Abstract
Introduction:
Ankylosis may be defined as the fusion of the articular surfaces with bony or fibrous tissue. The treatment of temporomandibular joint ankylosis poses a significant challenge because of the high incidence of recurrence. A number of interpositional materials have been used including alloplastic materials (acrylic, proplast–teflon, silastic), and autogenous tissues (temporalis muscle flaps, buccal fat pad, dermis, costochondral grafts, metatarsal, fibula, tibia, iliac crest, cranial bone and Sternoclavicular graft SCG and cartilage). Literature suggests that rather than growth centre, we need adaptive centre. SCG is presumed to be a more suitable material for interpositional arthroplasty because Sternoclavicular Joint (SCJ) and TMJ are very similar developmentally, histologically and morphologically throughout the growth period.
Material and Method:
Patients with TMJ ankylosis (8 males, 2 females) underwent release of the ankylosed joint by the senior author, between June 2013 and Novemeber 2015. The age of the patients ranged from 10 to 19 years. Pre- and post- operative assessment included a thorough history and physical examination to determine the cause of ankylosis, the maximal incisal opening, etiology and type of the ankylosis, recurrence rate.
Result:
MIO at 6 months follow up was 37.4±2.633 mm (range 32-40 mm), greater than MIO achieved in immediate postoperatively {34.4±2.22 mm (range 30-38 mm). After reconstruction of temporomandibular joint with sternoclavicular graft in the growing child there was a significant increase in the growth of mandible which was stunned due to ankylosis. And the ramal height also increased.
Conclusion:
The articular reconstruction with alloplastic or autogenous grafts, or gap arthroplasty for the treatment of ankylosis is shown to be efficient in relation to the post-operative maximal incisal opening, recurrence and articular function.
Keywords: Gap arthroplasty, remodeling, sternoclavicular graft, temporomandibular joint ankyloses
INTRODUCTION
Ankylosis of the temporomandibular joint (TMJ) is one of the most disabling conditions which can afflict a person. Ankylosis is a Greek word meaning “stiff joint.” A slightly more complete definition of the term is an abnormal immobility and consolidation of a joint.[1] Relative to oral and maxillofacial surgery, the condition which comes to mind when speaking of ankylosis is the finding of complete bony fusion of mandible to the base of the skull. TMJ ankylosis is a joint disorder which refers to either bone or fibrous adhesion of the anatomic joint components and the ensuing loss of function.[2] This is the most dreaded sequel to TMJ disease and is a relatively rare occurrence in the developed world, today with the advent of better health care and early diagnosis and correct management. This is particularly true in young children who are completely unable to open their mouths. It is an extremely disabling condition which most commonly affects the growing child (Topazian, 1964), resulting in difficulty in opening the mouth, thereby causing problems in mastication and speech, potential airway obstruction, improper dental care, and a progressive facial deformity with its associated psychological and social effects.[3]
The only effective means of correcting this debilitating condition is surgery. In the growing child, the aims of the treatment are (Sugar and Pradhan, 1984) as follows: (1) early release of ankylosis with restoration and maintenance of normal functional articulation, (2) establishment of an area where adaptive growth can occur so that normal growth pattern can be restored, (3) correction of an existing deformity, and (4) prevent relapse.[4] Surgery is the treatment of choice in patients of TMJ ankylosis. Since the beginning, concepts followed in its surgical management have remained the field of debate and discussion among professionals. The goals of managing such a patient should be to establish movement, function in the jaw, prevent relapse, restore appearance, and achieve normal growth and occlusion in the child.[5]
A number of interpositional materials have been used including alloplastic materials (acrylic, proplast–teflon, and silastic)[2] and autogenous tissues (temporalis muscle flaps, buccal fat pad, dermis, costochondral grafts (CCGs), metatarsal, fibula, tibia, iliac crest, cranial bone, and sternoclavicular graft (SCG) and cartilage).[6,7,8,9] Conventionally, CCG has been used as an interpositional material as it has a growth center, but it has some complications such as uncontrolled growth of rib and donor-site complications. Literature suggests that rather than growth center, we need adaptive center. SCG is presumed to be a more suitable material for interpositional arthroplasty because sternoclavicular joint (SCJ) and TMJ are very similar developmentally, histologically, and morphologically throughout the growth period. The clavicular head contains layers of cartilage typical of mandibular condyle, i.e., articular, prechondroblastic, chondroblastic, hypertrophic, and endochondral ossification layers. Furthermore, cartilaginous cells are arranged in apparently random, noncolumnar, fashion such that of the condyle.[10] The aim of this study was to assess the stability, adaptability, and remodeling of the SCJ as an interpositional material in the reconstruction of ankylosed TMJ with the objectives of recording the maximal incisal opening (MIO) and protrusive and laterotrusive movements pre- and post-operatively along with radiological assessment (PA chest) to assess the donor-site morbidity.
MATERIAL AND METHOD
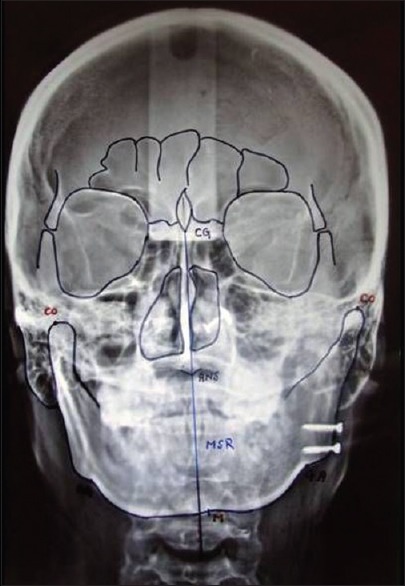
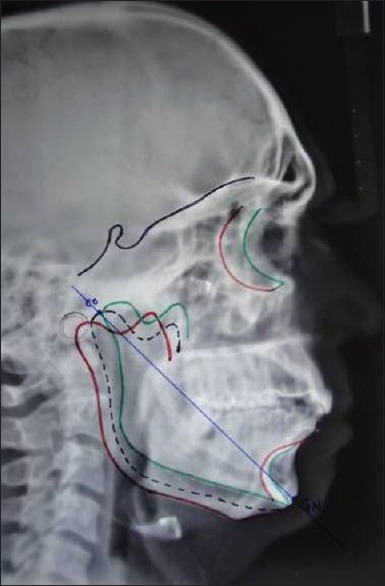
A total of 10 patients with TMJ ankylosis (8 males and 2 females) underwent release of the ankylosed joint by the senior author, between June 2013 and November 2015. The age of the patients ranged from 10 to 19 years. Limited mouth opening and asymmetry were the main complaints. In most cases, traumatic injury[6] in the chin region and ear infection[3] was the main etiology [Table 1]. All 10 patients (2 on the left and 8 on the right side) required unilateral release and sternoclavicular reconstruction. Preoperative assessment included a thorough history and physical examination to determine the cause of ankylosis, measurement of MIO, photographs and orthodontic evaluation of skeletal pattern, and occlusion and facial symmetry. Assessment of clinical parameters included mouth opening, lateral excursion, and protrusive movements at regular follow-up. Radiographic analysis included panoramic, cephalograms, computed tomography (CT) scan, and a posteroanterior (PA) view of the chest. CT scanning was used to clarify the status of the TMJ and for outlining the osseous mass. The PA chest radiograph was taken to assess the thickness of the clavicle and any abnormality. Cephalometric analysis was carried out using Grummons analysis of a PA cephalogram. The difference in length between the two mandibular rami was assessed by dropping a perpendicular from the mastoid to the bigonial line on each side and measuring the distance [Figure 1]. Lateral cephalograms were analyzed pre- and post-operatively to determine the length of the graft to restore the height of the ramus and to determine mandibular growth following grafting. The condylion–gonion and condylon–gnathion lengths were measured on the lateral cephalogram to assess any significant Changes subsequent to grafting [Figure 2].
Table 1.
Patient characteristics
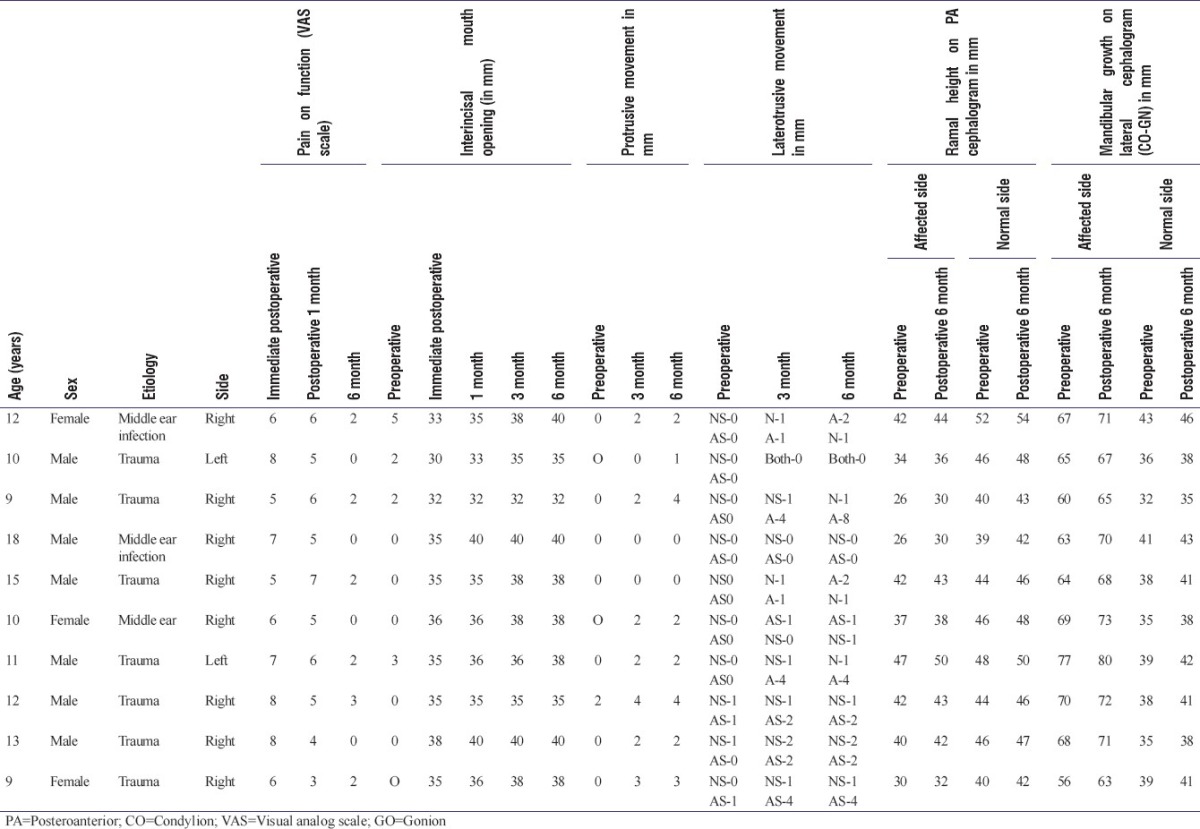
Figure 1.
Method to measure ramal height and chin deviation. CG=Crista galli, ANS=Anterior nasal spine, M=Menton, MSR=Midsagittal reference plane (CG=ANS-M), CO=Condylion, AG/GA=Gonion
Figure 2.
Method to measure mandibular growth (CO-GN). CO=Condylion, GN=Gnathion (Distance between condylion and Gnathion)
Surgical technique
All the patients were treated under general anesthesia with blind or fiber-optic naso-endotracheal intubation or tracheostomy. In all the cases, assess to TMJ was done using Al kayat Bramley incision with deep subfacial approach using CT scan as a guide to know the extent of ankylotic mass on the medial aspect. After releasing the ankylotic mass by gap arthroplasty (1.5–2 cm), intraoral coronoidectomy was performed on both the sides. TMJ was reconstructed using SCG. SCG was harvested from the ipsilateral side using supraclavicular incision, 1–2 cm above the clavicle. In female patients, the incision was kept 1–2 cm inferiorly for cosmetic reason. As proposed by Wolford et al., the incision extended from condylar head approximately 8–10 cm. Muscle attachments and periosteum were dissected from the superior and medial aspects of the clavicle. The integrity of the ligamentous attachment of the articular disc to the head of the clavicle was maintained. The superior half of the clavicle was used as a graft leaving the inferior part intact in all cases. To simulate the head of the condyle anatomically, the graft was prepared for insertion after shaping the cartilage. It is advisable to harvest the graft after osteoarthrotomy of the ankylosed bony part has been completed. The recipient bed was prepared to receive the graft by decorticating the lateral aspect of the ramus and preparing a groove wide enough to receive the graft. Multiple holes were made throughout the harvested graft for rapid revascularization. The graft was fixed on the lateral aspect of the ramus using 2.5 mm lag screws. A negative suction drain was then placed in the donor and recipient sites for 24–36 h after obtaining hemostasis. Subsequently, the muscle layer was sutured using 3-0 vicryl, and skin closure was done using 4-0 prolene at the donor site. On the other hand, the Alkayat and Bramley fascial closure was done using 3-0 vicryl and skin closure was done with 4-0 prolene. Pressure dressing was placed on both the sides for the next 48 h. Patients were instructed not to lift any heavy thing and not to use the arm for lifting themselves out of bed. Figure of eight bandage and arm strings were given to the patients if likelihood of clavicle fracture was suspected. Physiotherapy was started 1 week postoperatively and continued for 6 months. Regular follow-up was carried out weekly for a month, then at 3-month intervals for 1 year and yearly for the next 3 years.
All the surgeries were performed by the same surgeon. The clinical parameters including MIO pre- and post-operatively, facial asymmetry, protrusive movements, laterotrusive movements, and donor-site morbidity were evaluated. Furthermore, radiographic evaluation of recipient site was done for assessing stability, adaptability, and remodeling of the SCG using orthopantomogram, cephalogram, and CT scan/cone-beam CT. Figures 3-10 depict the pre- and post-operative images of one of the cases included in the study. Consent for the same was obtained from the patient).
Figure 3.

Preoperative frontal view
Figure 10.
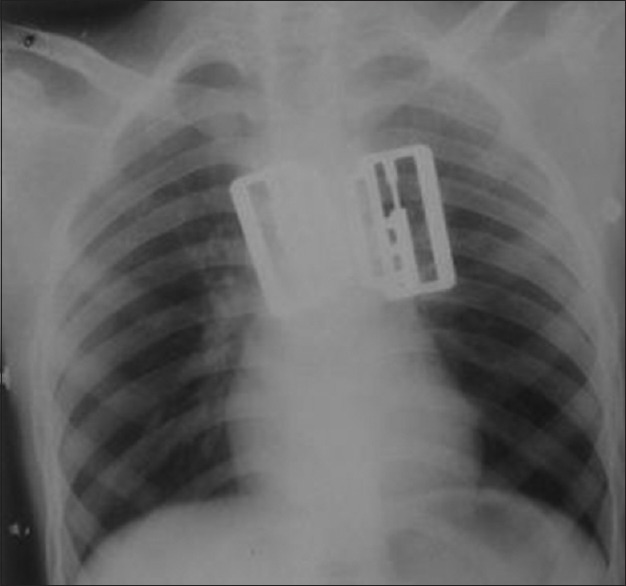
Immediate postoperative chest X-ray
Figure 4.

Preoperative mouth opening
Figure 5.

Preoperative orthopantomogram
Figure 6.

Preoperative chest X-ray
Figure 7.

Postoperative frontal view
Figure 8.

Postoperative mouth opening
Figure 9.

Postoperative orthopantomogram
Intra- and post-operative clinical pictures are shown in Figures 11-16.
Figure 11.

Marking to harvest sternoclavicular joint graft
Figure 16.

1-week postoperative at the harvested site
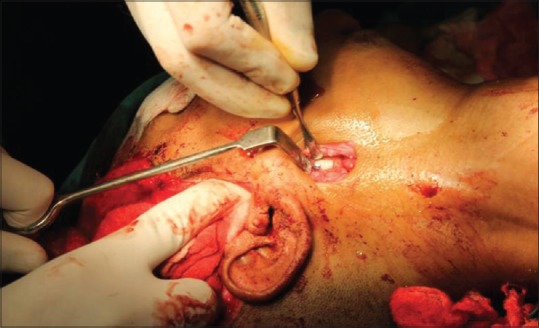
Figure 13.

Sternoclavicular joint graft being harvested
Figure 14.

The length of sternoclavicular joint graft
Figure 15.
Sternoclavicular joint graft in position after gap arthroplasty
RESULTS
The present study evaluated 10 cases (8 males and 2 females) of TMJ ankylosis operated in the Department of Oral and Maxillofacial surgery, SGT Dental College, Budhera, Gurgaon, which were followed for 1 year. All patients were operated by Gap arthroplasty with reconstruction by SCG. Mean age of the study group was 12.1 years. Etiology of TMJ ankylosis was ascertained on the basis of history given by the patients. Of 10 patients, trauma was the etiological factor in 7 patients (70%), and middle ear infection was the etiological factor in 3 patients (30%). Eight (80%) patients had right side ankylosis, and 2 had (20%) left side ankylosis. Of the 10 cases, 9 patients with the duration of ankylosis of ≥5 years had gross facial deformity marked by underdevelopment of the mandible on the affected side and chin deviation to the affected side. One patient had a duration of ankylosis of 2 years, and there was no facial deformity. All patients were in the growing period.
The range of movement was assessed by MIO, protrusion, and lateral excursions. Immediate postoperative MIO achieved was 34.4 ± mm (range 30–38 mm) and MIO at 6-month follow-up was 37.4 ± 2.633 mm (range 32–40 mm). Preoperative MIO was compared with immediate postoperative and with 6-month postoperative MIO. The results were found to be statistically significant.
DISCUSSION
Patients with ankylosis of TMJ usually present with a 2-fold problem: functional as well as esthetic. All affected patients present with the chief complaint of inability to open their mouth because of frozen joint. If, however, ankylosis should occur during the period of active growth, a predictable dentofacial deformity results. Over the past century and a half, many techniques of treatment for this affliction have been proposed and rejected. Controversy exists as to the ideal operation for true ankylosis. Interpositional arthroplasty is widely accepted as the primary surgical treatment for TMJ ankylosis. Rowe (1982)[10] laid down certain criteria for the restoration of ankylosed TMJ. The primary objective was the release of ankylosis by removing 1.5–2 cm of ankylotic mass, thus achieving a functional articulation with adequate mouth opening. He further emphasized that thereby mandibular growth can be restored in young children with the use of autogenous graft with growth potential, improving existing facial deformity. Inspite of implanting a growth center, the remnant facial deformity must be corrected by orthognathic procedures.
Autogenous tissue has become the preferred and safest graft material to be used as an interpositional material in TMJ reconstruction for reconstructing the TMJ, particularly in the past 20 years since recognition of the detrimental effects of alloplastic materials (i.e., silastic and proplast–teflon). Ear cartilage, fascia, temporalis muscle, pericranium, and dermis have all been used successfully to repair or replace the TMJ disc.[11]
Normal mandible behaves as a class 3 lever (a lever is defined as a rigid bar free to move about an axis of fulcrum). The condyle functions as fulcrum of rotation, elevator muscle as working forces, and food bolus as resisting force [Figure 12]. After gap arthroplasty, the system converts to class 1 lever with molar behaving as fulcrum of rotation, lying anterior to working force.[12] This phenomenon results in an imbalanced situation with the rotation of mandible upward and posteriorly leading to predisposition for open bite and misdirection for normal growth. Therefore, restoration of ramal height is very important for functional maintenance.[13,14]
Figure 12.

Exposure of the sternoclavicular joint site
Sir Harold Gillies was the first to use CCG joint for reconstruction of TMJ. The long-term results of reconstruction with CCG grafting for lengthening of the shortened ramus in the growing child tend to support the argument of those who see the condyle as a site for secondary adaptive and remodeling responses to changes in the enveloping soft tissue. The efficiency of CCGs in compensating for mandibular growth defects has been reported. The biggest drawbacks with CCGs are unpredictable growth, flexibility and elasticity of the bone, and warpage with continuous loading causing occlusal changes and fracture. This demands careful precautions to be taken such as immediate mobilization following grafting. Due to these problems, most traditionally accepted graft has created a background of dissatisfaction and the need for an alternative to overcome these drawbacks.
Mandible follows functional matrix theory in which condyle assumes a passive role and the functional matrix is the primary force.[15,16] Therefore, rather than growth center, we need adaptive center and for which SCG is presumed to be more suitable.
SCG in humans appears to be similar to the TMJ both anatomically and physiologically(Snyder et al. 1971).[16] The head of clavicle is composed of cartilage that is ontogenetically, phylogenetically, histologically, and embryologically similar to cartilage of mandibular condyle (Gardner 1968; Ellis and Carlson 1986).[17] It shows histomorphologic similarities to the TMJ in all stages of postnatal development (Ellis and Carlson 1986).[17] When grafted to the TMJ in monkeys, the SCG showed changes closer to those in TMJ than the CCG (Daniels, Ellis and Carlson 1987). Growth studies in monkeys with the SCJ showed no difference in growth characteristics between SCJ and TMJ over an 18-month period (Hennig, Ellis, Carlson, 1992).[18] For these above reasons, transplanting the SCJ to replace damaged TMJ articulations may produce better clinical results.
Out of all the three growth Centres (Metatarsal, SCG, and CCG) used in various studies over human beings, cephalometric analysis in relation to ramal height is available only for CCG in Wen-Ching et al. study.[19] Although Wolford has also done the cephalometric analysis of SCG for treatment objectives in few cases, he did not measure ramal height values.[20] We need a long-term radiographic follow-up for actual prediction of SCG behavior in terms of growth.
The graft can be placed on the mandibular ramus in any of the following positions for reconstruction: lateral aspect, along the posterior border and on the medial side. In our study, we placed the graft on the lateral surface of the ramus in all cases for revascularization and better graft adaptation. The graft was fixed to the ramus in all cases by lag screws or positional screws in the same way as Siemssen[21] and Wolford et al.[22,23,24]
In this study, we found postoperative results with MIO greater than 35 mm, the ability to make excursive movements, minimal to no pain during function, resumption of a normal diet, and nil pain at donor and recipient site at 1-year follow-up. Our results indicate the stability and adaptability of the SCG. In 5 cases, a second surgical procedure will have to be conducted for correction of facial asymmetry in patients with duration of ankylosis was more than 5 years. At 1-year follow-up, there was a complete regeneration of clavicle, and in 1 case, there was an overgrowth of the clavicle. Radiographs of SCG resonate the normal anatomy of TMJ.
On the basis of promising results of SCG, it may be a viable alternative to the traditional CCG in restoring the mechanics of mandible, thus providing near normal function and possibly a growth center in patients under 20 years of age. Hence, in terms of clinico-radiographic findings, we recommend routine use of this technique for TMJ reconstruction in TMJ ankylosis.
It is difficult to draw conclusions that may be applicable universally from a study of such small magnitude and duration. For anything conclusive to be said, further studies on a larger section and of a greater longitude will be required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Illustrated Medical Dictionary. 24th ed. Philadelphia: WB Saunders Company; 1965. [Google Scholar]
- 2.Zhi K, Ren W, Zhou H, Gao L, Zhao L, Hou C, et al. Management of temporomandibular joint ankylosis: 11 years’ clinical experience. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:687–92. doi: 10.1016/j.tripleo.2009.06.041. [DOI] [PubMed] [Google Scholar]
- 3.Topazian RG. Etiology of ankylosis of temporomandibular joint: Analysis of 44 cases. J Oral Surg Anesth Hosp Dent Serv. 1964;22:227–33. [PubMed] [Google Scholar]
- 4.Sugar AW, Pradhan R. Temporomandibular joint ankylosis in the growing child: Costochondral grafting as an approach to management. Indian J Surg. 1984;46:352–62. [Google Scholar]
- 5.James B, Danvelle S. Temporomandibular ankylosis. J Oral Surg. 1950;8:139–48. [Google Scholar]
- 6.Manganello-Souza LC, Mariani PB. Temporomandibular joint ankylosis: Report of 14 cases. Int J Oral Maxillofac Surg. 2003;32:24–9. doi: 10.1054/ijom.2002.0308. [DOI] [PubMed] [Google Scholar]
- 7.Verneuil A. De la cre´ation d’une fausse articulation par section ou re´section partielle de l’os maxillaire inferieur comme moyen de remedier a l’ankylose vraie ou fausse de la machoire inferieur. Arch Gen Med. 1860;15:174. [Google Scholar]
- 8.Topazian RG. Comparison of gap and interposition arthroplasty in the treatment of temporomandibular joint ankylosis. J Oral Surg. 1966;24:405–9. [PubMed] [Google Scholar]
- 9.Dimitroulis G. The interpositional dermis-fat graft in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 2004;33:755–60. doi: 10.1016/j.ijom.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Rowe NL. Ankylosis of the temporomandibular joint. Part 2. J R Coll Surg Edinb. 1982;27:167–73. [PubMed] [Google Scholar]
- 11.Hinds EC, Pleasants JE. Reconstruction of the temporomandibular joint. Am J Surg. 1955;90:931–9. doi: 10.1016/0002-9610(55)90725-x. [DOI] [PubMed] [Google Scholar]
- 12.Matsuura H, Miyamoto H, Ishimaru JI, Kurita K, Goss AN. Costochondral grafts in reconstruction of the temporomandibular joint after condylectomy: An experimental study in sheep. Br J Oral Maxillofac Surg. 2001;39:189–95. doi: 10.1054/bjom.2001.0622. [DOI] [PubMed] [Google Scholar]
- 13.Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990;48:1145–51. doi: 10.1016/0278-2391(90)90529-b. [DOI] [PubMed] [Google Scholar]
- 14.Silagi JL, Schow CE., Jr Temporomandibular joint arthroplasty: Review of literature and report of case. J Oral Surg. 1970;28:920–6. [PubMed] [Google Scholar]
- 15.Moss ML, Salentijn L. The primary role of functional matrices in facial growth. Am J Orthod. 1969;55:566–77. doi: 10.1016/0002-9416(69)90034-7. [DOI] [PubMed] [Google Scholar]
- 16.Snyder CC, Levine GA, Dingman DL. Trial of a sternoclavicular whole joint graft as a substitute for the temporomandibular joint. Plast Reconstr Surg. 1971;48:447–52. doi: 10.1097/00006534-197111000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Ellis E, 3rd, Carlson DS. Histologic comparison of the costochondral, sternoclavicular, and temporomandibular joints during growth in Macaca mulatta. J Oral Maxillofac Surg. 1986;44:312–21. doi: 10.1016/0278-2391(86)90082-0. [DOI] [PubMed] [Google Scholar]
- 18.Henning TB, Ellis E, 3rd, Carlson DS. Growth of the mandible following replacement of the mandibular condyle with the sternal end of the clavicle: An experimental investigation in Macaca mulatta. J Oral Maxillofac Surg. 1992;50:1196–206. doi: 10.1016/0278-2391(92)90154-r. [DOI] [PubMed] [Google Scholar]
- 19.Wen-Ching Ko E, Huang CS, Chen YR. Temporomandibular joint reconstruction in children using costochondral grafts. J Oral Maxillofac Surg. 1999;57:789–98. doi: 10.1016/s0278-2391(99)90816-9. [DOI] [PubMed] [Google Scholar]
- 20.Wolford LM, Cottrell DA, Henry C. Sternoclavicular grafts for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 1994;52:119–28. doi: 10.1016/0278-2391(94)90391-3. [DOI] [PubMed] [Google Scholar]
- 21.Siemssen SO. Temporomandibular arthroplasty by transfer of the sterno-clavicular joint on a muscle pedicle. Br J Plast Surg. 1982;35:225–38. doi: 10.1016/s0007-1226(82)90107-2. [DOI] [PubMed] [Google Scholar]
- 22.Wolford LM, Morales-Ryan CA, Morales PG, Cassano DS. Autologous fat grafts placed around temporomandibular joint total joint prostheses to prevent heterotopic bone formation. Proc (Bayl Univ Med Cent) 2008;21:248–54. doi: 10.1080/08998280.2008.11928404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolford LM, Karras SC. Autologous fat transplantation around temporomandibular joint total joint prostheses: Preliminary treatment outcomes. J Oral Maxillofac Surg. 1997;55:245–51. doi: 10.1016/s0278-2391(97)90535-8. [DOI] [PubMed] [Google Scholar]
- 24.Wolford LM, Smith BR. Sternoclavicular Grafts for Temporomandibular Joint Reconstruction. Presented at the AAOMS 69th Annual Meeting and Scientific Sessions Held in Anaheim, CA. 1987 [Google Scholar]


