Abstract
Background
Anterior cruciate ligament injury results in altered kinematics and kinetics in the knee and hip joints that persist despite surgical reconstruction and rehabilitation. Abnormal movement patterns and a history of osteoarthritis are risk factors for articular cartilage degeneration in additional joints. The purpose of this study was to determine if hip joint biomechanics early after anterior cruciate ligament injury and reconstruction differ between patients with and without post-traumatic knee osteoarthritis 5 years after reconstruction. The study’s rationale was that individuals who develop knee osteoarthritis after anterior cruciate ligament injury may also demonstrate large alterations in hip joint biomechanics.
Methods
Nineteen athletes with anterior cruciate ligament injury completed standard gait analysis before (baseline) and after (post-training) extended pre-operative rehabilitation and at 6 months, 1 year, and 2 years after reconstruction. Weightbearing knee radiographs were completed 5 years after reconstruction to identify medial compartment osteoarthritis.
Findings
Five of 19 patients had knee osteoarthritis at 5 years after anterior cruciate ligament reconstruction. Patients with knee osteoarthritis at 5 years walked with smaller sagittal plane hip angles (P: 0.043) and lower sagittal (P: 0.021) and frontal plane (P: 0.042) external hip moments in the injured limb before and after reconstruction compared to those without knee osteoarthritis.
Interpretation
The current findings suggest hip joint biomechanics may be altered in patients who develop post-traumatic knee osteoarthritis. Further study is needed to confirm whether the risk of non-traumatic hip pathology is increased after anterior cruciate ligament injury and if hip joint biomechanics influence its development.
Keywords: OA, ACL, moments, gait
1. INTRODUCTION
Anterior cruciate ligament (ACL) injury is a musculoskeletal pathology in the knee that results in altered movement patterns1–4 that persist despite surgical reconstruction and rehabilitation.5–12 Changes in joint kinematics and kinetics after ACL injury have been postulated to initiate degeneration of joints both directly and indirectly affected by the injury, by altering the location and magnitude of load bearing regions of articular cartilage.13 For example, altered knee mechanics early after ACL injury have been linked to radiographic osteoarthritis (OA) within the tibiofemoral joint.14 Aberrant kinematics and kinetics are also associated with OA in joints indirectly affected by ACL injury, such as the patellofemoral joint.15,16 An increased risk of patellofemoral joint OA in the presence of abnormal knee biomechanics suggests other joints in the lower extremity chain may also be at risk of joint pathology.
Movement patterns in the hip joint of the injured limb are also altered after ACL injury.17–24 Ferber et al. hypothesized that changes in movement patterns in the hip may be a compensatory effort by ACL-deficient individuals to reduce anterior tibial translation.22 Biomechanical hip strategies appear to be dependent on the extent of aberrant joint motion at the knee. Patients with smaller knee joint moments, angles, and excursions during gait display smaller hip joint moments, angles, and excursions in the sagittal plane compared to those with more normal gait patterns after ACL injury.19,25–27 Because individuals who develop post-traumatic knee OA demonstrate biomechanical knee asymmetry early after ACL injury,14 and because larger alterations in knee joint biomechanics lead to larger alterations in hip joint biomechanics, patients who develop knee OA after ACL injury may demonstrate greater changes in hip joint movement patterns than those who do not develop post-traumatic knee OA.
The purpose of this study was to determine if hip joint biomechanics early after ACL injury and reconstruction differ between patients with and without post-traumatic knee OA at 5 years after ACL reconstruction. Because smaller knee joint angles and moments are associated with reduced hip joint angles and moments and also with post-traumatic knee OA development, we hypothesized that patients with radiographic knee OA at 5 years after ACL reconstruction would demonstrate asymmetrically smaller hip joint angles and moments in the involved hip early after injury and reconstruction compared to those without radiographic knee OA at 5 years. The findings of this study will provide rationale for whether further investigation of abnormal movement patterns at the hip is warranted in individuals at risk for post-traumatic knee OA after ACL injury. If alterations in hip biomechanics are found in individuals with post-traumatic knee OA, future study will be needed to determine if these changes in hip biomechanics also predispose these individuals to the development of hip pathology.
2. METHODS
2.1 Subjects
Nineteen patients were included. All had been part of a larger, randomized control trial of 55 patients determining the effects of augmenting pre-operative rehabilitation with specialized neuromuscular training called perturbation training.28 All patients had a complete, unilateral ACL injury (confirmed by a positive Lachman test and 3-mm or greater difference in anterior tibial excursion with instrumented arthrometry (KT1000; MEDmetric Corporation, San Diego, CO)29 within the previous 7 months and were between the ages of 14–51. Patients were regular participants in level I (e.g. soccer, basketball) or II (e.g. tennis, downhill skiing) cutting and pivoting activities29,30 prior to injury and demonstrated dynamic knee instability after injury (classified as noncopers pre-operatively31). Exclusion criteria included a repairable meniscus, symptomatic grade III injury to other knee ligaments, and full-thickness articular cartilage lesions greater than 1 cm2. This study was approved by the Institutional Review Board at the University of Delaware and all patients completed written informed consent.
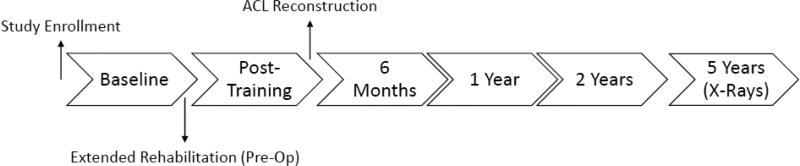
Patients were initially enrolled in this study within 7 months of ACL injury after effusion, range of motion, pain, and obvious gait impairments were resolved and quadriceps strength was at least 70% of the uninvolved limb through utilization of a physical therapy protocol described by Hurd et al.32 Following study enrollment, patients completed an additional 10 pre-operative rehabilitation sessions to further restore lower extremity strength and neuromuscular control.28 All patients underwent ACL reconstruction by a single, board-certified orthopedic surgeon using either a four-bundle semitendinosus-gracilis autograft or soft tissue allograft. Progressive, criterion-based post-operative rehabilitation was completed by all patients early after surgery.33 Gait analysis was completed at 5 time points (Figure 1): pre-operatively after initial impairment resolution (baseline), immediately following 10 sessions of additional pre-operative rehabilitation (post-training), 6 months after ACL reconstruction (6 months), 1 year after ACL reconstruction (1 year), and 2 years after ACL reconstruction (2 years). Radiographs were completed 5 years after ACL reconstruction.
Fig. 1.
Timeline of patient data collections for gait analysis (baseline, post-training, 6 months, 1 year, 2 years) and knee radiographs (5 years).
2.2 Gait Analysis
Kinematic and kinetic data was collected during gait analysis at baseline, post-training, 6 month, 1 year, and 2 year testing. Eight infrared cameras (VICON, Oxford Metrics Ltd., London, UK) sampled at 120 Hz were used to detect the position of sixteen-millimeter spherical retro-reflective markers placed at each iliac crest, greater trochanter, medial and lateral femoral epicondyle, medial and lateral malleoli, superior and inferior heel, base of the first metatarsal, and base of the fifth metatarsal. This marker set has previously been shown to have excellent intersession reliability.34 Rigid, thermoplastic shells each with four markers were secured laterally at each thigh and shank, and a pelvic shell with three markers was secured midway between the posterior superior iliac spines to track segment motion during gait. A standing calibration was used to identify joint centers and create local coordinate systems for each segment.
Patients walked at a self-selected speed along a 6-meter walkway with an embedded force plate sampled at 1,080 Hz (Bertec Corporation, Worthington, OH). Walking speed was established during the baseline testing session and maintained (±5%) at each follow-up session using a timing system. Stance phase joint angles and external moments were processed using inverse dynamics within custom software (Visual 3D, C-Motion, Germantown, MD) as the average of 5 walking trials. Kinematic and kinetic data were low pass filtered at 6 Hz and 40 Hz, respectively. Initial contact and end of stance were identified using a 50-Newton threshold. All trials were normalized to 100% of stance. External moments were normalized to mass (kg) and height (m). Variables of interest were peak hip joint angles and external moments during any part of stance phase in the sagittal plane and during the first 50% of stance phase (weight acceptance) in the frontal plane. Hip joint excursion was calculated as the difference between the peak hip flexion angle and peak hip extension angle during stance. Interlimb differences in joint angles and external moments were also calculated for each variable (involved limb minus uninvolved limb).
2.3 Radiographs
Patients completed bilateral weightbearing posterior-anterior (PA) bent knee (30°) radiographs 5 years after ACL reconstruction. SigmaView software (Agfa HealthCare Corporation, Greenville, SC) was used to view radiographs. The Kellgren-Lawrence (KL) system was used to grade OA in the medial tibiofemoral compartment.35 We have demonstrated excellent between-day, intrarater reliability for KL grading using 20 radiographs included in a larger project of patients at 5 years after ACL injury (graded by EW; Cohen’s kappa (κ): 0.904, p: <0.001). All Kellgren-Lawrence grades were verified by a board-certified orthopedic surgeon. The presence of OA in the medial tibiofemoral compartment was operationally defined as a KL grade greater than or equal to 2.
2.4 Statistical Analysis
Statistical analyses were completed using PASSW 23.0 software (SPSS Inc., Chicago, IL). Independent t-tests and Fisher’s exact tests were used to test differences in baseline characteristics and concomitant injuries between those with and without radiographic knee OA (OA, nonOA) 5 years after ACL reconstruction. Two-way mixed design analyses of variance (ANOVA) were used to test differences in hip joint angles and external moments (separate model for the involved limb and for the interlimb difference in each variable) with a between subjects factor of OA and within subjects factor of time. Post-hoc testing was completed using Bonferroni corrections. Minimal detectable change (MDC) values for interlimb differences in hip kinematics and kinetics were established from 15 healthy, active subjects (Table 1) tested within our lab at self-selected gait speed. Minimal detectable changes and effect sizes (ES)36 were used qualitatively to determine if meaningful asymmetry existed between limbs. A priori statistical significance was set at α≤0.05.
Table 1.
Minimal detectable change (MDC) values at a 95% confidence interval for interlimb differences in sagittal and frontal plane hip kinematics and kinetics during gait.
| Gait Variable during Stance | MDC95 |
|---|---|
| Peak Hip Flexion Angle | 3° |
| Peak Hip Extension Angle | 2° |
| Hip Excursion Angle | 4° |
| Peak Hip Adduction Angle | 3° |
| Peak Hip Flexion Moment | 0.08 Nm/kg·m |
| Peak Hip Extension Moment | 0.04 Nm/kg·m |
| Peak Hip Adduction Moment | 0.06 Nm/kg·m |
3. RESULTS
3.1 Baseline Characteristics
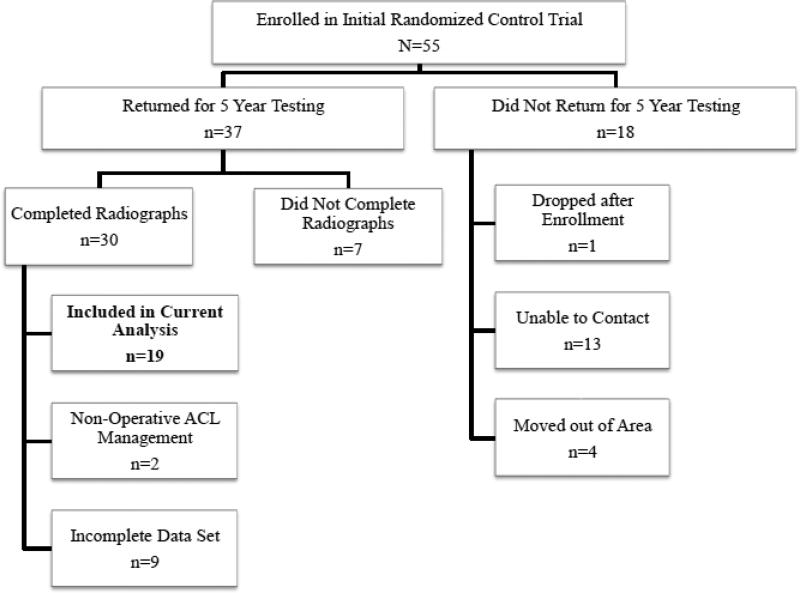
In total, 19 patients completed gait analysis at all 5 time points (baseline, post-testing, 6 months, 1 year, and 2 years) and radiographs 5 years after ACL reconstruction (Figure 2). Five patients demonstrated radiographic medial compartment OA in their ACL-injured knee at 5 years while 14 did not. No differences in knee symptoms and function were present at 5 years after ACL reconstruction between those with and without medial knee OA on the Knee Outcome Survey Activities of Daily Living Scale37 (P: 0.075, no knee OA: 98.5 (SD: 3.1); knee OA: 94.9 (SD: 5.1)), the International Documentation Committee 2000 Subjective Knee Form38 (P: 0.123, no knee OA: 95.9 (SD: 7.3); knee OA: 89.9 (SD: 6.3)), or worst pain scores on a 0–10 point visual analog scale (P: 0.779, no knee OA: 0.1 (SD: 0.4); knee OA: 0.2 (0.4)). No baseline differences existed in age, mass, body mass index (BMI), sex, pre-injury cutting and pivoting activity level, graft type, or gait speed between those did and did not later develop knee OA (Table 2). There were also no group differences in the time between ACL injury to baseline testing nor to ACL reconstruction, or from ACL reconstruction to 5-year radiographic testing (Table 2). Further, the proportion of patients who had radiographic lateral compartment knee OA in the involved limb or medial compartment OA in the uninvolved limb did not differ between those with and without involved limb medial compartment knee OA at 5 years (Table 2).
Figure 2.
Floe diagram of study cohort.
Table 2.
Baseline and concomitant injury characteristics between those with and without radiographic medial compartment knee OA 5 years after ACL reconstruction. Standard deviation within parentheses.
| nonOA (n=14) |
OA (n=5) |
P- value |
|
|---|---|---|---|
| Age (baseline) (yrs) | 32.1 (11.0) | 33.4 (13.1) | 0.837 |
| Mass (kg) | 87.1 (14.4) | 84.0 (17.5) | 0.703 |
| Body Mass Index (kg/m2) | 27.8 (3.2) | 27.6 (5.2) | 0.912 |
| Time from injury to basline (wks) | 4.7 (4.5) | 5.4 (2.1) | 0.718 |
| Time from injury to ACL reconstruction (wks) | 20.9 (18.7) | 12.0 (4.0) | 0.313 |
| Time from ACL reconstruction to radiographic testing (yrs) | 5.8 (0.9) | 5.6 (0.2) | 0.722 |
| Gait velocity (m/s) | 1.55 (0.15) | 1.48 (0.06) | 0.263 |
| Sex (M:F) | 11:3 | 2:3 | 0.262 |
| Pre-Injury Activity Level (1:2) | 8:6 | 1:4 | 0.303 |
| Graft type (Allo:Auto) | 10:4 | 3:2 | >0.999 |
| Involved lateral compartment OA at 5 years (No:Yes) | 2:12 | 1:4 | >0.999 |
| Uninvolved medial compartment OA at 5 years (No:Yes) | 1:13 | 2:3 | 0.155 |
Abbreviations: yrs, years; kg, kilogram; m, meter; wks, weeks; s, second; M, male; F, female; Allo, allograft; Auto, hamstring-gracilis autograft; OA, osteoathritis.
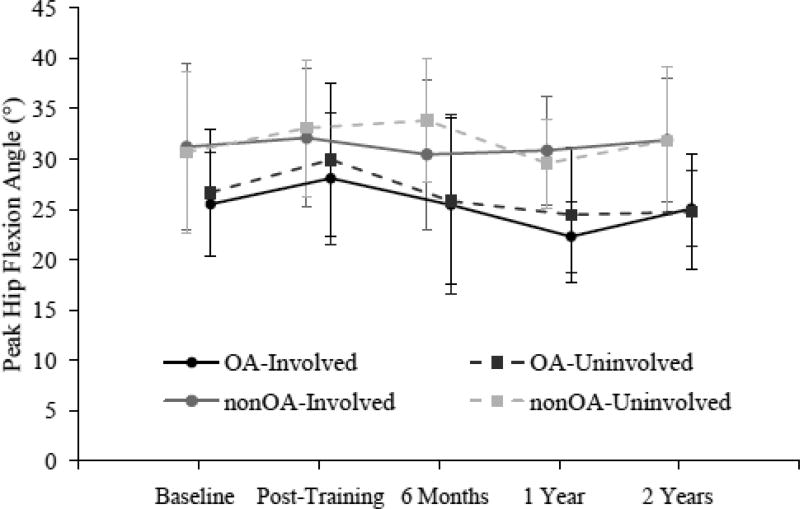
3.2 Hip Flexion Angle
A main effect of group was present for peak hip flexion angle in the involved limb as those who did develop knee OA at 5 years walked with a lower hip flexion angle across the 5 time points than those who did not develop knee OA (Mean across 5 time points: P: 0.043; no knee OA: 31.3° (SD: 1.4°); knee OA: 25.3° (SD: 2.4°); ES: 0.88) (Figure 3). A significant interaction effect existed between those who did and did not develop knee OA in the interlimb difference (involved limb minus uninvolved limb) of peak hip flexion angle (P: 0.038) with statistically significant group differences present only at 1 year (P: 0.040, no knee OA: 1.3° (SD: 0.8°); knee OA: −2.1° (SD: 1.3°)) (Figure 3). However, meaningful interlimb asymmetry exceeding the minimal detectable change of 3° only existed in patients who did not later develop knee OA at 6 months (Table 3).
Figure 3.
Mean value in peak hip flexion angle during stance phase of gait between those with and without radiographic medial compartment knee OA 5 years after ACL reconstruction. Whiskers represent ±1 standard deviation.
Table 3.
Involved limb and interlimb differences in sagittal and frontal plane hip kinematics and kinetics during stance phase of gait for those with and without knee OA 5 years after ACL reconstruction. Boldface numbers indicate statistically significant group differences.
| Group | Baseline | Post- Training |
6 Months |
1 Year | 2 Years | Interaction Effect |
Main Effect (Time) |
Main Effect (Group) |
|
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) |
Mean (SD) |
Mean (SD) |
Mean (SD) |
Mean (SD) |
P-value |
P- value |
P- value |
||
| Peak Hip Flexion Angle (°) | non OA | 31.2 (8.2) | 32.1 (6.9) | 30.5 (7.4) | 30.8 (5.4) | 31.9 (6.1) | 0.769 | 0.442 | 0.043 |
| OA | 25.5 (6.3) | 28.1 (7.6) | 25.5 (8.2) | 22.3 (6.7) | 25.1 (5.7) | ||||
| Interlimb Difference (°) | non OA | 0.5 (3.5) | 1.0 (2.4) | −3.4 (3.7) | 1.3 (2.7) | 0.0 (3.0) | 0.038 | 0.270 | 0.608 |
| OA | −1.2 (3.9) | 1.8 (3.8) | −0.4 (2.4) | −2.1 (3.7) | 0.3 (3.5) | ||||
| Peak Hip Extension Angle (°) | non OA | 19.2 (7.6) | 17.6 (6.2) | 17.3 (6.7) | 19.2 (6.5) | 15.4 (6.4) | 0.731 | 0.304 | 0.337 |
| OA | 21.1 (7.6) | 17.8 (6.2) | 19.8 (5.4) | 22.5 (6.3) | 20.4 (5.5) | ||||
| Interlimb Difference (°) | non OA | 0.4 (3.9) | 1.3 (4.3) | −1.1 (3.2) | −1.6 (3.4) | −2.7 (2.5) | 0.056 | 0.766 | 0.545 |
| OA | −1.6 (3.7) | 2.0 (3.5) | −1.7 (1.9) | 0.8 (3.7) | 1.5 (2.6) | ||||
| Hip Excursion Angle (°) | non OA | 50.4 (5.3) | 49.7 (5.7) | 47.6 (5.3) | 50.0 (4.5) | 47.3 (3.8) | 0.566 | 0.239 | 0.100 |
| OA | 46.6 (2.9) | 45.9 (5.0) | 45.2 (2.9) | 44.8 0.81) | 45.5 (2.5) | ||||
| Interlimb Difference (Nm/kg·m) | non OA | 1.0 (4.2) | 2.3 (5.1) | −4.5 (4.8) | −0.4 (4.8) | −2.6 (4.8) | 0.077 | 0.209 | 0.951 |
| OA | −2.8 (5.5) | 3.9 (5.4) | −2.1 (2.1) | −1.4 (1.5) | 1.8 (1.7) | ||||
| Peak Hip Adduction Angle (°) | non OA | 9.2 (4.2) | 9.4 (3.1) | 8.7 (3.1) | 7.9 (3.3) | 8.0 (3.4) | 0.545 | 0.063 | 0.928 |
| OA | 10.0 (4.0) | 9.4 (3.4) | 7.2 (2.3) | 7.1 (2.1) | 8.9 (3.2) | ||||
| Interlimb Difference (°) | non OA | 2.8 (5.4) | 3.6 (5.1) | 3.5 (4.4) | 2.4 (4.7) | 1.6 (4.9) | 0.463 | 0.635 | 0.289 |
| OA | 1.4 (5.9) | 1.4 (5.7) | −1.0 (3.9) | −0.5 (4.1) | 1.1 (4.0) | ||||
| Peak Hip Flexion Moment (Nm/kg·m) | non OA | 0.77 0.24) | 0.82 0.26) | 0.73 (0.24) | 0.70 (0.19) | 0.64 (0.16) | 0.977 | <0.001 | 0.414 |
| OA | 0.72 0.14) | 0.72 0.14) | 0.65 (0.16) | 0.62 (0.11) | 0.57 (0.09) | ||||
| Interlimb Difference (Nm/kg·m) | non OA | 0.02 0.12) | 0.01 0.13) | 0.02 (0.10) | 0.01 (0.10) | −0.01 (0.12) | 0.091 | 0.021 | 0.072 |
| OA | −0.05 0.21) | 0.06 0.14) | −0.01 (0.11) | 0.18 (0.08) | −0.13 (0.09) | ||||
| Peak Hip Extension Moment (Nm/kg·m) | non OA | 0.64 0.15) | 0.61 0.22) | 0.62 (0.17) | 0.69 (0.16) | 0.64 (0.11) | 0.946 | 0.919 | 0.131 |
| OA | 0.73 0.13) | 0.73 0.08) | 0.72 (0.13) | 0.73 (0.17) | 0.70 (0.12) | ||||
| Interlimb Difference (Nm/kg·m) | non OA | 0.00 0.10) | 0.02 0.09) | −0.01 (0.08) | 0.02 (0.09) | −0.03 (0.07) | 0.495 | 0.880 | 0.494 |
| OA | −0.01 (0.11) | 0.01 (0.10) | −0.02 (0.16) | 0.03 (0.10) | 0.04 (0.10) | ||||
| Peak Hip Adduction Moment (Nm/kg·m) | non OA | 0.58 (0.09) | 0.61 (0.16) | 0.56 (0.13) | 0.57 (0.12) | 0.61 (0.12) | 0.815 | 0.220 | 0.781 |
| OA | 0.56 (0.09) | 0.56 (0.05) | 0.56 (0.06) | 0.55 (0.07) | 0.63 (0.08) | ||||
| Interlimb Difference (Nm/kg·m) | non OA | 0.11 (0.13) | 0.07 (0.12) | 0.11 (0.10) | 0.06 (0.17) | 0.08 (0.15) | 0.555 | 0.786 | 0.042 |
| OA | −0.06 (0.21) | −0.08 (0.21) | −0.06 (0.13) | −0.03 (0.18) | 0.00 (0.10) |
Abbreviations: SD, standard deviation; N, newton; m, meter; kg, kilogram.
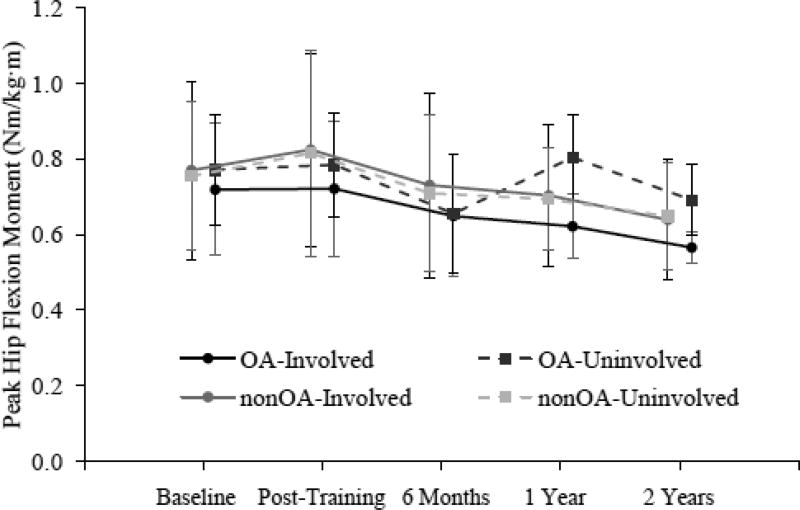
3.3 Hip Flexion Moment
A main effect of time was present in peak external hip flexion moment in the involved limb (P: <0.001) (Figure 4). The peak external hip flexion moment for all patients, independent of the presence of knee OA at 5 years, decreased over time from post-training to 2 years. The peak external hip flexion moment at 2 years (0.60 Nm/kg·m (SD: 0.15 Nm/kg·m)) was significantly lower than all previous testing time points (baseline: P: <0.001, 0.75 Nm/kg·m (SD: 0.21 Nm/kg·m); post-training: P: 0.002, 0.77 Nm/kg·m (SD: 0.23 Nm/kg·m); 6 months: P: 0.020, 0.69 Nm/kg·m (SD: 0.22 Nm/kg·m); 1 year: P: 0.017, 0.66 Nm/kg·m (SD: 0.17 Nm/kg·m)). A main effect of time also existed in the interlimb differences (involved limb minus uninvolved limb) of peak external hip flexion moment (P: 0.021) (Figure 4). The symmetrical external hip flexion moment demonstrated by all patients at 6 months (independent of the presence of knee OA at 5 years) (0.01 Nm/kg·m (SD: 0.10 Nm/kg·m)) was significantly different from the asymmetrical lower external hip flexion moment in the involved limb compared to uninvolved limb at 1 year (P: <0.001; −0.09 Nm/kg·m (SD: 0.13 Nm/kg·m)) and 2 years (P: 0.031; −0.07 Nm/kg·m (SD: 0.13 Nm/kg·m)). However, these asymmetries at 1 and 2 years were driven by the large asymmetries in patients who did later develop knee OA (1 year: −0.18 Nm/kg·m (SD: 0.08 Nm/kg·m); 2 years: −0.13 Nm/kg·m (SD: 0.09 Nm/kg·m)) and not by those who did not later develop knee OA (1 year: 0.01 Nm/kg·m (SD: 0.10 Nm/kg·m); 2 years: −0.01 Nm/kg·m (SD: 0.12 Nm/kg·m)).
Figure 4.
Mean value in peak hip flexion moment during stance phase of gait between those with and without radiographic medial compartment knee OA 5 years after ACL reconstruction. Whiskers represent ±1 standard deviation.
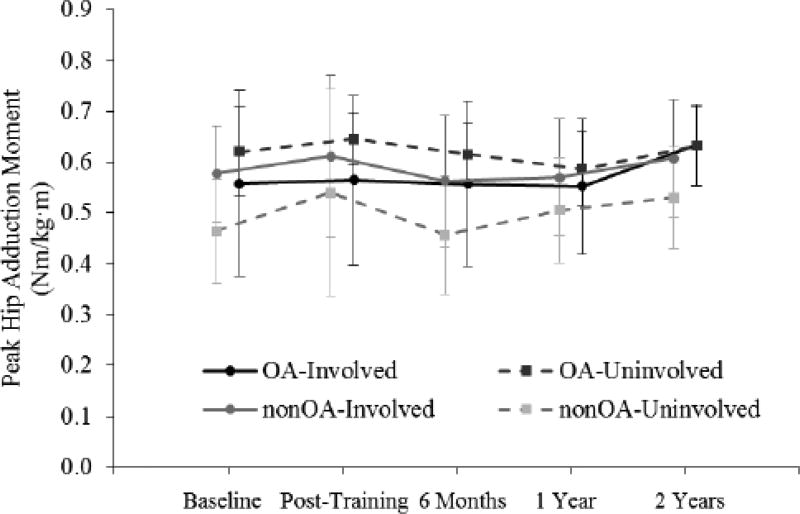
3.4 Hip Adduction Moment
Differences between those who did and did not develop knee OA at 5 years were also present in the frontal plane. A main effect of group existed in the interlimb difference for peak external hip adduction moment. Patients who did not develop later knee OA walked with an asymmetrically higher external hip adduction moment in the involved limb compared to the uninvolved limb across all 5 times points while patients who did develop later knee OA walked with an asymmetrically lower external adduction moment (Mean interlimb difference across 5 time points: P: 0.042; no knee OA: 0.09 Nm/kg·m (SD: 0.13 Nm/kg·m); knee OA: −0.05 Nm/kg·m (SD: 0.17 Nm/kg·m); ES: 0.95) (Figure 5). No further biomechanical differences in the hip existed between those who did and did not develop later knee OA (Table 3).
Figure 5.
Mean value in peak hip flexion moment during the first 50% of stance phase of gait between those with and without radiographic medial compartment knee OA 5 years after ACL reconstruction. Whiskers represent ±1 standard deviation.
4. DISCUSSION
4.1 Review of Findings
The purpose of this study was to determine if hip joint biomechanics early after ACL injury and reconstruction differ between patients with and without post-traumatic knee OA at 5 years after ACL reconstruction. Our findings indicate that patients who develop medial compartment knee OA within 5 years of ACL reconstruction walk with less involved hip flexion motion and asymmetrically lower peak external hip adduction moments both before and after surgery compared to their counterparts who did not develop knee OA at 5 years. In addition, and irrespective of the presence of knee OA at 5 years, all subjects demonstrated higher magnitudes of peak external hip flexion moment in the involved limb prior to ACL reconstruction that decreased over post-operative time points up to 2 years after surgery.
The presence of altered hip joint motion and loading after ACL injury is not surprising. Alterations in movement after ACL rupture are known to not only include changes in joint angles and moments in the knee but also proximally in the hip.19,22–27 Of greater interest is the finding that patients who developed radiographic OA in the ACL-injured knee within 5 years of reconstruction exhibited smaller joint angles and greater asymmetries in joint moments early after ACL injury and reconstruction than their counterparts who did not develop knee OA at 5 years. In our study, patients with medial compartment knee OA walked with lower peak hip flexion angles in both limbs. Patients who did develop later knee OA also walked with asymmetrically lower peak external hip adduction moments both prior to and 6 months after ACL reconstruction and asymmetrically lower peak external hip flexion moments at 1 and 2 years after surgery. In contrast, those who did not develop later knee OA walked with symmetric hip flexion moments and asymmetrically higher hip adduction moments in the involved compared to uninvolved limb across time points.
Biomechanical changes in proximal and distal joints within the kinetic chain exist presumably to compensate for altered knee joint motion after ACL injury.18 The decreasing peak external hip extension moment in the involved limb demonstrated by all patients from pre-operative time points up to 2 years after reconstruction is not surprising as moments in the knee increase over this same time period.5
The current analysis investigated differences in hip biomechanics between those with and without post-traumatic OA in the medial compartment of the knee. Hart et al. reported biomechanical hip findings of patients with lateral compartment knee OA 12 years after ACL reconstruction.17 Patients after ACL reconstruction had larger peak hip flexion angles compared to healthy control subjects, but no further kinematic or kinetic hip differences were found. The larger hip flexion angles reported by Hart and colleagues are in contrast to the smaller hip flexion angles exhibited by those with medial compartment knee OA in the current study. Several methodological differences between the two studies may explain this difference. The current study examined hip angles and moments within 2 years of ACL injury and reconstruction and used the contralateral limb and patients without radiographic OA for comparison. Hart et al. examined hip biomechanics 12 years after ACL reconstruction and referenced healthy controls for comparison; uninvolved limb measures were not reported. The findings of the two studies may also differ because lower extremity biomechanics influencing development of medial compartment knee OA may be different than those influencing lateral compartment OA.
4.2 Clinical Implications
Although early evidence suggests that lower joint loading after ACL injury may be a precursor to post-traumatic OA development in the knee,14 it is unknown if lower joint loading (i.e. asymmetrically lower external hip flexion and adduction moments in patients who did develop later knee OA in the current study) is detrimental or protective to the articular cartilage of the hip. A review of over 230,000 lower extremity total joint arthroplasties from the Australian Orthopaedic Association National Joint Replacement Registry and the Norwegian Arthroplasty Register found that contralateral non-cognate joints are at a higher risk for future end-stage OA than joints on the ipsilateral limb.39 Therefore, the possibility that the risk of contralateral hip OA could increase from asymmetrically higher joint moments in the contralateral hip of individuals who did develop later knee OA cannot be dismissed.
The current findings suggest that greater asymmetries in hip joint biomechanics exist both before and early after ACL reconstruction in patients who develop post-traumatic medial knee OA by 5 years after surgery compared to those who do not develop knee OA. Abnormal movement patterns at the hip represent a modifiable factor that may need to be addressed during rehabilitation already focused on improving movement patterns at the knee. However, because the hip joint may compensate for distal changes in the knee,22 the potential influence of restoring normal hip movement patterns on the knee joint must be considered. Further study is warranted to determine if ACL-injured patients at highest risk of post-traumatic knee OA are also subject to a greater risk of non-traumatic hip pathology, including OA development in either the ipsilateral or contralateral hip joint. If ACL injury does increase risk for chronic hip pathology, integration of secondary hip prevention strategies will be required by ACL rehabilitation protocols.
4.3 Limitations
The association between altered hip biomechanics and development of non-traumatic hip OA cannot be concluded from the current study. Diagnostic imaging of the hip joint was not completed 5 years after ACL reconstruction when radiographic knee testing was done. Further, although no subjects experienced additional hip joint pathology diagnosed by a physician or physical therapist during the time between ACL injury and 5 year testing, subjective reporting of hip symptoms that may represent underlying hip pathology was not completed. Diagnostic imaging of the patellofemoral joint was also not completed at 5 years, and analyses of those with lateral compartment knee OA was not completed in this study. Patients presenting with post-traumatic OA in these other knee compartments may also demonstrate unique alterations in hip biomechanics early after ACL injury. It is also acknowledged that multiple comparisons in hip biomechanics were made between those who did and did not develop later knee OA presenting risk for type I errors. However, group differences exceeded minimal detectable change values of biomechanical variables used in this study mitigating this risk.
5. CONCLUSIONS
Patients with medial knee OA 5 years after ACL reconstruction walked with smaller sagittal plane hip angles and lower sagittal and frontal plane hip moments in the ACL-injured limb before and after ACL reconstruction compared to those who did not develop knee OA at 5 years. The current findings suggest hip joint biomechanics may be altered in patients who develop post-traumatic knee OA. Further study is needed to confirm whether the risk of non-traumatic hip pathology is increased after anterior cruciate ligament injury and if hip joint biomechanics influence its development.
Highlights.
-
-
Post-traumatic osteoarthritis has been linked to early knee joint unloading
-
-
Later knee osteoarthritis found to relate to smaller hip joint angles and moments
-
-
Further study needed to determine if abnormal hip biomechanics lead to hip pathology
Acknowledgments
We would like to acknowledge Drs. Wendy Hurd, Erin Hartigan, and Stephanie Di Stasi for their assistance with data collection and the University of Delaware Physical Therapy Clinic for providing the physical therapy treatments for our research participants. We also thank Martha Callahan and the Delaware Rehabilitation Institute’s Clinical Research Core (http://www.udel.edu/dri/ResCore.html) for their assistance with patient recruitment, scheduling, and data management. This work was supported by the National Institute of Health (R01 AR048212, P30 GM103333).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chmielewski TL, Rudolph KS, Fitzgerald GK, Axe MJ, Snyder-Mackler L. Biomechanical evidence supporting a differential response to acute ACL injury. Clin Biomech (Bristol, Avon) 2001;16:586–591. doi: 10.1016/s0268-0033(01)00050-x. [DOI] [PubMed] [Google Scholar]
- 2.Gardinier ES, Manal K, Buchanan TS, Snyder-Mackler L. Gait and neuromuscular asymmetries after acute ACL rupture. Med Sci Sports Exerc. 2012;44(8):1490–1496. doi: 10.1249/MSS.0b013e31824d2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rudolph KS, Axe MJ, Buchanan TS, Scholz JP, Snyder-Mackler L. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9(2):62–71. doi: 10.1007/s001670000166. [DOI] [PubMed] [Google Scholar]
- 4.Rudolph KS, Eastlack ME, Axe MJ, Snyder-Mackler L. 1998 basmajian student award paper: Movement patterns after anterior cruciate ligament injury: A comparison of patients who compensate well for the injury and those who require operative stabilization. Journal of electromyography and kinesiology : official journal of the International Society of Electrophysiological Kinesiology. 1998;8:349–362. doi: 10.1016/s1050-6411(97)00042-4. [DOI] [PubMed] [Google Scholar]
- 5.Roewer BD, Di Stasi SL, Snyder-Mackler L. Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. J Biomech. 2011;44(10):1948–1953. doi: 10.1016/j.jbiomech.2011.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hooper DM, Morrissey MC, Drechsler WI, Clark NC, Coutts FJ, McAuliffe TB. Gait analysis 6 and 12 months after anterior cruciate ligament reconstruction surgery. Clin Orthop. 2002:168–178. doi: 10.1097/00003086-200210000-00025. [DOI] [PubMed] [Google Scholar]
- 7.Butler RJ, Minick KI, Ferber R, Underwood F. Gait mechanics after ACL reconstruction: Implications for the early onset of knee osteoarthritis. Br J Sports Med. 2009;43(5):366–370. doi: 10.1136/bjsm.2008.052522. [DOI] [PubMed] [Google Scholar]
- 8.Webster KE, Feller JA, Wittwer JE. Longitudinal changes in knee joint biomechanics during level walking following anterior cruciate ligament reconstruction surgery. Gait Posture. 2012;36:167–171. doi: 10.1016/j.gaitpost.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 9.Varma RK, Duffell LD, Nathwani D, McGregor AH. Knee moments of anterior cruciate ligament reconstructed and control participants during normal and inclined walking. BMJ Open. 2014;4(6):e004753-e004753. doi: 10.1136/bmjopen-2013-004753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zabala ME, Favre J, Scanlan SF, Donahue J, Andriacchi TP. Three-dimensional knee moments of ACL reconstructed and control subjects during gait, stair ascent, and stair descent. J Biomech. 2013;46:515–520. doi: 10.1016/j.jbiomech.2012.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Webster KE, McClelland JA, Palazzolo SE, Santamaria LJ, Feller JA. Gender differences in the knee adduction moment after anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2012;46:355–359. doi: 10.1136/bjsm.2010.080770. [DOI] [PubMed] [Google Scholar]
- 12.Patterson MR, Delahunt E, Caulfield B. Peak knee adduction moment during gait in anterior cruciate ligament reconstructed females. Clin Biomech. 2014;29:138–142. doi: 10.1016/j.clinbiomech.2013.11.021. [DOI] [PubMed] [Google Scholar]
- 13.Andriacchi TP, Mundermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32(3):447–457. doi: 10.1023/b:abme.0000017541.82498.37. [DOI] [PubMed] [Google Scholar]
- 14.Wellsandt E, Gardinier ES, Manal K, Axe MJ, Buchanan TS, Snyder-Mackler L. Decreased knee joint loading associated with early knee osteoarthritis after anterior cruciate ligament injury. Am J Sports Med. 2015;44(1):143–51. doi: 10.1177/0363546515608475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Culvenor AG, Schache AG, Vicenzino B, et al. Are knee biomechanics different in those with and without patellofemoral osteoarthritis after anterior cruciate ligament reconstruction? Arthritis Care Res (Hoboken) 2014;66(10):1566–1570. doi: 10.1002/acr.22313. [DOI] [PubMed] [Google Scholar]
- 16.Culvenor AG, Perraton L, Guermazi A, et al. Knee kinematics and kinetics are associated with early patellofemoral osteoarthritis following anterior cruciate ligament reconstruction. Osteoarthritis Cartilage. 2016;24(9):1548–1553. doi: 10.1016/j.joca.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 17.Hart HF, Collins NJ, Ackland DC, Cowan SM, Crossley KM. Gait characteristics of people with lateral knee OA after ACL reconstruction. Med Sci Sports Exerc. 2015(37):2406–2415. doi: 10.1249/MSS.0000000000000671. [DOI] [PubMed] [Google Scholar]
- 18.Hurd WJ, Snyder-Mackler L. Knee instability after acute ACL rupture affects movement patterns during the mid-stance phase of gait. J Orthop Res. 2007;25(10):1369–1377. doi: 10.1002/jor.20440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Di Stasi SL, Snyder-Mackler L. The effects of neuromuscular training on the gait patterns of ACL-deficient men and women. Clin Biomech (Bristol, Avon) 2012;27(4):360–365. doi: 10.1016/j.clinbiomech.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41:1310–8. doi: 10.1177/0363546513482718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferber R, Osternig LR, Woollacott MH, Wasielewski NJ, Lee JH. Gait mechanics in chronic ACL deficiency and subsequent repair. Clin Biomech. 2002;17(4):274–285. doi: 10.1016/s0268-0033(02)00016-5. [DOI] [PubMed] [Google Scholar]
- 23.Hall M, Stevermer CA, Gillette JC. Gait analysis post anterior cruciate ligament reconstruction: Knee osteoarthritis perspective. Gait Posture. 2012;36(1):56–60. doi: 10.1016/j.gaitpost.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Noehren B, Wilson H, Miller C, Lattermann C. Long-term gait deviations in anterior cruciate ligament-reconstructed females. Med Sci Sports Exerc. 2013;45(7):1340–1347. doi: 10.1249/MSS.0b013e318285c6b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alkjaer T, Simonsen EB, Jørgensen U, Dyhre-Poulsen P. Evaluation of the walking pattern in two types of patients with anterior cruciate ligament deficiency: Copers and non-copers. Eur J Appl Physiol. 2003;89(3–4):301–8. doi: 10.1007/s00421-002-0787-x. [DOI] [PubMed] [Google Scholar]
- 26.Torry MR, Decker MJ, Ellis HB, Shelburne KB, Sterett WI, Steadman JR. Mechanisms of compensating for anterior cruciate ligament deficiency during gait. Med Sci Sports Exerc. 2004;36(8):1403–1412. doi: 10.1249/01.mss.0000135797.09291.71. [DOI] [PubMed] [Google Scholar]
- 27.Di Stasi S, Hartigan EH, Snyder-Mackler L. Sex-specific gait adaptations prior to and up to 6 months after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2015;45(3):207–214. doi: 10.2519/jospt.2015.5062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40(3):141–154. doi: 10.2519/jospt.2010.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22(5):632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 30.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3–4):226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 31.Fitzgerald GK, Axe MJ, Snyder-Mackler L. A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2000;8(2):76–82. doi: 10.1007/s001670050190. [DOI] [PubMed] [Google Scholar]
- 32.Hurd WJ, Axe MJ, Snyder-Mackler L. A 10-year prospective trial of a patient management algorithm and screening examination for highly active individuals with anterior cruciate ligament injury: Part 1, outcomes. Am J Sports Med. 2008;36(1):40–47. doi: 10.1177/0363546507308190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Adams DL. Current concepts for anterior cruciate ligament reconstruction: A criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012 doi: 10.2519/jospt.2012.3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Di Stasi SL, Hartigan EH, Snyder-Mackler L. Unilateral stance strategies of athletes with ACL deficiency. Journal of Applied Biomechanics. 2012;28:374–386. doi: 10.1123/jab.28.4.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cohen J. Statistical power analysis for the behavioral sciences. 1988;2nd:567–567. doi: 10.1234/12345678. http://books.google.com/books?id=Tl0N2lRAO9oC&pgis=1. [DOI] [Google Scholar]
- 37.Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80(8):1132–1145. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 38.AOSSM. 2000 IKDC knee forms. The American Orthopaedic Society for Sports Medicine; http://www.sportsmed.org/tabs/research/downloads/IKDC2000-RevisedSubjectiveScoring.pdf. [Google Scholar]
- 39.Gillam MH, Lie SA, Salter A, et al. The progression of end-stage osteoarthritis: Analysis of data from the australian and norwegian joint replacement registries using a multi-state model. Osteoarthritis and Cartilage. 2013;21(3):405–412. doi: 10.1016/j.joca.2012.12.008. [DOI] [PubMed] [Google Scholar]