Abstract
BACKGROUND:
Accurate and timely diagnosis of acute surgical disease in pregnant patient is challenging. Although magnetic resonance imaging (MRI) is the most accurate modality to diagnose acute appendicitis in pregnant patients, it is often used as a last resort because of high cost and long scan time. We performed this study to analyze differential diagnoses of appendix MRI and to investigate if there are any blood tests that can predict surgical condition in pregnant patients.
METHODS:
A retrospective, cross-sectional study was conducted on 46 pregnant patients who underwent non-enhanced appendix MRI in suspicion of acute appendicitis from 2010 to 2016. Differential diagnoses of appendix MRI were analyzed and blood tests were compared between those who had surgical and non-surgical disease.
RESULTS:
Appendix MRI differentiated two surgical disease; acute appendicitis and ovarian torsion; and various non-surgical conditions such as uterine myoma, hydronephrosis, ureterolithiasis and diverticulitis among clinically suspected acute appendicitis in pregnancy. The diagnostic accuracy of MRI for acute appendicitis in this study was 93.5%. Patients who had surgical disease showed significantly higher WBC count (≥11,000/mm3), proportion of neutrophils in the WBC (≥79.9%), neutrophil-to-lymphocyte ratio (NLR≥6.4), levels of C-reactive protein (CRP≥1.82 mg/dL) and bilirubin (≥0.66 mg/dL) than those who had non-surgical disease.
CONCLUSION:
MRI can reliably differentiate surgical conditions and several blood tests (WBC, proportion of neutrophils in the WBC, NLR, CRP, bilirubin) can help anticipate acute surgical condition among pregnant patients suspected to have acute appendicitis.
Keywords: Appendicitis, Magnetic resonance imaging, Pregnancy, Neutrophils
INTRODUCTION
An accurate diagnosis of the source of abdominal pain in pregnant patients is often very difficult owing to several factors, such as nonspecific symptoms (nausea and vomiting), nonspecific leukocytosis, displacement of the abdominal structures from its normal location, difficult abdominal examination, and limited utilization of computed tomography (CT) owing to ionizing radiation. Acute appendicitis is the most frequent extra-uterine illness necessitating emergency surgery in pregnant patients, occurring approximately 1 in 1,700 pregnancies.[1-3] However, acute appendicitis is more difficult to diagnose, and complication rates, such as perforation rates, are higher in pregnant patients than in non-pregnant patients.[4-6] An accurate and timely preoperative diagnosis of acute appendicitis is crucial because an unnecessary operation will increase the rate of fetal loss and early delivery.[7,8]
Magnetic resonance imaging (MRI) has become increasingly popular in the evaluation of acute abdominal pain in pregnant patients. MRI provides multi-planar images with excellent soft-tissue contrast resolution without the drawback of exposing the fetus to the ionizing radiation.[9] The American College of Radiology (ACR) approves of MRI the use of MRI in pregnant patients in any trimester.[10] To our knowledge, MRI is the most accurate preoperative diagnostic modality for acute appendicitis in pregnant patients.[11] Furthermore, MRI is one of the best tools to demonstrate safely a wide range of conditions in the abdomen and pelvis beyond acute appendicitis.[12] When acute appendicitis is clinically suspected in pregnant patients, MRI can be performed as an initial diagnostic method or after ultrasound (US) in which the US findings are equivocal.[11]
However, a substantial proportion of pregnant patients who underwent MRI often have non-surgical sources of abdominal pain. Although there are no known biologic risks associated with MRI, some potential adverse effects of MRI fields, such as reduction in the fetal crown-rump length or increased developmental eye malformations in an animal model have been reported.[13,14] Moreover, unknown bio-effects may still exist, especially during the period of organogenesis.[9] Therefore, extra caution is urged when using MRI for pregnant patients, especially during the first trimester of pregnancy. We performed this study to investigate various differential diagnoses based on appendix MRI findings and to determine if there are any blood test biomarkers that can predict the need for surgical treatment.
METHODS
Study design
A retrospective, cross-sectional study was conducted after receiving approval from the Institutional Review Board (IRB) of our hospital. Written informed consent was exempted by the IRB. To maintain anonymity, the patient name, hospital number, date of birth, and social security number were deleted after assigning a serial number to each. This study was carried out in accordance with the World Medical Association Declaration of Helsinki.[15]
Selection of patients
We selected all pregnant subjects who underwent non-enhanced appendix MRI in suspicion of acute appendicitis during our study period (7 years; from 2010 to 2016). The subjects were then divided into 6 arbitrarily defined groups according to the formal report of appendix MRI: group 1, normal appendix without other abnormal findings; group 2, normal appendix with other findings potentially related to abdominal pain; group 3, non-visualization of appendix with other findings potentially related to abdominal pain; group 4, probable acute appendicitis without other abnormal findings; group 5, probable acute appendicitis with other findings potentially related to abdominal pain; and group 6, definite acute appendicitis. The patients were allocated to the “probable acute appendicitis” group when the radiologist reported their cases as “suspicious of (early) appendicitis” with descriptions such as “borderline or mild dilatation, mild or minimal inflamed appendix, or mild wall thickening”. Patient characteristics, clinical features, and blood test parameters were analyzed in accordance with the 6 defined groups.
Key outcome measures
We divided the subjects into those who had a non-surgical disease and those who had a surgical disease. Clinical features and blood test parameters were comparatively analyzed between the 2 groups. The results of the blood tests performed on the same day of appendix MRI were analyzed. The analyzed blood test results included the white blood cell (WBC) count, percentage of segmented neutrophil, lymphocyte and monocyte in the WBC, neutrophil-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), platelet count, platelet-to-lymphocyte ratio (PLR), red cell distribution width (RDW), C-reactive protein (CRP) and bilirubin. The NLR, MLR and PLR were calculated using the ratios of the neutrophil count to the lymphocyte count, monocyte count to lymphocyte count and platelet count to lymphocyte count, respectively. When the patients received the same blood test more than once on the same day, the initial test result was selected for the analysis.
Statistical analysis
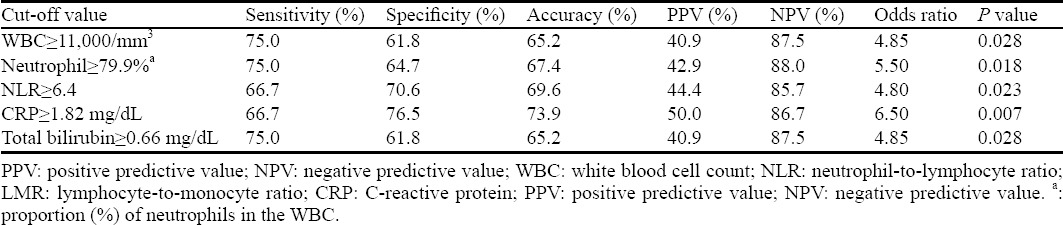
The blood test parameters showing significant statistical differences between the conservatively treated and surgically treated groups were further analyzed using the receiver operating characteristics (ROC) to verify their usefulness as a predictor of surgical treatment. For those parameters with ROC of > 0.7, the best cutoff value was calculated, and sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of that cutoff value were also calculated.
The continuous variables did not have a normal distribution; thus, they were presented as medians and interquartile ranges, and the categorical variables were described in frequencies (%). We compared the continuous variables using the Mann-Whitney test and the categorical variables using the Chi-square or the Fisher’s exact test according to the expected frequency. We used the STATA ver. 13.0 (StataCorp., College Station, TX, USA) program for our statistical analysis and the statistical significance was based on a P value < 0.05.
RESULTS
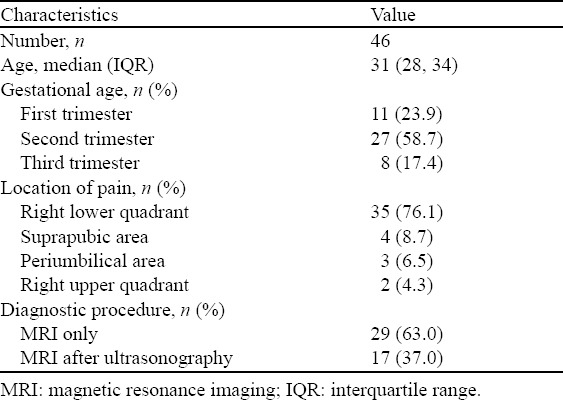
Forty-six pregnant patients underwent MRI due to acute abdominal pain during the 7-year study period. The characteristics of 46 patients are presented in the Table 1.
Table 1.
Summary of patient (pregnant patients who underwent appendix MRI due to acute abdominal pain) characteristics
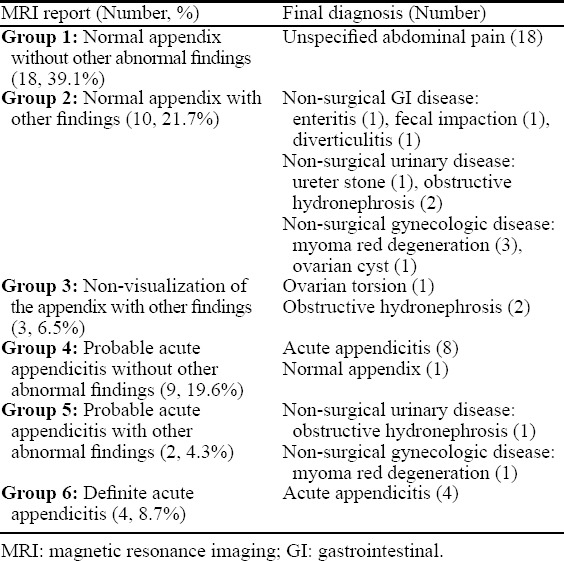
Appendix MRI showed various findings for the pregnant patients with acute abdominal pain. Normal appendix was reported in 28 (60.9%), non-visualization of the appendix in 3 (6.5%), probable appendicitis in 11 (23.9%), and definite appendicitis in 4 (8.7%) patients. Among the 28 patients with normal appendix, 18 patients showed no other abnormal findings and 10 patients showed other abnormal findings potentially related to abdominal pain. Red degeneration of uterine myoma was the most frequent abnormal finding followed by right obstructive hydronephrosis. The appendix was not visualized in 3 patients and one of these patients underwent emergency surgery due to right ovarian torsion. Eleven patients showed probable appendicitis (early appendicitis, borderline or mild dilatation of the appendix, mild or minimal inflamed appendix, or mild wall thickening of the appendix) in the appendix MRI. Nine patients with probable acute appendicitis without other abnormal findings underwent surgery, and the final pathologic report showed acute appendicitis in 8 patients and normal appendix in 1 patient. Two patients with probable acute appendicitis with other abnormal findings (1 obstructive hydronephrosis and 1 uterine myoma red degeneration) did not undergo surgery and were treated conservatively. Both of them recovered completely without surgery (Table 2). Four patients showed definite acute appendicitis. Nine patients with probable appendicitis and 4 patients with definite acute appendicitis underwent an appendectomy, and the negative appendectomy rate was 7.7% (1/13) among our study subjects.
Table 2.
Differential diagnoses of appendix MRI among the pregnant patients with acute abdominal pain
Twenty-nine patients underwent appendix MRI after US when the US findings were equivocal or the appendix was not visualized. Among them, 62.1% showed normal appendix, 27.6% showed probable acute appendicitis, and 10.3% had a non-visualized appendix. Twelve (41.4%) patients showed normal appendix without other abnormal findings (group 1 finding); 6 (20.7%) patients showed normal appendix with other findings potentially related to abdominal pain (group 2 finding); 3 (10.3%) patients showed non-visualization of the appendix with other findings potentially related to abdominal pain (group 3 finding); 6 (20.7%) patients showed probable acute appendicitis without other abnormal findings (group 4 finding); and 2 (6.9%) patients showed probable acute appendicitis with other findings potentially related to abdominal pain (group 5 finding) on the subsequent appendix MRI after US.
Laboratory features were compared between the surgical and non-surgical abdomen cases. Thirteen patients (12 acute appendicitis and 1 ovarian torsion) had a surgical disease, and 33 patients had non-surgical conditions. The patients who had conditions which required surgical treatment showed significantly higher WBC count, higher proportion of neutrophils in the WBC, lower proportion of lymphocytes in the WBC, higher NLR, and higher levels of CRP and bilirubin (Table 3). To determine if there were any blood tests that can aid in predicting the need for surgical treatment, an ROC analysis was performed for parameters that had statistically significant difference between the 2 groups. WBC, proportion of neutrophils in the WBC, NLR, and CRP and bilirubin levels had areas under the curve (AUC) of >0.7. NLR had the largest AUC (0.744) followed by the proportion of neutrophils in the WBC (0.728) (Table 4). The best cutoff value and its sensitivity, specificity, accuracy, PPV and NPV to predict the need for surgical treatment are presented in Table 5.
Table 3.
Comparison of the blood test results between the surgical and non-surgical abdomen cases of the pregnant patients with acute abdominal pain
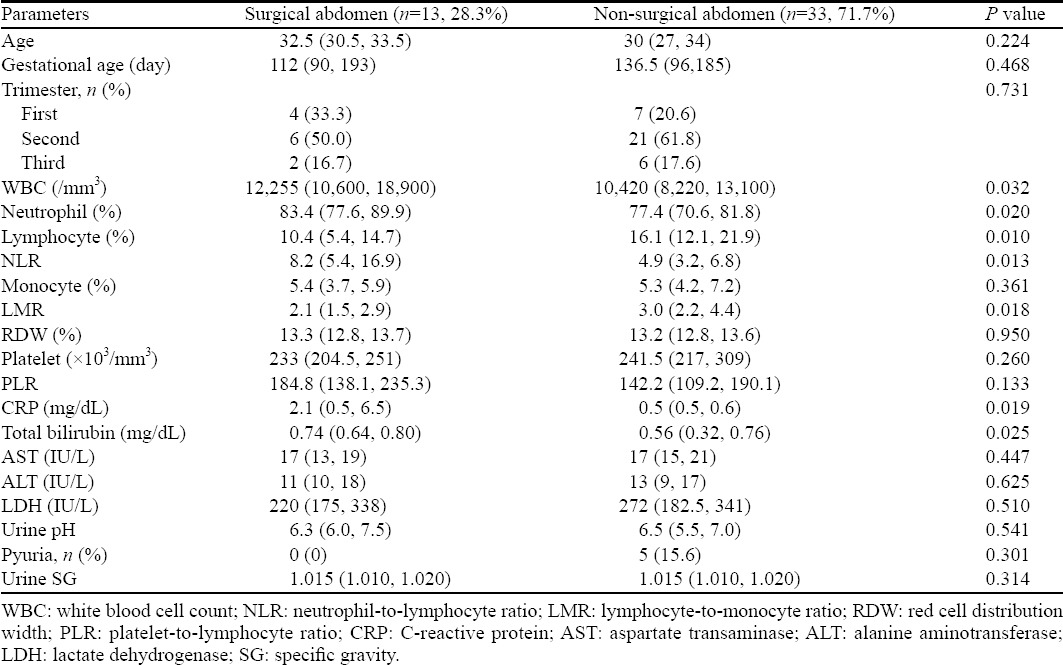
Table 4.
ROC analysis of the blood test parameters associated with the need for surgical treatment among the pregnant patients with acute abdominal pain
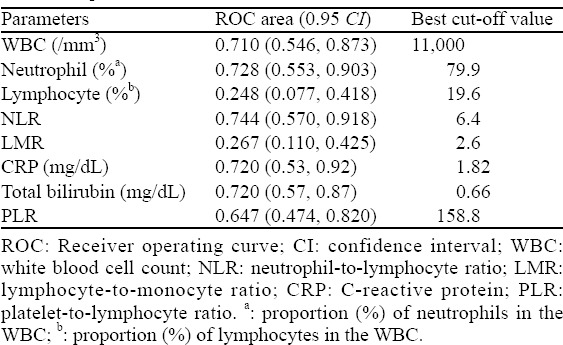
Table 5.
Usefulness of the blood tests in predicting the need for surgical treatment among the pregnant patients with acute abdominal pain
DISCUSSION
Imaging tests have become more important than before in making specific diagnosis of acute abdominal pain in pregnant women. In the case of acute appendicitis, which is the most common extra-uterine surgical disease, imaging tests can not only reduce the negative appendectomy rate,[16,17] but also distinguish complicated from benign form of acute appendicitis in which spontaneous resolution can be expected.[17,18]
To date, MRI is the most accurate diagnostic modality to differentiate acute surgical conditions for pregnant patients complaining of acute abdominal pain. One of most recent guidelines also recommends MRI in pregnant patients with suspected appendicitis, if this resource is available.[17] Our study results showed that the pregnant patients who underwent MRI in suspicion of acute appendicitis turned out to have both surgical and non-surgical conditions. Acute appendicitis was by far the most frequent surgical disease followed by ovarian torsion. Red degeneration of uterine myoma was the most frequent non-surgical condition followed by obstructive hydronephrosis of the right kidney
Although MRI is the most accurate diagnostic modality in differentiating acute surgical conditions in pregnant patients,[11] it also has disadvantages. MRI usually costs more than US, needs expert radiologists for interpretation, and is not possible for patients with claustrophobia. To our knowledge, there are no known deleterious effects on the fetus secondary to MRI use, MRI deposits energy in the patients in the form of heat.[10] In animal studies, reduction in the fetal crown-rump length and increased risk of eye malformations were reported after exposure to MRI energy.[13,14] The ACR still emphasizes to weigh the risks and benefits of MRI for pregnant patients.[10] Therefore, it is desirable if unnecessary MRIs can be avoided during the pregnancy, especially during the first trimester.
Negative appendectomy (NA) rate of pregnant patients is reported to be 25%–36%,[10,19] and this NA rate is significantly higher in pregnant women compared with nonpregnant women (36% vs. 14%; P<0.05).[19] NA is not free of risk to the fetus, and about 4% of pregnant women who underwent NA experienced fetal loss, and the odds ratio of NA to fetal loss was a high as 1.88.[8] Negative appendectomy occurred in 1 out of 13 cases (7.7%) in this study. Acute appendicitis was probable on MRI but confirmed as normal appendix later in the pathology report. Lower rate of NA in this study than previous reports may be attributed to the pre-operative MRI. Although a direct comparison may not be possible, MRI may reduce unnecessary laparotomies.
Cobben et al[9] and Israel et al[20] reported the sensitivity of MRI for the diagnosis of acute appendicitis as 100%. Oto et al[21] reported the sensitivity, specificity, PPV, and NPV of MRI for acute appendicitis in pregnant patients as 90%, 98.1%, 81.8%, and 99.1%, respectively. In the study of Oto et al,[21] there were 2 false positive cases in which acute appendicitis was suspected on MRI but recovered without surgery, and 1 false negative case in which the appendix was not visualized on MRI but confirmed as acute appendicitis after surgery. The diagnostic performance of MRI for acute appendicitis in this study was similar to those of previous studies. The sensitivity, specificity, PPV, and NPV and accuracy of MRI for acute appendicitis in the pregnant patients in this study were 100%, 91.2%, 80%, 100% and 93.5%, respectively. There was 1 false positive case in which acute appendicitis was suspected on MRI but confirmed as normal appendix after surgery.
US is safe for both the mother and fetus and is reliable in confirming clinical diagnoses, and when read as positive, requires no further test other than surgery.[22] Some authors recommended the routine use of ultrasounds in every pregnant patient for better patient assessment.[23] Although the utility US is similar between pregnant and non-pregnant patients,[24] but the utility of US becomes lesser in latter stages of pregnancy as the gravid uterus gets bigger and the vessels become engorged, leading to inconclusive findings.[17,25,26] Several studies[17,19,20,25] reported non-visualization of the appendix in a large percentage of pregnant women with suspected acute appendicitis. Therefore, physicians should be aware of the limitation of US in excluding acute surgical diseases, and MRI must be considered as a primary imaging modality in latter stages of pregnancy or if the ultrasonographic findings are inconclusive.
Twenty-nine patients underwent appendix MRI after US in this study. These patients had inconclusive findings or non-visualization of the appendix on US. Further MRI studies could delineate normal appendix in 18 (62.1%) patients with inconclusive or non-visualization of the appendix on US. Furthermore, 2 cases of non-visualization of the appendix and 2 cases of probable appendicitis showed other non-surgical abnormal findings potentially related to abdominal pain. They recovered completely only with conservative management. Among the 29 pregnant patients who had inconclusive findings or non-visualization of the appendix on US, 22 (75.9%) patients could avoid unnecessary laparotomies. In contrast, those who showed ovarian torsion (n=1) and probable appendicitis without other abnormal findings (n=6) on MRI underwent surgery and all recovered in a timely manner. The usefulness of MRI cannot be overemphasized for challenging cases for diagnosis and treatment planning of acute appendicitis during pregnancy, and the routine use of MRI should be recommended for all pregnant patients with equivocal findings on US.
Exploratory laparoscopy has been used since 1910 as one of tools for diagnosing and treating appendicitis. Laparoscopy might reduce the frequencies of unnecessary appendectomies in 20%–30% and an accuracy of diagnosis of appendicitis of 95%–99%.[27] Bachar et al[28] reported slightly better sensitivity but worse specificity of laparoscopic appendectomy compared with imaging studies such as US or CT. Laparoscopy in pregnant with suspected appendicitis may lead to a lower rate of NA when compared with open appendectomy,[26] and the potential advantages of diagnostic and therapeutic laparoscopy were recently highlighted.[29] Early utilization of MRI along with laparoscopy approach should be considered in pregnant patients with suspected appendicitis.
Some blood tests turned out to be helpful in predicting acute surgical abdomen. WBC count, proportion of neutrophils in the WBC, NLR, and CRP and bilirubin levels were significantly higher in the patients who required surgical treatment. The best cut-off values to predict the acute surgical conditions were as follows: WBC≥11,000/mm3, neutrophil≥79.9%, NLR≥6.4 mg/dL, CRP≥1.82 and bilirubin≥0.66 mg/dL. These findings may alert clinicians of the increased possibility of acute surgical conditions and to expedite the diagnostic process when dealing with pregnant patients with acute abdominal pain. We suggests that MRI should be performed immediately for pregnant patients if the NLR is ≥6.4 or the proportion of neutrophils in the WBC is ≥79.9% regardless of the trimester. We also suggest that MRI may be deferred after US examination if the NLR is <6.4 or the proportion of neutrophils in the WBC is <79.9%, especially during the first trimester.
NLR has been introduced as the most reliable predictive marker (AUC: 0.836) among other blood tests, such as WBC or CRP, for acute appendicitis.[30] Kahramanca et al[31] reported that an NLR≥ 4.68 was associated with acute appendicitis, and an NLR≥ 5.74 was associated with complicated appendicitis. Yazar et al[25] reported that NLR and PLR could diagnose acute appendicitis with high accuracy (90.5%) in pregnant patients. In this study, NLR turned out to be the most reliable blood test parameter in predicting acute surgical abdomen, which is consistent with those of previous studies. The best cutoff value of NLR to predict the need for surgery among the pregnant patients who underwent MRI was 6.4 in current study. The higher cutoff value in this study compared to those of previous studies may be attributed to the increased absolute neutrophil count and decreased lymphocyte count during gestation.[32-34]
There are several limitations in this study. First, several radiologists interpreted the MRI findings during the study period, and inter-observer agreement was not obtained. Second, the study subjects included those who underwent appendix MRI and blood tests on the same day. The findings of this study may not represent the features of all pregnant patients with acute abdominal pain. Third, this is a retrospective study; therefore, the clinical features presented may not be reliable. However, the main findings of this study (MRI findings and laboratory findings) should not have been hampered by its retrospective design. Fourth, the time elapsed from symptom onset to the blood tests was not obtained and analyzed. Fifth, the sample size was not calculated prior to this study, and the number of subjects was relatively small. Overgeneralization of the findings of this study should be avoided.
CONCLUSION
Appendix MRI in pregnant patients could differentiate surgical conditions, such as acute appendicitis and ovarian torsion, from non-surgical conditions, such as red degeneration of uterine myoma and obstructive hydronephrosis. Clinicians may anticipate surgical conditions if pregnant patients complain of acute abdominal pain show WBC≥11,000/mm3, neutrophil≥79.9%, NLR≥6.4, or CRP≥1.82 in their blood tests, and should expedite the diagnostic process using MRI for such pregnant patients.
Footnotes
Funding: This article was not financially supported by any company or organization.
Ethical approval: The study was approved by the Institutional Review Board (IRB) of our hospital.
Conflict of interests: The authors declare that there is no competing interest related to the study, authors, other individual or organizations.
Contributors: JYJ and JUN contributed equally to this study. All authors read and approved the final version of the paper.
REFERENCES
- 1.Mahmoodian S. Appendicitis complicating pregnancy. South Med J. 1992;85(1):19–24. doi: 10.1097/00007611-199201000-00006. [DOI] [PubMed] [Google Scholar]
- 2.McGee TM. Acute appendicitis in pregnancy. Aust N Z J Obstet Gynaecol. 1989;29(4):378–85. doi: 10.1111/j.1479-828x.1989.tb01773.x. [DOI] [PubMed] [Google Scholar]
- 3.Mourad J, Elliott JP, Erickson L, Lisboa L. Appendicitis in pregnancy:new information that contradicts long-held clinical beliefs. Am J Obstet Gynecol. 2000;182(5):1027–9. doi: 10.1067/mob.2000.105396. [DOI] [PubMed] [Google Scholar]
- 4.Unal A, Sayharman SE, Ozel L, Unal E, Aka N, Titiz I, et al. Acute abdomen in pregnancy requiring surgical management:a 20-case series. Eur J Obstet Gynecol Reprod Biol. 2011;159(1):87–90. doi: 10.1016/j.ejogrb.2011.07.028. [DOI] [PubMed] [Google Scholar]
- 5.Franca Neto AH, Amorim MM, Nobrega BM. Acute appendicitis in pregnancy:literature review. Rev Assoc Med Bras (1992) 2015;61(2):170–7. doi: 10.1590/1806-9282.61.02.170. [DOI] [PubMed] [Google Scholar]
- 6.Tamir IL, Bongard FS, Klein SR. Acute appendicitis in the pregnant patient. Am J Surg. 1990;160(6):571–5. doi: 10.1016/s0002-9610(05)80748-2. [DOI] [PubMed] [Google Scholar]
- 7.Maslovitz S, Gutman G, Lessing JB, Kupferminc MJ, Gamzu R. The significance of clinical signs and blood indices for the diagnosis of appendicitis during pregnancy. Gynecol Obstet Invest. 2003;56(4):188–91. doi: 10.1159/000074450. [DOI] [PubMed] [Google Scholar]
- 8.McGory ML, Zingmond DS, Tillou A, Hiatt JR, Ko CY, Cryer HM. Negative appendectomy in pregnant women is associated with a substantial risk of fetal loss. J Am Coll Surg. 2007;205(4):534–40. doi: 10.1016/j.jamcollsurg.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 9.Cobben LP, Groot I, Haans L, Blickman JG, Puylaert J. MRI for clinically suspected appendicitis during pregnancy. AJR Am J Roentgenol. 2004;183(3):671–5. doi: 10.2214/ajr.183.3.1830671. [DOI] [PubMed] [Google Scholar]
- 10.Franca Neto AH, Amorim MM, Nobrega BM. Acute appendicitis in pregnancy:literature review. Rev Assoc Med Bras (1992) 2015;61(2):170–7. doi: 10.1590/1806-9282.61.02.170. [DOI] [PubMed] [Google Scholar]
- 11.Duke E, Kalb B, Arif-Tiwari H, Daye ZJ, Gilbertson-Dahdal D, Keim SM, et al. A systematic review and meta-analysis of diagnostic performance of MRI for evaluation of acute appendicitis. AJR Am J Roentgenol. 2016;206(3):508–17. doi: 10.2214/AJR.15.14544. [DOI] [PubMed] [Google Scholar]
- 12.Spalluto LB, Woodfield CA, DeBenedectis CM, Lazarus E. MR imaging evaluation of abdominal pain during pregnancy:appendicitis and other nonobstetric causes. Radiographics. 2012;32(2):317–34. doi: 10.1148/rg.322115057. [DOI] [PubMed] [Google Scholar]
- 13.Heinrichs WL, Fong P, Flannery M, Heinrichs SC, Crooks LE, Spindle A, et al. Midgestational exposure of pregnant BALB/c mice to magnetic resonance imaging conditions. Magn Reson Imaging. 1988;6(3):305–13. doi: 10.1016/0730-725x(88)90407-9. [DOI] [PubMed] [Google Scholar]
- 14.Tyndall DA, Sulik KK. Effects of magnetic resonance imaging on eye development in the C57BL/6J mouse. Teratology. 1991;43(3):263–75. doi: 10.1002/tera.1420430310. [DOI] [PubMed] [Google Scholar]
- 15.World Medical Association declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. JAMA. 1997;277(11):925–6. [PubMed] [Google Scholar]
- 16.Shuaib A, Shuaib A, Fakhra Z, Marafi B, Alsharaf K, Behbehani A. Evaluation of modified Alvarado scoring system and RIPASA scoring system as diagnostic tools of acute appendicitis. World J Emerg Med. 2017;8(4):276–280. doi: 10.5847/wjem.j.1920-8642.2017.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Di Saverio S, Birindelli A, Kelly MD, Catena F, Weber DG, Sartelli M, et al. WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg. 2016;11:34. doi: 10.1186/s13017-016-0090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andersson RE. The natural history and traditional management of appendicitis revisited:spontaneous resolution and predominance of prehospital perforations imply that a correct diagnosis is more important than an early diagnosis. World J Surg. 2007;31(1):86–92. doi: 10.1007/s00268-006-0056-y. [DOI] [PubMed] [Google Scholar]
- 19.Ito K, Ito H, Whang EE, Tavakkolizadeh A. Appendectomy in pregnancy:evaluation of the risks of a negative appendectomy. Am J Surg. 2012;203(2):145–50. doi: 10.1016/j.amjsurg.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 20.Israel GM, Malguria N, McCarthy S, Copel J, Weinreb J. MRI vs. ultrasound for suspected appendicitis during pregnancy. J Magn Reson Imaging. 2008;28(2):428–33. doi: 10.1002/jmri.21456. [DOI] [PubMed] [Google Scholar]
- 21.Oto A, Ernst RD, Ghulmiyyah LM, Nishino TK, Hughes D, Chaljub G, et al. MR imaging in the triage of pregnant patients with acute abdominal and pelvic pain. Abdom Imaging. 2009;34(2):243–50. doi: 10.1007/s00261-008-9381-y. [DOI] [PubMed] [Google Scholar]
- 22.Freeland M, King E, Safcsak K, Durham R. Diagnosis of appendicitis in pregnancy. Am J Surg. 2009;198(6):753–8. doi: 10.1016/j.amjsurg.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 23.Di Saverio S, Tugnoli G, Sofia S, Masetti M, Catena F, Ansaloni L, et al. Re:Appendectomy in pregnancy:evaluation of the risks of a negative appendectomy. Am J Surg. 2012;204(4):560–1. doi: 10.1016/j.amjsurg.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 24.Barloon TJ, Brown BP, Abu-Yousef MM, Warnock N, Berbaum KS. Sonography of acute appendicitis in pregnancy. Abdom Imaging. 1995;20(2):149–51. doi: 10.1007/BF00201525. [DOI] [PubMed] [Google Scholar]
- 25.Yilmaz HG, Akgun Y, Bac B, Celik Y. Acute appendicitis in pregnancy--risk factors associated with principal outcomes:a case control study. Int J Surg. 2007;5(3):192–7. doi: 10.1016/j.ijsu.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 26.Gaitan HG, Reveiz L, Farquhar C, Elias VM. Laparoscopy for the management of acute lower abdominal pain in women of childbearing age. Cochrane Database Syst Rev. 2014;(5):CD007683. doi: 10.1002/14651858.CD007683.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Andren-Sandberg A, Ryska M. Exploratory laparoscopy at suspicion of acute appendicitis. Rozhl Chir. 2004;83(3):131–7. [PubMed] [Google Scholar]
- 28.Ünlüer EE, Urnal R, Eser U, Bilgin S, Hacıyanlı M, Oyar O, et al. Application of scoring systems with point-of-care ultrasonography for bedside diagnosis of appendicitis. World J Emerg Med. 2016;7(2):124–9. doi: 10.5847/wjem.j.1920-8642.2016.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Di Saverio S. Emergency laparoscopy:a new emerging discipline for treating abdominal emergencies attempting to minimize costs and invasiveness and maximize outcomes and patients'comfort. J Trauma Acute Care Surg. 2014;77(2):338–50. doi: 10.1097/TA.0000000000000288. [DOI] [PubMed] [Google Scholar]
- 30.Tugnoli G, Giorgini E, Biscardi A, Villani S, Clemente N, Senatore G, et al. The NOTA study:non-operative treatment for acute appendicitis:prospective study on the efficacy and safety of antibiotic treatment (amoxicillin and clavulanic acid) in patients with right sided lower abdominal pain. BMJ Open. 2011;1(1):e000006. doi: 10.1136/bmjopen-2010-000006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kahramanca S, Ozgehan G, Seker D, Gokce EI, Seker G, Tunc G, et al. Neutrophil-to-lymphocyte ratio as a predictor of acute appendicitis. Ulus Travma Acil Cerrahi Derg. 2014;20(1):19–22. doi: 10.5505/tjtes.2014.20688. [DOI] [PubMed] [Google Scholar]
- 32.Kirkil C, Karabulut K, Aygen E, Ilhan YS, Yur M, Binnetoglu K, et al. Appendicitis scores may be useful in reducing the costs of treatment for right lower quadrant pain. Ulus Travma Acil Cerrahi Derg. 2013;19(1):13–9. doi: 10.5505/tjtes.2013.88714. [DOI] [PubMed] [Google Scholar]
- 33.Jeong JS, Ryu DH, Yun HY, Jeong EH, Choi JW, Jang LC. Laparoscopic appendectomy is a safe and beneficial procedure in pregnant women. Surg Laparosc Endosc Percutan Tech. 2011;21(1):24–7. doi: 10.1097/SLE.0b013e3182051e44. [DOI] [PubMed] [Google Scholar]
- 34.de Bakker JK, Dijksman LM, Donkervoort SC. Safety and outcome of general surgical open and laparoscopic procedures during pregnancy. Surg Endosc. 2011;25(5):1574–8. doi: 10.1007/s00464-010-1441-z. [DOI] [PubMed] [Google Scholar]


