Abstract
The purpose of this clinical commentary is to review the anatomy, etiology, evaluation, and treatment techniques for nerve entrapments of the hip region. Nerve entrapment can occur around musculotendinous, osseous, and ligamentous structures because of the potential for increased strain and compression on the peripheral nerve at those sites. The sequela of localized trauma may also result in nerve entrapment if normal nerve gliding is prevented. Nerve entrapment can be difficult to diagnose because patient complaints may be similar to and coexist with other musculoskeletal conditions in the hip and pelvic region. However, a detailed description of symptom location and findings from a comprehensive physical examination can be used to determine if an entrapment has occurred, and if so where. The sciatic, pudendal, obturator, femoral, and lateral femoral cutaneous are nerves that can be entrapped and serve a source of hip pain in the athletic population. Manual therapy, stretching and strengthening exercises, aerobic conditioning, and cognitive-behavioral education are potential interventions. When conservative treatment is ineffective at relieving symptoms surgical treatment with neurolysis or neurectomy may be considered.
Level of Evidence
5
Keywords: Anatomy, etiology, evaluation, hip, nerve entrapment, treatment
Background and Purpose
Non-arthritic hip pain is area of increasing interest, particularly in field of sports medicine. Regional hip and pelvic pain can be difficult to diagnose and treat as symptoms can originate from osseous, capsulolabral, musculotendinous, and/or neurovascular structures. Intra-articular pathologies, such as labral tears and femoroacetabular impingement, and extra-articular pathologies, such as muscle strains and athletic pubalgia, have been clearly defined. However, nerve entrapments in the hip and pelvic region are sources of extra-articular symptoms that have not been well described.
Nerve entrapment can occur around musculotendinous, osseous, and ligamentous structures because of the potential for increased strain and compression on the peripheral nerve at those sites. The sequela of localized trauma may also result in nerve entrapment if normal nerve gliding is prevented. The mechanisms behind how peripheral nerve entrapment negatively affects nerve function is complex and thought to be related to local changes in vascular permeability, impairment of axonal transport, and the formation of edema.1-3 Individuals with nerve entrapment commonly complain of burning or lancinating type pain and/or paresthesia in the distribution of the involved nerve. It should be noted that neuralgia, a commonly used term, refers broadly to pain in the distribution of a nerve. Physical examination findings will vary depending on nerve function and can include impairments in sensation, reflexes, and/or motor function. Tinel's sign can be positive and recreate symptoms when the location of entrapment is superficial. Palpation may reveal localized tenderness in the area of entrapment and provocative movements that stretch the involved nerve are likely to reproduce symptoms. Diagnostic testing can include anesthetic injection, magnetic resonance imaging, ultrasonography, electromyography, and nerve conduction velocity tests.2
Identifying nerve entrapments in the hip and pelvic region can be difficult because of the similarity in symptoms and potential co-existence with other musculoskeletal conditions. In athletes, common nerve entrapments in this region include the sciatic, pudendal, obturator, femoral, and lateral femoral cutaneous nerves.4 In order to provide comprehensive treatment to young, active individuals, clinicians need to be aware of the potential location, clinical presentation, and treatment options for those with nerve entrapments in the hip region. The purpose of this clinical commentary is to review the anatomy, etiology, evaluation, and treatment techniques for nerve entrapments of the hip and pelvic region.
Posterior Nerve Entrapments
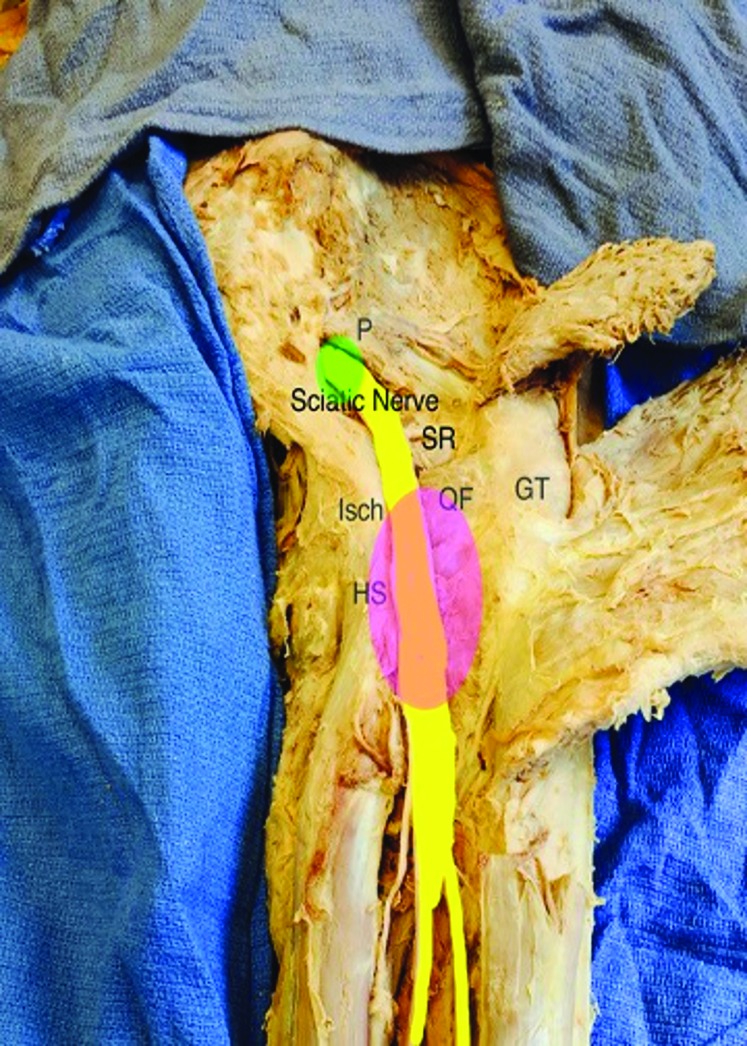
The sciatic and pudendal nerves are susceptible to entrapment in the posterior hip region. In the subgluteal space the sciatic nerve can be entrapped as it passes under piriformis and over the obturator, gemelli and/or quadratus femoris muscles.5 The sciatic nerve can be entrapped in ischiofemoral impingement between the ischium and lesser trochanter.6,7 Also at the level of the ischium, the proximal hamstring can be involved in sciatic nerve entrapment and is known as ischial tunnel syndrome.6,8(Figure 1) The pudendal nerve can be entrapped in several locations as it exits the greater sciatic foramen, travels over the sacrospinous ligament, traverses through the pudendal canal (also known as Alcock's canal) formed by the obturator fascia and sacrotuberous ligament, and emerges inferior to the pubic bone to innervate the perineum and genetalia.9,10 (Figure 2) The most common location of entrapment occurs in the space between the sacrospinous and sacrotuberous ligaments at the ischial spine. The obturator internus muscle may also compress the pudendal nerve medial to the ischium.10
Figure 1.
The Sciatic Nerve exits the Greater Sciatic Notch (green circle), inferior to the Piriformis (P) muscle, then travels over the short rotators (SR) and through the Ischiofemoral space (pink circle) formed by the Ischium (Isch) with the origin of the hamstring muscles (HS) and the lesser and greater trochanter (GT) of the femur.
Figure 2.
Pathway of the Pudendal Nerve (highlighted in yellow) that crosses over the sacrospinous ligament (SS), but deep to the sacrotuberous ligament (ST). GT = Greater Trochanter; P = piriformis; SN = Sciatic Nerve
The specific location of pain may help to identify the involved nerve and location source of entrapment. While those with sciatic nerve entrapment can have symptoms anywhere along the distribution of the sciatic nerve in the lower extremity, pain specifically in the buttock may indicate sciatic nerve entrapment. Individuals with sciatic nerve entrapment in the subgluteal space often present with a history of direct gluteal trauma and difficulty sitting for more than 30 minutes.5 Symptoms from ischiofemoral impingement typically occur during gait, when transitioning from mid-stance to terminal stance as the lesser trochanter contacts the ischium. This impingement may cause injury to the quadratus femoris and involve the sciatic nerve.11 In ischial tunnel syndrome, the origin of the hamstring tendon can be thickened due to trauma or partial hamstring avulsion and entrap the sciatic nerve.8 Symptoms radiating down the posterior thigh into popliteal fossa aggravated by running, with knee extension and hip flexion at heel strike, may indicate entrapment of the sciatic nerve in the ischial tunnel.6 Pudendal nerve entrapment results in pain medial to ischium, including the penis, scrotum, labia, perineum, and/or anorectal regions. These symptoms are generally made worse when sitting, except when sitting on a toilet seat. The area medial to ischium is not under compression when sitting on a toilet seat unlike sitting on a flat hard surface. Prolonged periods of cycling may be associated with pudendal nerve entrapment.10,12,13 Friction created in the pudendal canal from the repetitive nature of pedaling or direct compression of the nerve between the nose of the bicycle seat and pubic bone make cyclists susceptible to pathology of the pudendal nerve and its terminal motor and sensory branches.14
Physical exam for those with potential posterior nerve entrapments should include the seated palpation, seated piriformis stretch, active piriformis, ischiofemoral, and active knee flexion tests.6 The seated palpation test can be used to distinguish the source of entrapment based on location of tenderness. This test requires the patient to sit on the examiner's hand while the examiner simultaneously palpates three locations in the posterior hip: 1) the subgluteal space, lateral to the sacrum, in the area of deep hip external rotators; 2) the ischium and hamstring origin, and 3) the soft-tissue medial to the ischium.15 The seated piriformis stretch (Figure 3) and active piriformis test (Figure 4) can be used to identify those with sciatic nerve entrapment in the subgluteal space.16 A positive active piriformis test or seated piriformis stretch was found to identify those with sciatic nerve entrapment with sensitivity and specificity values of 0.91and 0.80, respectively, in subjects with posterolateral hip pain.16 The ischiofemoral impingement test assesses for reproduction of symptoms when the lesser trochanter contacts the ischium as the hip is moved into extension in an adducted and externally rotated position.17 (Figure 5) The sensitivity and specificity of this test for identifying individuals with ischiofemoral impingement in subjects with posterior hip pain were 0.82 and 0.85, respectively.7
Figure 3.
Seated Piriformis Stretch Test. The lower extremity is adducted and internally rotated while palpating the posterior hip region assessing for reproduction of symptoms in the area of palpation.
Figure 4.
Active Piriformis Test. The involved hip is abducted and externally rotated against resistance while palpating the posterior hip region assessing for reproduction of symptoms in the area of palpation.
Figure 5.
Ischiofemoral Impingement Test. Assess for reproduction of symptoms when the lesser trochanter contacts the ischium as the hip is moved into extension.
The active knee flexion tests at 30 ° and 90 ° have been described for assessment of proximal hamstring tendon pathology and ischial tunnel syndrome.6 These tests are performed while the patient is seated and their knee positioned in 30° flexion (Figure 6-A) and then in 90° flexion (Figure 6-B) with the examiner palpating the ischial tunnel. The patient actively flexes their knee for five seconds against resistance in each position with a positive test being reproduction of symptoms.6 A positive active knee flexion test at 30 ° or 90 ° was found to identify those with proximal hamstring pathology with sensitivity and specificity values of 0.84 and 0.97, respectively.31 It can be difficult to differentiate proximal hamstring pathology from ischial tunnel syndrome as the two conditions often occur together, particularly in more chronic situations. In the author's experience, ischial tunnel syndrome often have a positive active 30 ° knee flexion test with reproduction of radiating symptoms, although there is no evidence to support this suggestion.
Figure 6.
A. Active Knee Flexion Test at 30 °. B. The Active Knee Flexion Tests at 30 ° (Figure 6-A) and 90 °(Figure 6-B) have been describe to assess for proximal hamstring tendon pathology and ischial tunnel syndrome.
The physical examination for those with pudendal nerve entrapment is relatively benign with exception of pain reproduction.18,19 Careful palpation should be performed assessing for tenderness at the greater sciatic notch near the proximal aspect of the piriformis and medial to the ischium that may elicit symptoms from entrapment near the sacrospinous and sacrotuberous ligaments, the obturator internus muscle, and pudendal canal.18 A transvaginal or transrectal examination performed by an experienced pelvic health practitioner may be necessary to rule out intrapelvic entrapment. A summary of the common locations of posterior nerve entrapments as well as key subjective findings and signs are presented in Table 1.
Table 1.
Sites of Entrapment, Keys Signs and/or Symptoms with Nerves in the Anterior and Posterior Hip Region
| Posterior Nerve Entrapments | ||
|---|---|---|
| Involved Nerve | Common Site of Entrapment | Key Signs and/or Symptoms |
| Sciatic | Priformis and obturator internus/gemelli complex Proximal hamstring Lesser trochanter and Ischium |
Positive seated piriformis stretch and/or active piriformis tests Ischial tenderness Pain in the posterior thigh to the popliteal fossa aggravated with running Positive ischial femoral impingement test |
| Pudendal | Ischial spine, sacrospinous ligament, and lesser sciatic notch entrance Greater sciatic notch and piriformis Alcock's canal and obturator internus |
Pain medial to ischium Sciatic notch tenderness and piriformis muscle spasm and tenderness Obturator internus spasm and tenderness |
| Anterior Nerve Entrapments | ||
|---|---|---|
| Obturator | Obturator canal Adductor muscle fascia |
Pain in medial thigh Aggravation with movement into abduction |
| Femoral | Beneath iliopsoas tendon Inguinal ligament Adductor canal |
Reproduction of symptoms with modified Thomas test position Quadriceps muscle weakness Pain in the anteromedial knee joint, medial leg, and foot. |
| Lateral Femoral Cutaneous | Inguinal ligament | Positive pelvic compression test |
Anterior Nerve Entrapments
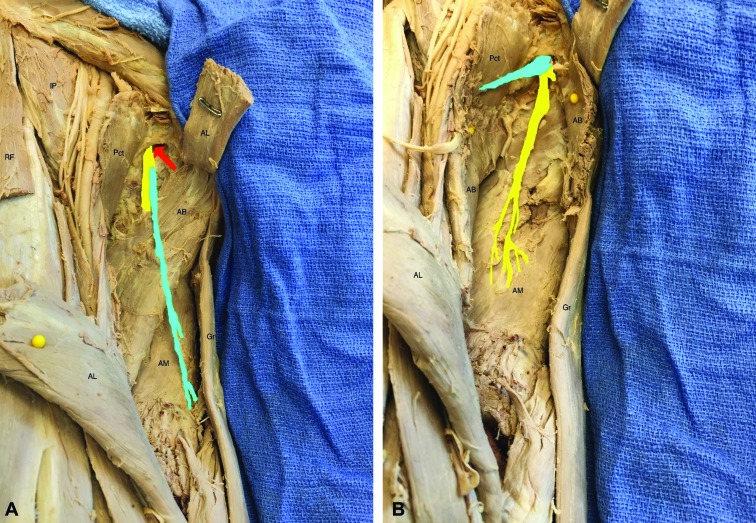
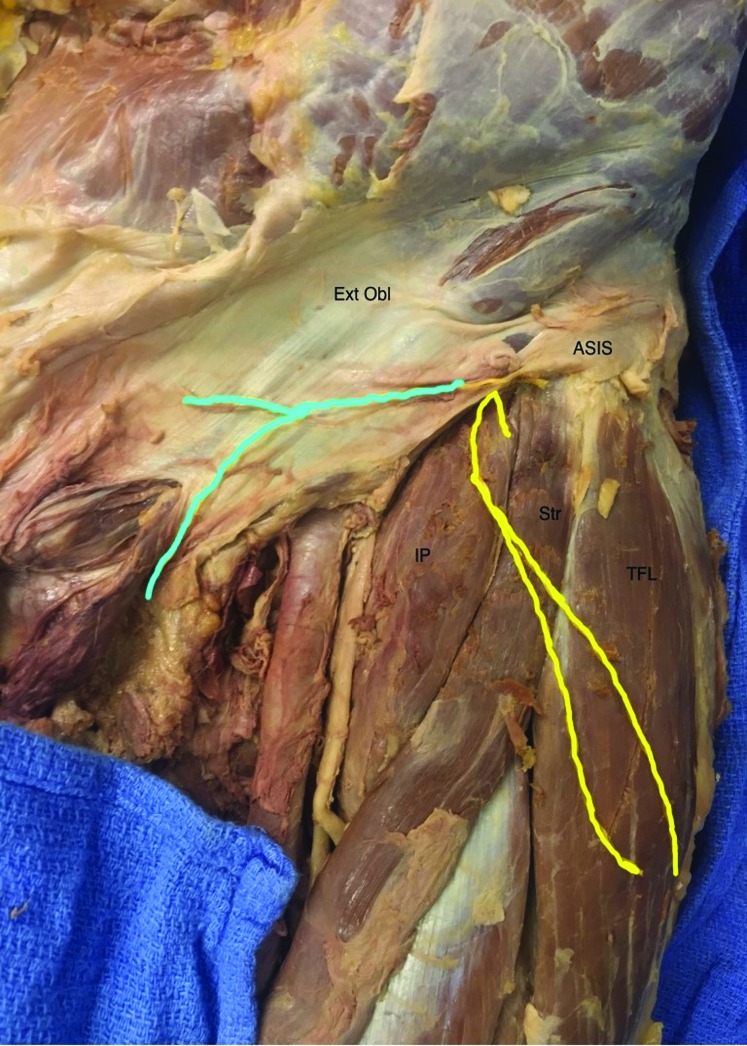
The obturator, femoral, and lateral femoral cutaneous are nerves that can be entrapped and serve as a source of symptoms in the anterior hip region. Although ilioinguinal, iliohypogastric, and genitofemoral nerve entrapment can occur, entrapment of these nerves is relatively rare, usually iatrogenic following surgery, and generally not directly related to sports or activity related injuries.4 The obturator nerve can be entrapped as it exits the obturator canal or more distally by fascia overlying the short adductor muscles.20(Figure 7) Entrapment of the femoral nerve can occur at the level of the inguinal ligament as it enters the femoral triangle.21 (Figure 8) Entrapment of the femoral nerve can occur in the iliacus compartment or adductor canal and involve the saphenous branch.21 The lateral femoral cutaneous nerve is commonly entrapped where it perforates the inguinal ligament approximately 2 cm medial to the anterior superior iliac spine.22-24(Figure 9)
Figure 7 A-B.
Pathway of the Obturator Nerve. The Obturator nerve divides into anterior (blue) and posterior branches (yellow) as it exits the obturator canal (red arrow) and enters into the thigh. IP=iliopsoas; Pct = Pectineus; RF = Rectus Femoris; AL = Adductor Longus; AB = Adductor Brevis; AM = Adductor Magnus; Gr = Gracilis.
Figure 8.
Pathway of the Femoral Nerve. The femoral nerve (yellow) passes posterior to the inguinal ligament (purple dotted line) , enters the femoral triangle, and sends branches to the pectineus, rectus femoris, and hip joint. As it continues, the femoral nerve divides into several branches which course superficial and deep to the sartorius (Str). The nerve innervates the sartorius, quadriceps, and the skin of the anterior and medial thigh. Str = Sartorius; IP = Iliopsoas; Pct = Pectineus; AL = Adductor Longus; RF = Rectus Femoris; VL = Vastus Lateralis; TFL = Tensor Fascia Lata
Figure 9.
Pathway of the Lateral Femoral Cutaneous Nerve. The lateral femoral cutaneous nerve (yellow) accesses the thigh approximately 2 cm medial to the anterior superior iliac spine (ASIS) and under the inguinal ligament and inferior to the iliohypogastric nerve (blue). The lateral femoral cutaneous nerve is an exclusively sensory nerve to the anterior and lateral aspect of the thigh. Str = Sartorius; IP = Iliopsoas; TFL = Tensor Fascia Lata; Ext Obl = External Abdominal Oblique; ASIS = Anterior Superior Iliac Spine
Athletes with obturator nerve entrapment typically present with exercise-induced medial thigh pain originating near the common origin of the adductor muscle group and radiating distally along the medial thigh.20,25 It should be noted these symptoms can be difficult to differentiate from isolated adductor tendinopathy. Subacute compartment syndrome resulting from pelvic trauma during contact sports can cause femoral nerve entrapment with progressive edema, swelling, and ischemia in the iliacus compartment.26-28 With femoral nerve entrapment pain, numbness, and paresthesias may be noted in the anterior thigh and when the saphenous branch is involved symptoms may be noted in the anteromedial knee joint, medial leg, and foot.4 In contrast, the lateral femoral cutaneous nerve is exclusively a sensory nerve with entrapment causing symptoms of paresthesia, numbness, stinging, or burning sensation in the anterior lateral thigh associated with hypersensitivity to touch.24 The symptoms associated with lateral femoral cutaneous nerve injury are commonly known as meralgia paresthetica.24 Female gymnasts may injure this nerve from repetitive trauma associated with uneven bar activities.4 Another sport-related cause of lateral femoral cutaneous nerve entrapment is seen in scuba divers where the weight belt worn around the waist directly compresses the nerve.4
A thorough physical examination should be performed in those with symptoms and a history suggestive of a nerve in the anterior hip region. Symptoms associated with obturator nerve entrapment include medial thigh symptoms aggravated by stretching into hip abduction and slight extension but not aggravated by resisted adduction and therefore inconsistent with adductor muscle involvement.20,25 The main clinical feature of patients with femoral nerve entrapment is quadriceps muscle weakness.29 Severe femoral nerve injury may produce quadriceps muscle atrophy and an absent patellar tendon reflex. Symptoms associated with femoral nerve entrapment are typically reproduced with movements of hip extension and knee flexion, such as with the Modified Thomas test position. A positive pelvic compression test and Tinel's sign can be used to identify those with lateral femoral cutaneous nerve entrapment.30 The pelvic compression test involves applying a downward force to the pelvis with the patient's symptomatic side facing up in side lying position in attempts to reduce tension on the inguinal ligament and relieve the patient's symptoms. This test was found to have 0.95 and 0.93 sensitivity and specificity values, respectively, when compared to neurophysiologic testing.30 A summary of the common locations of anterior nerve entrapments as well as subjective findings and signs are also presented in Table 1.
Conservative Treatment
Similar to diagnosing, treating those with nerve entrapment in the hip and pelvic region may be challenging as intervention strategies have not been well studied. Manual therapy, stretching and strengthening exercises, aerobic conditioning, and cognitive-behavioral education are potential interventions.2,31 A thorough examination and comprehensive treatment program should also asses for and direct treatment at abnormal movement patterns that effect the hip and pelvis. This would include abnormal kinematic motion secondary to osseous pathologies, such as femoroacetabular and ischiofemoral impingement, as well as other soft-tissue causes of flexion and/or extension range of motion restrictions of the hip.
Neural gliding or mobilization is a manual therapy technique that attempts to improve neurodynamics by restoring the balance between the relative movements of the nerve and surrounding structures.2 Although there is limited of evidence to support nerve mobilization for lower extremity entrapments, the hypothesized benefits from these techniques include facilitation of nerve gliding, reduction of nerve adherence, dispersion of noxious fluids, reduction of intraneural edema, increased neural vascularity, and improvement of axoplasmic flow.2 These techniques may also effect central mechanisms by decreasing nociceptive behavior in the spinal cord.2 Neural mobilization requires knowledge of the nerve pathway and movement that applies tension to the specific nerve. For example, sciatic nerve mobilization would combine movements of hip flexion, knee extension, and ankle dorsiflexion while femoral nerve mobilization would combine hip extension and knee flexion.
Manual therapy interventions in the form of soft-tissue mobilization can also be directed to musculotendinous structures affecting the nerve. Although there is limited of evidence to support soft-tissue mobilization for lower extremity nerve entrapments, these techniques can address goals of increasing range of motion, reducing pain, decreasing swelling, increasing flexibility, and/or improving muscle performance. Traditional massage strokes of effleurage, petrissage, and deep friction can be included as soft-tissue mobilization techniques.32 Other techniques may include soft tissue mobilization in conjunction with active patient movement.33 Soft-tissue mobilization can also include the use of specialized instruments in treatment administration. These instruments used during assisted soft-tissue mobilization techniques attempt to induce biological changes to affect scar tissue and to stimulate the regeneration of soft tissues.34 These techniques may also try to mechanically mobilize tissues that are restricting nerve gliding.35
In addition to manual therapy techniques, stretching and strengthening exercises, aerobic conditioning, and cognitive-behavioral education have been shown to be valuable in the treatment of those with nerve entrapments in the hip region.31 Stretching, whether performed independently by a patient or performed by a physical therapist, attempts to relieve nerve compression by lengthening shortened musculotendinous structures. However, aggressive stretching can be irritating to the nerve and must be controlled in a slow and progressive manner. One specific exercise for the sciatic nerve involves the combined passive movements of hip flexion, abduction, and external rotation to symptoms provocation followed by movements of hip adduction, internal rotation, and extension. (Figure 10) Although there no evidence to support the technique, this movement combination is purported to mobilize the sciatic nerve in the deep gluteal region. Strengthening exercises can also be performed to facilitate proper load transfer between the lumbosacral spine, pelvis, hip, and lower extremity when alterations or deficiencies of these relationships have been identified.2 For those with chronic pelvic pain, non-symptom provoking strengthening and training of the pelvic floor muscles is recommended.36 Aerobic conditioning can be useful because of the general positive effect it has on overall pain management. Cognitive behavioral therapy may assist an individual to gain a sense of control over pain by providing an understanding of pain mechanisms and coping strategies.2,31,37,38
Figure 10A-B.
Exercise to mobilize the sciatic nerve. This exercise involves the combined movements of hip flexion, abduction, and external rotation to symptoms provocation followed by movements of hip adduction, internal rotation, and extension.
Surgical Treatment
When conservative treatment, including injections, is ineffective at relieving symptoms associated with nerve entrapment, surgical treatment with neurolysis or neurectomy may be considered.39 Neurolysis involves surgical decompression and removal of adhesions that are causing the nerve entrapment. In cases where the nerve is being compressed by a hematoma, cyst, or bursea, surgical or percutaneous drainage may be necessary. Neuroectomy involves surgical lysis of the involved nerve and may have better long-term results in some cases. For example, neurectomy was found to be more effective in relieving pain with lower recurrence when compared to neurolysis in cases of meralgia paresthetica.40,41 Many of these procedures which were commonly performed with open approaches are now able to be performed using arthroscopic techniques.5
Conclusion
Nerve entrapments in the hip and pelvic region are sources of extra-articular symptoms in athletes and have not been well described. Entrapment of the sciatic, pudendal nerves, obturator, femoral and lateral femoral cutaneous are potential causes of hip pain. A detailed description of symptom location combined with physical examination findings can be used to identify the site of entrapment. Although not well defined, conservative intervention strategies can include soft-tissue and nerve mobilization, controlled stretching and strengthening exercises, aerobic conditioning, and cognitive-behavioral education. Surgical treatment with neurolysis or neurectomy can be considered in those with recalcitrant symptoms.
REFERENCES
- 1.Schmid AB Coppieters MW. The double crush syndrome revisited--a Delphi study to reveal current expert views on mechanisms underlying dual nerve disorders. Man ther. 2011;16:557-562. [DOI] [PubMed] [Google Scholar]
- 2.Schmid AB Nee RJ Coppieters MW. Reappraising entrapment neuropathies--mechanisms, diagnosis and management. Man ther. 2013;18:449-457. [DOI] [PubMed] [Google Scholar]
- 3.Dahlin LB. Aspects on pathophysiology of nerve entrapments and nerve compression injuries. Neurosurg Clin N Am. 1991;2:21-29. [PubMed] [Google Scholar]
- 4.McCrory P Bell S. Nerve entrapment syndromes as a cause of pain in the hip, groin and buttock. Sports Med. 1999;27:261-274. [DOI] [PubMed] [Google Scholar]
- 5.Martin HD Shears SA Johnson JC Smathers AM Palmer IJ. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy. 2011;27:172-181. [DOI] [PubMed] [Google Scholar]
- 6.Martin HD Khoury A Schroder R Palmer IJ. Ischiofemoral Impingement and Hamstring Syndrome as Causes of Posterior Hip Pain: Where Do We Go Next? Clin Sports Med. 2016;35:469-486. [DOI] [PubMed] [Google Scholar]
- 7.Kivlan BR Martin RL Martin HD. Ischiofemoral impingement: defining the lesser trochanter-ischial space. Knee Surg Sports Traumatol Arthrosc. 2017;25:72-76. [DOI] [PubMed] [Google Scholar]
- 8.Gomez-Hoyos J Reddy M Martin HD. Dry Endoscopic-Assisted Mini-Open Approach With Neuromonitoring for Chronic Hamstring Avulsions and Ischial Tunnel Syndrome. Arthrosc Tech. 2015;4:e193-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loukas M Louis RG, Jr. Hallner B Gupta AA White D. Anatomical and surgical considerations of the sacrotuberous ligament and its relevance in pudendal nerve entrapment syndrome. Surg Radiol Anat. 2006;28:163-169. [DOI] [PubMed] [Google Scholar]
- 10.Ploteau S Perrouin-Verbe MA Labat JJ Riant T Levesque A Robert R. Anatomical Variants of the Pudendal Nerve Observed during a Transgluteal Surgical Approach in a Population of Patients with Pudendal Neuralgia. Pain Physician. 2017;20:E137-E143. [PubMed] [Google Scholar]
- 11.Hernando MF Cerezal L Perez-Carro L Canga A Gonzalez RP. Evaluation and management of ischiofemoral impingement: a pathophysiologic, radiologic, and therapeutic approach to a complex diagnosis. Skeletal Radiol. 2016;45:771-787. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy J. Neurologic injuries in cycling and bike riding. Neurol clin. 2008;26:271-279. [DOI] [PubMed] [Google Scholar]
- 13.Possover M. Laparoscopic management of endopelvic etiologies of pudendal pain in 134 consecutive patients. J Urol. 2009;181:1732-1736. [DOI] [PubMed] [Google Scholar]
- 14.Leibovitch I Mor Y. The vicious cycling: bicycling related urogenital disorders. Eur Urol. 2005;47:277-286. [DOI] [PubMed] [Google Scholar]
- 15.Martin HD Reddy M Gomez-Hoyos J. Deep gluteal syndrome. J Hip Preserv Surg. 2015;2:99-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin HD Kivlan BR Palmer IJ Martin RL. Diagnostic accuracy of clinical tests for sciatic nerve entrapment in the gluteal region. Knee Surg Sports Traumatol Arthrosc. 2014;22:882-888. [DOI] [PubMed] [Google Scholar]
- 17.Hatem MA Palmer IJ Martin HD. Diagnosis and 2-year outcomes of endoscopic treatment for ischiofemoral impingement. Arthroscopy. 2015;31:239-246. [DOI] [PubMed] [Google Scholar]
- 18.Labat JJ Riant T Robert R Amarenco G Lefaucheur JP Rigaud J. Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourol Urodyn. 2008;27:306-310. [DOI] [PubMed] [Google Scholar]
- 19.Ploteau S Cardaillac C Perrouin-Verbe MA Riant T Labat JJ. Pudendal Neuralgia Due to Pudendal Nerve Entrapment: Warning Signs Observed in Two Cases and Review of the Literature. Pain Physician. 2016;19:E449-454. [PubMed] [Google Scholar]
- 20.Bradshaw C McCrory P Bell S Brukner P. Obturator nerve entrapment. A cause of groin pain in athletes. Am J Sports Med. 1997;25:402-408. [DOI] [PubMed] [Google Scholar]
- 21.Petchprapa CN Rosenberg ZS Sconfienza LM Cavalcanti CF Vieira RL Zember JS. MR imaging of entrapment neuropathies of the lower extremity. Part 1. The pelvis and hip. Radiographics. 2010;30:983-1000. [DOI] [PubMed] [Google Scholar]
- 22.Grossman MG Ducey SA Nadler SS Levy AS. Meralgia paresthetica: diagnosis and treatment. J Am Acad Orthop Surg. 2001;9:336-344. [DOI] [PubMed] [Google Scholar]
- 23.Lee SH Shin KJ Gil YC Ha TJ Koh KS Song WC. Anatomy of the lateral femoral cutaneous nerve relevant to clinical findings in meralgia paresthetica. Muscle Nerve. 2017;55:646-650. [DOI] [PubMed] [Google Scholar]
- 24.Cheatham SW Kolber MJ Salamh PA. Meralgia paresthetica: a review of the literature. Int J Sports Phys Ther. 2013;8:883-893. [PMC free article] [PubMed] [Google Scholar]
- 25.Tipton JS. Obturator neuropathy. Curr Rev Musculoskelet Med. 2008;1:234-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murray IR Perks FJ Beggs I Moran M. Femoral nerve palsy secondary to traumatic iliacus haematoma--a young athlete's injury. BMJ Case Rep. 2010;2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chambers S Berg AJ Lupu A Jennings A. Iliacus haematoma causing femoral nerve palsy: an unusual trampolining injury. BMJ Case Rep. 2015;2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pirouzmand F Midha R. Subacute femoral compressive neuropathy from iliacus compartment hematoma. Can J Neurol Sci. 2001;28:155-158. [DOI] [PubMed] [Google Scholar]
- 29.Kuntzer T van Melle G Regli F. Clinical and prognostic features in unilateral femoral neuropathies. Muscle Nerve. 1997;20:205-211. [DOI] [PubMed] [Google Scholar]
- 30.Nouraei SA Anand B Spink G O’Neill KS. A novel approach to the diagnosis and management of meralgia paresthetica. Neurosurgery. 2007;60:696-700. [DOI] [PubMed] [Google Scholar]
- 31.Schroder RG Martin RL Bobb VL Khoury NK Palmer IJ Martin HD. Outcomes of non-operative management of Deep Gluteal Syndrome – A Case Series of six Patients. J Musculoskelet Disord Treat. 2016;2:012. [Google Scholar]
- 32.Brummitt J. The role of massage in sports performance and rehabilitation: current evidence and future direction. N Am J Sports Phys Ther. 2008;3:7-21. [PMC free article] [PubMed] [Google Scholar]
- 33.Drover JM Forand DR Herzog W. Influence of active release technique on quadriceps inhibition and strength: a pilot study. J Manipulative Physiol Ther. 2004;27:408-413. [DOI] [PubMed] [Google Scholar]
- 34.McCormack JR. The management of bilateral high hamstring tendinopathy with ASTYM(R) treatment and eccentric exercise: a case report. J Man Manip Ther. 2012;20:142-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Looney B Srokose T Fernandez-de-las-Penas C Cleland JA. Graston instrument soft tissue mobilization and home stretching for the management of plantar heel pain: a case series. J Manipulative Physiol Ther. 2011;34:138-142. [DOI] [PubMed] [Google Scholar]
- 36.George SE Clinton SC Borello-France DF. Physical therapy management of female chronic pelvic pain: Anatomic considerations. Clin Anat. 2013;26:77-88. [DOI] [PubMed] [Google Scholar]
- 37.Perez-Lopez FR Hita-Contreras F. Management of pudendal neuralgia. Climacteric. 2014;17:654-656. [DOI] [PubMed] [Google Scholar]
- 38.Elkins N Hunt J Scott KM. Neurogenic Pelvic Pain. Phys Med Rehabil Clin N Am. 2017;28:551-569. [DOI] [PubMed] [Google Scholar]
- 39.Viswanathan A Kim DH Reid N Kline DG. Surgical management of the pelvic plexus and lower abdominal nerves. Neurosurgery. 2009;65:A44-51. [DOI] [PubMed] [Google Scholar]
- 40.van Eerten PV Polder TW Broere CA. Operative treatment of meralgia paresthetica: transection versus neurolysis. Neurosurgery. 1995;37:63-65. [DOI] [PubMed] [Google Scholar]
- 41.de Ruiter GC Wurzer JA Kloet A. Decision making in the surgical treatment of meralgia paresthetica: neurolysis versus neurectomy. Acta neurochirurgica. 2012;154:1765-1772. [DOI] [PubMed] [Google Scholar]