia, with short convalescence, fewer complications, and a greater patient satisfaction. The decision of reinforcing the diaphragm repair with mesh or performing a fundoplication is a decision that the surgeon must take during the surgical procedure, since there is no uniform concept about the need to add them to the procedure.
Conclusions
We have presented a rare case of a Bochdalek hernia (BH) and a concomitant para-esophageal hernia (PEH) in an octogenarian that was successfully treated with laparoscopic surgery. Although these two forms of hernia are a very rare association, this case report illustrates that the surgical approach should be individualized in each patient’s case to ensure a successful surgical outcome. In this case, the decision was made to suture the diaphragmatic crura and reinforce the diaphragm repair with mesh, rather than by fundoplication.
Footnotes
Conflict of interest
None.
References:
- 1.Loukas M, El-Sedfy A, Tubbs RS, et al. Vincent Alexander Bochdalek (1801–1883) World J Surg. 2008;32:2324–26. doi: 10.1007/s00268-008-9686-6. [DOI] [PubMed] [Google Scholar]
- 2.Kachlik D, Cech P. Vincenz Alexander Bochdalek (1801–83) J Med Biogr. 2011;19:38–43. doi: 10.1258/jmb.2010.010045. [DOI] [PubMed] [Google Scholar]
- 3.Bochdalek VA. Ueber den Peritonealueberzug der Milz und das Ligamentum pleurocolicum. Beitrag zur Anatomie des Bauchfells. Arch Anat Physiol Wiss Med. 1867:565–614. [in German] [Google Scholar]
- 4.Puri P, Wester T. Historical aspects of congenital diaphragmatic hernia. Pediatr Surg Int. 1997;21:95–100. [PubMed] [Google Scholar]
- 5.Gedik E, Tuncer MC, Onat S, et al. A review of Morgagni and Bochdalek hernias in adults. Folia Morphol (Warsz) 2011;70:5–12. [PubMed] [Google Scholar]
- 6.Newman BM, Afshani E, Karp MP, et al. Presentation of congenital diaphragmatic hernia past the neonatal period. Arch Surg. 1986;121:813–16. doi: 10.1001/archsurg.1986.01400070079017. [DOI] [PubMed] [Google Scholar]
- 7.Palanivelu C, Rangarajan M, Maheshkumaar GS, Parthasarathi R. Laparoscopic mesh repair of a Bochdalek diaphragmatic hernia with acute gastric volvulus in a pregnant patient. Singapore Med J. 2008;49:e26–28. [PubMed] [Google Scholar]
- 8.Langham MR, Jr, Kays DW, Ledbetter DJ, et al. Congenital diaphragmatic hernia: epidemiology and outcome. Clin Perinatol. 1996;23:671–88. [PubMed] [Google Scholar]
- 9.Mark E, Jeffrey SS, Saini SS, Peter RM. Prevalence of incidental Bochdalek’s hernia in a large adult population. Am J Roentgenol. 2001;177(2):363–66. doi: 10.2214/ajr.177.2.1770363. [DOI] [PubMed] [Google Scholar]
- 10.Åkerlund Å. I. Hernia Diaphragmatica Hiatus Oesophagei Vom Anatomischen und Rontgenologischen Gesichtspunkt. Acta Radiologica. 1926;6:3–22. [in German] [Google Scholar]
- 11.Hill LD, Tobias JA. Para-esophageal hernia. Arch Surg. 1968;96:735–44. doi: 10.1001/archsurg.1968.01330230043007. [DOI] [PubMed] [Google Scholar]
- 12.Luketich JD, Raja S, Fernando HC, et al. Laparoscopic repair of giant paraesophageal hernia: 100 consecutive cases. Ann Surg. 2000;232:608–18. doi: 10.1097/00000658-200010000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bawahab M, Mitchell P, Church N, Debru E. Management of acute paraesophageal hernia. Surg Endosc. 2009;23:255–59. doi: 10.1007/s00464-008-0190-8. [DOI] [PubMed] [Google Scholar]
- 14.Davis SS., Jr Current controversy in para-esophageal hernia repair. Surg Clin N Am. 2008;88:959–78. doi: 10.1016/j.suc.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 15.Fumiko K, Mitsutomi I, Satoshi H, et al. Late-presenting posterior transdiaphragmatic (Bochdalek) hernia in adults: Prevalence and MDCT characteristics. J Thoracic Imag. 2009;24:17–22. doi: 10.1097/RTI.0b013e31818c6bc8. [DOI] [PubMed] [Google Scholar]
- 16.Mullins ME, Stein J, Saini SS, Mueller PR. Prevalence of incidental Bochdalek’ s hernia in a large adult population. Am J Roentgenol. 2001;177:363–66. doi: 10.2214/ajr.177.2.1770363. [DOI] [PubMed] [Google Scholar]
- 17.Rodríguez HJ, Tuca RF, Ruiz FB, et al. [Diaphragmatic hernia of Morgagni-Larrey in adults: Analysis of 10 cases] Gastroenterol Hepatol. 2003;26:535–40. doi: 10.1016/s0210-5705(03)70408-7. [in Spanish] [DOI] [PubMed] [Google Scholar]
- 18.Snyder WH, Greaney EM. Congenital diaphragmatic hernia: 77 consecutive cases. Surgery. 1965;52:576–88. [PubMed] [Google Scholar]
- 19.Brown SR, Horton JD, Trivette E, et al. Bochdalek hernia in the adult: Demographics, presentation, and surgical management. Hernia. 2011;15:23–30. doi: 10.1007/s10029-010-0699-3. [DOI] [PubMed] [Google Scholar]
- 20.Machado NO. Laparoscopic repair of Bochdalek diaphragmatic hernia in adults. North Am J Med Sci. 2016;8:65–74. doi: 10.4103/1947-2714.177292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Demyttenaere SV, Nau P, Henn M, et al. Barbed suture for gastrointestinal closure: A randomized control trial. Surg Innov. 2009;16:237–42. doi: 10.1177/1553350609342988. [DOI] [PubMed] [Google Scholar]
- 22.Greenberg JA, Einarsson JI. The use of bidirectional barbed suture in laparoscopic myomectomy and total laparoscopic hysterectomy. J Minim Invasive Gynecol. 2008;15:621–23. doi: 10.1016/j.jmig.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 23.Lichtenstein IL, Shulman AG, Amid PK, et al. The tension free hernioplasty. Am J Surg. 1989;157:188–93. doi: 10.1016/0002-9610(89)90526-6. [DOI] [PubMed] [Google Scholar]
- 24.Gasior AC, St. Peter SD. A review of patch options in the repair of congenital diaphragm defects. Ped Surg Int. 2012;28:327–33. doi: 10.1007/s00383-012-3059-9. [DOI] [PubMed] [Google Scholar]
- 25.Schmidt E, Shaligram A, Reynoso JF, et al. Hiatal hernia repair with biologic mesh reinforcement reduces recurrence rate in small hiatal hernias. Dis Esophagus. 2014;27:13–17. doi: 10.1111/dote.12042. [DOI] [PubMed] [Google Scholar]
- 26.Köckerling F, Alam NN, Narang SK, et al. Biological meshes for inguinal hernia repair–review of the literature. Front Surg. 2015;2:48. doi: 10.3389/fsurg.2015.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huerta S, Varshney A, Patel PM, et al. Biological mesh implants for abdominal hernia repair: US food and drug administration approval process and systematic review of its efficacy. JAMA Surg. 2016;151:374–81. doi: 10.1001/jamasurg.2015.5234. [DOI] [PubMed] [Google Scholar]
- 28.Hunter JG, Swanstrom L, Waring JP. Dysphagia after laparoscopic antireflux surgery. Ann Surg. 1996;224:51–57. doi: 10.1097/00000658-199607000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Casabella F, Sinanan M, Horgan S, Pellegrini CA. Systematic use of gastric fundoplication in laparoscopic repair of paraesophageal hernias. Am J Surg. 1996;171:485–89. doi: 10.1016/S0002-9610(97)89609-2. [DOI] [PubMed] [Google Scholar]
- 30.Zornig C, Strate U, Fibbe C, et al. Nissen vs. Toupet laparoscopic fundoplication. Surg Endosc. 2002;16:758–66. doi: 10.1007/s00464-001-9092-8. [DOI] [PubMed] [Google Scholar]
- 31.Watson DI, Jamieson GG, Pike GK, et al. Prospective randomized double-blind trial between laparoscopic Nissen fundoplication and anterior partial fundoplication. Br J Surg. 1999;86:123–30. doi: 10.1046/j.1365-2168.1999.00969.x. [DOI] [PubMed] [Google Scholar]


