Abstract
BACKGROUND:
Diagnostic imaging is an integral aspect of care that is often insufficient, if not altogether absent, in rural and remote regions of low to middle income countries (LMICs) such as Tanzania. The introduction of ultrasound can significantly impact treatment in these countries due to its portability, low cost, safety, and usefulness in various medical assessments. This study reviews the implementation of a four-week ultrasound course administered annually from 2013–2016 in a healthcare professional school in Mwanza, Tanzania by first-year allopathic US medical students.
METHODS:
Participants (n=582, over 4 years) were recruited from the Tandabui Institute of Health Sciences and Technology to take the ultrasound course. Subjects were predominantly clinical officer students, but other participants included other healthcare professional students, practicing healthcare professionals, and school employees. Data collected includes pre-course examination scores, post-course examination scores, course quiz scores, demographic surveys, and post-course feedback surveys. Data was analyzed using two-tailed t-tests and the single factor analysis of variance (ANOVA).
RESULTS:
For all participants who completed both the pre- and post-course examinations (n=229, 39.1% of the total recruited), there was a significant mean improvement in their ultrasound knowledge of 42.5%, P<0.01.
CONCLUSION:
Our data suggests that trained first-year medical students can effectively teach a point of care ultrasound course to healthcare professional students within four weeks in Tanzania. Future investigation into the level of long-term knowledge retention, impact of ultrasound training on knowledge of human anatomy and diagnostic capabilities, and how expansion of an ultrasound curriculum has impacted access to care in rural Tanzania is warranted.
Keywords: Point of care ultrasound, Ultrasound education, Tanzania
INTRODUCTION
In rural and remote regions of low to middle income countries (LMICs), socioeconomic disparities and a lack of trained healthcare providers contribute to difficulties in providing adequate primary care coverage. The World Health Organization (WHO) estimates that at least 2.5 physicians, nurses, and midwives per 1,000 people are required to provide sufficient coverage of primary care interventions.[1] In the United Republic of Tanzania, there are 0.031 physicians per 1,000 and 0.436 nurses and midwives per 1,000 people.[2,3] Diagnostic imaging is another integral aspect of care that is often insufficient, if not altogether absent, in rural and remote regions of LMICs.[4] The United Republic of Tanzania has 0.122 Computerized Tomography machines per 1,000,000 people and 0.041 Magnetic Resonance Imaging machines per 1,000,000.[5]
Due to its portability, relatively low cost, safety, and usefulness in various medical assessments, ultrasound has been proposed to help boost the diagnostic capacity of rural health care centers, such as in Mwanza, Tanzania, while cost-effectively utilizing scarce resources.[6-10] Studies have shown that the introduction of ultrasound can significantly impact treatment, increase the potential for long term clinical skills, and can be helpful during field medical operations.[9,11-16] After ultrasound was introduced to two rural hospitals in Rwanda, ultrasound findings changed the initial patient management plan in 43% of cases.[11] Also, at a tertiary care center in Monrovia, Liberia, ultrasound was found to have changed patient management in 62% of cases.[12] Studies have shown that 24-hour basic obstetric and point of care ultrasound (POCUS) could be implemented in a rural hospital setting, which would decrease the sonographer’s demand and improve patient care.[9] However, a major challenge in the implementation of diagnostic ultrasound in remote areas in LMICs is accessing adequate training for health professionals.[17,18]
Studies evaluating the efficacy of training healthcare professionals in the performance of ultrasound showed a high concordance rate (>90%) between trainee and radiologist assessment.[9,11] With the expansion of ultrasound into medical education, practitioners with minimal training can utilize point of care ultrasound (POCUS) to identify anatomy and pathology with high fidelity. There have been successful ultrasound training courses in LMICs that have varied in length and scope, including courses that have ranged in length from four days to nine weeks.[9] Trainees of these programs have included clinical officers, nurses, nurse midwives, and physicians.[9] In Tanzania, prior studies have demonstrated both the importance of ultrasound in austere settings and the success of training programs in rural Tanzanian hospitals and clinics.[19-21]
Previously, physician education in diagnostic sonography was withheld until residency and varied widely between specialties.[22] Physician time constraints create unique challenges for providing instruction for courses of long duration, thereby raising the question of whether instruction could be competently performed by medical students. Studies have shown that given proper means and instruction, pre-clinical medical students can obtain a level of understanding of ultrasonography comparable to a resident.[23-25]
This study reviews the implementation of a four-week ultrasound course administered annually from 2013–2016 in a healthcare professional school in Mwanza, Tanzania. We hypothesized that healthcare professional students can achieve basic ultrasound proficiency within 4 weeks following instruction by first-year, allopathic American medical students.
METHODS
Study design
We performed a prospective, observational study using a convenience sample of subjects recruited from the Tandabui Institute of Health Science and Technology (TIHEST) in Mwanza, Tanzania. The study was approved by the Institutional Review Board (IRB) with the support of TIHEST administration. We provided all participants with a study information sheet and obtained verbal consent. This study took place over four consecutive years, 2013–2016, with participant recruitment and curriculum implementation taking place over the course of 16 total weeks; four weeks each year.
Study protocol
Subject recruitment and pre-assessment
We recruited subjects using flyers and school-wide announcements at TIHEST prior to the arrival of the research team. Study subjects included clinical officer students, laboratory technician students, health informatics students, practicing healthcare professionals, and school employees.
We enrolled study participants in a four-week ultrasound course. Prior to initiation of the ultrasound curriculum, all participants were given a pre-course examination to determine baseline ultrasound competency. In 2015 and 2016, participants were asked to complete surveys for additional demographic information. The pre-course examination consisted of multiple-choice questions that assessed participants’ knowledge of basic diagnostic ultrasound, focusing on the topics presented in the curriculum. We informed all subjects that their performance on this examination did not affect their grade in the course.
Course instructor preparation
Course instruction was performed by U.S. based allopathic medical students who had just completed their first year of medical. Participating medical students volunteered to act as course instructors for this curriculum as part of a student organized annual international trip to Tanzania taking place in the summer between the first and second years of medical school instruction.
Prior to arriving in Tanzania, all course instructors had satisfied all requirements to pass the first-year medical school curriculum. Specifically, medical students had achieved passing grades in courses covering human physiology, human anatomy, and basic POCUS. The first-year medical student POCUS curriculum required ten hours of supervised hands-on training, in addition to pre-recorded podcasts that detailed POCUS imaging of eight separate organ systems. Topics included ultrasound physics and instrumentation, cardiac, hepatobiliary, renal, pulmonary, vascular, pelvic, and musculoskeletal ultrasound. Student POCUS competence was evaluated with written exams administered as a component of the clinical foundations curriculum for first year medical students, with a grade of 70% or greater required to achieve a pass.
Ultrasound curriculum
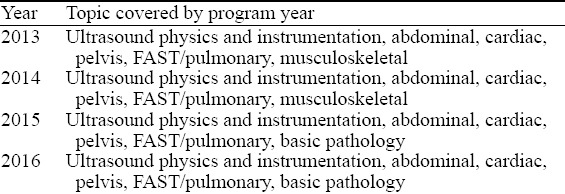
For the first three weeks we instructed subjects in ultrasound. During the fourth week we assessed each subject for their competency in window acquisition. Two teaching sessions took place each week for a total of six sessions. We began each session with a didactic lecture lasting 1–2 hours, which included ultrasound clips of pathologic examples in each application. This was followed by 1–2 hours of hands-on practice in small groups of three to ten participants led by instructors. Scans were performed using portable Sonosite Nanomaxx machines (Bothell, WA) utilizing the following three transducers: the phased array P21, curvilinear C60, and linear L38. During hands-on practice, healthy study participants also volunteered as human models for their classmates. We taught the following applications of POCUS: ultrasound physics and instrumentation, cardiac, abdominal, musculoskeletal, pulmonary, pelvic, and transabdominal obstetric ultrasound, as well as the Focused Assessment with Sonography in Trauma (FAST) exam. There were some variations in the topics presented each year, detailed in Table 1. We provided study guides in hard copy as well as copies of the lecture slides posted online for the students.
Table 1.
Ultrasound topic covered by program year
At the end of each week of instruction, we administered a written multiple-choice quiz in order to evaluate the participants’ knowledge on the topics that had been presented in the two sessions of that week. We curved the quiz grades based on the students’ answers and perceived language barriers. Following the quiz, we offered office hours which included hands-on practice to allow participants to review topics with the instructors.
The week following the last instructional session, we administered a final post-course examination made up of a written portion and a practical portion. The written portion consisted of multiple choice questions, of which a subset was identical to the pre-course evaluation administered prior to instruction. Static image examples of pathology were integrated into the written exam. The practical portion contained several focused stations. At each station, instructors directly observed whether subjects could independently acquire ultrasound views within three minutes. The course instructors determined the students’ scores by awarding points if the transducer was placed on the body in the correct location, in the correct orientation, and if they achieved the desired ultrasound view.
Subjects were graded with a composite of their attendance, their performance on the three weekly quizzes, and their final practical exam. A cumulative grade of 65% qualified as a “pass”. After completion of the course, the subjects completed a post-course feedback survey. In this survey, subjects rated which components of the class and which study materials they found most useful on a scale of 0 (corresponding to not useful at all) to 5 (corresponding to very useful) and provided general feedback.
Data collection and statistics
We collected data from the pre-course examination, course quiz scores, post-course final exam, demographic survey, and post-course survey. Statistical analysis was performed using R version 3.4.1.[26] A paired t-test was used to analyze the differences in the means between pre- and post-course examination scores. A two-way analysis of variance (ANOVA) was used to analyze the differences pre- and post-course exam scores for clinical officer students and non-clinical officer students in 2016. We also performed single factor ANOVA to analyze the difference in the means between reported usefulness of multiple course resources. A P value of < 0.05 was considered statistically significant.
RESULTS
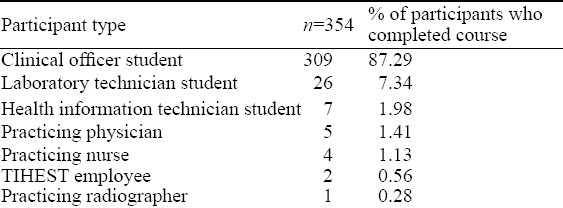
Between 2013–2016, 582 participants attended at least one ultrasound session and 354 (60.8%) participants completed the course (Figure 1). Most participants were clinical officer students (87.3%). Enrollment of practicing healthcare professionals and non-clinical officer students was low at 2.8% and 9.9%, respectively (Table 2). Age of participants ranged from 18 to 45 years old, and averaged 23 years and subjects were largely male (67.7%). Among responding participants in 2015, 95.7% (n=70) learned English as a second language.
Figure 1.
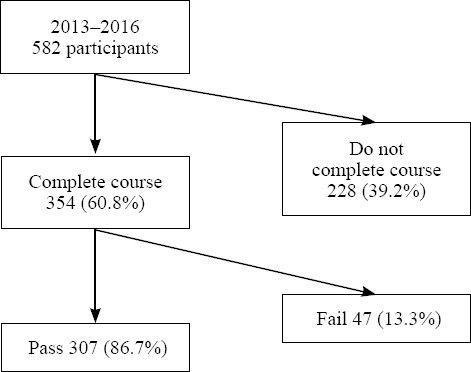
Four-year ultrasound course participation. Between 2013–2016, 354 of 582 (60.8%) participants completed the course. Of those who completed the course, 307 (86.7%) participants achieved a passing grade, and 47 (13.3%) participants did not achieve a passing grade.
Table 2.
Participants in ultrasound curriculum
Participation, attrition rates, and pass rates fluctuated by year, with pass rates of 92.7% in 2013, 84.0% in 2014, 95.6% in 2015, and 70.6% in 2016 (Figure 2). The 4-year pass rate was 86.7% (n=307). The number of students who attended a session but did not complete the course rose over the years: 12, 30, 76, and 112, respectively. The highest attrition rate was observed between the first session, when the pre-course test was administered and ultrasound physics and instrumentation was taught, and the second session.
Figure 2.
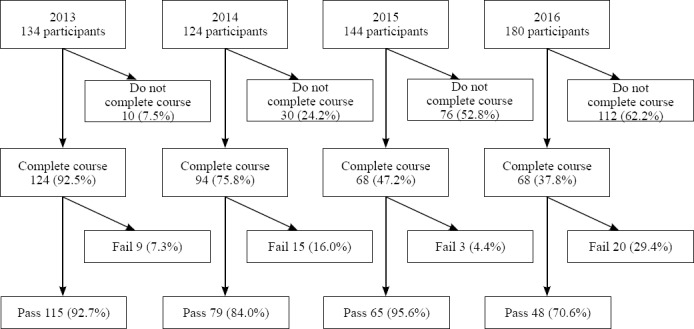
Course participation, segregated by year. Between 2013–2016, pass rates and participation fluctuated. Of the students who completed the course, the pass rate was 92.7% in 2013, 84.0% in 2014, 95.6% in 2015, and 70.6% in 2016.
For all participants who completed both the pre-course examination and the post-course examination (n=229) the mean pre-examination score was 29.9%, the mean post-course examination score was 72.4%, corresponding to a significant mean improvement of 42.5%, (P<0.01) (Figure 3). For participants who completed both the pre- and post-course examinations in 2013 (n=120), 2014 (n=55), and 2016 (n=54), there were significant mean improvements of 50.9% (P<0.01), 32.3% (P<0.01), and 34.1% (P<0.01) respectively. In 2015, the post-course final examination included 14 questions in addition to the pre-course examination. For participants who completed both the pre-course examination and post-course final examination in 2015 (n=63), the mean pre-course examination score was 33.2% and the mean post-course final examination score was 72.5%, corresponding to a mean improvement of 39.3%. Since the pre-course examination and post-course final exam in 2015 were not identical, this dataset was excluded from the pre-course examination vs. post-course examination analysis and figures.
Figure 3.
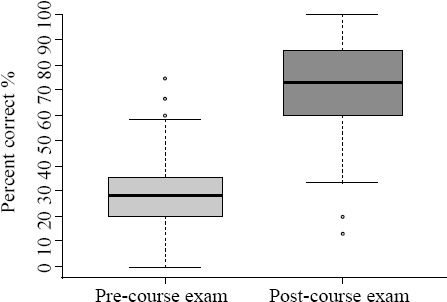
Overall pre- and post-course exam scores. Participants from 2013, 2014, and 2016 who completed both pre- and post-course examinations (n=229) demonstrated a significant improvement of 42.5% between combined pre-course and post-course exam scores (P< 0.01). Outliers are shown.
In 2016, non-clinical officer students who completed both the pre- and post-course examination (n=27) achieved a mean pre-course examination score of 29.4% and a significantly higher mean post-course examination score of 56.8% (P<0.01). Clinical officer students in 2016 who completed both the pre- and post-course examinations (n=27) achieved a mean pre-course examination score of 29.4% and a significantly higher mean post-course examination score of 70.1% (P<0.01). Of note, a two-way ANOVA demonstrated that the 2016 clinical officer students’ mean post-examination score was significantly higher than that of the non-clinical officer students (P<0.01) (Figure 4).
Figure 4.
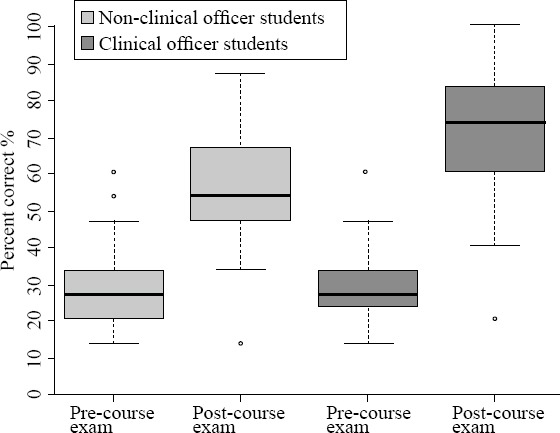
Clinical officer students vs. non-clinical health students in 2016. Non-clinical health student and clinical officer student pre-course and post-course exam scores are plotted on the X-axis, respectively. Percent correct is shown on the Y-axis. Both non-clinical officer students and clinical officer students scored significantly higher on the post-course exam than the pre-course exam (P<0.01). In addition, the clinical officer students had significantly higher post-course exam scores than non-clinical officer students (P<0.01). Outliers are shown.
Participants were also asked to rate the usefulness of various course resources for their ultrasound education on a scale of 0 to 5: classroom lectures, ultrasound scanning demonstrations by the instructor, active ultrasound scanning time, study guides from the instructors, and miscellaneous online resources (Figure 5). Participants rated instructor demonstration, active scanning, and classroom lectures the most useful and rated online materials and study guides the least useful (P<0.01). For general course feedback, participants most commonly requested additional active scanning time with a reduction in student to instructor ratio, additional accommodations for individuals less proficient in English, and an extension of the length and scope of the course.
Figure 5.
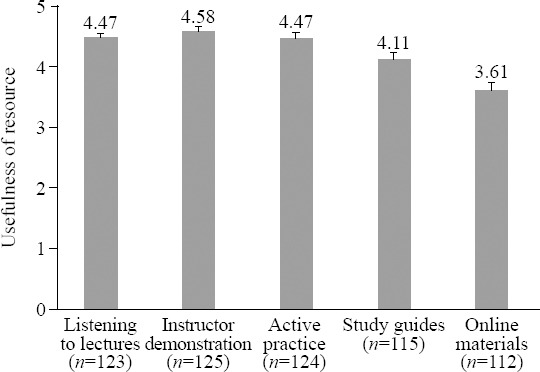
Post-course evaluation of various resources. After course completion, participants from 2015–2016 rated the usefulness of various resources from 0 to 5 for learning ultrasound (with 0 corresponding to not useful at all, and 5 corresponding to very useful). Instructor demonstration was found to be the most useful, and online materials the least useful (P<0.01). Resources and number of respondents (n) lie on the X-axis. Mean scores for each resource type lie above the standard error bars.
DISCUSSION
Our study aimed to determine if students at a healthcare professional school in Mwanza, Tanzania could achieve competency in basic ultrasound after completing an intensive 4-week course taught by ultrasound-trained pre-clinical allopathic medical students. The purpose was to introduce participants to ultrasound machine functionality, visualize anatomy that they had learned in textbooks, identify pathology, foster peer-to-peer learning, and to encourage additional ultrasound training in the future.
Between 2013–2016, 354 study participants completed the POCUS course taught by American first-year medical students. Most study participants achieved a passing grade. Study participants also demonstrated a significant improvement between pre- and post-course examinations. These results suggest acquisition of POCUS knowledge and supports the viability of this curriculum model. Participants demonstrated statistically significant improvement between pre- and post-course examinations in 2013, 2014, and 2016. In 2015, the post-course final examination included 14 questions in addition to the pre-course examination, but participants also demonstrated substantial improvement. Furthermore, most participants who completed the course each year achieved a “pass”. These results reflect the consistency and quality of the instructor training and teaching, despite changes in the instructor personnel every year.
Timing of the ultrasound curriculum and attrition
Communication failures and scheduling conflicts plagued the ultrasound curriculum and their effects are most prominently observed in the attrition rates nearing 40% across 2013–2016 (Figures 1 and 4). Summer break for first-year medical students partially overlaps with the break afforded to TIHEST students, and many TIHEST students voluntarily attended the course during their break, while others had familial obligations to attend to elsewhere. The highest attrition rates were observed between the first and the second sessions, when the pre-course exam was proctored and the ultrasound physics and instrumentation topic was covered. Student disappointment in their pre-course exam performance, having little prior knowledge of ultrasound, may have deterred students from returning to the second session.
Ultrasound curriculum in the setting of limited internet access
Students were unable to access online podcasts developed for this course due to the limited internet access of the student population. Over 75% of students at TIHEST reported access to internet was limited to once a week or less in 2014. Internet access for most students was infrequently available on the TIHEST campus computers, and rarely at their home. On the post-course survey, participants across multiple years rated online materials least useful of all available resources, reflecting the limited usefulness of internet resources without access. Until socioeconomic disparities are addressed such that robust internet access is made more widely available to students and their families, in-person sessions are the most effective way to teach POCUS in areas with limited internet access.
Optimizing ultrasound curriculum student population
Although practicing healthcare professionals were not excluded from the course, the primary goal of the study was to train future healthcare providers in POCUS techniques. Due to scheduling conflicts and a projected reduction in the participation of clinical officers, students from non-clinical tracks such as laboratory technician and health information technician were not excluded from participation. One readily important difference between these two tracks is that the clinical officers complete an anatomy course, without cadaveric dissection, while the other non-clinical tracks do not participate in a formal anatomy course. We found that clinical officer students had significantly better post-course examination scores than their non-clinical counterparts. While the ultrasound curriculum taught the non-clinical health students anatomy lessons and dispelled false rumors about ultrasound dangers circulating in their cohort, future efforts in training healthcare students in POCUS should prioritize their focus on clinical officer students to maximize future utilization of POCUS skills.
Limitations
There are several limitations to this study. There was some variance in topics presented each year, thereby limiting objective comparison between results obtained from participants each individual year. Basic pathology on ultrasound was taught using images and videos, as only healthy volunteer subjects were utilized for scanning practice. All didactic sessions were conducted in English, rather than Kiswahili, the official language of Tanzania. Hand-held portable ultrasound machines may not be able to produce as high quality images as cart-based machines. Additionally, there was no follow up to assess their retention of knowledge, which would have been more effective when assessing the efficacy of the course.[27]
The future of ultrasound in Mwanza, Tanzania
Over the course of 4 years, two ultrasound machines were donated to Mwanza clinics, increasing ultrasound access for the community. It is our hope that teaching healthcare students POCUS techniques will instill the desire to pursue ultrasound in later training and increase its utilization when providing care in rural communities. We also hope that these students can in turn teach their peers about ultrasound to turn this project into a local, self-sustaining part of their learning, which has proven to be more beneficial than being dependent on foreign programs.[28]
CONCLUSION
Our data suggests that trained first-year medical students can effectively teach a point of care ultrasound course to healthcare professional students within four weeks in Tanzania. By following this didactic model, wider implementation of ultrasound training for healthcare students can be achieved in low to middle income countries with limited internet access and countries with limited native English proficiency. Future investigation into the level of long-term knowledge retention of participants, how ultrasound training impacts knowledge of human anatomy, how point of care ultrasound knowledge impacts diagnostic capabilities and patient care, and how expansion of an ultrasound curriculum has impacted access to care in rural Tanzania, is warranted.
ACKNOWLEDGMENTS
UC Irvine Health Department of Emergency Medicine, UC Irvine School of Medicine.
Footnotes
Funding: None.
Ethical approval: The study was approved by the Institutional Review Board (IRB) with the support of TIHEST administration.
Conflicts of interest: Dr. J Christian Fox receives stock options from Sonosim for consulting. However, no Sonosim products were used in this research project.
Contributors: SPD proposed the study and wrote the first draft. All authors read and approved the final version of the paper.
REFERENCES
- 1.WHO. The World Health Report 2006 - Working Together for Health. Geneva, Switzerland: World Health Organization; 2006. [Google Scholar]
- 2.Physicians (per 1,000 people) |Data. Dataworldbankorg. 2017. [Accessed December 5 2016]. Available at: http://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=TZ .
- 3.Nurses and midwives (per 1,000 people) |Data. Dataworldbankorg. 2017. [Accessed December 5 2016]. Available at: http://data.worldbank.org/indicator/SH.MED.NUMW.P3?locations=TZ .
- 4.Ostensen H. Developing countries. Ultrasound Med Biol. 2000;26:S159–S161. doi: 10.1016/s0301-5629(00)00194-0. [DOI] [PubMed] [Google Scholar]
- 5.Global Atlas of Medical Devices - Tanzania, United Republic of 2014. [Accessed December 5 2016]. Available at: http://www.who.int/medical_devices/countries/tza.pdf .
- 6.Mindel S. Role of imager in developing world. The Lancet. 1997;350(9075):426–429. doi: 10.1016/S0140-6736(97)03340-0. [DOI] [PubMed] [Google Scholar]
- 7.Hoyer PF, Weber M. Ultrasound in developing world. The Lancet. 1997;350(9087):1330. doi: 10.1016/S0140-6736(05)62498-1. [DOI] [PubMed] [Google Scholar]
- 8.Steinmetz JP, Berger JP. Ultrasonography as an aid to diagnosis and treatment in a rural African hospital:a prospective study of 1 119 cases. Am J Trop Med Hyg. 1999;60(1):119–123. doi: 10.4269/ajtmh.1999.60.119. [DOI] [PubMed] [Google Scholar]
- 9.Sippel S, Muruganandan K, Levine A, Shah S. Use of ultrasound in the developing world. Int J Emerg Med. 2011;4:72. doi: 10.1186/1865-1380-4-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Felkel S. Ultrasound safety. J Diagn Med Sonogr. 1999;15(2):77–80. [Google Scholar]
- 11.Shah SP, Epino H, Bukhman G, Umulisa I, Dushimiyimana JM, Reichman A, et al. Impact of the introduction of ultrasound services in a limited resource setting:rural Rwanda 2008. BMC Int Health Hum Rights. 2009;9:4. doi: 10.1186/1472-698X-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kotlyar S, Moore CL. Assessing the utility of ultrasound in Liberia. J Emerg Trauma Shock. 2008;1(1):10–4. doi: 10.4103/0974-2700.41785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blaivas M, Kuhn W, Reynolds B, Brannam L. Change in differential diagnosis and patient management with the use of portable ultrasound in a remote setting. Wilderness Environ Med. 2005;16(1):38–41. doi: 10.1580/1080-6032(2005)16[38:ciddap]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 14.Spencer J, Adler R. Utility of portable ultrasound in a community in Ghana. J Ultrasound Med. 2008;27(12):1735–43. doi: 10.7863/jum.2008.27.12.1735. [DOI] [PubMed] [Google Scholar]
- 15.Henwood PC, Mackenzie DC, Rempell JS, Murray AF, Leo MM, Dean AJ, et al. A practical guide to self-sustaining point-of-care ultrasounz education programs in resource-limited settings. Ann Emerg Med. 2014;64(3):277–285.e2. doi: 10.1016/j.annemergmed.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 16.Nelson B, Melnick E, Li J. Portable ultrasound for remote environments, Part I:Feasibility of field deployment. J Emerg Med. 2011;40(2):190–7. doi: 10.1016/j.jemermed.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 17.LaGrone L, Sadasivam V, Kushner A, Groen RS. A review of training opportunities for ultrasonography in low and middle income countries. Trop Med Int Health. 2012;17(7):808–819. doi: 10.1111/j.1365-3156.2012.03014.x. [DOI] [PubMed] [Google Scholar]
- 18.Shah S, Bellows B, Adedipe A, Totten JE, Backlund BH, Sajed D. Perceived barriers in the use of ultrasound in developing countries. Crit Ultrasound J. 2015;7(1):28. doi: 10.1186/s13089-015-0028-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferraioli G, Meloni M. Sonographic Training program at a district hospital in a developing country:work in progress. Am J Roentgenol. 2007;189(3):W119–W122. doi: 10.2214/AJR.07.2202. [DOI] [PubMed] [Google Scholar]
- 20.Adler D, Mgalula K, Price D, Taylor O. Introduction of a portable ultrasound unit into the health services of the Lugufu refugee camp, Kigoma District, Tanzania. Int J Emerg Med. 2008;1(4):261–6. doi: 10.1007/s12245-008-0074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shaffer M, Brown H, McCoy C, Bashaka P. Evaluation of a short-term training program in bedside emergency ultrasound in southwestern Tanzania. J Ultrasound Med. 2017;36(3):515–521. doi: 10.7863/ultra.16.04006. [DOI] [PubMed] [Google Scholar]
- 22.Lee JB, Tse C, Keown T, Louthan M, Gabriel C, Anshus A, et al. Evaluation of a point of care ultrasound curriculum for Indonesian physicians taught by first-year medical students. World J Emerg Med. 2017;8(4):281–6. doi: 10.5847/wjem.j.1920-8642.2017.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Collins J, Riebe JD, Albanese MA, Dobos N, Heiserman K, Primack SL, et al. Medical students and radiology residents:Can they learn as effectively with the same educational materials? Acad Radiol. 1999;6(11):691–5. doi: 10.1016/S1076-6332(99)80119-6. [DOI] [PubMed] [Google Scholar]
- 24.Zaidman C, Wu JS, Wilder S, Darras BT, Rutkove SB. Minimal training is required to reliably perform quantitative ultrasound of muscle. Muscle Nerve. 2014;50(1):124–8. doi: 10.1002/mus.24117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bahner D, Adkins EJ, Hughes D, Barrie M, Boulger CT, Royall NA. Integrated medical school ultrasound:development of an ultrasound vertical curriculum. Crit Ultrasound J. 2013;5(1):6. doi: 10.1186/2036-7902-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.R:A Language And Environment For Statistical Computing. Vienna, Austria: R Development Core Team; 2016. [Google Scholar]
- 27.Baltarowich O, Goldberg BB, Wilkes AN, Anane-Firempong A, Veloski JJ. Effectiveness of “teaching the teachers” initiative for ultrasound training in Africa1. Acad Radiol. 2009;16(6):758–62. doi: 10.1016/j.acra.2008.12.023. [DOI] [PubMed] [Google Scholar]
- 28.Kawooya M. Training for rural radiology and imaging in sub-saharan africa:addressing the mismatch between services and population. J Clin Imaging Sci. 2012;2:37. doi: 10.4103/2156-7514.97747. [DOI] [PMC free article] [PubMed] [Google Scholar]


