Abstract
BACKGROUND:
Intravenous fluid (IVF) is commonly used in acute clinical management. This study aimed to review the choice and primary considerations in IVF prescriptions and to evaluate the adequacy of guidelines and trainings on it in the New Territories West Cluster (NTWC) of Hong Kong.
METHODS:
This is a descriptive study based on data collected from an online survey. Data were processed by SPSS for statistical analysis. This study focused on a general description and doctor-nurse between group comparison. Participants were asked the choice of IVF for nine acute clinical scenarios and provide reason. A 1–10 scale was used to assess the sufficiency of guideline, training and information, and time for revision on IVF prescription.
RESULTS:
0.9% sodium chloride was the most familiar IVF (36%), followed by 5% Dextrose solution (26%). In the nine scenarios, the most chosen IVF was 0.9% sodium chloride (37%–61%). There was significant difference in the choice of IVF between doctors and nurses in 7 cases. The second most chosen IVF for doctors was Plasma-Lyte A while that for nurses was Gelofusine. Departmental practice was the most chosen reason to account for the prescription. The adequacy of guideline, information and training, and time for revision was rated 5. Doctors had significantly more time at work than nurses to update knowledge in IVF prescription (5.41 versus 4.57).
CONCLUSION:
0.9% sodium chloride was mostly chosen. The choice of IVF was mainly based on departmental practice. Adequacy of guideline, information and training, and time for revision on IVF prescription were average, indicating significant training deficit.
Keywords: Intravenous fluid, Acute care, Resuscitation
INTRODUCTION
Fluid therapy is essential to maintain fluid volume as well as electrolyte balance especially in hemodynamically unstable patients. There are two main categories of intravenous fluid (IVF), namely crystalloid and colloid. Crystalloid fluid refers to sterile water solution in which inorganic ions and small organic ions dissolved. These ions are mainly glucose or sodium chloride. They readily diffuse through membranes and distribute within the body compartments. Examples are 0.9% sodium chloride, lactated Ringer’s, and Plasma-Lyte A. Colloid fluid refers to sterile water solution with added macromolecules that do not pass through membranes freely. They tend to stay in the vascular space and are used as volume expanders. Examples are gelatins, dextrans, hydroxyethyl starches, albumin, and plasma protein fraction.
Choice of intravenous fluid could interfere with the outcome of patients. Precautions do exist in prescription of IVF as different fluids have different characteristics. For example, 0.9% sodium chloride can result in acute kidney injury due to its rich chloride content.[1,2] Certain IVF may also be more suitable for specific cases. For instance, Plasma-Lyte A was shown to have more rapid result in replenishing serum bicarbonate and rehydration for children with acute gastroenteritis when compared with 0.9% sodium chloride.[3]
IVF serves an important role in clinical management. Therefore, it is crucial that clinicians are familiar with different types of IVF in order to make precise judgement on which IVF to use. Junior doctors are often inadequately trained in fluid management, yet they are the most frequently involved staff in IVF prescriptions. Variations in IVF prescription practices also exist amongst clinicians.[4,5] To review the understanding of clinicians on various IVF and evaluate the adequacy of IVF guidelines and trainings in the New Territories West Cluster (NTWC) of Hong Kong, this study aimed at gaining an insight on the primary considerations in IVF prescriptions based on several acute clinical scenarios.
METHODS
Data were collected from an online survey, which was divided into 3 parts. Subjects were recruited on a voluntary basis by email invitation.
In part 1, participants were asked the number of times they prescribed IVF in the past 30 days and the type of IVF they were most familiar with. For the number of times of prescription, there were 7 options: 1–10 times, 11–20 times, 21–30 times, 31–40 times, 41–50 times, 51–60 times, and over 60 times. For the type of IVF most familiar with, there were 8 options: 5% dextrose, 1/3 - Dextrose 3.3% + NaCl 0.3%, lactated Ringer’s or Hartmann solution, 0.9% sodium chloride, Plasma-Lyte A, Gelofusine, plasma or plasma protein fraction, and others. They were also asked to rate their understanding on the IVF using a 1 to 10 scale, with 1 being the least understood and 10 being the most understood.
In part 2, participants were given 9 different acute clinical scenarios and asked to determine the type of IVF they would prescribe in each case with reasoning. The acute clinical scenarios include hypovolemic shock due to dehydration, hypovolemic shock due to extensive burns, hemorrhagic shock from acute gastrointestinal bleeding, traumatic hemorrhagic shock, cardiogenic shock, septic shock, anaphylactic shock, obstructive shock due to pericardial tamponade, and cardiac arrest. There were 10 reasons from which participants can choose for IVF prescription, including IVF readily available, undergraduate knowledge, personal routine, departmental practice, directed by supervisor, working department trainings, professional college guidelines, clinical handbooks, medical literature reviewing (e.g. Cochrane), and others.
In part 3, participants were asked to rate whether there is sufficient guideline on IVF prescription, whether enough information or training on acute IVF treatment was provided by the hospital, and whether they have adequate time to update their knowledge in acute IVF use both at work and after work. A 1 to 10 scale was used to assess these parameters, with 1 being the least sufficient while 10 being the most sufficient.
Fisher’s exact test was used to test the association between doctor and nurse groups for the choice of IVF in different scenarios and reasons underneath. Mann-Whitney U test was used to test the difference of continuous and scaled outcomes between doctors and nurses.
RESULTS
A total of 109 participants were recruited. The data were analyzed in two categories: general and doctor versus nurse. For the general one, all 109 data were taken into consideration. For doctor versus nurse comparison, 100 out of the 109 data were valid while the remaining 9 were excluded due to incomplete reply of the survey. Amongst the 100 valid data, 30 were nurses and 70 were doctors.
Part 1
The number of times of IVF prescription varied. 29% of participants prescribed 1–10 times of IVF in the past 30 days. Around one-fifth of them had 21–30 times of IVF prescription. Another 15% of participants had IVF prescription for over 60 times. 36% of participants were most familiar with 0.9% sodium chloride. 5% Dextrose solution came second with 26% of participants found it accustomed. Regarding participants’ understanding on the chosen IVF in general, the mean score was 6.62 out of 10. For doctor versus nurse comparison, there was no significant difference in their understanding on IVF chose (P=0.788).
Part 2
Hypovolemic shock due to dehydration
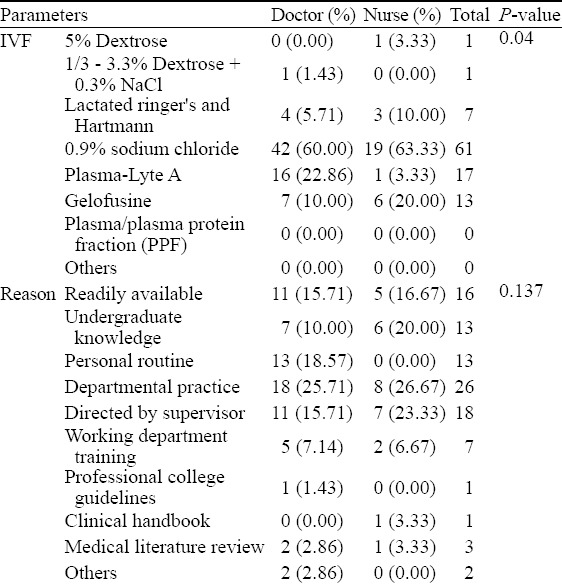
In general, 61% of the participants chose 0.9% sodium chloride. The second most chosen one was Plasma-Lyte A with 17% of participants choosing it. 26% of the underlying reason was departmental practice. For doctor-nurse comparison, there was significant difference in the choice of IVF (P=0.040). For the reason behind, the P-value was 0.137, indicating no significant difference among the two groups (Table 1).
Table 1.
Hypovolemic shock due to dehydration (n=100)
Hypovolemic shock due to extensive burns
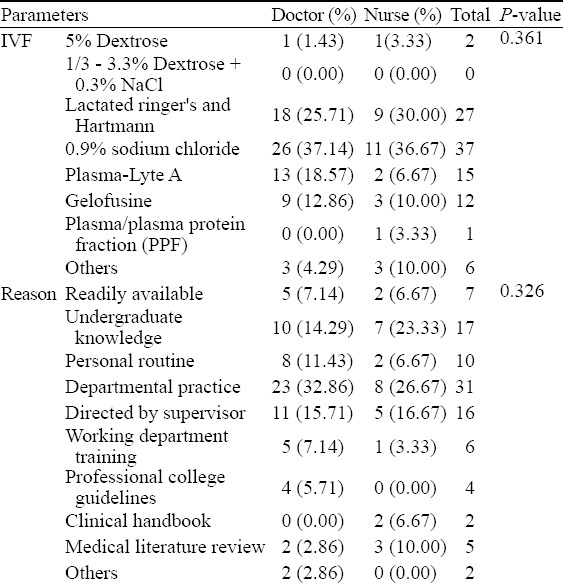
37% of the participants in general chose 0.9% sodium chloride followed by 27% of them choosing lactated Ringer’s or Hartmann solution. The most chosen reason was departmental practice which counted for 31%. For doctor-nurse comparison, there was no significant difference in the choice of IVF and reason with P-values of 0.361 and 0.326 respectively (Table 2).
Table 2.
Hypovolemic shock due to extensive burns (n=100)
Hemorrhagic shock from acute gastrointestinal bleeding
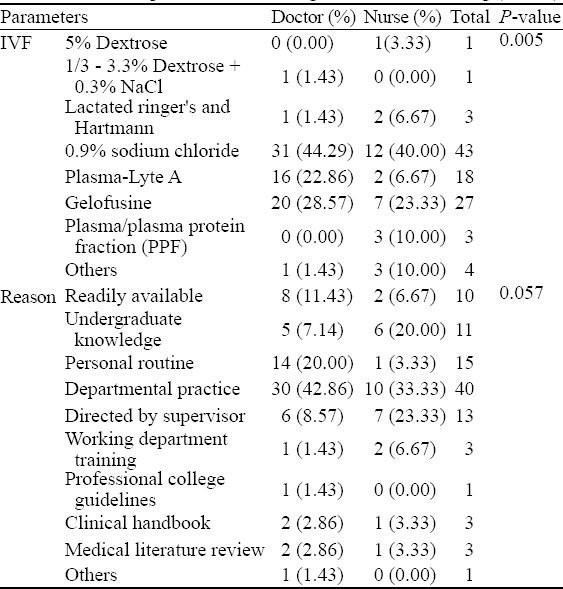
In general, 43% of the participants would prescribe 0.9% sodium chloride while 27% of them opted for Gelofusine. The most chosen reason for the choice was due to departmental practice, accounting for 40%. There was significant difference for the choice of IVF between doctors and nurses (P=0.005) but there was no significant difference in the reasoning with a P-value of 0.057 (Table 3).
Table 3.
Hemorrhagic shock from acute gastrointestinal bleeding (n=100)
Traumatic hemorrhagic shock
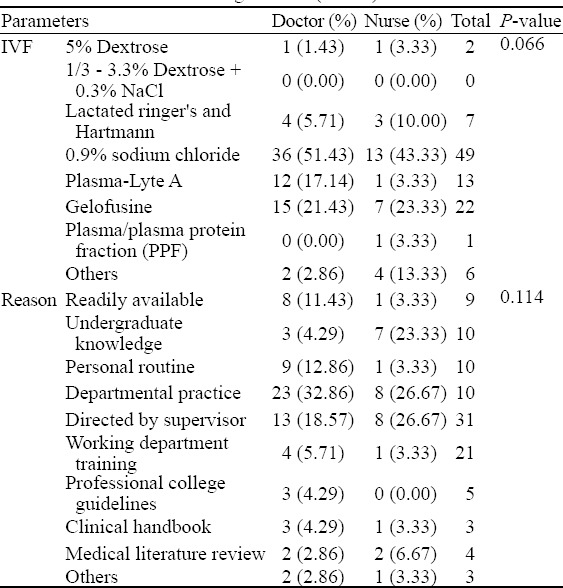
Nearly half of the participants (49%) chose to prescribe 0.9% sodium chloride in general. The second most chosen IVF was Gelofusine (22%). Departmental practice accounted for most of the underlying reason (31%). For doctor-nurse comparison, there was no significant difference in the choice of IVF and reason underneath with P-values of 0.066 and 0.114 respective-ly (Table 4).
Table 4.
Traumatic hemorrhagic shock (n=100)
Cardiogenic shock
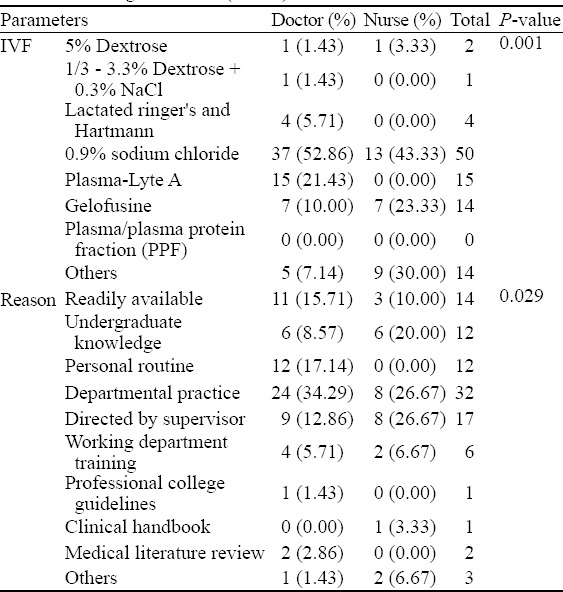
Half of the participants chose 0.9% sodium chloride in general, followed by Plasma-Lyte A (15%). The most chosen reason was departmental practice which counted for 32%. There was significant difference in the choice and underlying reason for IVF prescription between doctors and nurses with P-value of 0.001 and 0.029 respectively (Table 5).
Table 5.
Cardiogenic shock (n=100)
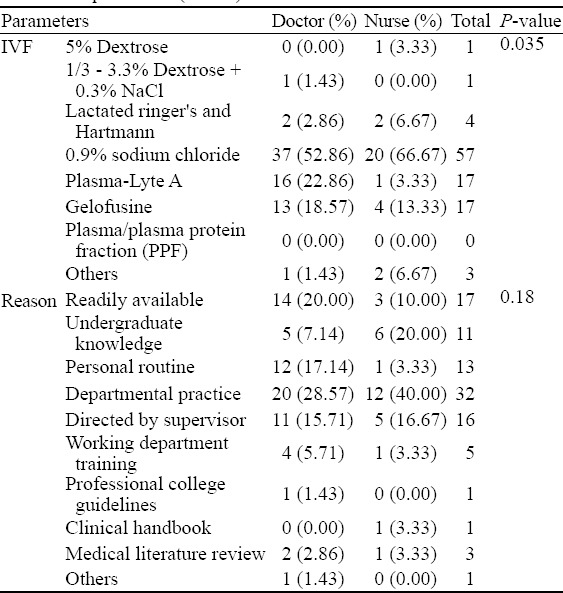
Septic shock
In general, 57% of the participants would prescribed 0.9% sodium chloride while Plasma-Lyte A and Gelofusine came second, counted 17% each. Departmental practice was the most chosen reason for the prescription (32%). For doctor-nurse comparison, there was significant difference in the IVF chosen (P=0.035). The P-value for the reason of IVF prescription among the two groups was 0.180, indicating no significant difference (Table 6).
Table 6.
Septic shock (n=100)
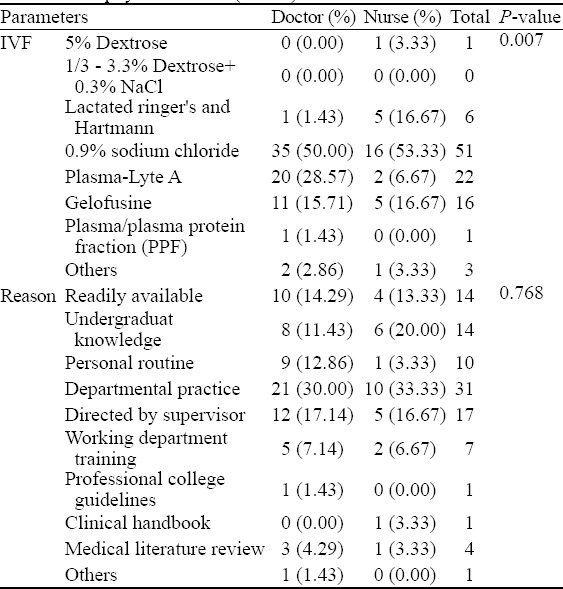
Anaphylactic shock
Around half (51%) of the participants in general chose to prescribe 0.9% sodium chloride while 22% chose Plasma-Lyte A. Around one third (31%) chose departmental practice to account for their choice. There was significant difference for the choice of IVF between doctors and nurses (P=0.007) while the P-value for the underlying reason was 0.768, indicating no significant difference among the two groups (Table 7).
Table 7.
Anaphylactic shock (n=100)
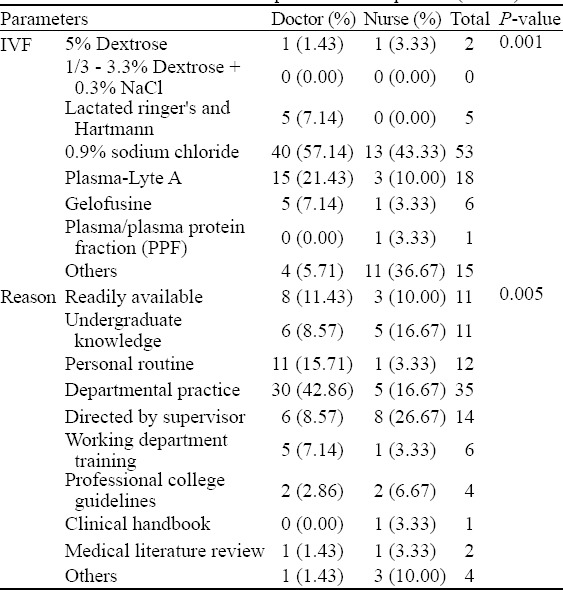
Obstructive shock due to pericardial tamponade
In general, 53% of the participants chose 0.9% sodium chloride, followed by 18% of them choosing Plasma-Lyte A. The most chosen reason was departmental practice which counted for 35%. For doctor-nurse comparison, the P-values for the choice of IVF and underlying reason were 0.001 and 0.005, indicating a significant difference between the two groups (Table 8).
Table 8.
Obstructive shock due to pericardial tamponade (n=100)
Cardiac arrest
60% of the participants would prescribe 0.9% sodium chloride. Another 18% of the participants chose to prescribe Plasma-Lyte A. Departmental practice accounted for 35% of the reason behind the choice. Comparing doctor and nurse groups, there was significant difference in the choice of IVF (P=0.000). The P-value for the reason was 0.092, indicating no significant difference among the two groups (Table 9).
Table 9.
Cardiac arrest (n=100)
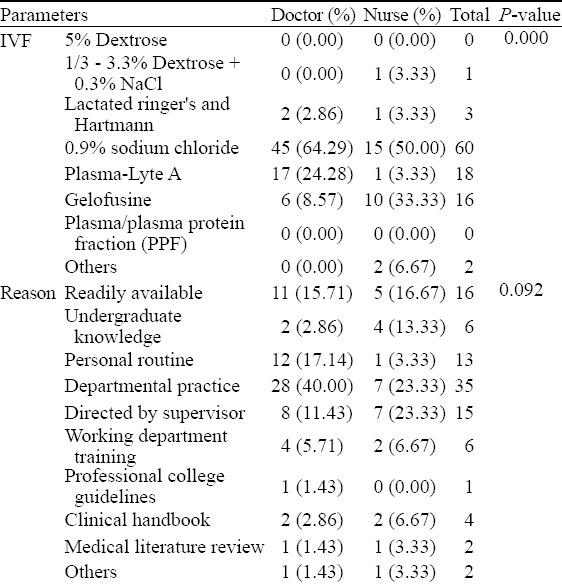
By summarizing the answers from the above nine scenarios, around half of the participants chose 0.9% sodium chloride as their prescription in any scenario. At the same time, the dominant reason for the choice of IVF prescription was departmental practice in all scenarios. For doctor versus nurse comparison, 7 out of the 9 scenarios showed significant difference on the choice of IVF pre-scription with P-value less than 0.05. For the underlying reason, only 2 out of the 9 scenarios showed a significant difference among the two groups.
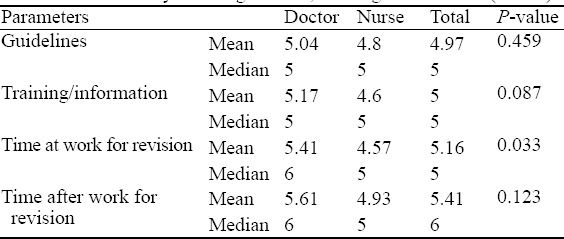
Part 3
Regarding whether there was sufficient guideline on IVF prescription, the mean was 4.97 out of 10 in general. The P-value for doctor-nurse comparison was 0.459, indicating no significant difference between the two groups. Concerning the adequacy of training or information provided on acute IVF treatment by hospital, the mean was 5 out of 10. There is no significant difference comparing doctor and nurse groups (P=0.087). For the sufficiency of time to update knowledge on IVF use, the mean for time at work was 5.16 out of 10 while that for time after work was 5.41 out of 10. There was significant difference of time at work for knowledge revision between doctor and nurse groups (P=0.033) while no significant difference was observed for time after work (P=0.123) (Table 10).
Table 10.
Sufficiency of IVF guideline, training and revision (n=100)
DISCUSSION
Clinicians frequently prescribe IVF in clinical management, especially in acute settings. Complications are prompt to occur if inappropriate IVFs are chosen. According to a prospective study conducted by Walsh,[1] around 20% of general surgical patients suffered from complications related to inappropriate IVF prescription. Hence, it is crucial to have better understanding of IVF.
In the 9 acute clinical scenarios proposed, 0.9% sodium chloride was the most chosen IVF, ranging from 37% to 61%. The results demonstrated in this study seemed consistent that most clinicians would opt for 0.9% sodium chloride when it comes to fluid resuscitation. In our study, most clinicians’ decision on the choice of IVF was based on departmental practice. 0.9% sodium chloride was the most chosen regardless of the scenarios. However, when the second most chosen IVF was taken into account, certain trend could be observed. Among the 9 scenarios, 4 of them involved body fluid loss, including hypovolemic shock due to dehydration, hypovolemic shock due to extensive burns, hemorrhagic shock from acute gastrointestinal bleeding, and traumatic hemorrhagic shock. Two out of the 4 scenarios had Gelofusine as the second most chosen IVF. In contrast, Plasma-Lyte A was the second most chosen IVF in the remaining 5 cases with no body fluid loss. This showed that in most acute cases, crystalloids are preferred by clinicians. However, cases in which loss of body fluid were evident, more clinicians may tend to prescribe colloids like Gelofusine. Comparing doctor and nurse groups, there was significant difference in the choice of IVF in 7 out of 9 scenarios. Although 0.9% sodium chloride was still the most chosen IVF, it was observed that the second most chosen IVF varied between the groups. In the majority of cases, the second most chosen IVF in the doctor group was Plasma-Lyte A (6 out of 9) while that in the nurse group was Gelofusine (7 out of 9). Substantially less percentage of nurses chose Plasma-Lyte A as the IVF of choice in the majority of cases, especially in the case of cardiogenic shock.
Throughout the years, whether infusion of crystalloid or colloid would be better in fluid resuscitation has been a hot topic. A study compared the performance of volume expansion in subjects with moderate hypovolemia showed that colloid may do better than crystalloid in a temporary manner.
When infused rapidly, it was found that intravascular volume expansion was significantly greater with 6% Hetastarch than with the same volume of lactated Ringer’s solution.[6] In another study comparing the long term mortality of crystalloid and colloid infusion in hypovolemic subjects, it was found that the 28-day mortality was comparable in both groups but the colloid group was asso-ciated with a lower 90-day mortality.[7] This randomized clinical trial also demonstrated that the colloid group resulted in more days free of mechanical ventilation and vasopressor support. Nevertheless, a Cochrane review failed to demonstrate mortality benefit in a variety of subjects including those with trauma, burns, or sepsis resuscitated with colloids when compared with those resuscitated with crystalloids.[8] As colloids are much more expensive than crystalloids, taking into consideration the economic opportunity cost, it was concluded that the use of colloids over crystalloids may not be justified. Furthermore, another systemic review even demonstrated harm for the use of colloid in resuscitation. When hydroxyethyl starches was used in fluid resuscitation, it was shown that there was significant rise in the risk of acute kidney injury and even death.[9]
In recent years, guidelines have been published about the recommendations of IVF prescription.[10,11] Balanced crystalloids were generally recommended as the IVF of choice. Liberal use of normal saline, however, can be associated with several complications. Despite being the most-chosen IVF, normal saline can lead to hyperchloremia and academia, contributing to morbidity of patients. Further studies may be needed to comment on whether crystalloids or colloids would be more superior than the other in fluid resuscitation. It is understandable that the choice of IVF may hardly induce immediate severe side effects particularly in healthy subjects with minor fluid deficit. Nonetheless, in acute clinical settings where patients can deteriorate rapidly, precise choice of IVF is crucial as any minor mistake would not be affordable.
IVF prescription is generally based on individual clinical judgment. However, it was shown in various studies that clinicians were deficient in the knowledge of IVF.[5,12] Regarding the results obtained from part 3 of our study, there is still room for improvement in the adequacy of guideline, training and information provided on IVF prescription. A study in the United Kingdom surveyed impression of consultant surgeons about their junior staff in peri-operative fluid replacement also showed similar result. It was reported that only 22% of junior staff were given written guidelines in IVF prescription and only 30% of consultant surgeons agreed that their postoperative patients received appropriate fluid and electrolyte replacement.[13] Although doctors may have more chance to be involved in the decision of IVF prescription during work, clinicians generally had average time to revise knowledge in IVF use. Further practical training with written guidelines may be needed to improve the standard in IVF prescription.
Limitations
Several limitations exist in this study. For instance, subjective measurement of the understanding on IVF was adopted using scales. Participants may however have different individual standards. It was also only a descriptive study based on an online survey with a small sample size. Sub-group analysis based on the different grade and experience of subjects was hence not feasible. Besides, not all the IVFs are available in every department. For example, Plasma-Lyte A is only found in certain departments like O&T, ICU, and A&E. Hence, some IVFs would not be reachable by clinicians in other departments. Moreover, the presentations of patients in the proposed acute clinical scenarios were not provided. Thus, clinicians, especially less experienced ones, might not have in-depth knowledge of the overall clinical picture of the cases, leading to possible misunderstanding of the topics.
Improvements can be made to make this study more comprehensive. The collection of data sample takes time. In the future, a larger sample size should be recruited which can cover the whole of Hong Kong but not limited to New Territories West Cluster and may even extend to multi-national study. Besides, details of the acute clinical scenarios can be given, such as blood loss volume and vital signs, so as to assist participants in decision making. Moreover, as combination of IVFs can be given during different stages of clinical management. The stage of the scenarios should also be specified. Future studies on this subject with larger scale and randomised sampling would help verify this pilot study.
CONCLUSION
0.9% sodium chloride was mostly chosen as the required IVF therapy in the various acute clinical situations. The choice of IVF was mainly based on departmental practice in all cases. Adequacy of guideline, information, training and time for revision on IVF prescription were rated as average, indicating a significant training deficit.
ACKNOWLEDGMENTS
The authors would like to thank Dr. CW Kam and Clinical Skills Training Centre in Tuen Mun Hospital for the invaluable input and support on this study.
Footnotes
Funding: None.
Ethical approval: Ethical approval was exempted from the ethics committee of the New Territories West Cluster Clinical Research Ethics Committee in Hong Kong as it was a descriptive study in which no intervention was implemented on any patient and there was no alternation on patients’ management.
Conflicts of interest: The authors have no competing interests relevant to the present study.
Contributors: WYSC proposed the study, analyzed the data and wrote the first drafts. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
- 1.Yunos NM, Bellomo R, Hegarty C, Story D, Ho L, Bailey M. Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA. 2012;308(15):1566–72. doi: 10.1001/jama.2012.13356. [DOI] [PubMed] [Google Scholar]
- 2.Young P, Bailey M, Beasley R, Henderson S, Mackle D, McArthur C, et al. Effect of a Buffered Crystalloid Solution vs Saline on Acute Kidney Injury Among Patients in the Intensive Care Unit:The SPLIT Randomized Clinical Trial. JAMA. 2015;314(16):1701–10. doi: 10.1001/jama.2015.12334. [DOI] [PubMed] [Google Scholar]
- 3.Allen CH, Goldman RD, Bhatt S, Simon HK, Gorelick MH, Spandorfer PR, et al. A randomized trial of Plasma-Lyte A and 0.9% sodium chloride in acute pediatric gastroenteritis. BMC Pediatr. 2016;16:117. doi: 10.1186/s12887-016-0652-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walsh SR, Walsh CJ. Intravenous fluid-associated morbidity in postoperative patients. Ann R Coll Surg Engl. 2005;87(2):126–30. doi: 10.1308/147870805X28127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lim CT, Dunlop M, Lim CS. Intravenous fluid prescribing practices by foundation year one doctors - a questionnaire study. JRSM Short Rep. 2012;3(9):64. doi: 10.1258/shorts.20121.012041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McIlroy DR, Kharasch ED. Acute intravascular volume expansion with rapidly administered crystalloid or colloid in the setting of moderate hypovolemia. Anesth Analg. 2003;96(6):1572–7. doi: 10.1213/01.ANE.0000061460.59320.B0. [DOI] [PubMed] [Google Scholar]
- 7.Annane D, Siami S, Jaber S, Martin C, Elatrous S, Declère AD, et al. Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock:the CRISTAL randomized trial. JAMA. 2013;310(17):1809–17. doi: 10.1001/jama.2013.280502. [DOI] [PubMed] [Google Scholar]
- 8.Perel P, Roberts I, Ker K. Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst Rev. 2013;(2):CD000567. doi: 10.1002/14651858.CD000567.pub6. [DOI] [PubMed] [Google Scholar]
- 9.Zarychanski R, Abou-Setta AM, Turgeon AF, Houston BL, McIntyre L, Marshall JC, et al. Association of hydroxyethyl starch administration with mortality and acute kidney injury in critically ill patients requiring volume resuscitation:a systematic review and meta-analysis. JAMA. 2013;309(7):678–88. doi: 10.1001/jama.2013.430. [DOI] [PubMed] [Google Scholar]
- 10.Soni N. British Consensus Guidelines on Intravenous Fluid Therapy for Adult Surgical Patients (GIFTASUP):Cassandra's view. Anaesthesia. 2009;64(3):235–8. doi: 10.1111/j.1365-2044.2009.05886_1.x. [DOI] [PubMed] [Google Scholar]
- 11.National Institute for Health and Care Excellence (NICE) (2017) Intravenous Fluid Therapy in Adults in Hospital:NICE Guideline [CG174] London: NICE; [PubMed] [Google Scholar]
- 12.Lobo DN, Dube MG, Neal KR, Simpson J, Rowlands BJ, Allison SP. Problems with solutions:drowning in the brine of an inadequate knowledge base. Clin Nutr. 2001;20(2):125–30. doi: 10.1054/clnu.2000.0154. [DOI] [PubMed] [Google Scholar]
- 13.Lobo DN, Dube MG, Neal KR, Allison SP, Rowlands BJ. Peri-operative fluid and electrolyte management:a survey of consultant surgeons in the UK. Ann R Coll Surg Engl. 2002;84(3):156–60. [PMC free article] [PubMed] [Google Scholar]


