Abstract
Objective
To ascertain the publication trends of interventions for paediatric kidney stone disease (KSD) we conducted a systematic review of literature over the last 16 years.
Patients and methods
With a rise of paediatric KSD and related interventions, a systematic review using PubMed was done over the last 16 years for all published papers on ‘Paediatric stone disease intervention – ureteroscopy (URS), shockwave lithotripsy (SWL), percutaneous nephrolithotomy (PCNL), open stone surgery, and laparoscopic stone surgery’. The search was limited to English language articles with a published abstract, whilst case reports, animal and laboratory studies, were excluded. We also analysed the data in two time periods, period-1 (2000–2007) and period-2 (2008–2015).
Results
During the last 16-years, 339 papers were published on paediatric stone disease intervention on PubMed. This included papers on URS (95), PCNL (97), SWL (102), open stone surgery (34) and laparoscopic stone surgery (11). During period-1 and period-2 there were 30 and 65 papers on URS, 16 and 81 papers on PCNL, 33 and 60 papers on SWL, nine and 25 papers on open surgery, respectively. When comparing the two periods, there were 92 published papers for all interventions in period-1 and this had risen almost threefold to 247 papers in period-2.
Conclusions
Our systematic review shows that intervention for KSD in the paediatric age group has risen over the last 8 years. Whilst URS, SWL, open surgery and laparoscopic surgery have all doubled, PCNL has risen fivefold reflecting an increase in the new minimally invasive PCNL techniques.
Abbreviations: KSD, kidney stone disease; MIST, minimally invasive surgical techniques; PCNL, percutaneous nephrolithotomy; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; SWL, shockwave lithotripsy; URS, ureteroscopy
Keywords: Publication trends, Urolithiasis, Stone, Ureteroscopy, Paediatrics
Introduction
Publication trends reflect changes in clinical practice and new surgical innovations. Over the last two decades, there has been a gradual rise in kidney stone disease (KSD) and related interventions in paediatric patients [1], [2], [3]. In certain parts of Europe, the Middle East and Asia, the incidence is quoted to be as high as 15% and can account for up to 4–8% of end-stage renal disease [4], [5]. This rise has been quoted to be fivefold due to improved diagnostic imaging, obesity, dietary and environmental factors, although most paediatric stones are also associated with metabolic and urinary tract anomalies [6].
The incidence and characteristics of stones show a wide geographical variation in children [3], [4]. With a high risk of recurrence, safe and effective treatment is paramount. Tailored management of paediatric stones often needs specialist paediatric centres and smaller instruments. Whilst historically the treatment of paediatric stones has been through open surgical removal, since the 1980s this has changed with the rise in shockwave lithotripsy (SWL) and other minimally invasive techniques (MIST) such as laparoscopy, percutaneous nephrolithotomy (PCNL), and ureteroscopy (URS).
Recent studies have shown a rise in the worldwide paediatric interventions for stone disease [7], [8]; however there is no bibliometric study looking at the publication trends on paediatric urolithiasis and aspects of treatment associated with it. Trends of publication reflect trends in treatments offered by clinicians and new surgical innovations, which are different in each era. To this end, we conducted a systematic review of the literature to investigate the publication trends on all surgical interventions for paediatric KSD as reported on PubMed over the last 16 years.
Patients and methods
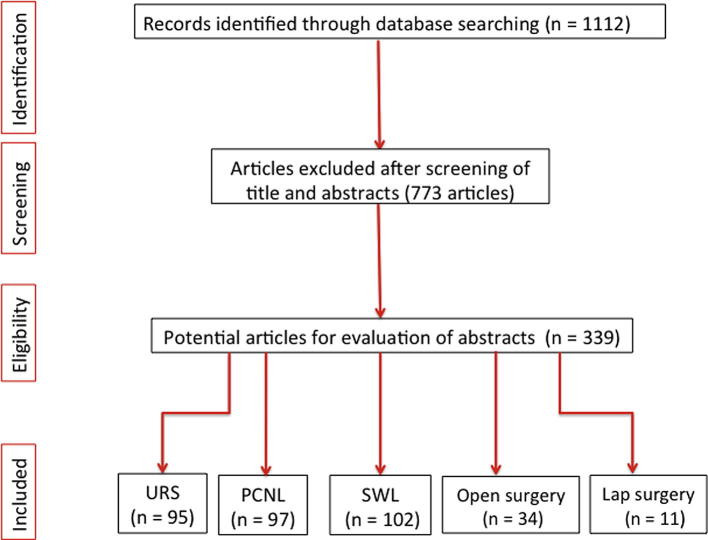
We conducted a systematic review of literature using PubMed over the last 16 years, from January 2000 to December 2015 for all published papers on interventions for ‘Paediatric Urolithiasis’ (Fig. 1).
Fig. 1.
PRISMA flowchart of the study.
Evidence acquisition: Criteria for including/excluding studies for this review
The inclusion criteria for our study were all English language studies reporting on surgical aspects of paediatric stone disease including: open surgery, laparoscopic surgery, SWL, PCNL and URS, whilst all non-English language studies and those without a published abstract were not included. Case reports, animal and laboratory studies were also not included.
Search strategy and study selection
The systematic review was performed according to the Cochrane Review and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The search strategy was conducted to find all relevant abstracts regarding each specific topic, which were analysed year by year from 2000 to 2015 (16-years). The specific terminology used was different for each topic: ‘Urolithiasis’, ‘kidney stones’, ‘renal stones’, ‘ureteric stones’, ‘paediatrics’, ‘kids’, ‘pediatrics’, ‘children’, ‘percutaneous nephrolithotomy’, ‘percutaneous stone surgery’, ‘PCNL’ and ‘PNL’, ‘ureteroscopy’, ‘URS’, ‘shockwave lithotripsy’, ‘extracorporeal shockwave lithotripsy’, ‘SWL’, ‘ESWL’, ‘lithotripsy’, ‘open stone surgery’, ‘laparoscopic surgery’, and ‘robotic surgery’.
These keywords were separately searched on PubMed amongst the literature published over the last 16-years from 2000 to 2015. Boolean operators (‘AND’, ‘OR’) were used to refine the search. Data were included for URS, PCNL, SWL, open stone surgery, and laparoscopic (including robotic surgery) stone surgery amongst paediatric studies.
We restricted our search to English language articles with published abstracts. To make an effective comparison and to identify and contrast different features, the data derived from each single research article were divided into two 8-year periods, period-1 (2000–2007) and period-2 (2008–2015). Data were collected using Microsoft Excel (version 2007) and analysed using the independent t-test and Pearson’s correlation coefficient, using the Statistical Package for the Social Sciences (SPSS®, version 24; SPSS Inc., IBM Corp., Armonk, NY, USA).
Results
During the initial PubMed database search 1112 records were identified and after screening of titles and abstracts, 773 were excluded. During the last 16 years, 339 papers were published on paediatric stone disease intervention, including URS (95), PCNL (97), SWL (102), open stone surgery (34) and laparoscopic stone surgery (11) (Fig. 1).
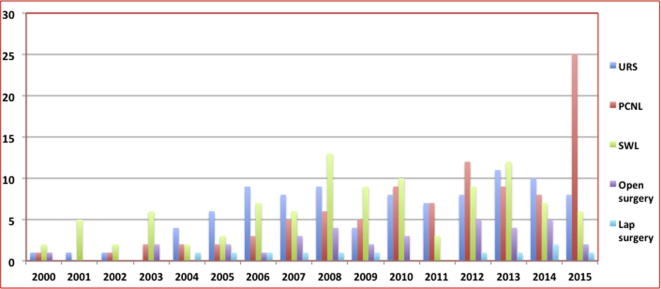
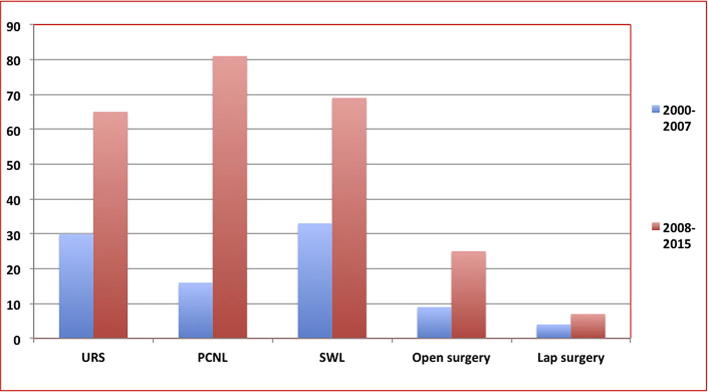
As can be seen in Fig. 2, Fig. 3, there have been dramatic changes in stone management over the last 16 years. Whilst URS, SWL, open surgery and laparoscopic surgery all doubled, PCNL rose five fold, reflecting an increase in the new PCNL MIST. Over the period as a whole, it is clear even if all techniques increased in different proportion, that the MIST such as PCNL, URS and SWL gradually overtook open surgery confirming their current supremacy. When comparing the two time periods, globally, 92 papers were published in period-1 and this rose almost three fold (+168%) to 247 papers in period-2 (Fig. 2).
Fig. 2.
Publication trends of various surgical options.
Fig. 3.
Publication trends over the two time periods.
URS
In all, 95 papers about paediatric URS were published on PubMed over the 16-year period. Based on an extrapolation of the data, there was a gradual increase in the publications of paediatric URS over the study period that has steadied to between eight and 11 papers published annually from 2010 onwards (Fig. 2). When comparing the two time periods, there was a total of 30 articles published in period-1, which had doubled (rise of 116%) to 65 articles in period-2 (P < 0.05) (Fig. 2, Fig. 3).
PCNL
In all, 97 studies on PCNL in paediatric patients were published on PubMed over the 16-year period. There was a linear increase in the rate of PCNL over the study period from one article in 2000 to 25 articles in 2015 (Fig. 2). This has been noticeable from 2008 onwards with more than six papers published annually, rising markedly to 25 papers in 2015. When comparing the two time periods, there were a total of 16 articles published in period-1, which had increased by almost five-times (rise of 406%) to 81 articles in period-2 (Fig. 3; P < 0.001). When looking at the newer PCNL MIST, during the last 6 years there were 17, eight and three papers on mini-PCNL, micro-PCNL and ultra-mini-PCNL respectively, with 16/28 (57%) in the last year alone.
SWL
In all, 102 studies on SWL in paediatric patients were published on PubMed over the 16-year period. The rates of SWL, despite some fluctuations, steadily increased over the study period (Fig. 2). When comparing the two time periods, there was a total of 33 articles published in period-1, which had increased by 109% to 69 articles in period-2 (Fig. 2, Fig. 3; P < 0.05).
Open surgery
During the last 16-years, 34 papers were published on open surgery for paediatric urolithiasis (Fig. 2). When comparing the two time periods, there were nine open surgery papers in period-1, which had increased to 25 in period-2 (Fig. 2, Fig. 3; P < 0.05).
Laparoscopic surgery
Over the study period, 11 papers were published on laparoscopic surgery for paediatric urolithiasis (Fig. 2). When comparing the two time periods, there were four laparoscopic surgery papers in period-1, which had increased to seven in period-2 (Fig. 3).
Discussion
Meaning of our study
This is one of the first bibliometric studies in the field of paediatric urolithiasis looking at publication trends over the last 16 years (2000–2015). There has been a significant rise in the total number of published papers (×2.7), with a rising trend in all interventions for stone disease. Over the period as a whole, the number of papers analysing paediatric stone surgery procedures witnessed dramatic changes, with the main features experiencing a significant increase not only in laparoscopy, URS and PCNL but also open surgery and SWL.
As can be seen from the global trend graph of interventions (Fig. 2, Fig. 3), at the end of this research period MIST, such as URS and PCNL, overtook SWL that used to predominate at the beginning of the period and became the most popular procedures for stone management in children. Whilst SWL remained the most popular intervention between 2000 and 2003, URS became more prominent between 2004 and 2007, and the last few years have seen a rapid rise in publications on PCNL.
European Association of Urology (EAU) paediatric stone guidelines
According to the 2016 EAU Guidelines [9], URS is recommended as the first-line treatment for distal ureteric stones and PCNL is recommended as the first-line treatment for staghorn stones, renal pelvic stones of >2 cm, and lower pole stones of >1 cm. However, for stones in all other locations SWL is recommended as the first-line treatment.
Similarly, whilst these guidelines recognise that MIST can manage most paediatric stones, they do acknowledge that there is a place for open surgery and laparoscopic surgery, especially in very young children or those with complex renal anatomy, body habitus or other concomitant pathology.
Change in worldwide trends for paediatric stone management
Renal stone management for children is usually dependent on several factors such as the number, location and size of stones, as well as the renal tract anatomy. A recent meta-analysis on the clinical efficacy of SWL shows that none of the 14 studies (1842 patients) were prospective in nature and there was significant heterogeneity of the included studies [10]. Outcomes showed significantly better results for stones of <1 cm, with 6% for steinstrasse and abdominal pain. Although SWL is meant to be less invasive compared to other MIST, paediatric patients frequently need a general anaesthesia for it, and with a rise in other forms of MIST, this seems to have taken a backseat in the recent years.
Technological advances, improved training and miniaturisation of the instrumentation have led to a sharp rise in URS and PCNL techniques worldwide [11]. Endoscopic MIST, such as mini-PCNL and URS, have recently been introduced and progressively adopted in paediatric patients in an increasing number of Urology centres [12]. Moreover, in one recent study, endourological management of all paediatric urolithiasis increased from 24.1% in the late 1980s/early 1990s to 99.8% from 2005 to 2010 [13]. These MIST have almost totally superseded open surgical treatment in adult patients, but this trend is becoming common even in children [14].
The major limitation of PCNL is its relatively higher morbidity, with serious complications such as significant bleeding and visceral injury, which can have devastating effects in the paediatric population. Due to these concerns about the size of the instruments, the patient’s body weight and the characteristics of the paediatric kidney (small size and hypermobile), reduced tract size has shown a lower morbidity compared to standard PCNL [15]. In response to these concerns, several percutaneous MIST approaches have been recently proposed and have been applied in paediatric cases: mini-PCNL, ultra-mini-PCNL, micro-PCNL [16]. According to our present study, the trend of PCNL treatment witnessed a significant increase over the last few years and this rise is likely to reflect the renewed interest towards miniaturised instruments and their wider field of application amongst the paediatric population. Of note, 16 of the 28 papers on miniaturised PCNL were published in the last year alone.
Strengths and weakness of bibliometric trend analysis
We used PubMed for bibliometric analysis of trends on management of paediatric urolithiasis over the last 16-years, as it gives a more realistic view of research trends in Endourology [17]. These show a rising trend of publications in interventions for paediatric stone disease. Although PubMed is an excellent source for bibliometric analysis, there are some journals that may not be indexed on PubMed [18]. We included only English language papers with published abstracts and whilst we captured the papers, a citation index or detailed co-author affiliation could not be established from PubMed, which might have provided more insight into these publication trends.
The design of the present study permits a worldwide assessment of publication trends on interventions for paediatric urolithiasis. The number of published papers in the second half (period-2) has increased significantly and this shows that innovations in MIST have led to a rise in popularity of these new techniques. It also highlights a growing popularity of the modern PCNL MIST for stone disease such as mini-, ultra-mini- and micro-PCNL, which use holmium laser for stone fragmentation [19]. Similarly, the use of URS has risen due to its feasibility and effectiveness in all age groups due to its minimally invasive profile, preservation of body integrity, and the relative absence of wounds or tubes [20]. Moreover, URS can directly access all stones throughout the urinary tract, regardless of location, and actively clear stone fragments regardless of stone size, whilst decreasing the morbidity associated with the active intervention [21].
Details on citation index, country or institution of origin of the study might provide more insight into future work in this area. This might also help in gathering the landmark papers in paediatric Endourology or in identifying self-citations and potential articles that were most cited in the literature [22]. Decreasing cost of procedures and improved training in Endourology will also help in the wider uptake of these procedures, whilst miniaturisation of the procedures will continue to improve its safety and efficacy [23], [24], [25], [26], [27].
The present study has certain limitations, which includes a lack of information on the number of patients per publication, multiple publications dealing with the same patients, and publications reporting on more than one technology that might also lead to over-representation of the paper dealing with techniques employed in few referral centres with specialised care.
Conclusion
Our present systematic review shows that over the last decade there seems to have been a rise in all forms of paediatric interventions for stone disease. In fact, whilst URS, SWL, open surgery and laparoscopic surgery have all doubled, PCNL has risen fivefold reflecting an increase in the new minimally invasive PCNL techniques for the treatment of upper urinary tract stones in children.
Conflict of interest
None.
Funding
No funding has been received for this paper.
Pediatric Urology
Footnotes
Peer review under responsibility of Arab Association of Urology.
References
- 1.Hernandez J.D., Ellison J.S., Lendvay T.S. Current trends, evaluation, and management of pediatric nephrolithiasis. JAMA Pediatr. 2015;169:964–970. doi: 10.1001/jamapediatrics.2015.1419. [DOI] [PubMed] [Google Scholar]
- 2.Sas D.J. An update on the changing epidemiology and metabolic risk factors in pediatric kidney stone disease. Clin J Am Soc Nephrol. 2011;6:2062–2068. doi: 10.2215/CJN.11191210. [DOI] [PubMed] [Google Scholar]
- 3.Rizvi S.A., Sultan S., Zafar M.N., Ahmed B., Aba Umer S., Naqvi S.A. Paediatric urolithiasis in emerging economies. Int J Surg. 2016;36:705–712. doi: 10.1016/j.ijsu.2016.11.085. [DOI] [PubMed] [Google Scholar]
- 4.Clayton D.B., Pope J.C. The increasing paediatric stone disease problem. Ther Adv Urol. 2011;3:3–12. doi: 10.1177/1756287211400491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sirin A., Emre S., Alpay H., Nayir A., Bilge I., Tanman F. Etiology of chronic renal failure in Turkish children. Paediatr Nephrol. 1995;9:549–552. doi: 10.1007/BF00860926. [DOI] [PubMed] [Google Scholar]
- 6.Bartosh S.M. Medical management of paediatric stone disease. Urol Clin North Am. 2004;31:575–587. doi: 10.1016/j.ucl.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Gnessin E., Chertin L., Chertin B. Current management of paediatric urolithiasis. Pediatr Surg Int. 2012;28:659–665. doi: 10.1007/s00383-012-3096-4. [DOI] [PubMed] [Google Scholar]
- 8.Geraghty R., Jones P., Somani B.K. Worldwide trends of urinary stone disease treatment over the last two decades: a systematic review. J Endourol. 2017;31:547–556. doi: 10.1089/end.2016.0895. [DOI] [PubMed] [Google Scholar]
- 9.Tekgül S., Dogan H.S., Hoebeke P., Kocvara R., Nijman J.M., Radmayr C. EAU Guidelines on Paediatric Urology. European Association of Urology; 2016. Available at: https://uroweb.org/wp-content/uploads/EAU-Guidelines-Paediatric-Urology-2016-1.pdf. Accessed October 2017. [DOI] [PubMed] [Google Scholar]
- 10.Lu P., Wang Z., Song R., Wang X., Qi K., Dai Q. The clinical efficacy of extracorporeal shockwave lithotripsy in paediatric urolithiasis: a systematic review. Urolithiasis. 2015;43:199–206. doi: 10.1007/s00240-015-0757-5. [DOI] [PubMed] [Google Scholar]
- 11.Oberlin D.T., Flum A.S., Bachrach L., Matulewicz R.S., Flury S.C. Contemporary surgical trends in the management of upper tract calculi. J Urol. 2015;193:880–884. doi: 10.1016/j.juro.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 12.Featherstone N.C., Somani B.K., Griffin S.J. Ureteroscopy and laser stone fragmentation (URSL) for large (≥1 cm) paediatric stones: Outcomes from a university teaching hospital. J Pediatr Urol. 2017;13:202.e1–202.e7. doi: 10.1016/j.jpurol.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 13.Onal B., Citgez S., Tansu N., Emin G., Demirkesen O., Talat Z. What changed in the management of pediatric stones after the introduction of minimally invasive procedures? A single-center experience over 24 years. J Pediatr Urol. 2013;9:910–914. doi: 10.1016/j.jpurol.2012.12.015. [DOI] [PubMed] [Google Scholar]
- 14.Rukin N.J., Siddiqui Z.A., Chedgy E.C., Somani B.K. Trends in upper tract stone disease in England: evidence from the Hospital Episodes Statistics (HES) database. Urol Int. 2017;98:391–396. doi: 10.1159/000449510. [DOI] [PubMed] [Google Scholar]
- 15.Guven S., Frattini A., Onal B., Desai M., Montanari E., Kums J. Percutaneous nephrolithotomy in children in different age groups: data from the Clinical Research Office of the Endourological Society (CROES) Percutaneous Nephrolithotomy Global Study. BJU Int. 2013;111:148–156. doi: 10.1111/j.1464-410X.2012.11239.x. [DOI] [PubMed] [Google Scholar]
- 16.Wright A., Rukin N., Smith D., De la Rosette J., Somani B.K. 'Mini, ultra, micro' – nomenclature and cost of these new minimally invasive percutaneous nephrolithotomy (PCNL) techniques. Ther Adv Urol. 2016;8:142–146. doi: 10.1177/1756287215617674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Falagas M.E., Pitsouni E.I., Malietzis G.A., Pappas G. Comparison of PubMed, scopus, web of science, and google scholar: strengths and weaknesses. FASEB J. 2008;22:338–342. doi: 10.1096/fj.07-9492LSF. [DOI] [PubMed] [Google Scholar]
- 18.Zyoud S.H., Al-Jabi S.W., Sweileh W.M. Worldwide research productivity of paracetamol (acetaminophen) poisoning: a bibliometric analysis (2003–2012) Hum Exp Toxicol. 2015;34:12–23. doi: 10.1177/0960327114531993. [DOI] [PubMed] [Google Scholar]
- 19.Karatag T., Tepeler A., Silay M.S., Bodakci M.N., Buldu I., Daggulli M. A Comparison of 2 percutaneous nephrolithotomy techniques for the treatment of pediatric kidney stones of sizes 10–20 mm: microperc vs miniperc. Urology. 2015;85:1015–1018. doi: 10.1016/j.urology.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 20.Ishii H., Griffin S., Somani B.K. Ureteroscopy for stone disease in the paediatric population: a systematic review. BJU Int. 2015;115:867–873. doi: 10.1111/bju.12927. [DOI] [PubMed] [Google Scholar]
- 21.Ishii H., Griffin S., Somani B.K. Flexible ureteroscopy and lasertripsy (FURSL) for paediatric renal calculi: Results from a systematic review. J Pediatric Urol. 2014;10:1020–1025. doi: 10.1016/j.jpurol.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 22.Schwartz S.P., Rehder K.J. Quality improvement in paediatrics: past, present, and future. Pediatr Res. 2017;81:156–161. doi: 10.1038/pr.2016.192. [DOI] [PubMed] [Google Scholar]
- 23.Somani B.K., Aboumarzouk O., Srivastava A., Traxer O. Flexible ureterorenoscopy: tips and tricks. Urol Ann. 2013;5:1–6. doi: 10.4103/0974-7796.106869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Somani B.K., Robertson A., Kata S.G. Decreasing cost of flexible ureterorenoscopic procedures: cost volume relationship. Urology. 2011;78:528–530. doi: 10.1016/j.urology.2010.12.073. [DOI] [PubMed] [Google Scholar]
- 25.Chapman A., Somani B.K., Robertson A., Kata S.G. Decreasing cost of flexible ureterorenoscopy. Single use laser fibre cost analysis. Urology. 2014;83:1003–1005. doi: 10.1016/j.urology.2013.12.019. [DOI] [PubMed] [Google Scholar]
- 26.Horuz R., Sarica K. The management of staghorn calculi in children. Arab J Urol. 2012;10:330–335. doi: 10.1016/j.aju.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Borgis S., Papatsoris A.G. Status quo of percutaneous nephrolithotomy in children. Urol Res. 2010;38:1–5. doi: 10.1007/s00240-009-0240-2. [DOI] [PubMed] [Google Scholar]