Abstract
Background
Well-differentiated thyroid carcinoma has a favorable prognosis, but patients with multiple recurrences have drastically lower survival. Filipinos in the US are known to have high thyroid cancer incidence and recurrence rates. It is unknown whether Filipinos also have higher thyroid cancer mortality rates.
Methods
We studied thyroid cancer mortality in Filipino, non-Filipino Asian (NFA), and non-Hispanic White (NHW) adults using US death records (2003–2012) and US Census data. Age-adjusted mortality rates (AMRs) and proportional mortality ratios (PMRs) were calculated. Gender, nativity status, age at death, and educational attainment were also examined.
Results
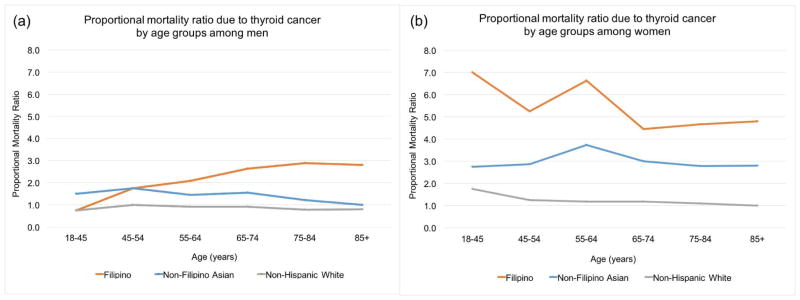
We examined 19,940,952 deaths. AMR due to thyroid cancer was highest in Filipinos (1.72 deaths per 100,000, 95% CI 1.51–1.95) compared to NFAs (1.03 per 100,000, 95% CI 0.95–1.12) and NHWs (1.17 per 100,000, 95% CI 1.16–1.18). Compared to NHWs, higher proportionate mortality was observed in Filipino women (3–5 times higher) across all age groups, and Filipino men had 2–3 times higher PMR in the subgroup over the age of 55. Filipinos that completed higher education had notably higher PMR (5.0) than their counterparts who had not (3.5).
Conclusions
Negative prognostic factors for thyroid cancer traditionally include “age greater than 45 years” and “male gender.” We demonstrate that Filipinos die of thyroid cancer at higher rates than NFAs and NHWs of similar ages. Highly-educated Filipinos and Filipino women may be especially at risk for poor thyroid cancer outcomes. Filipino ethnicity should be factored into clinical decision-making in the management of thyroid cancer.
Keywords: thyroid carcinoma, thyroid cancer, mortality, Filipino, Philippines, Asian Continental Ancestry Group, prognosis, clinical decision-making, female, health status disparities
Precis
Identifying demographic indicators of poor prognosis in thyroid cancer is vital to effective, personalized clinical decision-making. After analysis of approximately 19 million death records, we show that Filipinos die at a higher age-adjusted rate and have higher proportionate mortality than non-Filipino Asians and non-Hispanic Whites.
Introduction
Major prognostic factors considered for thyroid cancer are age, tumor size, multifocal disease, extra-thyroidal extension, and distant metastases1. Despite a large body of literature showing that people of Filipino heritage (hereafter, Filipinos), have increased thyroid cancer incidence2–6, few studies have examined whether Filipinos also have higher thyroid cancer mortality rates compared to other racial/ethnic groups
With a population of 3.4 million as of 2010, Filipinos are the second largest Asian population in the United States (US), and make up almost 20% of all Asian Americans7. Most cancer databases group all Asian subgroups together for data collection and analyses. This type of grouping can mask disparities, lead to a dearth of information regarding specific subgroups, and limit evidence-based cancer control, prevention, and intervention measures within these diverse populations8.
Recent work by Kus, et al. showed that Filipinos in Canada have a significantly increased risk of thyroid cancer recurrence compared to all other racial/ethnic groups even when adjusting for confounding factors such as gender, age, history of head and neck radiation therapy, and type of thyroid surgery (odds ratio 6.99, 95% CI 2.31–21.1). In the same study, 5.6% of the Filipino cohort died of thyroid cancer versus 1.9% of the non-Filipino cohort, a result that was not statistically significant, likely due to the relatively small sample size (N=499) and the difficulty of studying mortality in a disease with favorable prognosis9. A retrospective analysis performed at the Philippines General Hospital also found a higher recurrence rate among Filipinos (30.1%) as compared to Korean (17.5%) and Japanese (9.6%) populations studied by other research groups4. It remains unclear whether the higher recurrence rate observed in Filipinos also leads to a difference in mortality due to thyroid cancer in the United States.
Individuals diagnosed with well-differentiated thyroid carcinoma are considered to have an excellent prognosis, but a subgroup of patients experience multiple treatment failures and/or thyroid cancer recurrences. These individuals have significantly higher rates of death from the disease compared to those with one or no treatment failures (60% twenty-year-disease-specific-survival versus 94–100%, respectively) 10. Preemptive identification of individuals who are more likely to die from thyroid cancer based on demographic characteristics such as racial/ethnicity is imperative to helping clinicians create effective customized treatment and monitoring plans.
We used ten years of national mortality data to examine age-adjusted mortality rates (AMR) and proportional mortality ratios (PMR) due to thyroid cancer in Filipinos compared to non-Filipino Asians (NFAs) and non-Hispanic Whites (NHWs) with the hypothesis that AMR and PMR would be higher in Filipinos. To our knowledge, this is the first study to use national mortality data to evaluate death due to thyroid cancer in Filipinos in the US. Findings from our study will inform clinical management guidelines and empower clinicians and policy makers to bridge the gap in thyroid cancer outcomes for Filipinos.
Methods
Study Population
Causes of death, racial/ethnicity, and gender were identified using the Multiple Cause Mortality Files of the National Center for Health Statistics (NCHS) from 2003 to 2012. This database includes the 10th revision International Classification of Diseases (ICD-10) codes for both the underlying cause of death and up to 20 relevant conditions. ICD-10 codes were mapped into 260 categories using the Clinical Classifications Software (CCS), a tool developed at the Agency for Healthcare Research and Quality (AHRQ) for clustering patient diagnoses into clinically meaningful categories. Death due to thyroid cancer was defined as having CCS code 36 (i.e., “Cancer of Thyroid) as the underlying cause of death or as one of the 20 conditions. Decedents who were 18 years or older at time of death were selected. Cancer deaths were defined using ICD-10 code C00–C97 from all conditions.
Decedent characteristics consisted of racial/ethnic group (i.e., Filipinos, Non-Filipino Asians, and Non-Hispanic Whites), number of deaths due to any cancer or thyroid cancer alone, median and mean age at death, percentage of females, percent foreign born, and educational attainment. Educational attainment was classified into 5 categories from both the 2003 and 1989 revisions, considering different states adopted different revisions. The categorizations were: no formal education, high school or GED completed, some college, bachelor’s degree or higher, and unknown. To assess statistical significance, chi-squared tests were used for categorical vairables, and analysis of variance (ANOVA) tests were used for continuous variables. Differences between medians were assessed using the Wilcoxon rank sum test (Mann-Whitney U test).
Age at death was categorized into one of the following six age groups: 18–44, 45–54, 55–64, 65–74, 75–84, and 85+ years. A decedent’s nativity status was defined as “US-born” if the decedent was born within the 50 states or Washington D.C., and as “foreign-born” if the decedent was born outside of the United States or in one of the US territory islands (i.e., Puerto Rico, Virgin Islands, Guam, American Samoa, and Northern Marianas).
Statistical Analysis
Thyroid cancer AMRs per 100,000 were calculated using direct standardization to the 2000 US standard population, and were compared across racial/ethnic groups by gender. Population estimates were derived using linear interpolation from 2000 and 2010 US Census data. The proportions of deaths due to any cancer and thyroid cancer alone were calculated for each racial/ethnic group. The proportional mortality ratio (PMR) was defined as the proportion of deaths due to thyroid cancer in a specified racial/ethnic group divided by the proportion of deaths due to thyroid cancer for all NHWs (i.e., men and women combined). PMRs were compared across racial/ethnic groups by nativity and educational attainment (collapsed into the two categories “no bachelor’s degree” and “bachelor’s degree or higher”), as well as for each combination of age group and gender. For AMRs, we reported p-values for pairwise differences (i.e., Filipino vs. NFA, NFA vs. NHW and NHW vs. Filipino), overall and by gender. For PMRs, we reported p-values for testing whether the PMRs in specific groups were different from the PMR of all NHWs (see Supplementary Material 3). Thyroid cancer mortality (i.e., AMR and the proportion of deaths due to thyroid cancer) was reported for other Asian subgroups as a sensitivity analysis in Supplementary Table 1.
All analyses were performed in R and SAS (version 9.4), and statistical tests were based on two-sided tests with a significance level of 0.05 unless otherwise noted. P-values and confidence intervals corresponding to the a-priori hypotheses that the AMR and PMR of Filipinos are different from (i.e., higher than) those of NFAs and NHWs are confirmatory findings. All other p-values and confidence intervals (e.g. from analyzing subgroups such as by gender or age) are exploratory in nature and should be confirmed in follow-up studies.
Results
We examined 19,940,952 US death records from 2003 to 2012. The number of total deaths, deaths due to any cancer, deaths due to thyroid cancer, and average annual population estimates are presented by racial/ethnic group in Table 1. Demographic information (i.e., age at death, gender, nativity status, and educational attainment) is also presented in Table 1. Both median and mean age of death were not meaningfully different between Filipinos and the referent groups. Compared to NFA and NHW decedents, more Filipinos were foreign-born (90.2% versus 76.0% and 6.1%, respectively). Filipino decedents also had higher educational attainment than other racial/ethnic groups: 32.3% had obtained a Bachelor’s degree or higher versus 22.3% of NFAs and 14.6% of NHWs (Table 1). Percentages of deaths due to cancer were similar across all groups. The percentage of deaths due to thyroid cancer was 0.31% in Filipinos, which was 1.8 and 3.9 times higher than NFAs (0.17%) and NHWs (0.08%), respectively.
Table 1.
Decedent characteristics for Filipinos and reference populations, Non-Filipino Asian and Non-Hispanic White, 2003–2012.
| Decedent characteristics | Filipino | Non-Filipino Asian | Non-Hispanic White |
|---|---|---|---|
| Total deaths | 85,821 | 364,926 | 19,490,205 |
| Deaths due to cancer | 25,148 (29.3) | 108,951 (29.9) | 5,041,314 (25.9) |
| Deaths due to thyroid cancer (%) | 267 (0.31) | 623 (0.17) | 15,398 (0.08) |
| Avg. annual population* | 1,901,612 | 8,168,174 | 155,457,164 |
| Median age at death (IQR) | 75 (63, 84) | 76 (62, 85) | 79 (66, 87) |
| Mean age at death (SD) | 72.4 (16.1) | 72.1 (17.3) | 75.4 (15.7) |
| Female (%) | 42204 (49.2) | 174466 (47.8) | 9966886 (51.1) |
| Foreign born (%) | 77,431 (90.2) | 277,244 (76.0) | 1,193,627 (6.1) |
| Educational attainment (%) | |||
| No formal education | 20,773 (24.2) | 107,505 (29.5) | 4,531,882 (23.3) |
| High school or GED completed | 19,829 (23.1) | 117,417 (32.2) | 8,285,975 (42.5) |
| Some college | 16,103 (18.8) | 44,764 (12.3) | 3,087,613 (15.8) |
| Bachelor’s degree or higher | 27,641 (32.2) | 81,346 (22.3) | 2,839,034 (14.6) |
| Unknown | 1,475 (1.7) | 13,894 (3.8) | 745,701 (3.8) |
Average annual population data was based on 2000 and 2010 Census population for the study period.
Note: All characteristics were statistically significantly different (p<0.0001) across all groups.
The following AMR and PMR results are reported in Table 2. Overall, PMR due to thyroid cancer tended to be higher in foreign-born populations (see Table 2). PMR due to thyroid cancer was 4.1 in foreign-born Filipinos and 2.6 in US-born Filipinos. Foreign-born NFAs had a PMR of 2.3 versus US-born counterparts, who had a PMR of 1.8. Compared to NFAs and NHWs, Filipinos had the highest thyroid-cancer AMR of 1.72; the AMR for NFAs was 1.03 for NFAs, and was 1.17 for NHWs. Filipinos who had completed a Bachelor’s degree or higher had a notably higher PMR (5.0) than Filipinos who had not (3.5). Similarly, NHWs who had completed a Bachelor’s degree or higher also had a notably higher PMR (1.5) than NHWs who had not (0.9). Filipinos of any education status nevertheless had the highest PMRs of all comparison groups.
Table 2.
Age-adjusted mortality rate and proportional mortality ratio due to thyroid cancer by gender, nativity status, and educational attainment.
| Filipino | Non-Filipino Asian | Non-Hispanic White | |
|---|---|---|---|
| Age-adjusted mortality rate*, per 100,000 people | |||
| Total | 1.72 (1.51, 1.95) | 1.03 (0.95, 1.12) | 1.17 (1.16, 1.18) |
| Male | 1.57 (1.25, 1.95) | 0.76 (0.66, 0.88) | 0.83 (0.81, 0.85) |
| Female | 1.83 (1.56, 2.13) | 1.22 (1.11, 1.35) | 1.44 (1.41, 1.46) |
| Pairwise P-Value of age-adjusted mortality rate | Filipino vs. NFA | NFA vs. NHW | NHW vs. Filipino |
| Total | <0.0001 | 0.0013 | <0.0001 |
| Male | <0.0001 | 0.12 | <0.0001 |
| Female | <0.0001 | 0.0005 | 0.0014 |
| Proportional mortality ratio* | |||
| Total | 3.94 (3.49, 4.44) | 2.16 (1.99, 2.34) | 1 |
| Foreign-born | 4.09 (3.61, 4.63) | 2.27 (2.08, 2.49) | 1.14 (1.07, 1.21) |
| US-born | 2.56 (1.59, 4.13) | 1.80 (1.51, 2.15) | 0.99 (0.97, 1.01) |
| No Bachelor’s degree | 3.46 (2.95, 4.05) | 2.11 (1.92, 2.31) | 0.93 (0.91, 0.95) |
| Bachelor’s degree or higher | 5.04 (4.18, 6.08) | 2.33 (1.99, 2.74) | 1.47 (1.42, 1.53) |
| P-value of proportional mortality ratio | |||
| Total | <0.0001 | <0.0001 | - |
| Foreign-born | <0.0001 | <0.0001 | <0.0001 |
| US-born | <0.0001 | <0.0001 | 0.17 |
| No Bachelor’s degree | <0.0001 | <0.0001 | <0.0001 |
| Bachelor’s degree or higher | <0.0001 | <0.0001 | <0.0001 |
95% confidence intervals presented within parentheses.
Note: Referent population for proportional mortality ratio was all Non-Hispanic Whites.
PMR by racial/ethnic group and age group (separated by gender) is illustrated in Figure 1. Among men, PMRs for Filipinos were similar to those of comparison groups when younger (18- to 64-years-old at death), and about two to three times higher when older (>64 years) (Figure 1a). Among women, Filipinos had the highest PMRs at every age, and NHWs had the lowest PMRs at every age (Figure 1b). Filipino women had higher PMRs than Filipino men at all ages. For Filipinos, the female PMR was about seven, three, and two times the male PMR for decedents younger than 45-years-old, those 45–64-years-old, and those 64-years-old or older at death, respectively.
Figure 1. Proportional mortality ratios (PMRs) due to thyroid cancer, by gender and age group Caption.
(a) PMRs by age group for Filipino, non-Filipino Asian, and non-Hispanic white men, and (b) women. Older Filipino men have higher PMR compared to other men. At all ages, Filipino women have a much higher PMR than the comparison groups. PMR is defined as the proportion of deaths due to thyroid cancer in a specified racial/ethnic/gender group divided by the proportion of deaths due to thyroid cancer for all NHWs.
Other findings by racial/ethnic group and age group are reported as follows. NFA women also had higher PMRs than NFA men at all ages. NHW women younger than 45-years-old at death had higher PMRs than all NHW men, but PMRs were similar between NHW women and men at older ages (results not shown). As expected, the total number of deaths due to thyroid cancer in individuals younger than 45-years-old was small (see Supplementary Table 2).
In summary, Filipino racial/ethnicity is associated with higher rates of death from thyroid cancer, even when adjusted for age. Among all Filipino decedents, having been highly educated or a woman corresponded with particularly high proportionate mortality compared to all other groups. In supplementary sensitivity analysis (Supplementary Table 1), we did not find any comparable disparities in mortality outcomes among other disaggregated Asian-American subgroups (i.e. Asian Indian, Chinese, Japanese, Korean, and Vietnamese).
Of note, due to the large sample sizes involved in our analysis, we expected most p-values to be very small, thereby providing statistical evidence that a difference exists. However, statistical significance does not imply scientific importance. In fact, findings with large p-values might be more informative in this setting; they could indicate that the true difference, if it exists, is perhaps so small as to not be detectable even with a sample as large as ours.
Discussion
Why Filipinos?
The mechanism behind increased disease recurrence rates in Filipino thyroid cancer patients remains unclear, but past studies have theorized that cultural factors, such as diet, or environmental exposures are responsible for the higher incidence of thyroid cancer in Filipinos 3,11,12. Studies examining diet and thyroid cancer outcome are scarce. Post-thyroidectomy thyroid cancer patients are often placed on low-iodine diets before radioactive iodine (RAI) treatment in order to enhance I-131 uptake and maximize the destruction of cancerous thyroid cells13. One study found that among a cohort of Korean females, approximately 37% did not know that fish pastes, hams, and sausages contained high levels of iodine, and 36% over-estimated the amount of dairy they were allowed to consume on a low-iodine diet14. It is plausible that Filipino patients have similar misunderstandings and a higher intake of iodine-rich foods, such as seafood and dairy, than other patients preparing for RAI treatment, which may render the treatment less effective, or may modulate tumor behavior.
We did not identify a scientific difference in proportionate mortality between foreign-born Filipinos and their US counterparts. This makes environmental exposures present in the Philippines, such as carcinogenic volcanic lava11,15, unlikely to explain the differential outcomes we observed.
Filipinos had higher educational attainment than other comparison groups in our study, and highly-educated Filipinos had higher proportionate mortality due to thyroid cancer. Many Filipino immigrants who arrived to the US in the 1970s and 80s were health professionals16. Up until the mid-1980s Filipino nurses represented 75 percent of all foreign nurses in the U.S. nurse workforce17. Consequently, it is possible that occupational exposures within hospitals, such as radiation, could be leading to disproportionately worse outcomes within this population. A retrospective chart review by Seaberg et al. found that patients who had prior radiation exposure, including both acute high-dose and chronic low-dose exposure, had a higher percentage of multifocal disease, extrathyroidal spread, stage IV disease, and death18. Conversely, other studies have not found any relationship between prior radiation exposure and clinical outcome19–22. Higher education may be a proxy for other factors that influence clinical outcome, such as an exposure specific to a generation of immigrants, different approaches to accessing healthcare, or other behavioral habits.
Perhaps the most plausible explanation for the differential thyroid cancer outcomes observed in Filipinos is the existence of genetic predisposition in the host and/or tumor. Recent work by the Cancer Genome Atlas Research Network has drastically increased our understanding of the genetic basis of thyroid cancer behavior23. Alterations and gene expression patterns of specific genes (i.e. TERT, CHEK2, and ATM) and sets of functionally-related genes have been shown to define clinical sub-classes of thyroid cancer and may contribute to loss of differentiation and tumor progression23. For example, TERT promoter mutations and increased expression of a specific microRNA (miR-21) were linked to aggressive forms of papillary thyroid carcinoma. Filipinos may carry an allele that predisposes them as a population to the somatic mutations that drive thyroid tumor aggressiveness.
Gender and Prognosis
Within both Filipinos and NFAs, women had higher PMRs than men at all ages. Filipino women had especially high proportionate mortality compared to other racial/ethnic/gender groups at all ages. Given the gender differences we observe in this study, it is plausible that an X-linked allele could be predisposing Filipino women to more aggressive thyroid cancer. Our findings differ from the popularly-held belief that men have poorer outcomes when diagnosed with thyroid cancer 24. Of note, many of these studies analyzed patient cohorts from single medical institutions outside of the US. For example, Ito et al. found that Japanese men with thyroid cancer died from the disease at greater than twice the rate as compared to women (hazard ratio of 2.88 for cause-specific survival) 24. Lin et al found that among Chinese patients with distant metastases who died of thyroid cancer, older patients and men represented a larger percentage25. Conversely, a later study by Ito, et al. found that male gender did not predict death26.
Study Limitations
The volume of individuals included in ten years of US death records allowed us to feasibly examine age-adjusted mortality rates and proportional mortality due to thyroid cancer, a disease with a low overall mortality rate. As expected, the number of individuals younger than 45-years-old who died of thyroid cancer was small (Supplementary Table 2). Thus, it is unclear whether the PMR we estimated for this population is robust. However, the number of decedents in our sample was are sufficiently large to examine many important strata such as the older age groups, sex, educational attainment and nativity
Other limitations of our study include using data based on national death certificates, which may misclassify racial/ethnicity27 and contain errors in the documented cause of death 28. A recent study reported that misclassification may account for up to 3% of the US death certificates for Asian or Pacific Islanders29. Census data also exhibit misclassification of racial/ethnicity which may have affected age-adjusted mortality rates30. Nonetheless, racial/ethnicity reporting by the US Census is based on self-report, which is the gold standard. One of the advantages of the proportionate mortality (PMR) approach is that a single data source is used (death records only) rather than both data sources, which may minimize the effects of racial/ethnicity misclassification.
Estimates of the frequency of incorrect diagnoses have been highly variable given that there is no gold standard (i.e. actual cause of death) with which to compare a reported cause of death28. Past studies have shown that there is greater reliability in cause-of-death reporting when studying cancer compared to other causes of death 28.
Our approach is also limited by dependence on ICD-10 diagnostic coding, which does not differentiate histopathological sub-types of thyroid cancer. A study based on Surveillance, Epidemiology, and End Results 13-Registry Database (SEER) data found that 85% of thyroid cancer diagnosed in the US from 1992–2006 was papillary thyroid carcinoma. The same study observed that Asians in the US had the highest incidence rate of papillary carcinoma as compared to other racial/ethnicity groups. Racial/ethnic differences in the incidence of anaplastic thyroid cancer, the subtype with the worst prognosis, was less pronounced but highest in Hispanics and Asians 31. The study did not disaggregate Filipinos from other Asians. Given this information, the majority of deaths due to thyroid cancer were likely due to papillary carcinoma or anaplastic thyroid cancer, though due to the limitations of ICD-10 coding, we were unable to study racial/ethnic differences by histopathological subtype.
We accounted for confounding by age through age-adjustment in calculating AMRs, and by gender, nativity status, and educational attainment by making stratified comparisons of AMR (see Table 2). However, we could not account for a few other potential confounders of mortality, such as stage at diagnosis, age at diagnosis, type of cancer treatment (i.e. extent of thyroidectomy and neck dissection, RAI), socioeconomic status, level of acculturation, or occupational and environmental exposures, given our use of death-certificate data. Information related to diet and environmental exposures (i.e. radiation) were also not available to help inform potential explanations for differences in outcome.
Future Steps
Future studies of thyroid cancer prognosis should include Filipino ethnicity, separate from other Asians and Pacific Islanders, to further validate our findings in different cohorts and richer cancer databases.
To investigate pathophysiology, future studies should also examine whether aggressive histopathological subtypes, such as anaplastic thyroid cancer or tall cell variant PTC, and genetic alterations associated with thyroid de-differentiation and tumor progression, such as TERT promoter mutations, are more common in thyroid cancers surgically removed from Filipinos. Genetic epidemiology studies should investigate whether Filipinos as a population carry a higher proportion of any specific allele that predisposes them to aggressive thyroid tumors. Investigations of this sort would provide invaluable information on the pathophysiology of aggressive thyroid cancer, could support clinical decision-making, and could lead to more targeted thyroid cancer treatment plans for this population.
Conclusions
Filipinos represent approximately 20% of the Asian-American population in the US7, and approximately 10.2 million Filipinos live and work outside of the Philippines worldwide32. Despite convincing evidence that Filipinos have higher incidence of thyroid cancer and worse outcomes when diagnosed with thyroid cancer, no clinical guidelines include Filipino ethnicity as a potential prognostic factor. Our analysis suggests that Filipino ethnicity is associated with higher rates of death from thyroid cancer independent of age. Filipino women, in particular, may be at higher proportionate risk of death from thyroid cancer. We hope that our findings will better inform and empower researchers, clinicians, prevention specialists, and policy makers to bridge the gap in thyroid cancer outcomes for Filipinos.
Supplementary Material
Acknowledgments
Funding Sources: This work was supported by the National Institute on Minority Health and Health Disparities (R01 MD007012 CAUSES: Causes of Asian American Mortality Understood by Socio-Economic Status) and the Stanford University School of Medicine Medical Scholars Program.
Footnotes
Author Disclosure Statement: No competing financial interests exist.
Authors’ Contributions: M-L.T. Nguyen: lead conceptualization, equal methodology, equal project administration, lead writing -- original draft, equal visualization, equal funding acquisition; J Hu: supporting conceptualization, equal methodology, lead software, lead verification, lead data curation, lead formal analysis, equal visualization, supporting writing -- original draft; K.G. Hastings: equal project administration, supporting conceptualization, supporting writing – review & editing; E.J. Daza: supporting conceptualization, equal methodology, supporting visualization, supporting writing – review & editing; M.R. Cullen: supporting supervision, supporting writing – review & editing; L.A. Orloff: supporting conceptualization, supporting supervision, supporting funding acquisition; L.P. Palaniappan: lead supervision, supporting methodology, supporting verification, supporting visualization, supporting writing – review & editing, equal funding acquisition.
References
- 1.Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clark JR, Eski SJ, Freeman JL. Risk of malignancy in Filipinos with thyroid nodules—A matched pair analysis. Head Neck. 2006;28(5):427–431. doi: 10.1002/hed.20333. [DOI] [PubMed] [Google Scholar]
- 3.Haselkorn T, Bernstein L, Preston-Martin S, Cozen W, Mack WJ. Descriptive epidemiology of thyroid cancer in Los Angeles County, 1972–1995. Cancer Causes Control CCC. 2000;11(2):163–170. doi: 10.1023/a:1008932123830. [DOI] [PubMed] [Google Scholar]
- 4.Lo TEN, Uy AT, Maningat PDD. Well-Differentiated Thyroid Cancer: The Philippine General Hospital Experience. Endocrinol Metab. 2016;31(1):72. doi: 10.3803/EnM.2016.31.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Horn-Ross PL, McClure LA, Chang ET, et al. Papillary thyroid cancer incidence rates vary significantly by birthplace in Asian American women. Cancer Causes Control. 2011;22(3):479–485. doi: 10.1007/s10552-010-9720-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gomez SL, Noone A-M, Lichtensztajn DY, et al. Cancer Incidence Trends Among Asian American Populations in the United States, 1990–2008. JNCI J Natl Cancer Inst. 2013;105(15):1096–1110. doi: 10.1093/jnci/djt157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoeffel Elizabeth M, Rastogi Sonya, Kim Myoung Ouk, Shahid Hasan. The Asian Population: 2010. United States Census Bureau; 2012. [Accessed April 19, 2017]. https://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf. [Google Scholar]
- 8.Martin DN, Lam TK, Brignole K, et al. Recommendations for Cancer Epidemiologic Research in Understudied Populations and Implications for Future Needs. Cancer Epidemiol Biomarkers Prev. 2016;25(4):573–580. doi: 10.1158/1055-9965.EPI-15-1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kus LH, Shah M, Eski S, Walfish PG, Freeman JL. Thyroid Cancer Outcomes in Filipino Patients. Arch Otolaryngol Neck Surg. 2010;136(2):138. doi: 10.1001/archoto.2009.206. [DOI] [PubMed] [Google Scholar]
- 10.Palme CE, Waseem Z, Raza SN, Eski S, Walfish P, Freeman JL. Management and Outcome of Recurrent Well-Differentiated Thyroid Carcinoma. Arch Otolaryngol Neck Surg. 2004;130(7):819. doi: 10.1001/archotol.130.7.819. [DOI] [PubMed] [Google Scholar]
- 11.Spitz MR, Sider JG, Katz RL, Pollack ES, Newell GR. Ethnic patterns of thyroid cancer incidence in the United States, 1973–1981. Int J Cancer. 1988;42(4):549–553. doi: 10.1002/ijc.2910420413. [DOI] [PubMed] [Google Scholar]
- 12.Rossing MA, Schwartz SM, Weiss NS. Thyroid cancer incidence in Asian migrants to the United States and their descendants. Cancer Causes Control CCC. 1995;6(5):439–444. doi: 10.1007/BF00052184. [DOI] [PubMed] [Google Scholar]
- 13.Li JH, He ZH, Bansal V, Hennessey JV. Low iodine diet in differentiated thyroid cancer: a review. Clin Endocrinol (Oxf) 2016;84(1):3–12. doi: 10.1111/cen.12846. [DOI] [PubMed] [Google Scholar]
- 14.Moon J-A, Yoo C-H, Kim MH, et al. Knowledge, Self-Efficacy, and Perceived Barriers on the Low-Iodine Diet among Thyroid Cancer Patients Preparing for Radioactive Iodine Therapy. Clin Nutr Res. 2012;1(1):13. doi: 10.7762/cnr.2012.1.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cho YA, Kim J. Dietary Factors Affecting Thyroid Cancer Risk: A Meta-Analysis. Nutr Cancer. 2015;67(5):811–817. doi: 10.1080/01635581.2015.1040517. [DOI] [PubMed] [Google Scholar]
- 16.Naylor L. Cultural Diversity in the United States. Greenwood Publishing Group; 1997. [Google Scholar]
- 17.Brush BL, Sochalski J, Berger AM. Imported Care: Recruiting Foreign Nurses To U.S. Health Care Facilities. Health Aff (Millwood) 2004;23(3):78–87. doi: 10.1377/hlthaff.23.3.78. [DOI] [PubMed] [Google Scholar]
- 18.Seaberg RM, Eski S, Freeman JL. Influence of Previous Radiation Exposure on Pathologic Features and Clinical Outcome in Patients With Thyroid Cancer. Arch Otolaryngol Neck Surg. 2009;135(4):355. doi: 10.1001/archoto.2009.13. [DOI] [PubMed] [Google Scholar]
- 19.Furlan J, Rosen I. Prognostic relevance of previous exposure to ionizing radiation in well-differentiated thyroid cancer. Langenbecks Arch Surg. 2004;389(3) doi: 10.1007/s00423-003-0424-0. [DOI] [PubMed] [Google Scholar]
- 20.Rubino C, Cailleux A-F, Abbas M, et al. Characteristics of Follicular Cell-Derived Thyroid Carcinomas Occurring After External Radiation Exposure: Results of a Case Control Study Nested in a Cohort. Thyroid. 2002;12(4):299–304. doi: 10.1089/10507250252949423. [DOI] [PubMed] [Google Scholar]
- 21.Samaan NA, Schultz PN, Ordonez NG, Hickey RC, Johnston DA. A Comparison of Thyroid Carcinoma in Those Who Have and Have Not Had Head and Neck Irradiation in Childhood*. J Clin Endocrinol Metab. 1987;64(2):219–223. doi: 10.1210/jcem-64-2-219. [DOI] [PubMed] [Google Scholar]
- 22.Zielinski J, Garner M, Band P, et al. Health outcomes of low-dose ionizing radiation exposure among medical workers: a cohort study of the Canadian national dose registry of radiation workers. Int J Occup Med Environ Health. 2009;22(2) doi: 10.2478/v10001-009-0010-y. [DOI] [PubMed] [Google Scholar]
- 23.Agrawal N, Akbani R, Aksoy BA, et al. Integrated Genomic Characterization of Papillary Thyroid Carcinoma. Cell. 2014;159(3):676–690. doi: 10.1016/j.cell.2014.09.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ito Y, Miyauchi A. Prognostic factors and therapeutic strategies for differentiated carcinomas of the thyroid. Endocr J. 2009;56(2):177–192. doi: 10.1507/endocrj.k08e-166. [DOI] [PubMed] [Google Scholar]
- 25.Lin J-D, Hsueh C, Chao T-C. Long-Term Follow-Up of the Therapeutic Outcomes for Papillary Thyroid Carcinoma With Distant Metastasis. Medicine (Baltimore) 2015;94(26):e1063. doi: 10.1097/MD.0000000000001063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ito Y, Kudo T, Kobayashi K, Miya A, Ichihara K, Miyauchi A. Prognostic Factors for Recurrence of Papillary Thyroid Carcinoma in the Lymph Nodes, Lung, and Bone: Analysis of 5,768 Patients with Average 10-year Follow-up. World J Surg. 2012;36(6):1274–1278. doi: 10.1007/s00268-012-1423-5. [DOI] [PubMed] [Google Scholar]
- 27.Sorlie PD, Rogot E, Johnson NJ. Validity of demographic characteristics on the death certificate. Epidemiol Camb Mass. 1992;3(2):181–184. doi: 10.1097/00001648-199203000-00018. [DOI] [PubMed] [Google Scholar]
- 28.Institute of Medicine (US) Committee for the Workshop on the Medicolegal Death Investigation System. 8, MEDICOLEGAL DEATH INVESTIGATION, PUBLIC HEALTH, AND HEALTH CARE. Medicolegal Death Investigation System: Workshop Summary. Washington, D.C: National Academies Press; 2003. [Accessed May 16, 2017]. https://www.ncbi.nlm.nih.gov/books/NBK221918/ [PubMed] [Google Scholar]
- 29.Arias E, Heron M, Hakes J National Center for Health Statistics, US Census Bureau. The Validity of Race and Hispanic-origin Reporting on Death Certificates in the United States: An Update. Vital Health Stat. 2016;2(172):1–21. [PubMed] [Google Scholar]
- 30.Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age Standardization of Rates: A New WHO Standard. World Health Organization; 2001. [Google Scholar]
- 31.Aschebrook-Kilfoy B, Ward MH, Sabra MM, Devesa SS. Thyroid Cancer Incidence Patterns in the United States by Histologic Type, 1992–2006. Thyroid. 2011;21(2):125–134. doi: 10.1089/thy.2010.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Commission on Filipinos Overseas. Stock Estimate of Overseas Filipinos as of Dec. 2013. Office of the President of the Philippines; 2013. [Accessed April 26, 2017]. http://www.cfo.gov.ph/images/statistics/stock_estimate/2013-Stock-Estimate.xlsx. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.