Abstract
Objectives:
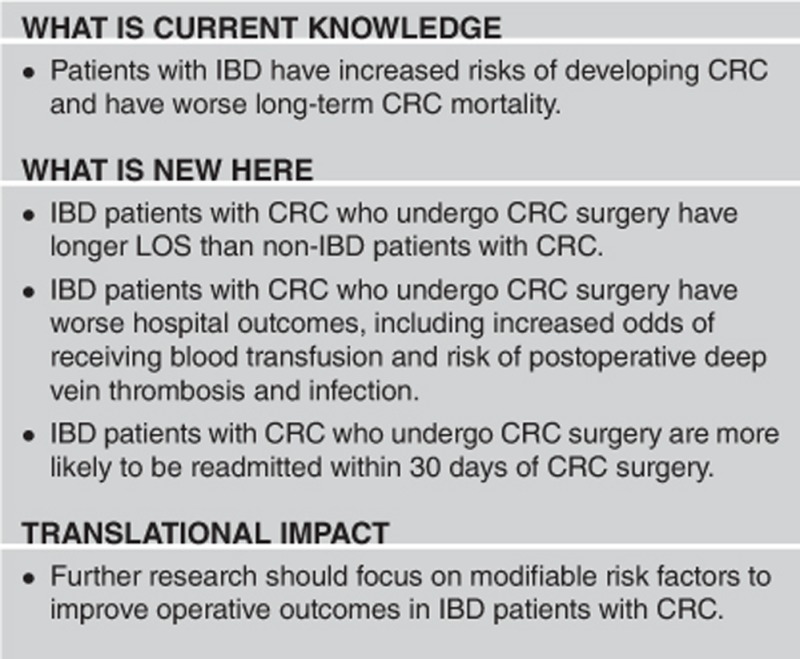
Inflammatory bowel disease (IBD) is associated with an increased risk of colorectal cancer (CRC) compared to patients without IBD. There is a lack of population-based data evaluating the in-patient surgical outcomes of CRC in IBD patients. We sought to compare the hospital outcomes of CRC surgery between patients with and without IBD.
Methods:
We used the National Inpatient Sample (2008–2012) and Nationwide Readmissions Database (NRD, 2013) and selected all adult patients (age ≥18 years) with ulcerative colitis (UC) or Crohn’s disease (CD) who underwent CRC surgery. Multivariate analysis for in-patient outcomes of postoperative complications, health-care resource utilization, readmission rate, and mortality were performed.
Results:
A total of 397,847 patients underwent CRC surgery from 2008 to 2012, of which 0.8% (3,242) had IBD. Compared to CRC in non-IBD patients, CRC in IBD patients had longer length of stay (adjusted coefficient (AC) 0.86 days, 95% confidence interval (CI): 0.42, 1.30), more likely developed postoperative complications (adjusted odds ratio (AOR) 1.26, 95% CI: 1.06, 1.50), including postoperative infection (AOR 1.69, 95% CI: 1.20, 2.38) and deep vein thrombosis (AOR 2.42, 95% CI: 1.36, 4.28), and more frequently required blood transfusion (AOR 1.59, 95% CI: 1.30, 1.94). CRC in IBD patients was more likely to be readmitted within 30 days (AOR 1.44, 95% CI: 1.01, 2.04).
Conclusion:
At a population level, IBD adversely impacts outcomes at the time of CRC surgery.
Introduction
Inflammatory bowel disease (IBD) is associated with an increased risk of colorectal cancer (CRC).1, 2 Patients with IBD are 60% more likely to develop CRC than patients without IBD, which has been stable from 1998 to 2010.3 The prevalence of ulcerative colitis (UC) and Crohn’s disease (CD) have increased by 33% and 41%, respectively, from 2001 to 2011, and the authors extrapolate that there may be 1.6 million US residents living with IBD.4 Although current guidelines recommend increased surveillance for CRC in this population, adherence remains poor.5, 6, 7 Furthermore, the 5-year survival may be worse in patients with IBD-associated CRC when compared to patients with non-IBD-associated CRC, but the reason has not been identified.8, 9 It is established that carcinogenesis in IBD-associated CRC differs from sporadic CRC, which might contribute to the distinct response to CRC treatments, such as CRC surgery, in IBD patients.10 However, there is a dearth of literature on hospital outcomes of IBD patients undergoing surgery for CRC.11, 12 Thus, we hypothesized that the IBD patients with CRC who undergo surgery for CRC would have more frequent postsurgical complications and longer hospital courses compared to non-IBD patients with CRC.
Methods
Data sources
Data were extracted from the Healthcare Cost and Utilization Project National Inpatient Sample (NIS) between 2008 and 2012. NIS is the largest all-payer in-patient care database in the United States. The database represents a 20% sample of nonfederal, acute-care hospitals in the United States. The sampling frame includes community and general hospitals and academic medical centers comprising ~90% of all-hospital discharges in the United States. Each data entry includes a unique identifier, demographic variables (defined as age, gender, and race/ethnicity), type of admission, source of admission, principal and secondary diagnoses, primary insurance payers, total hospital charges, and length of stay (LOS). The comorbidity burden was stratified based on Elixhauser score <3 and ≥3.13
Additional data were obtained from the Healthcare Cost and Utilization Project Nationwide Readmissions Database (NRD) for the year 2013. Similar to the NIS, the NRD samples community and general hospitals and academic centers. The NRD accounts for nearly 50% of the population of the United States, and accounts for 49.1% of hospitalizations in the United States.14 Each data entry contains over 100 variables, including procedures, diagnoses, patient demographics, total hospital charges, length of in-patient stay, and length of time between admissions.14
The Ohio State Data and Specimen Policy and Human Subjects Research policy does not require Institutional Review Board approval for population-based public data set.15
Study population and definition of variables
Our study population consisted of all adult discharges aged 19 years or older who underwent CRC surgery from 2008 to 2012. Relevant hospitalizations were selected using appropriate International Classification of Diseases, Ninth Revision, Clinical Modification codes (ICD-9-CM) (Supplementary Appendix 1). The discharges were considered to be IBD with CRC if they met one of the following criteria: (a) principal diagnosis was ulcerative colitis (UC) or Crohn’s disease (CD) with a secondary diagnosis of CRC; or (b) a principal diagnosis of CRC and a secondary diagnosis of UC or CD. The controls were CRC patients with no history of either UC or CD. These criteria have been used previously in prior studies.11, 13 Patients were excluded if they had discharge diagnoses of both UC and CD or were missing demographic information. The additional data from the NRD had the same inclusion and exclusion criteria.
For patients with multiple surgical codes, the patient was classified according to the most complex surgery received. In order from the most complicated to the least complicated, the surgical codes included total colectomy, proctectomy, and partial colectomy. Thus, a patient who underwent total colectomy and proctectomy would have been classified as having undergone total colectomy.
Outcomes
Our outcomes of interest were LOS, total hospital charges, postsurgical complications including deep vein thrombosis (DVT) and postsurgical infection, need for blood transfusion, in-hospital mortality, and 30-day readmission rate.
Statistics
SAS 9.4 (SAS Institute, Cary, NC) was used to perform all analyses, using appropriate survey estimation commands and strata weights. Continuous variables are summarized with means and confidence intervals (CIs) and categorical variables were summarized with frequencies and percentages. Using the NIS data, differences between CRC patients undergoing surgery with and without IBD were analyzed using χ2 tests or Student’s t-tests, as appropriate. Differences between patients readmitted within 30 days and those who were not were analyzed similarly with the NRD data set. Multivariate linear regression was used to evaluate the effect of IBD on LOS and hospital costs and multivariate logistic regression was used to calculate adjusted odds ratios (AOR) and corresponding 95% CIs for in-hospital mortality, incidence of postsurgical complications, requirement of blood transfusion, and all other bivariate outcomes. Each multivariate model adjusted for variables significantly associated with the presence of IBD at a level of P≤0.1 on univariate analysis. Using the NRD data an additional model was fit to assess the predictors of 30-day readmission containing all patient and hospital characteristics (age, gender, race, insurance, income, Elixhauser score, hospital size, type, and region, lymph node positivity, distance metastasis, postoperative complications, surgery type and location, and IBD status).
Results
Univariate analysis of demographic characteristics, hospital features, and comorbidities
During the study period, a total of 397,847 patients undergoing CRC surgery were identified after 82,836 patients were excluded. During the same period of time, 937,698 adult patients had either UC or CD. Of these patients with either UC or CD, 3,242 (0.4%) required hospitalization for CRC surgery. Our study included 3,242 (0.8%) IBD patients with CRC and 394,605 (99.2%) non-IBD patients with CRC. Compared to non-IBD patients with CRC, IBD patients with CRC were more likely to be Caucasian (P<0.001), younger (P<0.001), managed at urban teaching hospitals (P<0.001), have private insurance (P<0.001), live in a higher income zip code area (P<0.001), have fewer comorbidities (P=0.002), and have lower prevalence of lymph node positivity (P=0.036) and distant metastasis (P=0.012) (Table 1).
Table 1. Univariate analysis of baseline characteristics among patients with and without IBD who underwent CRC surgery: National Inpatient Sample 2008–2012.
| Non-IBD CRC ( n =394,605) | IBD CRC ( n =3,242) | P value | UC ( n =1,902) | P value | CD ( n =1,340) | P value | |
|---|---|---|---|---|---|---|---|
| Age (mean, CI) | 67.82 (67.64, 68.01) | 61.33 (60.17, 62.48) | <0.0001 | 61.62 (60.14, 63.10) | <0.0001 | 60.91 (59.13, 62.70) | <0.0001 |
| Sex | 0.0751 | 0.0048 | 0.5576 | ||||
| Male | 197,489 (50.05%) | 1,731 (53.39%) | 1,085 (57.02%) | 646 (48.22%) | |||
| Female | 197,116 (49.95%) | 1,511 (46.61%) | 817 (42.98%) | 694 (51.78%) | |||
| Race | <0.0001 | 0.0058 | 0.0001 | ||||
| White | 304,569 (77.18%) | 2,790 (86.06%) | 1,607 (84.47%) | 1,183 (88.33%) | |||
| Black | 40,805 (10.34%) | 187 (5.77%) | 109 (5.74%) | 78 (5.81%) | |||
| Hispanic | 26,179 (6.63%) | 140 (4.31%) | 99 (5.21%) | 41 (3.04%) | |||
| Other | 23,052 (5.84%) | 125 (3.85%) | 87 (4.58%) | 38 (2.82%) | |||
| Insurance | <0.0001 | <0.0001 | <0.0001 | ||||
| Medicare | 226,264 (57.34%) | 1,309 (40.38%) | 764 (40.18%) | 545 (40.65%) | |||
| Medicaid | 20,484 (5.19%) | 192 (5.91%) | 123 (6.46%) | 69 (5.13%) | |||
| Private | 128,021 (32.44%) | 1,597 (49.28%) | 923 (48.54%) | 674 (50.33%) | |||
| Other | 19,836 (5.03%) | 144 (4.44%) | 92 (4.83%) | 52 (3.88%) | |||
| Income quartile a | <0.0001 | 0.0002 | <0.0001 | ||||
| 1 | 100,612 (25.50%) | 550 (16.96%) | 340 (17.87%) | 210 (15.66%) | |||
| 2 | 100,372 (25.44%) | 730 (22.51%) | 433 (22.75%) | 297 (22.16%) | |||
| 3 | 97,319 (24.66%) | 919 (28.34%) | 536 (28.20%) | 382 (28.53%) | |||
| 4 | 96,302 (24.40%) | 1,044 (32.20%) | 593 (31.18%) | 451 (33.64%) | |||
| Elixhauser comorbidity | 0.0015 | 0.0233 | 0.0310 | ||||
| <3 | 212,795 (53.93%) | 1,949 (60.13%) | 1,137 (59.77%) | 812 (60.65%) | |||
| ≥3 | 181,810 (46.07%) | 1,292 (39.87%) | 765 (40.23%) | 527 (39.35%) | |||
| Hospital bed size b | 0.0011 | 0.0082 | 0.0712 | ||||
| Small | 44,345 (11.24%) | 305 (9.40%) | 178 (9.35%) | 127 (9.47%) | |||
| Medium | 95,707 (24.25%) | 607 (18.73%) | 351 (18.43%) | 256 (19.14%) | |||
| Large | 254,553 (64.51%) | 2,330 (71.88%) | 1,374 (72.22%) | 956 (71.39%) | |||
| Hospital type | <0.0001 | <0.001 | 0.0213 | ||||
| Rural | 40,699 (10.31%) | 158 (4.86%) | 85 (4.48%) | 72 (5.40%) | |||
| Urban non-teaching | 166,988 (42.32%) | 1,217 (37.54%) | 650 (34.18%) | 567 (42.30%) | |||
| Urban teaching | 186,918 (47.37%) | 1,867 (57.60%) | 1,167 (61.34%) | 701 (52.30%) | |||
| Hospital region | 0.0033 | 0.0068 | 0.2265 | ||||
| Northeast | 87,938 (22.29%) | 850 (26.23%) | 505 (26.56%) | 345 (25.77%) | |||
| Midwest | 73,744 (18.69%) | 670 (20.66%) | 386 (20.31%) | 283 (21.16%) | |||
| South | 161,975 (41.05%) | 1,087 (33.54%) | 614 (32.30%) | 473 (35.29%) | |||
| West | 70,948 (17.98%) | 634 (19.57%) | 396 (20.83%) | 238 (17.79%) | |||
| Lymph node positivity | 0.0359 | 0.0373 | 0.4166 | ||||
| No | 313,145 (79.36%) | 2,680 (82.68%) | 1,589 (83.55%) | 1,091 (81.44%) | |||
| Yes | 81,460 (20.64%) | 561 (17.32%) | 313 (16.45%) | 249 (18.56%) | |||
| Distant metastasis | 0.0121 | 0.0287 | 0.2342 | ||||
| No | 337,748 (85.59%) | 2,880 (88.85%) | 1,702 (89.47%) | 1,178 (87.97%) | |||
| Yes | 56,857 (14.41%) | 362 (11.15%) | 200 (10.53%) | 161 (12.03%) |
Abbreviations: CD, Crohn’s disease; CI, confidence interval; CRC, colorectal cancer; IBD, inflammatory bowel disease; UC, ulcerative colitis.
Income quartile 1 contains lowest earning households. The exact income ranges vary from year to year.
Hospital bed size is classified by number of beds, and also by hospital region and type. For example, a large hospital requires more than 450 beds if it is an urban teaching hospital in the Southern region, while a large rural hospital in the Southern region only requires 75 beds. For additional information, please see www.hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp.
Among the 3,242 IBD patients with CRC, there were 1,340 patients with CD and 1,902 patients with UC. When compared with non-IBD patients with CRC, patients with CD and UC were more likely to be Caucasian, younger, have private insurance, live in a higher income zip code area, and have fewer comorbidities (Table 1). UC Patients with CRC, but not CD patients with CRC, were less likely to have lymph node positivity (P=0.037) and distant metastasis (P=0.029) when compared to non-IBD patients with CRC (Table 1).
Multivariate analysis of CRC location
The cancer location was different between these groups on multivariate analysis. After adjusting for age; gender; race; insurance; income; Elixhauser score; hospital size, type, and region; lymph node positivity, and distance metastasis, IBD patients CRC were more likely to have rectal cancer than non-IBD patients with CRC (31.4% vs. 23.8%), but the overall most common site for both groups was the right colon (40.4% and 47.1%, respectively) (Table 2). In the subgroup analysis, UC or CD patients with CRC were also more likely to have rectal cancers compared to non-IBD patients with CRC (30.9% and 32.2% vs. 23.8%, respectively) (Table 2). When compared to UC patients with CRC, CD patients with CRC was more likely to occur in the rectum (32.2% vs. 30.9%) and the right colon (47.4% vs. 35.5%) (Supplementary Table 1).
Table 2. Multivariate analysis of CRC location, surgical approach, and surgery location among patients with and without IBD: National Inpatient Sample 2008–2012.
| Non-IBD ( n =394,605) | IBD ( n =3,242) | Adjusted P value | UC ( n =1,902) | Adjusted P value | CD ( n =1,340) | Adjusted P value | |
|---|---|---|---|---|---|---|---|
| Cancer location | 0.0006a | 0.0046a | 0.0004a | ||||
| Right colon | 185,999 (47.14%) | 1,311 (40.44%) | 676 (35.53%) | 635 (47.41%) | |||
| Left colon | 92,374 (23.41%) | 649 (20.01%) | 473 (24.87%) | 175 (13.10%) | |||
| Non-specified colon | 22,523 (5.71%) | 263 (8.12%) | 165 (8.67%) | 98 (7.34%) | |||
| Rectal | 93,708 (23.75%) | 1,019 (31.44%) | 588 (30.94%) | 431 (32.15%) | |||
| Surgery type | 0.0003b | 0.0009b | 0.0839b | ||||
| Laparoscopic | 99,454 (25.20%) | 659 (20.33%) | 365 (19.18%) | 294 (21.95%) | |||
| Open | 295,151 (74.80%) | 2,583 (79.67%) | 1,537 (80.82%) | 1,046 (78.05%) | |||
| Surgery location c | <0.0001a | <0.0001a | <0.0001a | ||||
| Total colectomy | 5,510 (1.40%) | 1,120 (34.54%) | 882 (46.36%) | 238 (17.76%) | |||
| Proctectomy | 95,311 (24.15%) | 638 (19.69%) | 307 (16.13%) | 332 (24.75%) | |||
| Partial colectomy | 293,783 (74.45%) | 1,483 (45.76%) | 713 (37.51%) | 770 (57.49%) |
Abbreviations: CD, Crohn’s disease; CRC, colorectal cancer; IBD, inflammatory bowel disease; UC, ulcerative colitis.
Multivariate analysis adjusts for age; gender; race; insurance; income; Elixhauser score; hospital size, type, and region; lymph node positivity; and distant metastasis.
Multivariate analysis adjusts for age; gender; race; insurance; income; Elixhauser score; hospital size, type, and region; cancer location; lymph node positivity; and distant metastasis.
Patients were classified according to most complex surgery received. Some patients with total colectomy may have also undergone proctectomy.
Multivariate analysis of CRC surgery type
The surgical type was different between these groups on multivariate analysis. After adjusting for age; gender; race; insurance; income; Elixhauser score; hospital size, type, and region; lymph node positivity, and distant metastasis, IBD patients with CRC were more likely to undergo total colectomy or total proctocolectomy than partial colectomy when compared to non-IBD patients with CRC (AOR 33.84, 95% CI: 27.81, 41.18) (Supplementary Table 2). Similarly, in the subgroup analysis, both UC and CD patients with CRC were more likely to undergo total colectomy or total proctocolectomy (AOR 56.46, 95% CI: 44.68, 71.35, and AOR 13.69, 95% CI: 9.74, 19.25, respectively) (Supplementary Table 2). After adjusting for the above covariates and cancer location, IBD patients with CRC were more likely to have open surgery than laparoscopic surgery when compared to non-IBD patients with CRC (AOR 1.46, 95% CI: 1.19, 1.79) (Supplementary Table 2). In the subgroup analysis, UC patients with CRC, but not CD patients with CRC, were more likely to have open surgery when compared to non-IBD patients with CRC (AOR 1.59, 95% CI: 1.21, 2.09) (Supplementary Table 2). When compared to patients with UC patients with CRC, CD patients with CRC were less likely to undergo total colectomy or total proctocolectomy than partial colectomy (AOR 0.23, 95% CI: 0.15, 0.34) (Supplementary Table 3).
Multivariate analysis of study outcomes
On multivariate analysis after adjusting for age; gender; race; insurance; income; Elixhauser comorbidity score; hospital size, type, and region; postoperative complications; cancer location; lymph node positivity; distant metastasis; and surgery type and location, IBD patients with CRC undergoing CRC surgery had longer LOS (adjusted coefficient (AC) 0.86 days, 95% CI: 0.42, 1.30), and more likely received transfusion (AOR 1.59, 95% CI: 1.30, 1.94) than non-IBD patients with CRC (Table 3). In the subgroup analysis, both UC and CD patients with CRC more likely received transfusion (AOR 1.66, 95% CI: 1.29, 2.13, and AOR 1.49, 95% CI: 1.10, 2.02, respectively). However, only CD patients with CRC had longer LOS (AC 1.44, 95% CI: 0.69, 2.18) (Table 3). However, there was no difference in mortality between cohorts (Table 3). After adjusting for the above variables and LOS, there was no difference in total hospital charges (Table 3).
Table 3. Multivariate analysis of health-care resource utilization and CRC surgical outcomes among patients with and without IBD: National Inpatient Sample 2008–2012a.
| Non-IBD ( n =394,605) | IBD ( n =3,242) | AC/AOR (95% CI) | UC ( n =1,902) | AC/AOR (95% CI) | CD ( n =1,340) | AC/AOR (95% CI) | |
|---|---|---|---|---|---|---|---|
| LOS (days)b | 8.66 (8.59, 8.74) | 9.90 (9.32, 10.47) | 0.86 (0.42, 1.30) | 9.71 (9.02, 10.41) | 0.38 (−0.16, 0.91) | 10.16 (9.18, 11.14) | 1.44 (0.69, 2.18) |
| Total hospital charge (US$)c | 72,038 (70,454, 73,621) | 87,619 (80,241, 94,998) | 1,929 (−2,472, 6,329) | 88,035 (78,450, 97,620) | 2,232 (−4,545, 9,008) | 87, 029 (76,036, 98,023) | 1,433 (−3,351, 6,216) |
| Blood transfusionb | 84,413 (21.39%) | 854 (26.34%) | 1.59 (1.30, 1.94) | 512 (26.90%) | 1.66 (1.29, 2.13) | 342 (25.54%) | 1.49 (1.10, 2.02) |
| All postsurgical complicationsd | 115,414 (29.25%) | 1,090 (33.63%) | 1.26 (1.06, 1.50) | 608 (31.99%) | 1.10 (0.88, 1.38) | 482 (35.96%) | 1.51 (1.17, 1.95) |
| Postoperative infectiond | 15,480 (3.92%) | 256 (7.90%) | 1.69 (1.20, 2.38) | 131 (6.89%) | 1.58 (1.04, 2.42) | 125 (9.33%) | 2.50 (1.65, 3.78) |
| Deep vein thrombosisd | 3,319 (0.84%) | 68 (2.09%) | 2.42 (1.36, 4.28) | 40 (2.11%) | 2.57 (1.19, 5.55) | 28 (2.05%) | 2.79 (1.25, 6.25) |
| Respiratoryd | 8,859 (2.25%) | 36 (1.11%) | 0.46 (0.22, 0.95) | 10 (0.49%) | 0.22 (0.06, 0.89) | 27 (1.99%) | 1.01 (0.45, 2.30) |
| Included central nervous systemd | 647 (0.16%) | ≤10 (0.29%) | 1.00 (0.22, 4.52) | ≤10 (0.49%) | 1.73 (0.36, 8.28) | 0 (0.00%) | — |
| Cardiacc | 8,641 (2.19%) | 52 (1.61%) | 0.66 (0.34, 1.25) | 33 (1.73% | 0.76 (0.35, 1.66) | 19 (1.45%) | 0.75 (0.27, 2.06) |
| Peripheral vasculard | 934 (0.24%) | ≤10 (0.15%) | 0.57 (0.07, 4.52) | ≤10 (0.26%) | 1.13 (0.13, 9.70) | 0 (0.00%) | — |
| Gastrointestinald | 36,531 (9.26%) | 299 (9.22%) | 0.81 (0.60, 1.11) | 165 (8.66%) | 0.93 (0.65, 1.32) | 134 (10.03%) | 1.17 (0.78, 1.76) |
| Genitourinaryd | 5,483 (1.39%) | 32 (0.98%) | 0.57 (0.25, 1.28) | 13 (0.71%) | 0.46 (0.14, 1.50) | 18 (1.36%) | 0.99 (0.36, 2.73) |
| Hemorrhage, hematoma, or seromad | 16,338 (4.14%) | 205 (6.33%) | 1.14 (0.80, 1.63) | 105 (5.52% | 1.10 (0.69, 1.75) | 100 (7.48%) | 1.81 (1.15, 2.85) |
| Wound dehiscence, rupture, non-healing, or disruptiond | 5,139 (1.30%) | 73 (2.25%) | 1.40 (0.81, 2.41) | 29 (1.54%) | 1.01 (0.45, 2.26) | 44 (3.26%) | 2.73 (1.37, 5.43) |
| Pulmonary embolismd | 3,587 (0.91%) | 30 (0.94%) | 0.93 (0.39, 2.18) | 26 (1.36%) | 1.47 (0.57, 3.77) | ≤10 (0.33%) | 0.40 (0.06, 2.87) |
| Postoperative anemiad | 48,215 (12.22%) | 465 (14.33%) | 1.16 (0.86, 1.56) | 269 (14.15%) | 1.23 (0.91, 1.65) | 196 (14.60%) | 1.38 (0.94, 2.02) |
| Mortalityb | 8,118 (2.06%) | 54 (1.66%) | 0.93 (0.50, 1.72) | 32 (1.69%) | 0.88 (0.40, 1.98) | 22 (1.66%) | 0.96 (0.38, 2.43) |
Abbreviations: AC, adjusted coefficients; AOR, adjusted odds ratios; CD, Crohn’s disease; CI, confidence interval; CRC, colorectal cancer; IBD, inflammatory bowel disease; LOS, length of stay; UC, ulcerative colitis.
AC and AOR are compared to patients without IBD.
Multivariate analysis adjusts for age; gender; race; insurance; income; Elixhauser score; hospital size, type, and region; postoperative complications; cancer location; lymph node positivity; distant metastasis; and surgery type and location.
Multivariate analysis adjusts for age; gender; race; insurance; income; Elixhauser score; hospital size, type, and region; postoperative complications; cancer location; lymph node positivity; distant metastasis; LOS; and surgery type and location.
Multivariate analysis adjusts for age; gender; race; insurance; income; Elixhauser score; hospital size, type, and region; cancer location; surgery type and location; lymph node positivity; and distant metastasis.
After adjusting for age; gender; race; insurance; income; Elixhauser score; hospital size, type, and region; cancer location; surgery type and location; lymph node positivity; and distant metastasis, IBD patients with CRC undergoing CRC surgery more frequently developed postsurgical complications than non-IBD patients with CRC (AOR 1.26, 95% CI: 1.06, 1.50) (Table 3). Among the individual postsurgical complications, DVT (AOR 2.42, 95% CI: 1.36, 4.28) and postsurgical infection (AOR 1.69, 95% CI: 1.20, 2.38) were significantly more likely to occur in IBD patients with CRC (Table 3). In the subgroup analysis, CD patients with CRC were more likely to develop postsurgical complication compared to non-IBD patients with CRC (AOR 1.51, 95% CI: 1.17, 1.95) (Table 3). CD patients with CRC were more likely to develop postoperative hemorrhage, hematoma, or seroma (AOR 1.81, 95% CI: 1.15, 2.85), and wound dehiscence or poor wound healing (AOR 2.73, 95% CI: 1.37, 5.43) (Table 3). UC and CD patients with CRC were more likely to develop postoperative infection (AOR 1.58, 95% CI: 1.04, 2.42, and AOR 2.50, 95%CI: 1.65, 3.78, respectively) and DVT (AOR 2.57, 95% CI: 1.19, 5.55, and AOR 2.79, 95% CI: 1.25, 6.25, respectively) when compared to non-IBD patients with CRC (Table 3). When comparing UC and CD patients with CRC, there was no difference in postsurgical complications, need for blood transfusion, LOS, total hospital charges, or in-hospital mortality (data not shown).
Rates of readmission
After adjusting for age; gender; insurance; income; Elixhauser score; hospital size and type; postoperative complications, cancer location; lymph node positivity; distant metastases; and surgery type and location, IBD patients with CRC undergoing CRC surgery were nearly 1.4 times more likely to be readmitted within 30 days than non-IBD patients with CRC (AOR 1.44, 95% CI: 1.01–2.04) (Table 4). However, in the subgroup analysis, when comparing UC and CD patients with CRC to non-IBD patients with CRC, 30-day readmission rates were not significantly different (Table 4).
Table 4. Multivariate analysis of readmission within 30 days for IBD patients with CRC compared to non-IBD patients with CRC.
| Overall (%) | 95% CI | Adjusted odds ratio a | 95% CI | P value | |
|---|---|---|---|---|---|
| Non-IBD | 13.15 | 12.73, 13.57 | Reference | ||
| IBD | 20.20 | 14.68, 25.72 | 1.44 | 1.01, 2.04 | 0.0424 |
| UC | 19.70 | 12.83, 26.58 | 1.46 | 0.89, 2.41 | 0.1357 |
| CD | 20.49 | 14.57, 26.40 | 1.44 | 0.91, 2.26 | 0.1203 |
Abbreviations: CD, Crohn’s disease; CI, confidence interval; CRC, colorectal cancer; IBD, inflammatory bowel disease; UC, ulcerative colitis.
Multivariate analysis adjusts for age, gender, insurance, income, Elixhauser score, hospital size and type, postoperative complications, cancer location, lymph node positivity, distance metastasis, surgery type, and surgery location.
Discussion
In our study, IBD patients with CRC who underwent CRC surgery had longer duration of hospitalization and a higher 30-day readmission rate when compared to non-IBD patients with CRC. In addition, IBD patients with CRC were more likely to undergo open surgery and total colectomy or total proctocolectomy. Moreover, IBD patients more likely received blood transfusion and experienced postsurgical complications including DVT and postoperative infection. To our knowledge, this is the first study to use a US in-patient database to evaluate the surgical outcomes of IBD patients with CRC and adds incrementally to the literature on this topic.
Despite lower cancer stage, IBD patients with CRC undergo more radical surgery than sporadic CRC, which is likely due to the increased risk of metachronous tumors in patients with IBD and the presence of underlying colonic inflammation that makes partial colectomy and anastomosis unsafe.11, 12 Therefore, total colectomy and total proctocolectomy are more likely performed for IBD patients with CRC to eliminate the colorectal manifestations of IBD and decrease the risk of subsequent CRC.
The location of cancer is different between IBD and non-IBD patients with CRC. A small study found that IBD-associated CRC is most likely to involve the rectum, followed by right colon.16 In our study, when compared to non-IBD patients with CRC, more rectal cancer was found in IBD patients, including both UC and CD patients. However, overall, IBD patients with CRC, including UC and CD patients with CRC had the greatest predilection to the right colon, which is similar to a prior study.17 Further studies are needed to explain this difference.
Similar to a previous study at a single medical center,12 by using a large nationally representative in-patient database, our study showed that hospital mortality was not significantly different between IBD and non-IBD patients with CRC undergoing CRC surgery. When compared to patients with sporadic CRC or diverticular disease undergoing elective colectomy, IBD patients without CRC were generally healthier, yet had increased health-care resource utilization including longer hospitalization and higher hospital costs.18 Similarly, we have demonstrated that IBD, specifically CD, was also associated with longer hospital stay following CRC surgery. However, in our study, the hospital cost was not different after adjusting for LOS, indicating that longer LOS might be an important factor driving the increased hospital cost.
When compared to non-IBD patients with CRC, UC, and CD patients with CRC undergoing CRC surgery have increased odds of receiving blood transfusion. However, IBD patients with CRC had similar incidence of postoperative anemia (AOR 1.16, 95% CI: 0.86, 1.56) (Table 3), suggesting that the requirement of transfusion might be partially due to intraoperative blood loss or preexisting anemia in IBD patients with CRC. Anemia is very prevalent among IBD patients and is seen more commonly in active disease and in patients on steroids, thus increasing the risk for presurgical anemia.19 Additionally, IBD patients with CRC are more likely to require intraoperative blood transfusion than non-IBD patients with CRC, likely due to inflammatory changes.12 Perioperative blood transfusion has been shown to be associated with postoperative infection and worse hospital outcomes.20 Therefore, preoperative optimization of anemia; for instance, intravenous iron therapy, may be an avenue to improve outcomes of CRC surgery in IBD patients.21
IBD, particularly CD, was also associated with increased postsurgical complications, including infection and DVT. IBD is a known independent risk factor for surgical site infection.22 Additionally, preoperative corticosteroid use, which is common in IBD patients, is also an important risk factor for postoperative infection.23 Lastly, 75% of complications after CRC surgery are infectious.24 It is well established that patients with IBD are at greater risk for DVT, particularly in patients who undergo surgery for CRC.25, 26 Thus, reducing inflammation and minimizing use of corticosteroids before surgery might reduce risk of postoperative infection. In addition, perioperative DVT prophylaxis is critical in IBD patients with CRC who undergo CRC surgery.
IBD patients with CRC undergoing CRC surgery were more likely to be readmitted within 30 days when compared to non-IBD patients with CRC. However, in the subgroup analysis, the 30-day readmission rates of UC or CD patients with CRC were not different than non-IBD patients with CRC, which might be due to small number of patients readmitted in the CD or UC patients with CRC cohorts (56 patients with UC and 100 patients with CD, respectively) (Supplementary Table 4). Further study is needed to clarify the indications for the increased readmission rate for IBD patients with CRC after CRC surgery.
Our study had several limitations. The accuracy of ICD-9-CM coding could not be verified by chart review, owing to privacy safeguards. However, the Agency for Healthcare Research and Quality has reviewed the NIS and similar databases and found good reliability.27 In addition, any errors in administrative data would be distributed non-differentially across all groups.28 Furthermore, administrative discharge codes have been previously used and validated for outcomes research in a variety of diseases. The ICD-9-CM codes in our study have been used in several previous studies.29, 30 Also, the IBD patients with CRC in our study included both IBD-related CRC and sporadic CRC in patients with IBD. Due to the large number of patients included in the study, there is a risk of identifying statistically significant findings which are of no clinical significance. We reported ORs and 95% CIs to determine the strength of the correlations and improve interpretation. There are no laboratory values or medication data in the NIS (i.e., unable to determine use of immunomodulators, or postoperative DVT prophylaxis), and no details about disease duration or distribution. There is no longitudinal data following hospital discharge in the NIS database and thus we are unable to comment on postdischarge outcomes or hospital readmissions. To overcome this weakness, we included an NRD analysis in the year of 2013.
Despite the above limitations, our study also has several strengths. The NIS and NRD databases provide a large number of patients with a discharge diagnosis of CRC who have undergone colorectal surgery, which otherwise would not be possible from single or even multicenter study. The benefit of using the NIS and NRD databases is that the results represent the current national in-patient health-care utilization of IBD patients with CRC who undergo CRC surgery.
Conclusion
IBD adversely impacts the health-care outcomes of CRC surgery. While prior studies have shown many predisposing factors to explain these suboptimal outcomes, future research should emphasize alleviating modifiable presurgical IBD-related patient factors to improve short-term postsurgical outcomes.
Study Highlights
Footnotes
Supplementary Information accompanies this paper on the Clinical and Translational Gastroenterology website (http://www.nature.com/ctg)
Guarantor of the article: Cheng Zhang, MD, PhD.Specific author contributions: M.R. developed the concept, drafted the manuscript; S.G.K. developed the concept and edited the manusript; P.P.S. developed the concept and edited the manuscript; S.H. developed the concept and edited the manuscript; A.H. performed the statistical analysis; E.J.L. edited the manuscript; D.C. developed the concept and edited the manuscript; A.H. performed the statistical analysis; C.Z. developed the concept, performed the statistical analysis, interpreted the results, and edited the manuscript.Financial support: None.Potential competing interests: None.
Supplementary Material
References
- Beaugerie L, Itzkowitz SH. Cancers complicating inflammatory bowel disease. N Engl J Med 2015; 372: 1441–1452. [DOI] [PubMed] [Google Scholar]
- Fornaro R, Caratto M, Caratto E et al. Colorectal cancer in patients with inflammatory bowel disease: the need for a real surveillance program. Clin Colorectal Cancer 2016; 15: 204–212. [DOI] [PubMed] [Google Scholar]
- Herrinton LJ, Liu L, Levin TR et al. Incidence and mortality of colorectal adenocarcinoma in persons with inflammatory bowel disease from 1998 to 2010. Gastroenterology 2012; 143: 382–389. [DOI] [PubMed] [Google Scholar]
- Shivashankar R, Tremaine WJ, Harmsen WS et al. Incidence and prevalence of Crohn's disease and ulcerative colitis in Olmsted County, Minnesota from 1970 through 2010. Clin Gastroenterol Hepatol 2017; 15: 857–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Rijn AF, Fockens P, Siersema PD et al. Adherence to surveillance guidelines for dysplasia and colorectal carcinoma in ulcerative and Crohn's colitis patients in the Netherlands. World J Gastroenterol 2009; 15: 226–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feuerstein JD, Lewandowski JJ, Martinez-Vazquez M et al. Documented compliance with inflammatory bowel disease quality measures is poor. Dig Dis Sci 2015; 60: 339–344. [DOI] [PubMed] [Google Scholar]
- Mowat C, Cole A, Windsor A et al. Guidelines for the management of inflammatory bowel disease in adults. Gut 2011; 60: 571–607. [DOI] [PubMed] [Google Scholar]
- Adams SV, Ahnen DJ, Baron JA et al. Survival after inflammatory bowel disease-associated colorectal cancer in the Colon Cancer Family Registry. World J Gastroenterol 2013; 19: 3241–3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peyrin-Biroulet L, Lepage C, Jooste V et al. Colorectal cancer in inflammatory bowel diseases: a population-based study (1976–2008). Inflamm Bowel Dis 2012; 18: 2247–2251. [DOI] [PubMed] [Google Scholar]
- Herszenyi L, Barabas L, Miheller P et al. Colorectal cancer in patients with inflammatory bowel disease: the true impact of the risk. Dig Dis 2015; 33: 52–57. [DOI] [PubMed] [Google Scholar]
- Gearhart SL, Nathan H, Pawlik TM et al. Outcomes from IBD-associated and non-IBD-associated colorectal cancer: a surveillance epidemiology and end results medicare study. Dis Colon Rectum 2012; 55: 270–277. [DOI] [PubMed] [Google Scholar]
- Renz BW, Thasler WE, Preissler G et al. Clinical outcome of IBD-associated versus sporadic colorectal cancer: a matched-pair analysis. J Gastrointest Surg 2013; 17: 981–990. [DOI] [PubMed] [Google Scholar]
- Zhang C, Krishna SG, Hinton A et al. Cytomegalovirus-related hospitalization is associated with adverse outcomes and increased health-care resource utilization in inflammatory bowel disease. Clin Transl Gastroenterol 2016; 7: e150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Introduction to the HCUP Nationwide Readmissions Database (NRD) 2013. Healthcare Cost and Utilization Project (HCUP) 2013 November 2015 [cited 2017 July] Available from https://www-hcup-us-ahrq-gov.proxy.lib.ohio-state.edu/db/nation/nrd/NRD_Introduction_2013.jsp.
- Krishna SG, Hinton A, Oza V et al. Morbid obesity is associated with adverse clinical outcomes in acute pancreatitis: a propensity-matched study. Am J Gastroenterol 2015; 110: 1608–1619. [DOI] [PubMed] [Google Scholar]
- Kiran RP, Khoury W, Church JM et al. Colorectal cancer complicating inflammatory bowel disease: similarities and differences between Crohn's and ulcerative colitis based on three decades of experience. Ann Surg 2010; 252: 330–335. [DOI] [PubMed] [Google Scholar]
- Jewel Samadder N, Valentine JF, Guthery S et al. Colorectal Cancer in inflammatory bowel diseases: a population-based study in Utah. Dig Dis Sci 2017; 62: 2126–2132. [DOI] [PubMed] [Google Scholar]
- Van Arendonk KJ, Tymitz KM, Gearhart SL et al. Outcomes and costs of elective surgery for diverticular disease: a comparison with other diseases requiring colectomy. JAMA Surg 2013; 148: 316–321. [DOI] [PubMed] [Google Scholar]
- Portela F, Lago P, Cotter J et al. Anaemia in patients with inflammatory bowel disease—a nationwide cross-sectional study. Digestion 2016; 93: 214–220. [DOI] [PubMed] [Google Scholar]
- Li Y, Stocchi L, Rui Y et al. Perioperative blood transfusion and postoperative outcome in patients with Crohn's disease undergoing primary ileocolonic resection in the "Biological Era". J Gastrointest Surg 2015; 19: 1842–1851. [DOI] [PubMed] [Google Scholar]
- Gasche C, Berstad A, Befrits R et al. Guidelines on the diagnosis and management of iron deficiency and anemia in inflammatory bowel diseases. Inflamm Bowel Dis 2007; 13: 1545–1553. [DOI] [PubMed] [Google Scholar]
- Bhakta A, Tafen M, Glotzer O et al. Increased incidence of surgical site infection in IBD patients. Dis Colon Rectum 2016; 59: 316–322. [DOI] [PubMed] [Google Scholar]
- Nguyen GC, Elnahas A, Jackson TD. The impact of preoperative steroid use on short-term outcomes following surgery for inflammatory bowel disease. J Crohn's Colitis 2014; 8: 1661–1667. [DOI] [PubMed] [Google Scholar]
- Holubar SD, Hedrick T, Gupta R et al. American Society for Enhanced Recovery (ASER) and Perioperative Quality Initiative (POQI) joint consensus statement on prevention of postoperative infection within an enhanced recovery pathway for elective colorectal surgery. Periop Med 2017; 6: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alatri A, Schoepfer A, Fournier N et al. Prevalence and risk factors for venous thromboembolic complications in the Swiss Inflammatory Bowel Disease Cohort. Scand J Gastroenterol 2016; 51: 1200–1205. [DOI] [PubMed] [Google Scholar]
- Gross ME, Vogler SA, Mone MC et al. The importance of extended postoperative venous thromboembolism prophylaxis in IBD: a National Surgical Quality Improvement Program analysis. Dis Colon Rectum 2014; 57: 482–489. [DOI] [PubMed] [Google Scholar]
- Whalen D, Houchens R, Elixhauser A. 2002 HCUP Nationwide Inpatient Sample (NIS) comparison report. US Agency for Healthc Res Qual 2005: 1–89.
- Nguyen GC, Bayless TM, Powe NR et al. Race and health insurance are predictors of hospitalized Crohn's disease patients undergoing bowel resection. Inflamm Bowel Dis 2007; 13: 1408–1416. [DOI] [PubMed] [Google Scholar]
- Ananthakrishnan AN, McGinley EL, Binion DG. Does it matter where you are hospitalized for inflammatory bowel disease? A nationwide analysis of hospital volume. Am J Gastroenterol 2008; 103: 2789–2798. [DOI] [PubMed] [Google Scholar]
- Ananthakrishnan AN, McGinley EL, Binion DG et al. A nationwide analysis of changes in severity and outcomes of inflammatory bowel disease hospitalizations. J Gastrointest Surg 2011; 15: 267–276. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


