Abstract
Objective:
The aim of this randomized clinical trial was to assess the efficacy of exclusive lingual nerve block (LNB) in achieving selective lingual soft-tissue anesthesia in comparison with conventional inferior alveolar nerve block (IANB).
Materials and Methods:
A total of 200 patients indicated for the extraction of lower premolars were recruited for the study. The samples were allocated by randomization into control and study groups. Lingual soft-tissue anesthesia was achieved by IANB and exclusive LNB in the control and study group, respectively. The primary outcome variable studied was anesthesia of ipsilateral lingual mucoperiosteum, floor of mouth and tongue. The secondary variables assessed were (1) taste sensation immediately following administration of local anesthesia and (2) mouth opening and lingual nerve paresthesia on the first postoperative day.
Results:
Data analysis for descriptive and inferential statistics was performed using SPSS (IBM SPSS Statistics for Windows, Version 22.0, Armonk, NY: IBM Corp. Released 2013) and a P < 0.05 was considered statistically significant. In comparison with the control group, the study group (LNB) showed statistically significant anesthesia of the lingual gingiva of incisors, molars, anterior floor of the mouth, and anterior tongue.
Conclusion:
Exclusive LNB is superior to IAN nerve block in achieving selective anesthesia of lingual soft tissues. It is technically simple and associated with minimal complications as compared to IAN block.
Keywords: Inferior alveolar nerve block, lingual nerve block, lingual soft-tissue, selective anesthesia
INTRODUCTION
Anesthesia which is highly selective and confined to the area of surgical concern is an essential part of surgical practice. Selective anesthetic techniques eliminate undesirable, concomitant anesthesia of tissues which are not involved in surgical procedure and may cause patient discomfort.
In the maxillofacial region, the anesthesia of different anatomic units is achieved by various nerve block techniques. When anesthesia of the lingual soft tissues, namely, the tongue, floor of the mouth and lingual mucoperiosteum is needed, the most commonly used technique is the inferior alveolar nerve block (IANB).[1] However, this is associated with anesthesia of the other adjacent areas innervated by the inferior alveolar nerve. The block anesthetizes the 3 terminal branches of the inferior alveolar nerve; (1) the inferior alveolar nerve which supplies the mandibular teeth; (2) Buccal nerve supplying the skin over buccinator, buccal mucous membrane, and buccal gingiva of molars; and (3) lingual nerve supplying the lingual gingiva, mucosa of anterior two-third of tongue, and floor of mouth.[2] As a result, patients experience various unwanted side effects such as anesthesia of lip, and chin.[1] Exclusive block technique for the lingual nerve is not practiced routinely, although there are numerous indications. Lingual soft-tissue anesthesia is indicated for a myriad of surgical procedures involving the lingual mucoperiosteum, floor of the mouth and tongue such as management of infection, suturing of traumatic lacerations, incision, or excision biopsy of pathological lesions, removal of sialolith,[3] periodontal surgery, surgical excision or marsupialization of cyst, lingual frenectomy,[4] surgical drainage of sublingual abscess, and removal of foreign body in the lingual region. The aim of this clinical trial is thus to compare the efficacy of exclusive lingual nerve block (LNB) with IANB in achieving exclusive lingual soft-tissue anesthesia.
MATERIALS AND METHODS
This study was designed and implemented as a single-blind, randomized, controlled clinical trial. The necessary approval for the study was obtained from the Institutional Review Board and was done in accordance with the consolidated standards of reporting trials statement [Figure 1]. The Helsinki's declaration guidelines were followed. A total of 200 patients who reported to the Department of Oral and Maxillofacial surgery for extraction of lower premolars were randomly selected for the study. All the patients were explained about the procedure, and informed consent was obtained.
Figure 1.
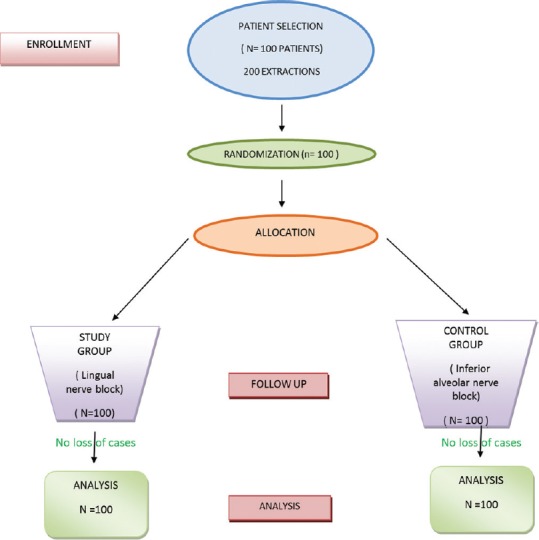
CONSORT Chart
The study sample involved patients requiring extraction of the mandibular premolar. The inclusion criteria consisted of patients aged 20–50 years and presence of lower second molar. Patients with infection or edentulous ridge in the lower molar region, patients aged above 60 years and absence of second mandibular molar were excluded from the study
The patient sample was allocated to two equal groups, control, and study by simple randomization; for each patient, lots were picked up from sealed envelopes containing the technique to be used
For the control group, the pulpal and lingual soft-tissue anesthesia was achieved by conventional IANB[5] which anesthetizes both inferior alveolar (1.5 ml) and lingual nerve (0.2 ml)
For the study group, the pulpal anesthesia was achieved by incisive nerve block and lingual soft-tissue anesthesia by the LNB as described below
A 2.5-ml syringe of 24 gauge (0.55 mm × 25 mm) with a 2 mm bevel (Dispovan, Hindustan syringes and medical devices Ltd, Faridabad, India) was used for both the injection techniques
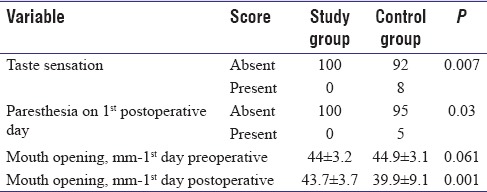
LNB: The point of insertion is distal to and 6–8 mm inferior to the lingual gingival margin of lower second molar [Figure 2]. The barrel of the syringe is placed over the contralateral incisor, canine region and angulated toward the lower second molar. The target area is the lingual nerve in the third molar region. The depth of penetration of needle is 5–8 mm. The volume of anesthetic solution to be injected is 0.5 ml[6]
Figure 2.
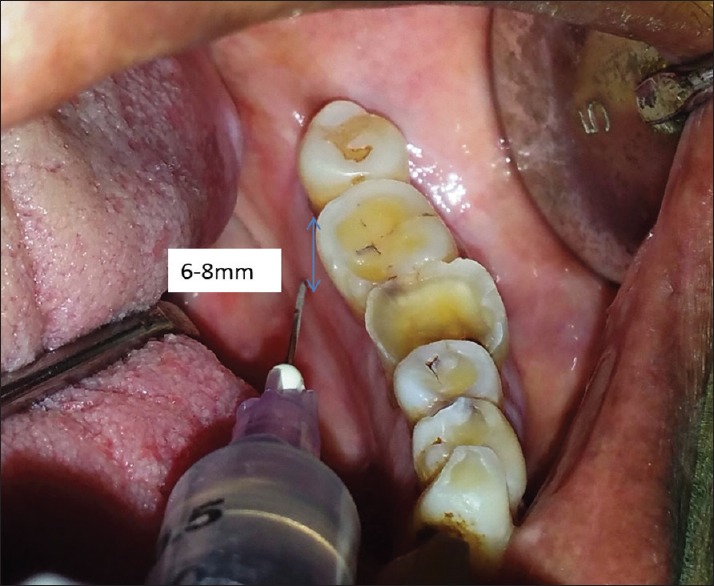
Lingual nerve block landmark
The local anesthetic solution used was Lignocaine Hydrochloride with1:80,000 adrenaline (“Lignocaine 2%” Indoco remedies Ltd, Changodar, Mumbai). The rate of injection was maintained at 1 ml/1 min[7]
The extraction procedure was standardized by a single operating surgeon performing all the extractions
The assessment of outcome parameters was done by an independent investigator who was blinded to the groups
-
Outcome parameters; The outcome parameters assessed were;
- Pain in the ipsilateral lingual mucoperiostium of molar, premolar, canine, and incisors
- Pain in the ipsilateral floor of the mouth – anterior and posterior
- Pain in the ipsilateral tongue – anterior and posterior
- Taste sensation in the ipsilateral tongue; present or absent
- Mouth opening; preoperative and on the 1st postoperative day
- Postinjection paresthesia on the 1st postoperative day.
Pain was assessed 5 min[8] after administration of LA injection using pin-prick test[9] in the anterior and posterior parts of the tongue and floor of the mouth as demarcated in the [Figure 3]. The pain in the lingual mucoperiosteum was checked in 3 zones; 1-molars, 2-premolars and canine, and 3-incisors [Figure 3]. The responses were given scores using the modified visual analog scale.[10] The taste sensation was assessed by application of sugar and salt solution using cotton bud.[11] A divider and scale were used to measure the inter-incisal mouth opening in millimeters. Paresthesia was recorded using[12] pin-prick test.
Figure 3.
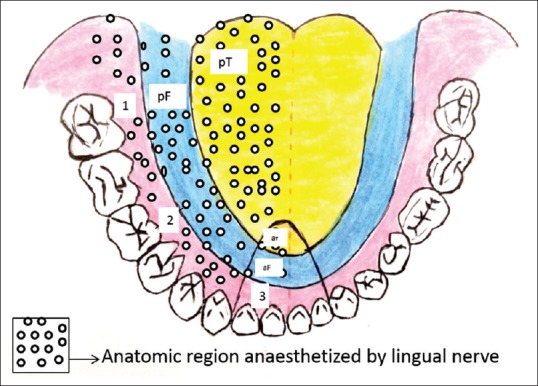
Anatomic zones to check pain 1- Lingual gingiva of molars 2- Lingual gingiva of canine & premolar 3- Lingual gingiva of incisors aF- anterior part of the floor of the mouth pF- posterior part of the floor of the mouth aT- anterior part of the tongue pT- posterior part of the tongue
Statistical tests
The normality tests Kolmogorov–Smirnov and Shapiro–Wilk's tests results revealed that variables followed normal distribution. Therefore, to analyze the data parametric methods were applied. To compare proportions Chi-Square test was used, if any expected cell frequency was <5 then Fisher's exact test was applied. To compare the mean values between study and control groups independent samples t-test was applied. To compare the mean values between time points paired t-test was applied. SPSS (IBM SPSS Statistics for Windows, Version 22.0, Armonk, NY: IBM Corp. Released 2013) was used to analyze the data. The P < 0.05 was considered statistically significant.
RESULTS
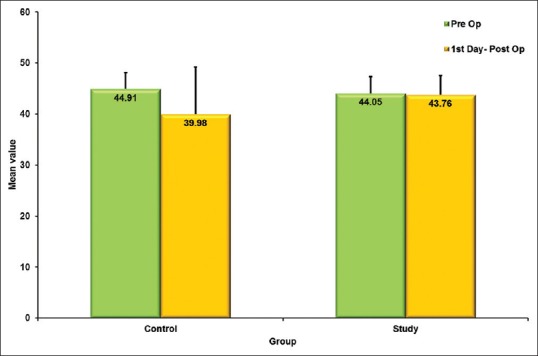
In comparison with the control group, the study group (LNB) showed statistically significant anesthesia in the lingual gingiva of incisors, molars, anterior floor of the mouth, and anterior tongue. All the patients in the study group demonstrated complete anesthesia (pain score-0) in relation to the lingual gingiva of canine, premolar, molar, posttongue, and postfloor of the mouth. However, in the control group, the percentage of patients who experienced complete anesthesia varied according to the site; 96% at the lingual gingiva of canine and premolar, 80% at molars, and 96% at posterior floor of the mouth and posterior tongue. The lingual gingiva at the canine, premolar, posterior floor of the mouth and tongue demonstrated superior anesthesia in the study group though it was statistically insignificant [Figures 4-6].
Figure 4.
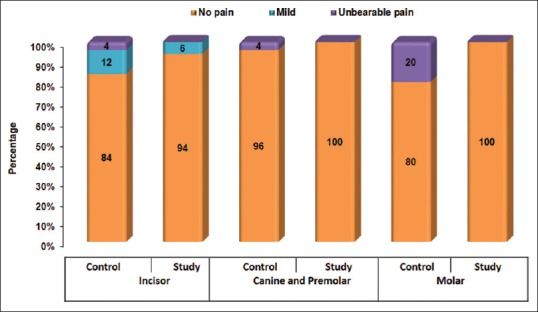
Graph demonstrating pain in the lingual gingiva
Figure 6.
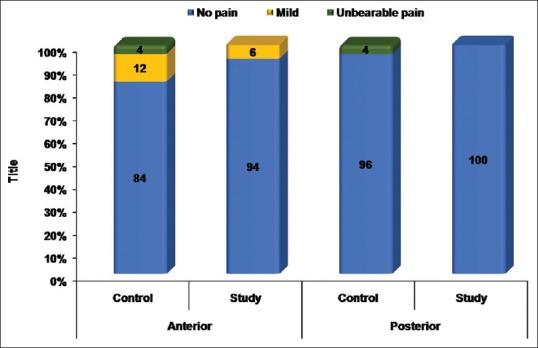
Graph demonstrating pain in the tongue
Figure 5.
Graph demonstrating pain in the floor of the mouth
No patient in the study group experienced unbearable pain in any of the sites. However, in the control group, unbearable pain was seen in 4% of patients at the lingual gingiva of incisors, canine and premolar, floor of the mouth (anterior and posterior), tongue (anterior and posterior), and 20% of patients at lingual gingiva of the molar.
The loss of taste sensation was noticed in 92% of patients in the control group and all patients in the study group. Lingual nerve paresthesia on the first postoperative day was present in 5% of patients in the control group in contrast to nil paresthesia in the study group.
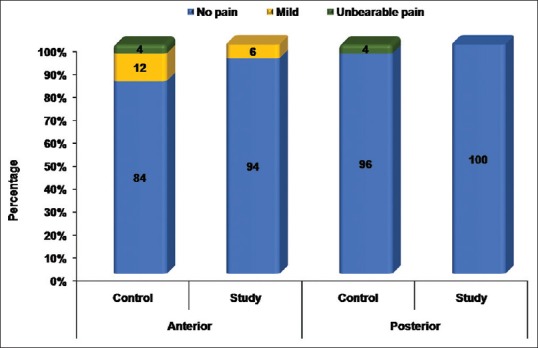
The difference between the mean 1st day postoperative mouth opening in the study and control group demonstrates less trismus in the study group which was statistically significant [Figure 7] (P < 0.001). The summary of primary and secondary outcomes variables are tabulated [Tables 1-3].
Figure 7.
Graph demonstrating Mean mouth opening on 1st post extraction day
Table 1.
Summary of primary outcome variables
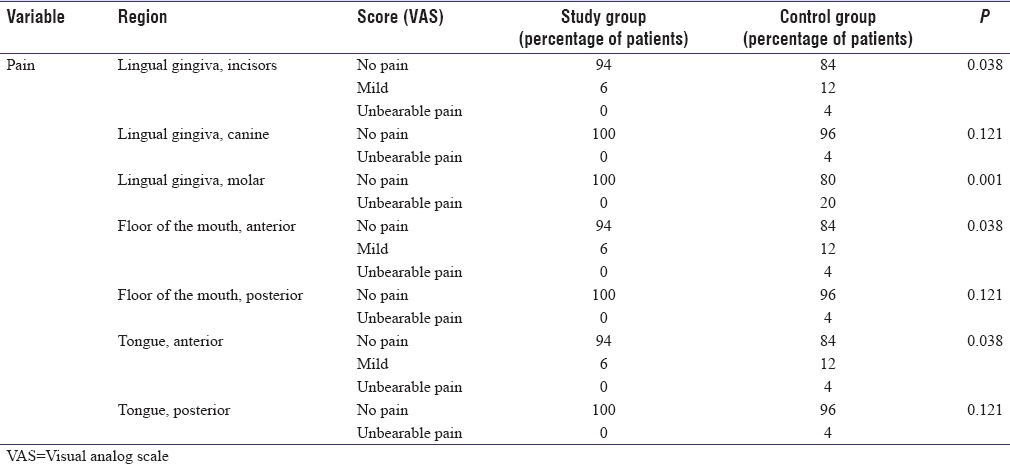
Table 3.
Demographic data
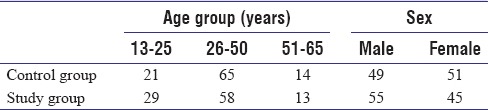
Table 2.
Summary of secondary outcome variable
DISCUSSION
Lingual soft-tissue anesthesia is indicated for the surgical management of numerous clinical conditions involving the lingual tissues such as traumatic lacerations, infections, minor pathological lesions, and presence of foreign body. It may also be required in managing painful clinical conditions such as glossodynia, eagle's syndrome,[13] lingual neuralgia,[14] and burning mouth syndrome.[15] Lingual anesthesia in such conditions is achieved by IANB which is accompanied by undesirable concomitant anesthesia of the lips, teeth, and chin which have clinical implications in some patients. Furthermore, there are potential complications associated with IANB such as nerve injury, trismus, facial paralysis, intravascular injection of local anesthetic solution, etc. The aim of this study was thus to choose an alternative to IAN block technique that eliminates the abovementioned adverse effects and produces selective lingual soft-tissue anesthesia. This clinical trial comparing the efficacy of the conventional IANB and exclusive LNB demonstrates the superiority of LNB in achieving selective lingual anesthesia. There has been no similar study done, so far. The primary drawback of IANB when used to anesthetize the lingual tissues is the concomitant anesthesia of the lip, chin, and teeth. This is undesirable and annoying especially in children, elderly, and mentally retarded patients in whom traumatic lip biting has been reported.[16,17] This complication may be eliminated with the use of exclusive LNB which offers exclusive anesthesia of lingual tissues. Besides, following IANB, there is a frequent failure of lingual nerve anesthesia[18,19] often necessitating a second injection. This can be attributed to multiple reasons, namely, greater depth of penetration to reach the target site (lingual nerve), individual variation in mandibular morphology, and technique sensitivity of IANB. In addition, the presence of accessory innervation contribute greatly to insufficient lingual anesthesia, especially at the lower third molar and retromolar region where collateral branches from the lingual nerve (81.2%) supply the lingual gingiva of the third molar region.[20,21] It is noteworthy that in comparison with IANB, our study showed a statistically significant success rate of exclusive LNB due to the ease of LNB technique in depositing LA solution closer to the lingual nerve, minimal depth of needle penetration and negligible anatomic variation in the site of needle penetration. The LNB technique as described by Balaji[6] describes a point of needle entry which is posteroinferior to the third molar. However, for this study, the point of needle insertion was precisely fixed at 6–8 mm inferior to the lingual gingival margin of mandibular second molar. This was based on the anatomical study of 669 nerves by Behnia et al.,[22] according to which the vertical distance from the lingual crest was 1.7–4 mm which ensured greater accuracy in reaching the nerve [Figure 8]. Furthermore, for this study, the target point of the needle was in relation to the second molar, in consideration of the fact that the third molar may or may not be present in all individuals. Nevertheless, the mild pain experienced by 6% of study group patients in the anterior floor of the mouth and anterior tip of tongue could be the result of cross-innervation of the lingual nerve in the anterior region as observed by Rusu et al.[23]
Figure 8.
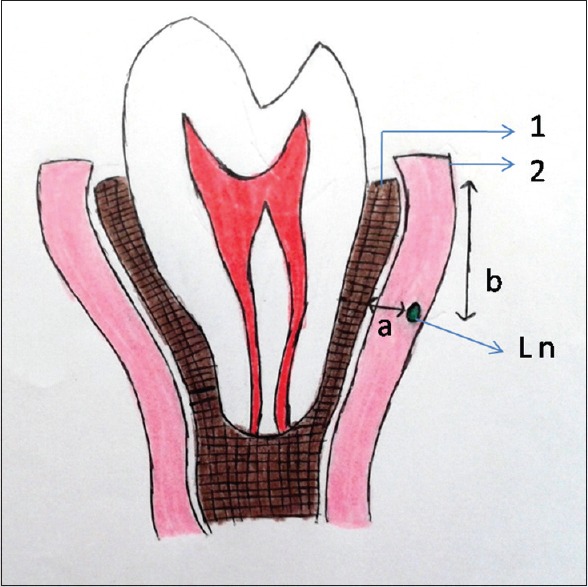
Position of the lingual nerve Ln- Lingual nerve 1- Lingual crest 2- Lingual gingiva a- Horizontal position of the lingual nerve from the lingual plate (0.00-3.20 mm) b- Vertical position of lingual nerve from lingual crest (1.70 to 4.00 mm)
Furthermore, the complications associated with injection technique are more with IANB. During injection, the proximity of the needle to the neurovascular bundle frequently results in complications such as hematoma,[24,25] paresthesia,[26] intravascular injection (incidence 15%– 20%),[27,28] and trismus.[25] This study has compared the incidence of paresthesia, loss of taste sensation, and trismus following both IANB and exclusive LNB.
Lingual nerve paresthesia is a bothersome clinical presentation following administration of local anesthesia.[26,29] The percentage of nerve injury following IAN block was found to be 4.5% in an anatomic study[30] which correlated with the clinical study by Harn and Durham who demonstrated 3.62%[31] of nerve injury. The fascicular pattern of a nerve determines the relative frequency of the nerve injury. A multifascicular nerve pattern is less prone to penetrating or blunt injury as compared to the unifascicular nerve. Lingual nerve is characteristically multifascicular at the third molar region and unifascicular at the pterygomandibular region in 33% of individuals.[32] This may account for the nil observation of paresthesia in the study (LNB) group of our study. On the contrary, the incidence of lingual nerve paresthesia following IANB in the control group was 5% although it was temporary.
Trismus is a common occurrence after IAN block. Postinjection trismus is mainly caused by needle injury to the masticatory muscles during injection.[25] With exclusive LNB, this is negated as the technique does not require passage of the needle through the muscles. Our study also demonstrated the same with no trismus observed in the study group as compared to the control group. Contrary to the IANB landmarks, the target area of exclusive LNB is not surrounded by vital structures like the neurovascular bundle. Hence, the risk of complications such as intravascular injection and hematoma are nil. The minimal depth of needle penetration in addition to ensuring precise injection technique and effective anesthesia, also avoids needle breakage which is possible with IANB.[33] Furthermore, the risk of facial nerve paralysis[34] associated with IANB is absolutely not possible with the exclusive LNB.
Thus, exclusive LNB offers many advantages; (1) greater success rate due to easier and closer access to the target area, (2) nil possibility of positive aspiration, and (3) less chances of postinjection trismus. The chance of failure of LNB is almost nil as established by this study. This is because the target site is precisely and easily reached due to the superficial position of the nerve and reduced penetration depth. Finally, the most important advantage associated with LNB is the exclusive lingual soft-tissue anesthesia without the concomitant pulpal or soft-tissue anesthesia of the lip or buccal soft tissues. Bilateral LNB may also be administered without patient discomfort. Nevertheless, LNB is contraindicated in infection of lingual soft tissue.
CONCLUSION
Exclusive LNB is superior to the IAN nerve block in achieving selective anesthesia of the lingual soft tissues. Exclusive LNB has definite clinical indications. It is technically simple and associated with minimal complications as compared to IAN block.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Malamed SF. Handbook of Local Anesthesia. 6th ed. St. Louis, Missouri: Elsevier; 2013. p. 227. [Google Scholar]
- 2.Standring S. Gray's Anatomy. The Anatomical Basis of Clinical Practice. 39th ed. Philadelphia, USA: Elsevier; 2005. p. 524. [Google Scholar]
- 3.Langdon J, Patel M, Ord R, Brennan P. Operative Oral and Maxillofacial Surgery. 2nd ed. London: Hodder and Stoughton Limited; 2009. p. 366. [Google Scholar]
- 4.Miloro M, Ghali GE, Larsen PE, Waite PD. Peterson's Principles of Oral and Maxillofacial Surgery. 3rd ed. USA, Shelton: People's Medical Publishing House; 2011. p. 142. [Google Scholar]
- 5.Malamed SF. Handbook of Local Anesthesia. 6th ed. St. Louis, Missouri: Elevier; 2013. pp. 228–33. [Google Scholar]
- 6.Balaji SM. Textbook of Oral and Maxillofacial Surgery. 2nd ed. New Delhi, India: Elsevier; 2013. p. 191. [Google Scholar]
- 7.Bennet RC. Monheim's Local Anesthesia and Pain Control in Dental Practice. 7th ed. Ontario, Canada: B.C. Decker; 1990. p. 147. [Google Scholar]
- 8.Bennet RC. Monheim's Local Anesthesia and Pain Control in Dental Practice. 7th ed. Ontario, Canada: B.C. Decker; 1990. p. 106. [Google Scholar]
- 9.Malamed SF. Handbook of Local Anesthesia. 6th ed. St. Louis, Missouri: Elevier; 2013. p. 235. [Google Scholar]
- 10.Panneerselvam E, Balasubramanian S, Raja VB, Kannan R, Rajaram K, Rajendra Sharma A, et al. ‘Plain lignocaine’ vs. ‘lignocaine with vasoconstrictor’-comparative evaluation of pain during administration and post-extraction wound healing by a double blinded randomized controlled clinical trial. Acta Odontol Scand. 2016;74:374–9. doi: 10.3109/00016357.2016.1160148. [DOI] [PubMed] [Google Scholar]
- 11.Kumar GS. Orban's Oral Histology and Embryology. 6th ed. New Delhi, India: Elsevier; 2011. p. 270. [Google Scholar]
- 12.Ghali GE, Epker BN. Clinical neurosensory testing: Practical applications. J Oral Maxillofac Surg. 1989;47:1074–8. doi: 10.1016/0278-2391(89)90184-5. [DOI] [PubMed] [Google Scholar]
- 13.Jain S, Bansal A, Paul S, Prashar DV. Styloid-stylohyoid syndrome. Ann Maxillofac Surg. 2012;2:66–9. doi: 10.4103/2231-0746.95326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rehman SU, Khan MZ, Hussain R, Jamshed A. Pulsed radiofrequency modulation for lingual neuralgia. Br J Oral Maxillofac Surg. 2012;50:e4–5. doi: 10.1016/j.bjoms.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Grémeau-Richard C, Dubray C, Aublet-Cuvelier B, Ughetto S, Woda A. Effect of lingual nerve block on burning mouth syndrome (stomatodynia): A randomized crossover trial. Pain. 2010;149:27–32. doi: 10.1016/j.pain.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 16.Malamed SF. Handbook of Local Anesthesia. 6th ed. St. Louis, Missouri: Elevier; 2013. p. 302. [Google Scholar]
- 17.Chi D, Kanellis M, Himadi E, Asselin ME. Lip biting in a pediatric dental patient after dental local anesthesia: A case report. J Pediatr Nurs. 2008;23:490–3. doi: 10.1016/j.pedn.2008.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khalil H. A basic review on the inferior alveolar nerve block techniques. Anesth Essays Res. 2014;8:3–8. doi: 10.4103/0259-1162.128891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thangavelu K, Kannan R, Kumar NS, Rethish E, Sabitha S, Sayeeganesh N, et al. Significance of localization of mandibular foramen in an inferior alveolar nerve block. J Nat Sci Biol Med. 2012;3:156–60. doi: 10.4103/0976-9668.101896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim SY, Hu KS, Chung IH, Lee EW, Kim HJ. Topographic anatomy of the lingual nerve and variations in communication pattern of the mandibular nerve branches. Surg Radiol Anat. 2004;26:128–35. doi: 10.1007/s00276-003-0179-x. [DOI] [PubMed] [Google Scholar]
- 21.Rodella LF, Buffoli B, Labanca M, Rezzani R. A review of the mandibular and maxillary nerve supplies and their clinical relevance. Arch Oral Biol. 2012;57:323–34. doi: 10.1016/j.archoralbio.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 22.Behnia H, Kheradvar A, Shahrokhi M. An anatomic study of the lingual nerve in the third molar region. J Oral Maxillofac Surg. 2000;58:649–51. doi: 10.1016/s0278-2391(00)90159-9. [DOI] [PubMed] [Google Scholar]
- 23.Rusu MC, Nimigean V, Podoleanu L, Ivaşcu RV, Niculescu MC. Details of the intralingual topography and morphology of the lingual nerve. Int J Oral Maxillofac Surg. 2008;37:835–9. doi: 10.1016/j.ijom.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 24.Vasconcelos BC, Freitas KC, Canuto MR. Frequency of positive aspirations in anesthesia of the inferior alveolar nerve by the direct technique. Med Oral Patol Oral Cir Bucal. 2008;13:E371–4. [PubMed] [Google Scholar]
- 25.Blanton PL, Jeske AH. ADA Council on Scientific Affairs, ADA Division of Science. Avoiding complications in local anesthesia induction: Anatomical considerations. J Am Dent Assoc. 2003;134:888–93. doi: 10.14219/jada.archive.2003.0288. [DOI] [PubMed] [Google Scholar]
- 26.Pogrel MA, Thamby S. Permanent nerve involvement resulting from inferior alveolar nerve blocks. J Am Dent Assoc. 2000;131:901–7. doi: 10.14219/jada.archive.2000.0308. [DOI] [PubMed] [Google Scholar]
- 27.Frangiskos F, Stavrou E, Merenditis N, Tsitsogianis H, Vardas E, Antonopoulou I, et al. Incidence of penetration of a blood vessel during inferior alveolar nerve block. Br J Oral Maxillofac Surg. 2003;41:188–9. doi: 10.1016/s0266-4356(03)00045-7. [DOI] [PubMed] [Google Scholar]
- 28.Taghavi Zenouz A, Ebrahimi H, Mahdipour M, Pourshahidi S, Amini P, Vatankhah M, et al. The incidence of intravascular needle entrance during inferior alveolar nerve block injection. J Dent Res Dent Clin Dent Prospects. 2008;2:38–41. doi: 10.5681/joddd.2008.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hillerup S, Jensen R. Nerve injury caused by mandibular block analgesia. Int J Oral Maxillofac Surg. 2006;35:437–43. doi: 10.1016/j.ijom.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 30.Morris CD, Rasmussen J, Throckmorton GS, Finn R. The anatomic basis of lingual nerve trauma associated with inferior alveolar block injections. J Oral Maxillofac Surg. 2010;68:2833–6. doi: 10.1016/j.joms.2010.06.193. [DOI] [PubMed] [Google Scholar]
- 31.Harn SD, Durham TM. Incidence of lingual nerve trauma and postinjection complications in conventional mandibular block anesthesia. J Am Dent Assoc. 1990;121:519–23. doi: 10.14219/jada.archive.1990.0198. [DOI] [PubMed] [Google Scholar]
- 32.Pogrel MA, Schmidt BL, Sambajon V, Jordan RC. Lingual nerve damage due to inferior alveolar nerve blocks: A possible explanation. J Am Dent Assoc. 2003;134:195–9. doi: 10.14219/jada.archive.2003.0133. [DOI] [PubMed] [Google Scholar]
- 33.Faura-Solé M, Sánchez-Garcés MA, Berini-Aytes L, Gay-Escoda C. Broken anesthetic injection needles: Report of 5 cases. Quintessence Int. 1999;30:461–5. [PubMed] [Google Scholar]
- 34.Tzermpos FH, Cocos A, Kleftogiannis M, Zarakas M, Iatrou I. Transient delayed facial nerve palsy after inferior alveolar nerve block anesthesia. Anesth Prog. 2012;59:22–7. doi: 10.2344/11-03.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


