Abstract
Objectives
This study looked to analyse the expression levels of microRNA-140-3p and microRNA-140-5p in synovial fluid, and their correlations to the severity of disease regarding knee osteoarthritis (OA).
Methods
Knee joint synovial fluid samples were collected from 45 patients with OA of the knee (15 mild, 15 moderate and 15 severe), ten healthy volunteers, ten patients with gouty arthritis, and ten with rheumatoid arthritis. The Kellgren–Lawrence grading (KLG) was used to assess the radiological severity of knee OA, and the patients were stratified into mild (KLG < 2), moderate (KLG = 2), and severe (KLG > 2). The expression of miR-140-3p and miR-140-5p of individual samples was measured by SYBR Green quantitative polymerase chain reaction (PCR) analysis. The expression of miR-140-3p and miR-140-5p was normalised to U6 internal control using the 2-△△CT method. All data were processed using SPSS software.
Results
Expression of both miR-140-3p and miR-140-5p was downregulated in OA synovial fluid, showing a statistical difference between the OA and non-OA group, and increased OA severity was associated with a decreased expression of miR-140-3p or miR-140-5p. The Spearman rank correlation analysis suggested that the expression of miR-140-3p or miR-140-5p was negatively correlated with OA severity. In addition, the expression of miR-140-5p was 7.4 times higher than that of miR-140-3p across all groups.
Conclusion
The dysregulation of miR-140-3p and miR-140-5p in synovial fluid and their correlations with the disease severity of OA may provide an important experimental basis for OA classification, and the miR-140-3p/miR-140-5p are of great potential as biomarkers in the diagnosis and clinical management of patients with OA.
Cite this article: C-M. Yin, W-C-W. Suen, S. Lin, X-M. Wu, G. Li, X-H. Pan. Dysregulation of both miR-140-3p and miR-140-5p in synovial fluid correlate with osteoarthritis severity. Bone Joint Res 2017;6:612–618. DOI: 10.1302/2046-3758.611.BJR-2017-0090.R1.
Keywords: Osteoarthritis, miR-140, Synovial fluid
Article focus
Expression of miR-140-3p and miR-140-5p is significantly reduced in chondrocytes in osteoarthritis (OA), while these miRNAs are highly expressed in uncultured articular chondrocytes.
Expression of miR-140-3p and miR-140-5p in synovial fluid from knee OA is still unclear.
The aim of this study was to assess the levels of miR-140-3p and miR-140-5p in SF from knee OA and their correlations to the severity of disease in knee OA.
Key messages
Expression of miR-140-3p and miR-140-5p was downregulated in SF from knee OA and there is a significant inverse correlation between the expression of these miRNAs and the severity of disease in knee OA.
The age of patients is correlated with the severity of knee OA; however, there is no correlation between age and the expression of miR-140-3p and miR-140-5p.
Intra-group analysis showed that the expression of miR-140-5p was 7.4 times higher than that of miR-140-3p across all groups.
Strengths and limitations
This study reports the expression profiles of miR-140-3p and miR-140-5p in synovial fluid from patients with OA of the knee with varying severity.
The findings provide important information that will improve the pathological diagnosis and should also help in the clinical management of patients with OA.
The detailed mechanisms leading to the discrepancy in miR140-3p and miR-140-5p expression in synovial fluid need further study.
Introduction
Osteoarthritis (OA) is associated with an age-related imbalance between degradation and repair of articular cartilage.1-3 This dysregulation induces senescence, differentiation, proliferation, and death of joint cells through gene and/or protein expression networks that switch from anabolic to catabolic outcomes.4 Micro-ribonucleic acid (miRNA) is essential for the maintenance of cellular functions through fine-tuning the expressions of multiple target genes.5 Both upregulation and downregulation of miRNAs have been associated with OA,6-8 and targeting these changes may have future clinical benefit. Alternatively, miRNA levels might also be used as biomarkers.9
Currently, OA is diagnosed pathologically, clinically, or radiologically, where it is graded on a five-level scale of joint space narrowing, sclerosis of the subchondral bone, and osteophyte and subchondral cyst formation.10,11 Due to a lack of early-stage diagnostic markers, delayed diagnosis of OA is common, which could affect the potential for preventing further disease progression. Therefore, finding a reliable and standardised diagnostic tool could increase the quality of life and treatment for patients with OA. Although systemic ‘metabolomic’ biomarkers of OA have already been identified in the urine and serum,12,13 the metabolite concentrations could be significantly altered in any joint in which there is difficulty in diagnosing OA. Measuring biomarkers in tissue fluids, such as synovial fluid (SF) of the knee, could provide more information about the condition of the diseased joint. They would be in higher concentrations than in blood or urine, giving a higher sensitivity and specificity.14,15 In addition, OA-specific biomarkers are likely to be detected earlier in SF samples compared with blood samples.16 In addition, as OA is defined as the degradation of cartilage and joint tissue, SF has real potential for further study because it is in direct contact with cartilage.
MicroRNA-140 (miR-140) is strongly expressed in the cartilage of developing zebrafish, medaka, and mice.17-19 Miyaki et al20 found that miR-140-/- mice showed age-related OA-like changes characterised by proteoglycan loss and fibrillation of articular cartilage, and by 12 months, miR-140-/- mice showed severe structural cartilage defects. They also showed that transgenic mice overexpressing miR-140 in cartilage were resistant to antigen-induced arthritis.20 This study demonstrated that miR-140 is a regulator of cartilage homeostasis, and changes in its expression and functions play an important role in diseases associated with cartilage destruction.
Nakamura et al21 found that miR-140 was located in one intron of the WW domain containing the E3 ubiquitin-protein ligase 2 (WWP2) gene. Analysis of the intronic sequence has revealed that there are two miR-140 variants: miR-140-3p and miR-140-5p. Although both miR-140-3p and miR-140-5p are transcribed from the same precursor transcript pre-miR-140, they have different seed sequences, and are predicted to target different genes.22 While miR-140-5p was shown to target several genes involved in OA, such as histone deacetylase 4 (HADC4),19 insulin-like growth factor-binding protein 5 (IGFBP5),23 and bone morphogenetic protein 2 (BMP2),24 miR-140-3p has been reported to target dynamin 1, which plays a role in the central nervous system,25 and the nuclear factor kappa B (NF-κB), which is a co-activator nuclear receptor-interacting protein.26 However, recent studies have shown that the expression levels of both miR-140-3p and miR-140-5p are markedly and significantly reduced in OA chondrocytes.22 In chondrogenically differentiated mesenchymal stem cells and uncultured articular chondrocytes, miR-140-3p and miR-140-5p were both highly expressed.27 These findings suggest that miR-140-3p and miR-140-5p are both essential for chondrogenesis and cartilage homeostasis, but whether miR-140-3p and miR-140-5p are expressed in the SF of knee OA remains unclear. We investigated the expression profile of both miR-140-3p and miR-140-5p in the SF from patients with various stages of primary knee OA. The aim of the study was to assess whether the SF levels of miR-140-3p and miR-140-5p correlated with the severity of the disease.
Materials and Methods
Research subjects
Informed consent was obtained from 75 patients (45 with OA, ten with gouty arthritis (GA), ten with rheumatoid arthritis (RA), and ten healthy volunteers). All primary OA patients met the American College of Rheumatology clinical symptomatic and radiographical criteria for OA.28 All of the RA patients were diagnosed based on the American Rheumatism Association (ARA) 1987 revised criteria.29 All of the GA patients met the 1977 preliminary ARA classification criteria for gout.30 All of the patients underwent weight-bearing anteroposterior radiographs to assess the structural changes of the diseased knee. Kellgren–Lawrence grading (KLG)31 was used to assess the radiological severity of the knee joint and were stratified into mild (< 2), moderate (= 2), or severe (> 2). Patients were excluded if they had secondary post-traumatic OA, systemic inflammatory or autoimmune disorders, previous knee injury or joint infection, or a history of corticosteroid medication.
Synovial fluid collection
SF samples were obtained from the diseased knee of patients via non-lavage arthrocentesis under sterile conditions. Once SF samples had been collected, they were transported immediately to the laboratory on ice and were centrifuged at 3000 × g for 15 minutes at 4°C. The supernatant was then stored in liquid nitrogen.
RNA extraction
300 μl aliquots of the SF sample were thawed on ice and 1.2 ml TRIzol (Invitrogen, Carlsbad, California) was added. 200 μl of chloroform was added to the SF, which was shaken vigorously for 20 seconds. The aliquot was incubated at room temperature for three minutes for the complete dissociation of nucleoprotein complexes and centrifuged at 10 000 × g for 15 minutes at room temperature. The aqueous phase, excluding the interphase, was transferred to a fresh tube and 10 μl of silicon dioxide (SiO2) adsorption liquid was added, mixed and centrifuged at 8000 × g for one minute. The supernatant was discarded and replaced with 400 μl 75% ethanol, followed by centrifugation at 8000 × g for one minute. The RNA pellet was air-dried for 15 minutes and dissolved in 30 μl RNase-free water at 55°C to 60°C for ten minutes. The RNA was stored at -80°C.
Reverse transcription and quantitation of miRNA real-time polymerase chain reaction (PCR)
The stem-loop method to target specific stem-loop reverse transcription primers that bind the three-inch portion of miRNA molecules and Moloney murine leukaemia virus (M-MLV) reverse transcriptase were used for complementary DNA (cDNA) synthesis by using reverse transcription. Employing SYBR Green qPCR SuperMix (Invitrogen), real-time PCR was carried out on an Applied Biosystems 7300 Real-time PCR System (Applied Biosystems, Tokyo, Japan). The expression of miR-140-3p and miR-140-5p was normalised to U6 internal control using the 2-ΔΔCT method.32 The sequences of the primers for miR-140-3p, miR-140-5p, and U6 small nuclear RNA (snRNA) used in this study are shown in Table I.
Table I.
Primer sequences and product sizes in quantitative PCR
| Target gene | Forward primer (5’-3’) | Reverse primer (5’-3’) | cDNA product size (base pair) | GenBank accession number |
|---|---|---|---|---|
| miR-140-3p | ACACTCCAGCTGGGAGGCGGGGCGCCGCGGGA | CTCAACTGGTGTCGTGGA | 71 | MIMAT0004597 |
| miR-140-5p | ACACTCCAGCTGGGAGGCGGGGCGCCGCGGGA | CTCAACTGGTGTCGTGGA | 72 | MIMAT0000431 |
| U6 | CTCGCTTCGGCAGCACA | AACGCTTCACGAATTTGCGT | 94 | N/A |
All procedures performed in this study were approved by the medical ethics committee of Shenzhen 8th People’s Hospital (Grant number: 20130201), and the consent to participate followed the ethical standards of the Chinese Institutional and National Research Committee, and the 1964 Helsinki Declaration and its later amendments. Informed consent was obtained from all participants included in the study.
Statistical analysis
Data are presented as the mean, standard deviation (sd), and range. All data were processed using SPSS software, version 13.0 (SPSS Inc., Chicago, Illinois). The Kolmogorov–Smirnov normality test (K–S test) was used to analyse the expression values of miR-140-3p and miR-140-5p. Log transformation was used for parametric analysis if the expression values did not show a normal distribution. Homogeneity of variance was analysed using the Levene test.33 Intra-group comparisons were carried out by using one-way analysis of variance (ANOVA) or multiple comparison tests (least significant difference) for homogeneous data, while Tamhane’s T2 test was applied if the data were heterogeneous. Correlations between miR-140-3p or miR-140-5p expression and OA severity were estimated using Spearman’s correlation. The Pearson correlation was used to examine the relationships between expression of miR-140-3p or miR-140-5p and age in varying severity of OA. A p-value of < 0.05 was considered statistically significant.
Results
General characteristics of the subjects
Ten SF samples were collected from each of the GA and RA patients, as well as the healthy volunteers. A total of 45 SF samples from OA patients were collected, of which 15 samples were from groups of differing severity of OA (mild, moderate and severe). The age, height, body weight, and body mass index (BMI) of subjects in each group, as well as the number of patients in each group, are shown in Table II. One-way ANOVA showed that there were no statistically significant differences in gender, height, body weight, and BMI among the different groups, but there was a statistically significant difference in age among the different groups (f = 3.73, p = 0.005).
Table II.
General characteristics of the subjects in each study group, presented as mean (sd; range)
| Group | Age, yrs | Height, cm | Weight, kg | Body mass index, kg/m2 |
|---|---|---|---|---|
| Control, n = 10 | 49.6 (8.82; 38 to 66) | 166 (6.32; 156 to 175) | 63.2 (6.12; 56.5 to 75) | 22.91 (1.39; 20.21 to 24.49) |
| GA, n = 10 | 50 (12.56; 34 to 66) | 165.9 (5.97; 156 to 176) | 64.55 (4.06; 58.5 to 70.5) | 23.49 (1.72; 20.73 to 26.9) |
| RA, n = 10 | 46.9 (12.75; 33 to 67) | 165.6 (7.65; 155 to 177) | 63.3 (8.63; 55.5 to 81) | 23.03 (2.12; 19.63 to 27.06) |
| Mild OA, n = 15 | 51.07 (9.31; 39 to 62) | 164.93 (7.03; 155 to 177) | 64.67 (5.66; 56.5 to 76.5) | 23.77 (1.44; 21.3 to 27.1) |
| Moderate OA, n = 15 | 58.00 (11.98; 41 to 81) | 163.93 (7.66; 155 to 178) | 62.53 (4.69; 56 to 74.5) | 23.32 (1.75; 19.41 to 26.5) |
| Severe OA, n = 15 | 63.2 (8.4; 52 to 80) | 163.8 (4.84; 156 to 172) | 63.47 (3.18; 58 to 68) | 23.69 (1.56; 21.3 to 27.59) |
Control, healthy volunteers; GA, arthritis due to gout; RA, rheumatoid arthritis; OA, osteoarthritis
miR-140-3p/miR-140-5p expression in the SF of each group
The expression of miR-140-3p/miR-140-5p was detected in the SF from all patients, and K-S tests showed that the relative expression quantity 2-ΔΔCT of miR-140-3p/miR-140-5p in the SF from each group was normally distributed. The Levene method showed that the variance of miR-140-3p/miR-140-5p expression in each group was not homogeneous (Tables III and IV). The result from Tamhane’s T2 test showed that there was significant statistical difference in the expression of miR-140-3p or miR-140-5p between the SF from OA and non-OA groups, while there was no difference among the GA, RA, and normal control groups (Table III). The non-OA groups and normal control group, respectively, showed a 9.6-fold and 11.4-fold greater expression of miR-140-3p and a 7.9-fold and 9.4-fold greater expression of miR-140-5p than OA groups. Increased OA severity was associated with a decreased expression of miR-140-3p/miR-140-5p.
Table III.
The expression of miR-140-3p/miR-140-5p in SF of each group, presented as mean (sd; range)
| Group | miR-140-3p | miR-140-5p |
|---|---|---|
| 2-ΔΔCT | 2-ΔΔCT | |
| Control | 1.07 (0.43; 0.59 to 1.972) | 1.08 (0.47; 0.624 to 1.879) |
| GA | 0.82 (0.24; 0.529 to 1.214) | 0.85 (0.25; 0.48 to 1.206) |
| RA | 0.86 (0.39; 0.308 to 1.464) | 0.8 (0.33; 0.382 to 1.24) |
| Mild OA | 0.274 (0.13; 0.086 to 0.54)* | 0.36 (0.275; 0.14 to 1)† |
| Moderate OA | 0.132 (0.086; 0.021 to 0.299)* | 0.173 (0.102; 0.09 to 0.356)‡ |
| Severe OA | 0.031 (0.019; 0.008 to 0.08)* | 0.036 (0.031; 0.013 to 0.117)* |
Significant difference in the marked group compared with the other groups
Significant difference in the marked group compared with the control, GA, RA, and severe OA groups
Significant difference in the marked group compared with the control, GA, RA, and severe OA groups, p < 0.05
ΔΔCT = [(CTmiR-140-3p/5p - CTU6)group - (CTmiR-140-3p/5p - CTU6)control], 2-ΔΔCT = log transformed ΔΔCT, the fold change in miR-140-3p or miR-140-5p expression normalised to U6 and relative to control
CT, threshold cycle; GA, arthritis due to gout; RA, rheumatoid arthritis; OA, osteoarthritis
Table IV.
Correlation between the expression of miR-140-3p and miR-140-5p in each group, presented as mean (sd; range)
| Group | ΔCT3p | ΔCT5p | ΔΔCT | 2-ΔΔCT |
|---|---|---|---|---|
| Control | 11.93 (0.55; 10.95 to 12.69) | 9.48 (0.58; 8.57 to 10.16) | -2.45 (0.75; 1 to 3.59) | 6.12 (3.02; 2 to 12.042) |
| GA | 12.28 (0.42; 11.65 to 12.85) | 9.78 (0.44; 9.21 to 10.54) | -2.5 (0.26; 2.04 to 2.97) | 5.74 (1.07; 4.11 to 7.84) |
| RA | 12.3 (0.71; 11.38 to 13.63) | 9.92 (0.65; 9.17 to 10.87) | -2.39 (0.59; 1.13 to 3.12) | 5.59 (2.03; 2.19 to 8.69) |
| Mild OA | 13.95 (0.69; 12.82 to 15.47)* | 11.27 (0.93; 9.48 to 12.32)* | -2.68 (0.97; 1.69 to 5.4) | 8.56 (9.78; 3.23 to 42.22) |
| Moderate OA | 15.2 (1.12; 13.67 to 17.53)† | 12.21 (0.75; 10.97 to 12.96)† | -2.99 (1.13; 0.73 to 4.63) | 10.38 (7.66; 1.66 to 24.76) |
| Severe OA | 17.16 (0.86; 15.57 to 18.87)‡ | 14.65 (1.03; 12.58 to 15.74)‡ | -2.51 (0.69; 1.85 to 4.63) | 6.63 (5.25; 3.61 to 24.76) |
Significant difference in the marked group compared with the control, GA, RA, and severe OA groups
Significant difference in the marked group compared with the control, GA, RA, and severe OA groups, p < 0.05
Significant difference in the marked group compared with the other groups
ΔCT3p = (CTmiR-140-3p - CTU6), ΔCT5p = (CTmiR-140-5p - CTU6), ΔΔCT = [(CTmiR-140-5p - CTU6) - (CTmiR-140-3p - CTU6)]], 2-ΔΔCT = log transformed ΔΔCT, the fold change in miR-140-5p expression normalised to U6 and relative to mR-140-3p
CT, threshold cycle; GA, arthritis due to gout; RA, rheumatoid arthritis; OA, osteoarthritis
Spearman rank correlation analysis was performed to study the correlation of miR-140-3p/miR-140-5p expression among the normal control group, mild OA group, moderate OA group and severe The rank correlation coefficient of miR-140-3p was r = -0.87 (p = 0.001), and the rank correlation coefficient of miR-140-5p was r = -0.899 (p = 0.001). With α = 0.05 as the level of significance, the expression of miR-140-3p/miR-140-5p was negatively correlated with severity of OA.
Correlation analysis of the expression of miR-140-3p/miR-140-5p and age
Scatter diagrams (Fig. 1) were drawn to illustrate the relative expression of miR-140-3p/miR-140-5p and age in the normal control, mild, moderate, and severe OA groups. As shown in the scatter diagrams, there were no significant linear correlations between age and the expression of miR-140-3p/miR-140-5p in SF. Pearson correlation analysis was further performed to investigate the correlation between miR-140-3p/miR-140-5p expression and age in the normal controls, mild, moderate, and severe OA. The results from Pearson correlation analysis showed that the Pearson correlation coefficient between miR-140-3p and age was r = -0.144 (p = 0.293), and that of miR-140-5p and age was r = -0.214 (p = 0.116), indicating that there was no linear correlation between age and the expression of miR-140-3p/miR-140-5p in SF.
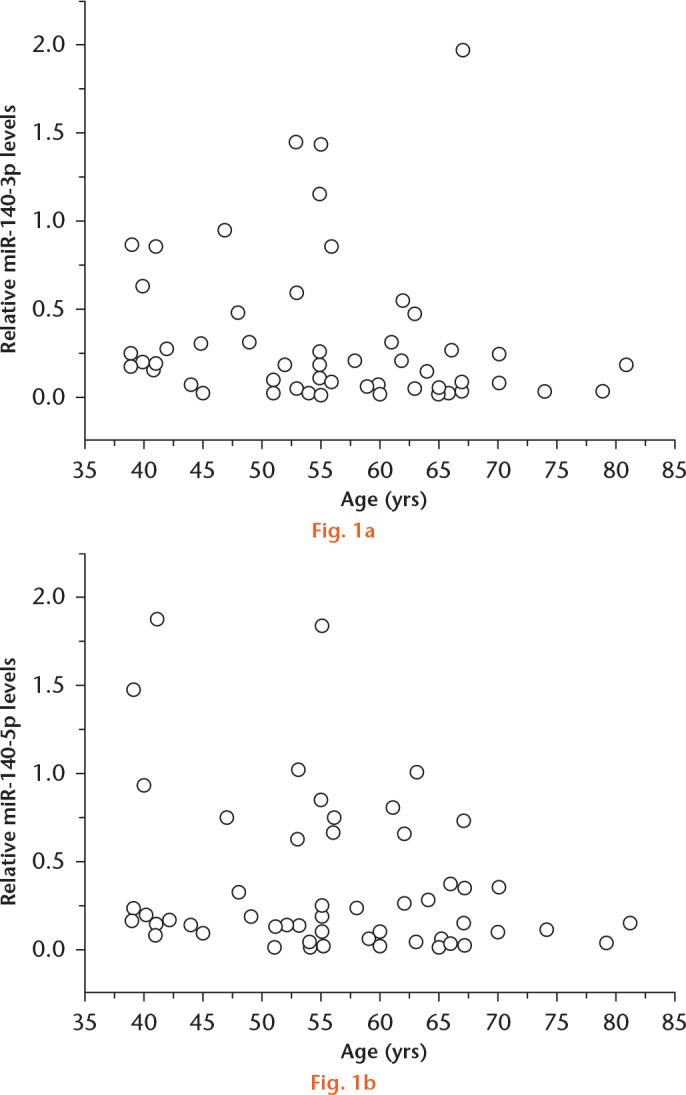
Scatter diagrams showing the correlation between the expression of a) miR-140-3p, b) miR-140-5p, and age. They were drawn for the relative expression of miR-140-3p/miR-140-5p and age in the normal controls, mild, moderate and severe osteoarthritis. As shown in the scatter diagram, there was no significant linear correlation between age and the expression of miR-140-3p/miR-140-5p in synovial fluid.
Correlation analysis of the expression of miR-140-3p/miR-140-5p in each group
Analysis of the intra-group relative expression of miR-140-3p/miR-140-5p showed that there was statistical difference in the expression of miR-140-3p/miR-140-5p in SF from the same group (Table IV), and the expression of miR-140-5p was 7.4 times higher than that of miR-140-3p across all groups. One-way ANOVA showed that the fold change of miR-140-3p/miR-140-5p expression across groups was not statistically significant (f = 1.23, p = 0.305).
Discussion
OA is the most common form of arthritis that affects the elderly, and is the leading cause of disability in terms of its considerable impact on public health and society.34 The risk factors of OA have been extensively studied and age is one of the major factors for OA in most joints,35 as the ageing process renders joints vulnerable and susceptible to disease.36 Also, there is diminished capacity for cartilage repair with age, and hormonal changes occur along with the cumulative effects of environmental exposure, all of which are possible mechanisms for OA.37 Age is a strong predictor of OA development,38 and Pereira et al39 reported that age was positively associated with the radiological and pain scores; we also found that the severity of knee OA increases with age. However, although relationships between miRNA expression patterns and the ageing process are not fully understood, previous studies have provided evidence that miRNAs are associated with ageing.40-43 The miRNA expression was predominantly upregulated rather than downregulated in the livers of mice during ageing and the level of miR-22 was upregulated during cardiac ageing, in both fibroblasts and epithelial cells.44,45 miR-140-deficient mice have been shown to exhibit early onset age-related OA like changes when compared with wild-type mice, despite the joint structures appearing to be normal at birth and at one month of age.20 However, it was uncertain whether the expression of miR-140 in OA SF was determined by age. Our study confirms that there was no linear correlation between age and the relative expression of miR-140-3p/miR-140-5p, which is in accordance with the finding of this study that the differences in the expression of miR-140-3p/miR-140-5p across varying degrees of OA severity were not caused by age.
During the progress of OA, the associated alterations in the molecular composition and organisation of the cartilage matrix can lead to deterioration in the material properties and structural integrity of the articular surface and underlying hyaline cartilage.46 As the development of OA continues, there is evidence of increased catabolic activity related to enhanced expressions of degradative proteinase genes, associated with the gradual loss of proteoglycans, followed by type II collagen degradation.46 Analyses of human OA cartilage have shown increased amounts of a number of proteins indicative of the catabolic state, including matrix metalloproteinase (MMP), the family of a disintegrin and metalloproteinase with thrombospondin motifs (ADAMTS), ADAMTS5, ADAMTS4, and ADAMTS9.47 miR-140 regulates multiple targets, including MMP-13,48 ADAMTS5,20 IGFBP523 and aggrecan, suggesting that miR-140 plays an important role in regulating the balance between extracellular matrix formation and degradation.49 Zhang et al49 showed that the expression levels of miR-140-3p and miR-140-5p were both markedly and significantly reduced in OA chondrocytes. In our study, the miR-140-3p /miR-140-5p expression in knee SF was found to be significantly different between knee OA patients and healthy volunteers and the expression of miR-140-3p/miR-140-5p was negatively correlated with severity of OA. In previous studies, miR-140-5p has been proved to regulate several genes associated with cartilage homeostasis.20,50,51 In combination with the downregulation of miR-140-3p in OA SF shown in this study, we infer that miR-140-3p is one of the potential factors related to OA progression.
Tissue miRNAs have been noted not only as key molecules in intracellular regulatory networks for gene expressions, but also as biomarkers for various pathological conditions.52 Recent studies suggested that miRNAs in plasma can be biomarkers for the diagnosis of lung, colorectal, and prostate cancer.53,54 We have demonstrated the expression profiles of miR-140-3p/miR-140-5p in the SF of the knee with OA, and also found that the expression of miR-140-3p/miR-140-5p in the varying severity of OA SF was distinct from that in non-OA SF. This may reflect the condition of the joint cavity. Using SF miRNAs as biomarkers is a convenient method, and Murata et al9 have demonstrated that miRNAs in SF were as stable as plasma miRNAs at -20°C for up to seven days.
The miRNA-140 gene is located between exons 16 and 17 of the WWP2 gene on murine chromosome eight and in the small arm of chromosome 16 in humans.55 It was first believed that the regulation of intronic miRNAs followed that of their host genes as they are often co-expressed.56 However, recent reports showed that some intronic miRNAs have their own promoter and that their expression/regulation differs from that of their host genes.57,58 miR-140 may be derived from its own specific transcript during chondrogenesis, although the detailed mechanisms are not fully understood. The difference in the expression levels of WWP2 and miR-140 in OA chondrocytes23,59 suggested that, in addition to the WWP2 promoter, this miRNA is also controlled by intronic regulatory sequences. Tardif et al22 indicated the presence of regulatory elements in the sequence upstream of pre-miR-140 (rsmiR-140). The rsmiR-140 sequence has several potential binding sites for transcription factors, such as nuclear matrix transcription factor 4 (NMP4), myc-associated zinc (MAZ), nuclear factor of activated T-cells (NFAT), and mothers against decapentaplegic homolog 3 (SMAD3). The binding sites at NFAT3 (activator) and SMAD3 (repressor) directly regulated the miR-140-5p expression independently of WWP2.22 It may be that the transcription factors which target other binding sites of rsmiR-140 cause the discrepancy between the expression of miR-140-3p and miR-140-5p in OA chondrocytes.
We have demonstrated that there was a significant difference in the expression of miR-140-3p/miR-140-5p in the SF of the same group and that the expression of miR-140-5p was 7.4 times higher than that of miR-140-3p. Yamashita et al60 demonstrated that the proximal upstream region of pri-miR-140 has chondrogenic promoter activity in vivo. Furthermore, a gender-determining region Y-box (SOX) trio response element (L-SOX5/SOX6/SOX9) and details about the binding site in the promoter region were detected and miR-140 promoter activity was upregulated by the critical transcription factors L-SOX5, SOX6, and SOX9. Further studies are needed to explore the mechanisms responsible for the difference in miR140-3p and miR-140-5p expression in SF. Due to the limitations of our study design, other body fluid samples were not taken and a further study on miR140-3p and miR-140-5p could sample the blood and urine, which would be less invasive than sampling SF. In addition, as only the KLG radiological system has been applied in our study to assess the severity of knee OA, functional criteria have not been considered when classifying patients. Other severity scoring systems, such as the Knee injury and Osteoarthritis Outcome Score (KOOS) or the Western Ontario & McMaster Universities Osteoarthritis Index (WOMAC), could be used to provide objective functional classifications.61
In conclusion, this study has shown that expression of miR-140-3p/miR-140-5p was downregulated in 45 OA patients compared with 30 non-OA patients, and that the expression of miR-140-3p/miR-140-5p was negatively correlated with severity of OA. These findings should provide important clues to improve the pathological diagnosis and also to guide the clinical management of patients with OA.
Acknowledgments
The authors gratefully acknowledge the valuable contribution of Prof. Zhang Ge, School of Chinese Medicine, Hong Kong Baptist University and Department of Orthopaedics and Traumatology of Shenzhen People’s Hospital.
Footnotes
Author Contribution: C-M. Yin: First author, Sample collection, Experimental work, Statistical analysis, Approving the final manuscript.
W-C-W. Suen: Co-first author, Preparing and revising the manuscript, Approving the final manuscript.
S. Lin: Second author, Preparing and revising the manuscript, Approving the final manuscript.
X-M. Wu: Third author, Statistical analysis, Approving the final manuscript
G. Li: Co-corresponding author. Study design, Approving the final manuscript
X-H. Pan: Co-corresponding author, Study design, Samples collection, Experimental work, Approving the final manuscript.
Conflicts of Interest Statement: None declared
Funding Statement
This study was funded by the Shenzhen Science and Technology Research and Development Fund: grant numbers JCYJ20130402101926968 and JCYJ20150402152005636. The work was also partially supported by grants from Hong Kong Government Research Grant Council, General Research Fund (14119115, 14160917 and T12-402/17-N); National Natural Science Foundation of China (81371946, 81430049 and 81772322); and Shenzhen City Science and Technology Bureau, China (JCYJ20150630165236960).
References
- 1. Lotz MK, Kraus VB. New developments in osteoarthritis. Posttraumatic osteoarthritis: pathogenesis and pharmacological treatment options. Arthritis Res Ther 2010;12:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hashimoto M, Nakasa T, Hikata T, Asahara H. Molecular network of cartilage homeostasis and osteoarthritis. Med Res Rev 2008;28:464-481. [DOI] [PubMed] [Google Scholar]
- 3. Goldring MB, Marcu KB. Cartilage homeostasis in health and rheumatic diseases. Arthritis Res Ther 2009;11:224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Miyaki S, Asahara H. Macro view of microRNA function in osteoarthritis. Nat Rev Rheumatol 2012;8:543-552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gibson G, Asahara H. microRNAs and cartilage. J Orthop Res 2013;31:1333-1344. [DOI] [PubMed] [Google Scholar]
- 6. Iliopoulos D, Malizos KN, Oikonomou P, Tsezou A. Integrative microRNA and proteomic approaches identify novel osteoarthritis genes and their collaborative metabolic and inflammatory networks. PLoS One 2008;3:e3740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jones SW, Watkins G, Le Good N, et al. The identification of differentially expressed microRNA in osteoarthritic tissue that modulate the production of TNF-alpha and MMP13. Osteoarthritis Cartilage 2009;17:464-472. [DOI] [PubMed] [Google Scholar]
- 8. Yamasaki K, Nakasa T, Miyaki S, et al. Expression of MicroRNA-146a in osteoarthritis cartilage. Arthritis Rheum 2009;60:1035-1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Murata K, Yoshitomi H, Tanida S, et al. Plasma and synovial fluid microRNAs as potential biomarkers of rheumatoid arthritis and osteoarthritis. Arthritis Res Ther 2010;12:R86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sovani S, Grogan SP. Osteoarthritis: detection, pathophysiology, and current/future treatment strategies. Orthop Nurs 2013;32:25-36; quiz 37-28. [DOI] [PubMed] [Google Scholar]
- 11. Kijowski R, Blankenbaker DG, Stanton PT, Fine JP, De Smet AA. Radiographic findings of osteoarthritis versus arthroscopic findings of articular cartilage degeneration in the tibiofemoral joint. Radiology 2006;239:818-824. [DOI] [PubMed] [Google Scholar]
- 12. Lamers RJ, van Nesselrooij JH, Kraus VB, et al. Identification of an urinary metabolite profile associated with osteoarthritis. Osteoarthritis Cartilage 2005;13:762-768. [DOI] [PubMed] [Google Scholar]
- 13. Zhai G, Wang-Sattler R, Hart DJ, et al. Serum branched-chain amino acid to histidine ratio: a novel metabolomic biomarker of knee osteoarthritis. Ann Rheum Dis 2010;69:1227-1231. [DOI] [PubMed] [Google Scholar]
- 14. Felson DT. The current and future status of biomarkers in osteoarthritis. J Rheumatol 2014;41:834-836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Blanco FJ. Osteoarthritis year in review 2014: we need more biochemical biomarkers in qualification phase. Osteoarthritis Cartilage 2014;22:2025-2032. [DOI] [PubMed] [Google Scholar]
- 16. Brandt KD. The role of analgesics in the management of osteoarthritis pain. Am J Ther 2000;7:75-90. [DOI] [PubMed] [Google Scholar]
- 17. Ason B, Darnell DK, Wittbrodt B, et al. Differences in vertebrate microRNA expression. Proc Natl Acad Sci U S A 2006;103:14385-14389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wienholds E, Kloosterman WP, Miska E, et al. MicroRNA expression in zebrafish embryonic development. Science 2005;309:310-311. [DOI] [PubMed] [Google Scholar]
- 19. Tuddenham L, Wheeler G, Ntounia-Fousara S, et al. The cartilage specific microRNA-140 targets histone deacetylase 4 in mouse cells. FEBS Lett 2006;580:4214-4217. [DOI] [PubMed] [Google Scholar]
- 20. Miyaki S, Sato T, Inoue A, et al. MicroRNA-140 plays dual roles in both cartilage development and homeostasis. Genes Dev 2010;24:1173-1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nakamura Y, He X, Kobayashi T, et al. Unique roles of microRNA140 and its host gene WWP2 in cartilage biology. J Musculoskelet Neuronal Interact 2008;8:321-322. [PMC free article] [PubMed] [Google Scholar]
- 22. Tardif G, Pelletier JP, Fahmi H, et al. NFAT3 and TGF-β/SMAD3 regulate the expression of miR-140 in osteoarthritis. Arthritis Res Ther 2013;15:R197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tardif G, Hum D, Pelletier JP, Duval N, Martel-Pelletier J. Regulation of the IGFBP-5 and MMP-13 genes by the microRNAs miR-140 and miR-27a in human osteoarthritic chondrocytes. BMC Musculoskelet Disord 2009;10:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hwang S, Park S-K, Lee HY, et al. miR-140-5p suppresses BMP2-mediated osteogenesis in undifferentiated human mesenchymal stem cells. FEBS Lett 2014;588:2957-2963. [DOI] [PubMed] [Google Scholar]
- 25. Huang W, Li MD. Nicotine modulates expression of miR-140*, which targets the 3′-untranslated region of dynamin 1 gene (Dnm1). Int J Neuropsychopharmacol 2009;12:537-546. [DOI] [PubMed] [Google Scholar]
- 26. Takata A, Otsuka M, Kojima K, et al. MicroRNA-22 and microRNA-140 suppress NF-κB activity by regulating the expression of NF-κB coactivators. Biochem Biophys Res Commun 2011;411:826-831. [DOI] [PubMed] [Google Scholar]
- 27. Karlsen TA, Jakobsen RB, Mikkelsen TS, Brinchmann JE. microRNA-140 targets RALA and regulates chondrogenic differentiation of human mesenchymal stem cells by translational enhancement of SOX9 and ACAN. Stem Cells Dev 2014;23:290-304. [DOI] [PubMed] [Google Scholar]
- 28. Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 1986;29:1039-1049. [DOI] [PubMed] [Google Scholar]
- 29. Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315-324. [DOI] [PubMed] [Google Scholar]
- 30. Wallace SL, Robinson H, Masi AT, et al. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum 1977;20:895-900. [DOI] [PubMed] [Google Scholar]
- 31. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001;25:402-408. [DOI] [PubMed] [Google Scholar]
- 33. Levene H. Robust tests for equality of variances. In: Olkin I, ed. Contributions to Probability and Statistics: Essays in Honor of Harold Hotelling. Palo Alto, California: Stanford University Press, 1960:278-292. [Google Scholar]
- 34. Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthritis Cartilage 2013;21:1145-1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med 2000;133:635-646. [DOI] [PubMed] [Google Scholar]
- 36. Felson DT, Nevitt MC. Epidemiologic studies for osteoarthritis: new versus conventional study design approaches. Rheum Dis Clin North Am 2004;30:783-797, vii. [DOI] [PubMed] [Google Scholar]
- 37. Hart DJ, Doyle DV, Spector TD. Incidence and risk factors for radiographic knee osteoarthritis in middle-aged women: the Chingford Study. Arthritis Rheum 1999;42:17-24. [DOI] [PubMed] [Google Scholar]
- 38. Laxafoss E, Jacobsen S, Gosvig KK, Sonne-Holm S. Case definitions of knee osteoarthritis in 4,151 unselected subjects: relevance for epidemiological studies: the Copenhagen Osteoarthritis Study. Skeletal Radiol 2010;39:859-866. [DOI] [PubMed] [Google Scholar]
- 39. Pereira D, Severo M, Ramos E, et al. Potential role of age, sex, body mass index and pain to identify patients with knee osteoarthritis. Int J Rheum Dis 2017;20:190-198. [DOI] [PubMed] [Google Scholar]
- 40. Chen LH, Chiou GY, Chen YW, Li HY, Chiou SH. MicroRNA and aging: a novel modulator in regulating the aging network. Ageing Res Rev 2010;9(Suppl 1):S59-66. [DOI] [PubMed] [Google Scholar]
- 41. Jung HJ, Suh Y. MicroRNA in aging: from discovery to biology. Curr Genomics 2012;13:548-557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Smith-Vikos T, Slack FJ. MicroRNAs and their roles in aging. J Cell Sci 2012;125:7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Noren Hooten N, Fitzpatrick M, Wood WH, III, et al. Age-related changes in microRNA levels in serum. Aging (Albany NY) 2013;5:725-740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jazbutyte V, Fiedler J, Kneitz S, et al. MicroRNA-22 increases senescence and activates cardiac fibroblasts in the aging heart. Age (Dordr) 2013;35:747-762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Xu D, Takeshita F, Hino Y, et al. miR-22 represses cancer progression by inducing cellular senescence. J Cell Biol 2011;193:409-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Goldring MB, Goldring SR. Articular cartilage and subchondral bone in the pathogenesis of osteoarthritis. Ann N Y Acad Sci 2010;1192:230-237. [DOI] [PubMed] [Google Scholar]
- 47. Murphy G, Nagase H. Reappraising metalloproteinases in rheumatoid arthritis and osteoarthritis: destruction or repair? Nat Clin Pract Rheumatol 2008;4:128-135. [DOI] [PubMed] [Google Scholar]
- 48. Liang ZJ, Zhuang H, Wang GX, et al. MiRNA-140 is a negative feedback regulator of MMP-13 in IL-1β-stimulated human articular chondrocyte C28/I2 cells. Inflamm Res 2012;61:503-509. [DOI] [PubMed] [Google Scholar]
- 49. Zhang R, Ma J, Yao J. Molecular mechanisms of the cartilage-specific microRNA-140 in osteoarthritis. Inflamm Res 2013;62:871-877. [DOI] [PubMed] [Google Scholar]
- 50. Buechli ME, Lamarre J, Koch TG. MicroRNA-140 expression during chondrogenic differentiation of equine cord blood-derived mesenchymal stromal cells. Stem Cells Dev 2013;22:1288-1296. [DOI] [PubMed] [Google Scholar]
- 51. Mirzamohammadi F, Papaioannou G, Kobayashi T, Kobayashi T. MicroRNAs in cartilage development, homeostasis, and disease. Curr Osteoporos Rep 2014;12:410-419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Waldman SA, Terzic A. MicroRNA signatures as diagnostic and therapeutic targets. Clin Chem 2008;54:943-944. [DOI] [PubMed] [Google Scholar]
- 53. Mitchell PS, Parkin RK, Kroh EM, et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci U S A 2008;105:10513-10518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Chen X, Ba Y, Ma L, et al. Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res 2008;18:997-1006. [DOI] [PubMed] [Google Scholar]
- 55. Araldi E, Schipani E. MicroRNA-140 and the silencing of osteoarthritis. Genes Dev 2010;24:1075-1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Yang J, Qin S, Yi C, et al. MiR-140 is co-expressed with Wwp2-C transcript and activated by Sox9 to target Sp1 in maintaining the chondrocyte proliferation. FEBS Lett 2011;585:2992-2997. [DOI] [PubMed] [Google Scholar]
- 57. Monteys AM, Spengler RM, Wan J, et al. Structure and activity of putative intronic miRNA promoters. RNA 2010;16:495-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Isik M, Korswagen HC, Berezikov E. Expression patterns of intronic microRNAs in Caenorhabditis elegans. Silence 2010;1:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Miyaki S, Nakasa T, Otsuki S, et al. MicroRNA-140 is expressed in differentiated human articular chondrocytes and modulates interleukin-1 responses. Arthritis Rheum 2009;60:2723-2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Yamashita S, Miyaki S, Kato Y, et al. L-Sox5 and Sox6 proteins enhance chondrogenic miR-140 microRNA expression by strengthening dimeric Sox9 activity. J Biol Chem 2012;287:22206-22215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken) 2011;63(suppl 11):S208-S228. [DOI] [PMC free article] [PubMed] [Google Scholar]


