Abstract
Microscopic colitis (MC) is a chronic inflammatory bowel disease characterized by chronic watery diarrhea and diagnosed with the histologic hallmarks of disease despite a macroscopically normal large bowel. Although 2 distinct disease phenotypes exist, their clinical presentations and epidemiologic characteristics have overlapping features. This article summarizes evidence regarding the pathogenesis of MC, mechanisms of diarrhea in this cohort, and associations with medications. In addition, currently recommended and novel therapeutic approaches to achieving remission in this patient population are reviewed.
Keywords: Lymphocytic, microscopic, collagenous, colitis, diarrhea
Microscopic colitis (MC) is a chronic inflammatory condition characterized by chronic diarrhea, normal colonic mucosa, and abnormal histologic hallmarks. Features of collagenous colitis (CC) were first described by Lindström in 1976,1 followed by features of lymphocytic colitis (LC) by Lazenby and colleagues in 1989.2 These 2 disease subtypes have overlapping clinical and epidemiologic features. CC is characterized by the presence of a subepithelial collagen band at least 20 μm thick, and in LC, infiltration of more than 10% of intraepithelial lymphocytes is a hallmark finding.3,4 It is probable that the innate immune response and environmental exposures contribute to pathogenesis in an interdependent manner in genetically susceptible individuals. This article attempts to summarize evidence of the potential etiology and therapeutic strategies of MC.
Incidence and Risk Factors
The reported prevalence rates of CC and LC are 42 and 69 per 100,000 persons, respectively,5 and the incidence rates of these diseases in patients under investigation for chronic diarrhea are higher, from 10% to 20%.3,6,7 Established risk factors include increasing age, with 75% of the people affected being over 50 years old.8 The ratio of women to men is 2.4 to 1, and women have a proportionally greater risk of CC.9 A recent French study reported that the incidence of MC was 7.9 per 100,000 inhabitants, similar to the incidence of Crohn’s disease in that population.10 Although a history of smoking is associated with transient risk, current smoking increases the risk of persistent disease11 and CC diagnosis at a young age (odds ratio [OR], 2.4; 95% CI, 1.5-3.8).12 In addition, a history of autoimmune disease, including diabetes mellitus, rheumatoid arthritis, and celiac sprue, is associated with MC.13,14 Celiac disease is associated with a 50 to 70 times greater risk of MC, especially in middle-aged women, and with severe villous atrophy.14,15 In a multicenter, prospective study of 433 patients with MC or functional diarrhea, Macaigne and colleagues found that MC was associated with age over 50 years (OR, 3.1; 95% CI, 1.6-5.9), nocturnal diarrhea (OR, 2.0; 95% CI, 1.1-3.9), weight loss (OR, 2.5; 95% CI, 1.3-4.7), new medications (OR, 3.7; 95% CI, 2.1-6.6), and autoimmune disease (OR, 5.5; 95% CI, 2.5-12.0).13
Etiology
Dysregulated Collagen Metabolism
In CC, collagen accumulation in the subepithelial layer reflects disturbance in the homeostasis of the extracellular matrix and is predominantly driven by attenuated matrix degradation and tissue inhibitor of metalloproteinase-1 (TIMP-1) imbalance. This inhibits several metalloproteinases involved in collagen degradation16 and upregulation of transforming growth factor-β, which contributes to fibrogenesis and collagen deposition. Vascular endothelial growth factor is implicated in repair mechanisms in MC with increased tissue immunostaining in remission, counteracting TIMP-1 activity and facilitating collagen breakdown through innate metalloproteinases.17
Abnormal Epithelial Barrier Function
Histology before and after ileostomy reversal found increased transcellular and tight junction permeability, proposing that mucosal barrier dysfunction has a role in CC.18 Gastrointestinal luminal interleukin-2, -23, and -12 levels rise after restoration of intestinal continuity, supporting the idea that luminal toxins drive inflammation in CC.19 Furthermore, downregulation of the tight junction proteins claudin-4, -5, and -8, and their redistribution off the tight junction, triggered by tumor necrosis factor-α (TNF-α) and interferon-γ, contribute to diarrhea in LC.20
Drug Exposure and Microscopic Colitis
Medications associated with MC include nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin; selective serotonin reuptake inhibitors; proton pump inhibitors (PPIs); and drugs with various other mechanisms of action, including statins, beta blockers, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers.21-24 Multidrug use, particularly concomitant NSAIDs and PPIs, further increases the risk of MC.23 MC does not progress in a dose-dependent manner,23 and symptoms may be reported days to months after drug initiation, with a median time of 4 days to symptom onset.25
A retrospective case-control study of 136 patients with MC reported that 38% of CC patients had a history of PPI use, yielding an OR of 4.5 vs matched controls for MC.26 Controlling for celiac disease, hypothyroidism, and rheumatoid arthritis in multivariate analysis, the OR increased to 5.8. PPIs alter intestinal microbial communities and induce acid suppression27 as well as increase intercellular permeability, which may contribute to disease given the known tight junction dysfunction in MC.26,28 In summary, there is evidence to suggest that certain drugs may precipitate the onset of MC, and there should be consideration to stop these drugs to reduce the risk of relapse.
Clinical Features
There is considerable overlap in the clinical presentations of LC and CC. The natural histories of these diseases are variable, with reports of occasional spontaneous remission of symptoms with eventual recurrence, often without an identifiable trigger. A retrospective analysis of 199 patients reported a median 6-month disease duration in LC patients until treatment.9 Symptoms may vary from mild chronic watery diarrhea to incapacitating, increased stool frequency9,13,29,30 with urgency and fecal incontinence. Stool consistency is very loose, with 88% of MC patients having a median stool form of 6 on the Bristol Stool Scale, compared with 35% of patients with functional diarrhea.31 Patients with MC have features of both secretory and osmotic diarrhea. Marked reduction in stool frequency may occur in response to reduced oral intake, suggesting an osmotic component. Secretory features seem to be driven by active chloride secretion, and analysis of fecal electrolytes reveals increased fecal fluid sodium and potassium concentration, with 87% of MC patients meeting the diagnostic criteria for secretory diarrhea. It is likely that reduced sodium absorption drives diarrhea in LC, contrasting with increased chloride secretion and reduced rates of bicarbonate/chloride exchange in CC.32,33 In LC, chromogranin (Cg) A–positive cells are present in the epithelial layer at higher density, possibly suggesting a role of colonic neuroendocrine cells in chronic diarrhea.34 Higher levels of fecal neuroendocrine peptides, including secretoneurin, CgA, and CgB, are present in active CC, and secretoneurin levels revert in clinical remission to values comparable to those of healthy controls.35 However, the diagnostic utility of these peptides has not been established.
Approximately half of the affected population will report some weight loss13,29,36-38 or abdominal pain.9,39 A meta-analysis of 10 published studies has refuted perceptions that there is a link between MC and irritable bowel syndrome (IBS).40 In the analysis, the pooled prevalence was 33.4% (13.8%-55.7%) for IBS in MC, not a significantly greater prevalence than in chronic functional diarrhea (OR, 1.39). Considered separately or pooled together, patients with IBS did not have increased odds of diagnosis with MC.40
A daily stool frequency of more than 3 motions per day in CC patients is associated with reduced health-related quality-of-life scores.41 Therefore, improvement in quality of life is often included as a measure of clinical response and remission in therapeutic efficacy studies.41 There are few cases of severe complications, including amyloidosis with subsequent colon stricturing and ulceration due to long-standing inflammation,42 protein-losing enteropathy with hypoalbuminemia,43 and spontaneous colonic perforation in individual cases of CC.44-47
Diagnosis
Laboratory investigations often have normal or mildly deranged findings in patients with MC and offer limited diagnostic value. Approximately 50% of MC patients have mild anemia and mildly elevated inflammatory markers.8 Objective fecal biomarkers such as fecal calprotectin are not reliable indicators of MC. Although the median fecal calprotectin level was higher in MC patients in 2 small studies of active MC vs functional diarrhea, the absolute fecal calprotectin level was low, between 48 to 80 μg/g,48,49 and up to 38% of patients with active disease had a normal calprotectin level, limiting its use to reliably differentiate between MC and functional diarrhea. Fecal lactoferrin, also of neutrophilic origin, has very low sensitivity in MC patients, with only 10% having increased levels in an analysis of 39 patients.49,50
Histologic hallmarks of disease in macroscopically unremarkable colon form the diagnostic cornerstone in MC. Colonoscopy and biopsies of the right and left colon are recommended; when only left-sided sampling is performed, the diagnosis can be missed in up to 40% of patients51,52 due to the reduction in histologic burden from proximal to distal colon.53 However, subsequent research has suggested that up to 97.5% of cases could be diagnosed with only left colon biopsies.30 In cases of diagnostic uncertainty, CD3 staining may accurately quantify the extent of intraepithelial lymphocytosis. A third entity, incomplete MC or MC not otherwise specified, has been identified, describing a cohort with chronic diarrhea and classic pathologic features not meeting diagnostic criteria for LC or CC. These cases have responded to standard MC therapies, including budesonide.30
Treatment of Microscopic Colitis
If medications are implicated in individual MC cases, withdrawal alone is usually insufficient to achieve clinical response.54 These patients usually require medical treatment to achieve remission. Randomized, controlled trials and meta-analyses favor budesonide for induction of clinical remission. A Cochrane systematic review reported an OR of 12.32 to induce and 8.82 to maintain response in CC over 6 months with a number needed to treat (NNT) of 2 per outcome. A minority of patients achieve histologic remission. Similar response rates were seen in LC with an OR of 9 to induce response and a NNT of 3.55 Budesonide improves quality-of-life scores using the gastrointestinal quality-of-life index.56 American Gastroenterological Association (AGA) guidelines recommend an 8-week course of budesonide as first-line therapy for induction of clinical remission based on a meta-analysis of 6 studies showing a net beneficial effect and 152% increase in the likelihood of remission over 6 to 8 months.4,57 Data supporting the use of oral prednisolone for induction of remission are modest, so its use is not recommended as first-line treatment, particularly considering the side-effect burden associated with corticosteroids. An analysis of 17 patients treated with prednisolone vs 63 with budesonide showed lower remission rates and increased relapse with prednisolone.58
Clinical relapse after stopping budesonide is common and reported in 40% to 81% as soon as 2 weeks after withdrawal.59-61 Analysis of predictors of recurrence identified risk factors, including older patients (>60 years), longer duration of symptoms (>12 months), and high daily stool frequency (>5/day). Maintenance therapy with oral budesonide may be required to restore quality of life and maintain clinical remission in a proportion of patients.61 Maintenance therapy with 4.5 mg of budesonide daily was associated with maintenance of remission, sustained improvement in quality-of-life scores for CC patients, and nonserious adverse effects in 7 of 44 patients.59 Little research has examined the success rates of budesonide for maintenance of remission in LC.55 Although minimal side effects have been reported in MC during budesonide therapy,62 the association between long-term budesonide use and reduced bone density scores in Crohn’s disease63 underlines the importance of monitoring bone health in these patients. For maintenance, the lowest effective dose of budesonide should be used. Consideration should also be given to the specific budesonide formulation used. The preferred form of budesonide is absorbed in the ileum and right colon, rather than the alternative, which is associated with mainly left colon absorption and, hence, may be less effective in MC.57
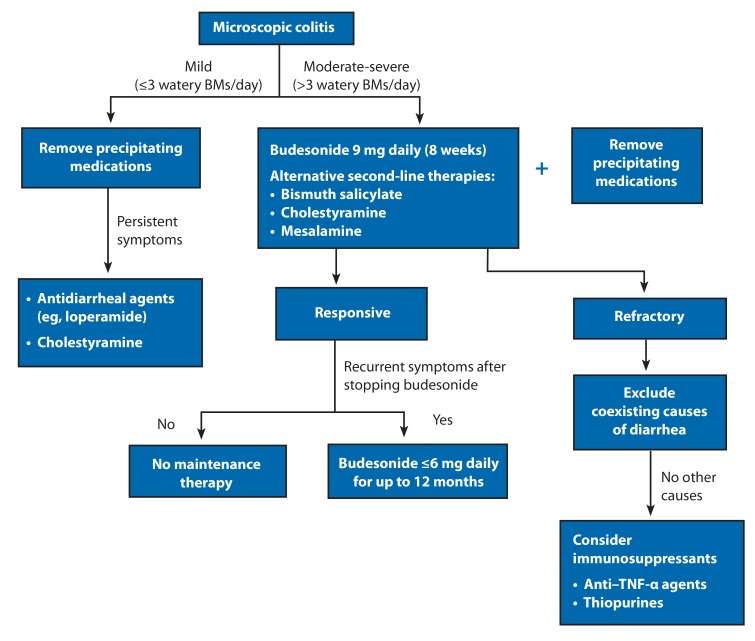
The AGA recommends that treatment with mesalamine or bismuth subsalicylate should be considered over no treatment when budesonide is contraindicated or fails.57 Treatment with bismuth subsalicylate was associated with favorable clinical outcomes in a small open-label study of LC and CC resulting in clinical and histologic responses.64 Clinical efficacy studies of mesalamine have yielded mixed results, finding this therapy inferior to budesonide for induction of remission (relative risk [RR], 1.82 for remission with budesonide vs mesalamine).4,65 Although mesalamine is recommended as second-line therapy in MC, the clinical data available do not strongly support this recommendation. In LC, mesalamine in combination with cholestyramine did not significantly increase the likelihood of achieving clinical remission, although in CC, dual therapy was associated with a greater chance of remission than mesalamine alone. The modest increased response was offset by adverse effects.66 Despite morphologically normal distal ileum, bile acid malabsorption has been identified in approximately 40% of MC patients in 2 studies, with induction of clinical remission following cholestyramine in 19 of 22 patients with abnormal 75Se-homocholic acid taurine scans.67,68 In the absence of bile acid malabsorption, there is weak evidence for clinical response to cholestyramine. These recommendations are limited by a lack of controlled clinical trials for these drugs, with the exception of bismuth and budesonide, and some mixed results and methodologies in the available data (Figure). Standard antidiarrheal agents, including loperamide, may have a role in controlling symptoms in patients with mild clinical disease. Symptomatic improvement may also be provided by the elimination of dietary secretagogues such as caffeine, lactose, and fats.
Figure.
An algorithm of diagnostic and therapeutic recommendations for patients with microscopic colitis.
BMs, bowel movements; TNF, tumor necrosis factor
A few studies have investigated the potential benefit of probiotics in MC without evidence of clinical efficacy to date after treatment with Lactobacillus acidophilus and Bifidobacterium animalis subsp lactis.4,69 In a study that randomized 26 patients to receive placebo or Boswellia serrata extract, patients with CC showed some clinical response, but the lack of histologic response combined with no improved quality-of-life scores means that this approach cannot be currently recommended.70 Further clinical trials would be useful to determine whether probiotics have a place within the clinical paradigm.
Refractory Microscopic Colitis
Some patients may have persistent symptoms despite medical therapy. In these individuals, coexistent conditions such as celiac disease should be first excluded. If contraindicated, or relapse occurs despite budesonide maintenance, immunomodulators (azathioprine and 6-mercaptopurine) are reasonably efficacious in MC, although their use may be limited by intolerance in approximately one-third of patients in this setting.71,72 Methotrexate has been used with mixed results in retrospective and prospective analyses, although inadequate power may have influenced the outcome.71,73 Similarly, calcineurin inhibitors have been used in individual reports and were well tolerated, but only 1 patient achieved complete response. These drugs are not currently recommended in refractory MC.71
A case series points to the use of anti–TNF-α agents in refractory disease.42 Excellent early response rates have been reported, with a reduction of daily stool frequency of up to 90% and sustained remission in a proportion of patients.42 One analysis over almost 20 years included 10 patients treated with anti–TNF-α therapy for a median of 4 months, and reported that a proportion of patients achieved partial response to anti–TNF-α therapy. Long-term use in MC may not be necessary if a precipitating agent such as a PPI has been identified and discontinued.71
Colectomy and consequent diversion of the fecal stream have been used to treat a small cohort of patients with medically refractory MC. A case of LC74 and a case of CC75 successfully treated with colectomy and subsequent fashioning of ileal J-pouch have been reported. Although histologic remission does not always coexist with clinical remission after medical therapy, diversion of the fecal stream resolves histologic changes, which recur after ileostomy reversal.76
Summary
In an aging population, the prevalence of MC is likely to rise, and recent guidelines provide clarity and clear approaches for management of this disease. Although serious and life-threatening complications are uncommon, symptoms may be debilitating and negatively impact quality of life for elderly patients. A high index of suspicion is required in female patients over 50 years old reporting chronic watery diarrhea, particularly with a history of autoimmune or celiac disease. Careful histories are recommended to identify possible triggers, especially in patients taking multiple medications for comorbidities. Budesonide remains the recommended first-line therapy, and maintenance therapy with the drug is often required.
References
- 1.Lindström CG. ‘Collagenous colitis’ with watery diarrhoea—a new entity? Pathol Eur. 1976;11(1):87–89. [PubMed] [Google Scholar]
- 2.Lazenby AJ, Yardley JH, Giardiello FM, Jessurun J, Bayless TM. Lymphocytic (“microscopic”) colitis: a comparative histopathologic study with particular reference to collagenous colitis. Hum Pathol. 1989;20(1):18–28. doi: 10.1016/0046-8177(89)90198-6. [DOI] [PubMed] [Google Scholar]
- 3.Münch A, Aust D, Bohr J, et al. European Microscopic Colitis Group (EMCG) Microscopic colitis: current status, present and future challenges: statements of the European Microscopic Colitis Group. J Crohns Colitis. 2012;6(9):932–945. doi: 10.1016/j.crohns.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 4.Pardi DS, Tremaine WJ, Carrasco-Labra A. American Gastroenterological Association Institute Technical Review on the medical management of microscopic colitis. Gastroenterology. 2016;150(1):247–274.e11. doi: 10.1053/j.gastro.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Pardi DS, Loftus EV, Jr, Smyrk TC, et al. The epidemiology of microscopic colitis: a population based study in Olmsted County, Minnesota. Gut. 2007;56(4):504–508. doi: 10.1136/gut.2006.105890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cotter TG, Binder M, Pardi DS. Validation of a scoring system to predict microscopic colitis in a cohort of patients with chronic diarrhea. Clin Gastroenterol Hepatol. 2016;14(5):777–778. doi: 10.1016/j.cgh.2015.12.015. [DOI] [PubMed] [Google Scholar]
- 7.Olesen M, Eriksson S, Bohr J, Järnerot G, Tysk C. Microscopic colitis: a common diarrhoeal disease. An epidemiological study in Orebro, Sweden, 1993-1998. Gut. 2004;53(3):346–350. doi: 10.1136/gut.2003.014431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bohr J, Tysk C, Eriksson S, Abrahamsson H, Järnerot G. Collagenous colitis: a retrospective study of clinical presentation and treatment in 163 patients. Gut. 1996;39(6):846–851. doi: 10.1136/gut.39.6.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olesen M, Eriksson S, Bohr J, Järnerot G, Tysk C. Lymphocytic colitis: a retrospective clinical study of 199 Swedish patients. Gut. 2004;53(4):536–541. doi: 10.1136/gut.2003.023440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fumery M, Kohut M, Gower-Rousseau C, et al. on behalf on the Somme MC group; EPIMAD group. Incidence, clinical presentation, and associated factors of microscopic colitis in northern France: a population-based study. Dig Dis Sci. 2017;62(6):1571–1579. doi: 10.1007/s10620-016-4306-z. [DOI] [PubMed] [Google Scholar]
- 11.Roth B, Gustafsson RJ, Jeppsson B, Manjer J, Ohlsson B. Smoking- and alcohol habits in relation to the clinical picture of women with microscopic colitis compared to controls. BMC Womens Health. 2014;14(1):16. doi: 10.1186/1472-6874-14-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yen EF, Pokhrel B, Du H, et al. Current and past cigarette smoking significantly increase risk for microscopic colitis. Inflamm Bowel Dis. 2012;18(10):1835–1841. doi: 10.1002/ibd.22838. [DOI] [PubMed] [Google Scholar]
- 13.Macaigne G, Lahmek P, Locher C, et al. Microscopic colitis or functional bowel disease with diarrhea: a French prospective multicenter study. Am J Gastroenterol. 2014;109(9):1461–1470. doi: 10.1038/ajg.2014.182. [DOI] [PubMed] [Google Scholar]
- 14.Stewart M, Andrews CN, Urbanski S, Beck PL, Storr M. The association of coeliac disease and microscopic colitis: a large population-based study. Aliment Pharmacol Ther. 2011;33(12):1340–1349. doi: 10.1111/j.1365-2036.2011.04666.x. [DOI] [PubMed] [Google Scholar]
- 15.Green PH, Yang J, Cheng J, Lee AR, Harper JW, Bhagat G. An association between microscopic colitis and celiac disease. Clin Gastroenterol Hepatol. 2009;7(11):1210–1216. doi: 10.1016/j.cgh.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 16.Günther U, Schuppan D, Bauer M, et al. Fibrogenesis and fibrolysis in collagenous colitis. Patterns of procollagen types I and IV, matrix-metalloproteinase-1 and -13, and TIMP-1 gene expression. Am J Pathol. 1999;155(2):493–503. doi: 10.1016/S0002-9440(10)65145-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Griga T, Tromm A, Schmiegel W, Pfisterer O, Müller K-M, Brasch F. Collagenous colitis: implications for the role of vascular endothelial growth factor in repair mechanisms. Eur J Gastroenterol Hepatol. 2004;16(4):397–402. doi: 10.1097/00042737-200404000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Münch A, Söderholm JD, Wallon C, Öst A, Olaison G, Ström M. Dynamics of mucosal permeability and inflammation in collagenous colitis before, during, and after loop ileostomy. Gut. 2005;54(8):1126–1128. doi: 10.1136/gut.2004.058750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daferera N, Kumawat AK, Hultgren-Hörnquist E, Ignatova S, Ström M, Münch A. Fecal stream diversion and mucosal cytokine levels in collagenous colitis: a case report. World J Gastroenterol. 2015;21(19):6065–6071. doi: 10.3748/wjg.v21.i19.6065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barmeyer C, Erko I, Awad K, et al. Epithelial barrier dysfunction in lymphocytic colitis through cytokine-dependent internalization of claudin-5 and -8. J Gastroenterol. published online January 30, 2017. doi:10.1007/s00535-017-1309-2. [DOI] [PubMed]
- 21.Masclee GM, Coloma PM, Kuipers EJ, Sturkenboom MC. Increased risk of microscopic colitis with use of proton pump inhibitors and non-steroidal anti-inflammatory drugs. Am J Gastroenterol. 2015;110(5):749–759. doi: 10.1038/ajg.2015.119. [DOI] [PubMed] [Google Scholar]
- 22.Fernández-Bañares F, Esteve M, Espinós JC, et al. Drug consumption and the risk of microscopic colitis. Am J Gastroenterol. 2007;102(2):324–330. doi: 10.1111/j.1572-0241.2006.00902.x. [DOI] [PubMed] [Google Scholar]
- 23.Verhaegh BP, de Vries F, Masclee AA, et al. High risk of drug-induced microscopic colitis with concomitant use of NSAIDs and proton pump inhibitors. Aliment Pharmacol Ther. 2016;43(9):1004–1013. doi: 10.1111/apt.13583. [DOI] [PubMed] [Google Scholar]
- 24.Riddell R, Tanaka M, Mazzoleni G. Non-steroidal anti-inflammatory drugs as a possible cause of collagenous colitis: a case-control study. Gut. 1992;33(5):683–686. doi: 10.1136/gut.33.5.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beaugerie L, Pardi DS. Review article: drug-induced microscopic colitis—proposal for a scoring system and review of the literature. Aliment Pharmacol Ther. 2005;22(4):277–284. doi: 10.1111/j.1365-2036.2005.02561.x. [DOI] [PubMed] [Google Scholar]
- 26.Keszthelyi D, Jansen SV, Schouten GA, et al. Proton pump inhibitor use is associated with an increased risk for microscopic colitis: a case-control study. Aliment Pharmacol Ther. 2010;32(9):1124–1128. doi: 10.1111/j.1365-2036.2010.04453.x. [DOI] [PubMed] [Google Scholar]
- 27.Imhann F, Bonder MJ, Vich Vila A, et al. Proton pump inhibitors affect the gut microbiome. Gut. 2016;65(5):740–748. doi: 10.1136/gutjnl-2015-310376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mullin JM, Valenzano MC, Whitby M, et al. Esomeprazole induces upper gastrointestinal tract transmucosal permeability increase. Aliment Pharmacol Ther. 2008;28(11-12):1317–1325. doi: 10.1111/j.1365-2036.2008.03824.x. [DOI] [PubMed] [Google Scholar]
- 29.Cotter TG, Binder M, Harper EP, Smyrk TC, Pardi DS. Optimization of a scoring system to predict microscopic colitis in a cohort of patients with chronic diarrhea. J Clin Gastroenterol. 2017;51(3):228–234. doi: 10.1097/MCG.0000000000000565. [DOI] [PubMed] [Google Scholar]
- 30.Bjørnbak C, Engel PJ, Nielsen PL, Munck LK. Microscopic colitis: clinical findings, topography and persistence of histopathological subgroups. Aliment Pharmacol Ther. 2011;34(10):1225–1234. doi: 10.1111/j.1365-2036.2011.04865.x. [DOI] [PubMed] [Google Scholar]
- 31.Stotzer PO, Abrahamsson H, Bajor A, et al. Are the definitions for chronic diarrhoea adequate? Evaluation of two different definitions in patients with chronic diarrhoea. United European Gastroenterol J. 2015;3(4):381–386. doi: 10.1177/2050640615580219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Protic M, Jojic N, Bojic D, et al. Mechanism of diarrhea in microscopic colitis. World J Gastroenterol. 2005;11(35):5535–5539. doi: 10.3748/wjg.v11.i35.5535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bürgel N, Bojarski C, Mankertz J, Zeitz M, Fromm M, Schulzke JD. Mechanisms of diarrhea in collagenous colitis. Gastroenterology. 2002;123(2):433–443. doi: 10.1053/gast.2002.34784. [DOI] [PubMed] [Google Scholar]
- 34.El-Salhy M, Lomholt-Beck B, Gundersen TD. High chromogranin A cell density in the colon of patients with lymphocytic colitis. Mol Med Rep. 2011;4(4):603–605. doi: 10.3892/mmr.2011.492. [DOI] [PubMed] [Google Scholar]
- 35.Wagner M, Stridsberg M, Peterson CG, Sangfelt P, Lampinen M, Carlson M. Increased fecal levels of chromogranin A, chromogranin B, and secretoneurin in collagenous colitis. Inflammation. 2013;36(4):855–861. doi: 10.1007/s10753-013-9612-4. [DOI] [PubMed] [Google Scholar]
- 36.Kane JS, Rotimi O, Everett SM, Samji S, Michelotti F, Ford AC. Development and validation of a scoring system to identify patients with microscopic colitis. Clin Gastroenterol Hepatol. 2015;13(6):1125–1131. doi: 10.1016/j.cgh.2014.12.035. [DOI] [PubMed] [Google Scholar]
- 37.Larsson JK, Sjöberg K, Vigren L, Benoni C, Toth E, Olesen M. Chronic non-bloody diarrhoea: a prospective study in Malmö, Sweden, with focus on microscopic colitis. BMC Res Notes. 2014;7(1):236. doi: 10.1186/1756-0500-7-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fernández-Bañares F, de Sousa MR, Salas A, et al. RECOMINA Project, GETECCU Grupo Español de Enfermedades de Crohn y Colitis Ulcerosa. Epidemiological risk factors in microscopic colitis: a prospective case-control study. Inflamm Bowel Dis. 2013;19(2):411–417. doi: 10.1002/ibd.23009. [DOI] [PubMed] [Google Scholar]
- 39.Fernández-Bañares F, Salas A, Forné M, Esteve M, Espinós J, Viver JM. Incidence of collagenous and lymphocytic colitis: a 5-year population-based study. Am J Gastroenterol. 1999;94(2):418–423. doi: 10.1111/j.1572-0241.1999.00870.x. [DOI] [PubMed] [Google Scholar]
- 40.Kamp EJ, Kane JS, Ford AC. Irritable bowel syndrome and microscopic colitis: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2016;14(5):659–668.e1. doi: 10.1016/j.cgh.2015.09.031. [DOI] [PubMed] [Google Scholar]
- 41.Hjortswang H, Tysk C, Bohr J, et al. Defining clinical criteria for clinical remission and disease activity in collagenous colitis. Inflamm Bowel Dis. 2009;15(12):1875–1881. doi: 10.1002/ibd.20977. [DOI] [PubMed] [Google Scholar]
- 42.Esteve M, Mahadevan U, Sainz E, Rodriguez E, Salas A, Fernández-Bañares F. Efficacy of anti-TNF therapies in refractory severe microscopic colitis. J Crohns Colitis. 2011;5(6):612–618. doi: 10.1016/j.crohns.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 43.Ozeki T, Ogasawara N, Izawa S, et al. Protein-losing enteropathy associated with collagenous colitis cured by withdrawal of a proton pump inhibitor. Intern Med. 2013;52(11):1183–1187. doi: 10.2169/internalmedicine.52.0232. [DOI] [PubMed] [Google Scholar]
- 44.Cottreau J, Kelly R, Topp T, Costa A, Filter ER, Arnason T. Spontaneous colonic perforation: a rare complication of collagenous colitis. Clin J Gastroenterol. 2016;9(3):140–144. doi: 10.1007/s12328-016-0652-9. [DOI] [PubMed] [Google Scholar]
- 45.Mitchell A, Dugas A. Collagenous colitis presenting as spontaneous perforation in an 80 year old woman: report of a case. BMC Gastroenterol. 2016;16(1):124. doi: 10.1186/s12876-016-0533-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Allende DS, Taylor SL, Bronner MP. Colonic perforation as a complication of collagenous colitis in a series of 12 patients. Am J Gastroenterol. 2008;103(10):2598–2604. doi: 10.1111/j.1572-0241.2008.01998.x. [DOI] [PubMed] [Google Scholar]
- 47.Bennett M, Tompkins H, Seymour B, O’Brien MJ, Farraye FA. Spontaneous colonic perforation in a patient with collagenous colitis. Gastroenterol Hepatol (N Y) 2013;9(4):262–264. [PMC free article] [PubMed] [Google Scholar]
- 48.von Arnim U, Ganzert C, Wex T, Schulz C, Malfertheiner P. Faecal calprotectin useful for clinical differentiation of microscopic colitis and irritable bowel syndrome. Gastroenterology. 2011;140(5):S-88. doi: 10.2147/CEG.S97701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wildt S, Nordgaard-Lassen I, Bendtsen F, Rumessen JJ. Metabolic and inflammatory faecal markers in collagenous colitis. Eur J Gastroenterol Hepatol. 2007;19(7):567–574. doi: 10.1097/MEG.0b013e328058ed76. [DOI] [PubMed] [Google Scholar]
- 50.Fine KD, Ogunji F, George J, Niehaus MD, Guerrant RL. Utility of a rapid fecal latex agglutination test detecting the neutrophil protein, lactoferrin, for diagnosing inflammatory causes of chronic diarrhea. Am J Gastroenterol. 1998;93(8):1300–1305. doi: 10.1111/j.1572-0241.1998.413_l.x. [DOI] [PubMed] [Google Scholar]
- 51.Carpenter HA, Tremaine WJ, Batts KP, Czaja AJ. Sequential histologic evaluations in collagenous colitis. Correlations with disease behavior and sampling strategy. Dig Dis Sci. 1992;37(12):1903–1909. doi: 10.1007/BF01308086. [DOI] [PubMed] [Google Scholar]
- 52.Offner FA, Jao RV, Lewin KJ, Havelec L, Weinstein WM. Collagenous colitis: a study of the distribution of morphological abnormalities and their histological detection. Hum Pathol. 1999;30(4):451–457. doi: 10.1016/s0046-8177(99)90122-3. [DOI] [PubMed] [Google Scholar]
- 53.Surawicz CM. Collating collagenous colitis cases. Am J Gastroenterol. 2000;95(1):307–308. doi: 10.1111/j.1572-0241.2000.01739.x. [DOI] [PubMed] [Google Scholar]
- 54.Wilcox GM, Mattia AR. Microscopic colitis associated with omeprazole and esomeprazole exposure. J Clin Gastroenterol. 2009;43(6):551–553. doi: 10.1097/MCG.0b013e31817d3fa1. [DOI] [PubMed] [Google Scholar]
- 55.Chande N, MacDonald JK, McDonald JW. Interventions for treating microscopic colitis: a Cochrane Inflammatory Bowel Disease and Functional Bowel Disorders Review Group systematic review of randomized trials. Am J Gastroenterol. 2009;104(1):235–241. doi: 10.1038/ajg.2008.16. [DOI] [PubMed] [Google Scholar]
- 56.Madisch A, Heymer P, Voss C, et al. Oral budesonide therapy improves quality of life in patients with collagenous colitis. Int J Colorectal Dis. 2005;20(4):312–316. doi: 10.1007/s00384-004-0660-y. [DOI] [PubMed] [Google Scholar]
- 57.Nguyen GC, Smalley WE, Vege SS, Carrasco-Labra A Clinical Guidelines Committee. American Gastroenterological Association Institute Guideline on the medical management of microscopic colitis. Gastroenterology. 2016;150(1):242–246. doi: 10.1053/j.gastro.2015.11.008. quiz e17-e18. [DOI] [PubMed] [Google Scholar]
- 58.Gentile NM, Abdalla AA, Khanna S, et al. Outcomes of patients with microscopic colitis treated with corticosteroids: a population-based study. Am J Gastroenterol. 2013;108(2):256–259. doi: 10.1038/ajg.2012.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Münch A, Bohr J, Miehlke S, et al. Low-dose budesonide for maintenance of clinical remission in collagenous colitis: a randomised, placebo-controlled, 12-month trial. Gut. 2016;65(1):47–56. doi: 10.1136/gutjnl-2014-308363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stewart MJ, Seow CH, Storr MA. Prednisolone and budesonide for short- and long-term treatment of microscopic colitis: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2011;9(10):881–890. doi: 10.1016/j.cgh.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 61.Miehlke S, Hansen JB, Madisch A, et al. Risk factors for symptom relapse in collagenous colitis after withdrawal of short-term budesonide therapy. Inflamm Bowel Dis. 2013;19(13):2763–2767. doi: 10.1097/01.MIB.0000438135.88681.98. [DOI] [PubMed] [Google Scholar]
- 62.Baert F, Schmit A, D’Haens G, et al. Belgian IBD Research Group; Codali Brussels. Budesonide in collagenous colitis: a double-blind placebo-controlled trial with histologic follow-up. Gastroenterology. 2002;122(1):20–25. doi: 10.1053/gast.2002.30295. [DOI] [PubMed] [Google Scholar]
- 63.Cino M, Greenberg GR. Bone mineral density in Crohn’s disease: a longitudinal study of budesonide, prednisone, and nonsteroid therapy. Am J Gastroenterol. 2002;97(4):915–921. doi: 10.1111/j.1572-0241.2002.05609.x. [DOI] [PubMed] [Google Scholar]
- 64.Fine KD, Lee EL. Efficacy of open-label bismuth subsalicylate for the treatment of microscopic colitis. Gastroenterology. 1998;114(1):29–36. doi: 10.1016/s0016-5085(98)70629-8. [DOI] [PubMed] [Google Scholar]
- 65.Miehlke S, Madisch A, Kupcinskas L, et al. Budesonide is more effective than mesalamine or placebo in short-term treatment of collagenous colitis. Gastroenterology. 2014;146(5):1222–1230.e1-2. doi: 10.1053/j.gastro.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 66.Calabrese C, Fabbri A, Areni A, Zahlane D, Scialpi C, Di Febo G. Mesalazine with or without cholestyramine in the treatment of microscopic colitis: randomized controlled trial. J Gastroenterol Hepatol. 2007;22(6):809–814. doi: 10.1111/j.1440-1746.2006.04511.x. [DOI] [PubMed] [Google Scholar]
- 67.Fernandez-Bañares F, Esteve M, Salas A, et al. Bile acid malabsorption in microscopic colitis and in previously unexplained functional chronic diarrhea. Dig Dis Sci. 2001;46(10):2231–2238. doi: 10.1023/a:1011927302076. [DOI] [PubMed] [Google Scholar]
- 68.Ung KA, Gillberg R, Kilander A, Abrahamsson H. Role of bile acids and bile acid binding agents in patients with collagenous colitis. Gut. 2000;46(2):170–175. doi: 10.1136/gut.46.2.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wildt S, Munck LK, Vinter-Jensen L, et al. Probiotic treatment of collagenous colitis: a randomized, double-blind, placebo-controlled trial with Lactobacillus acidophilus and Bifidobacterium animalis subsp. Lactis. Inflamm Bowel Dis. 2006;12(5):395–401. doi: 10.1097/01.MIB.0000218763.99334.49. [DOI] [PubMed] [Google Scholar]
- 70.Madisch A, Miehlke S, Eichele O, et al. Boswellia serrata extract for the treatment of collagenous colitis. A double-blind, randomized, placebo-controlled, multicenter trial. Int J Colorectal Dis. 2007;22(12):1445–1451. doi: 10.1007/s00384-007-0364-1. [DOI] [PubMed] [Google Scholar]
- 71.Cotter TG, Kamboj AK, Hicks SB, Tremaine WJ, Loftus EV, Pardi DS. Immune modulator therapy for microscopic colitis in a case series of 73 patients. Aliment Pharmacol Ther. 2017;46(2):169–174. doi: 10.1111/apt.14133. [DOI] [PubMed] [Google Scholar]
- 72.Pardi DS, Loftus EV, Jr, Tremaine WJ, Sandborn WJ. Treatment of refractory microscopic colitis with azathioprine and 6-mercaptopurine. Gastroenterology. 2001;120(6):1483–1484. doi: 10.1053/gast.2001.23976. [DOI] [PubMed] [Google Scholar]
- 73.Riddell J, Hillman L, Chiragakis L, Clarke A. Collagenous colitis: oral low-dose methotrexate for patients with difficult symptoms: long-term outcomes. J Gastroenterol Hepatol. 2007;22(10):1589–1593. doi: 10.1111/j.1440-1746.2007.05128.x. [DOI] [PubMed] [Google Scholar]
- 74.Varghese L, Galandiuk S, Tremaine WJ, Burgart LJ. Lymphocytic colitis treated with proctocolectomy and ileal J-pouch-anal anastomosis: report of a case. Dis Colon Rectum. 2002;45(1):123–126. doi: 10.1007/s10350-004-6126-z. [DOI] [PubMed] [Google Scholar]
- 75.Williams RA, Gelfand DV. Total proctocolectomy and ileal pouch anal anastomosis to successfully treat a patient with collagenous colitis. Am J Gastroenterol. 2000;95(8):2147–2147. doi: 10.1111/j.1572-0241.2000.02225.x. [DOI] [PubMed] [Google Scholar]
- 76.Järnerot G, Tysk C, Bohr J, Eriksson S. Collagenous colitis and fecal stream diversion. Gastroenterology. 1995;109(2):449–455. doi: 10.1016/0016-5085(95)90332-1. [DOI] [PubMed] [Google Scholar]