Abstract
The majority of oral pigmentations are benign lesions such as nevi, melanotic macules, melanoacanthomas or amalgam tattoos. Conversely, mucosal melanomas are rare but often lethal; therefore, excluding oral melanomas in this setting is crucial. Reflectance confocal microscopy is a non-invasive, in vivo imaging system with cellular resolution that has been used to distinguish benign from malignant pigmented lesions in the skin, and more recently in the mucosa. However, lesions located posteriorly in the oral cavity are difficult to assess visually and difficult to biopsy due to their location. Herein we present a patient with previous multiple melanomas presenting with an oral amalgam tattoo in the buccal mucosa, which was imaged using an intraoral telescopic probe attached to a commercially available handheld RCM. In this case report we describe this novel probe, the first RCM description of an amalgam tattoo and we discuss its differences with the findings described in oral melanomas.
Keywords: reflectance confocal microscopy, amalgam tattoo, melanoma, oral, mucosa
Introduction
The majority of oral pigmentations are benign lesions such as nevi, melanotic macules, melanoacanthomas or amalgam tattoos [1,2]. Conversely, mucosal melanomas are rare, but often lethal [2]. Reflectance confocal microscopy (RCM) allows imaging with cellular resolution and has excellent diagnostic accuracy to diagnose cutaneous melanoma [3]. However, RCM can be challenging to perform in the oropharynx using the current probes.
Herein we present a patient with previous multiple melanomas presenting with an oral amalgam tattoo in the buccal mucosa, which was imaged using a novel intraoral telescopic probe attached to a commercially available handheld RCM.
Case
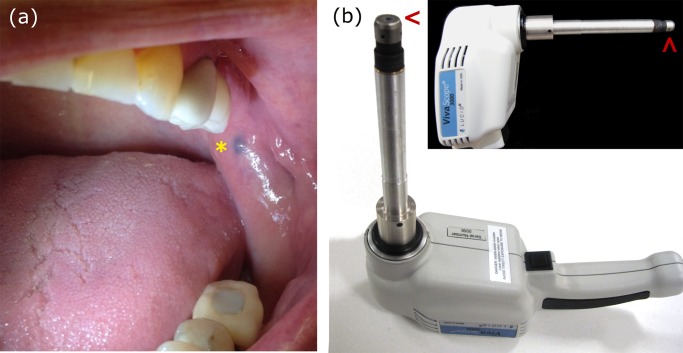
A woman in her 70s was referred by her dentist for a pigmented lesion on the oral mucosa. She had a history of four cutaneous melanomas —three in situ and one invasive (Breslow 0.25 mm)— excised four years prior. At physical examination, she presented with a 3 mm asymptomatic bluish papule on the left buccal mucosa (Figure 1a, asterisk). To evaluate this location, a handheld RCM (Vivascope3000, Caliber ID, Rochester, NY) fitted with a telescopic probe was used (Figure 1b). The probe was designed to be sufficiently small (12 mm) and long (~150 mm) to allow access inside the oral cavity [4]. The probe consists of a telescope and an objective lens of numerical aperture 0.7, providing a ~0.75 × 0.75 mm field of view, ~4 μm optical sectioning and ~1 μm lateral resolution, allowing imaging to a depth of ~300 μm. Enclosing the lens there is a cap with a coverslip, which provides contact to the mucosa and keeps the tissue gently flattened and still during the imaging procedure (Figure 1b, arrowheads). Two caps are used: a shorter cap allows for imaging in the deeper epithelium/mucosal-submucosal junction and a longer cap in the superficial lamina propria. We acquired images and videos that were converted into videomosaics [5].
Figure 1.
(a) Clinical image of pigmented lesion located on the left buccal mucosa (asterisk). Note the presence of a dental filling in the third left lower molar. (b) This lesion was imaged with a telescopic probe attached to a handheld reflectance confocal microscope. Attached to the probe is a small objective lens, which is enclosed in a small cap with a coverslip (arrowhead). The approach of using caps with different lengths allows for imaging at different depths in oral tissue. [Copyright: ©2017 Yélamos et al.]
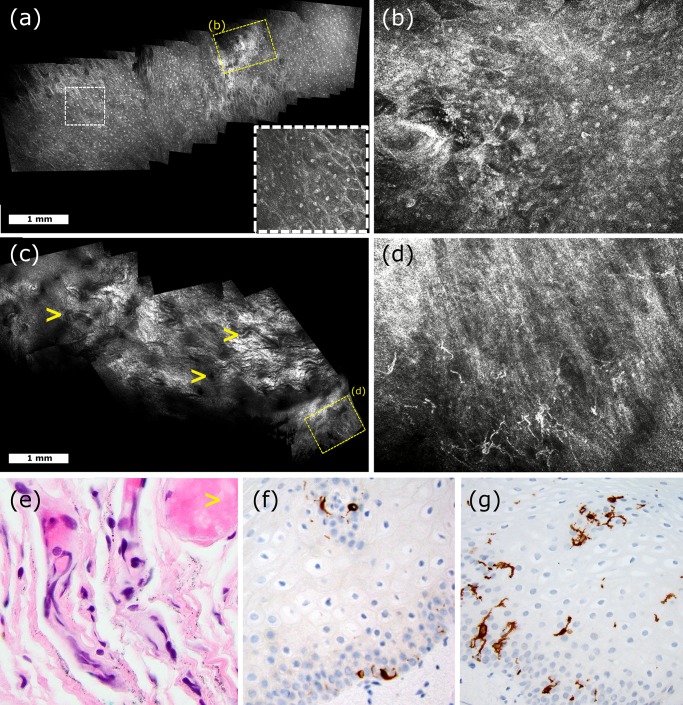
During imaging, the patient was awake and tolerated the procedure well. Superficially, RCM showed an overall normal epithelium with focal areas of epithelial disarray (Figure 2a, b). Deeper, we identified increased vascularity (Figure 2c) and numerous large dendritic cells admixed with plump cells and bright dots (Figure 2d). In light of her past medical history, the lesion was biopsied to exclude a primary or metastatic melanoma. Histopathologic analysis revealed fine black granular pigment within the dermis suggestive of an amalgam tattoo (Figure 2e).
Figure 2.
Reflectance confocal microscopy images (panels a – d) and its histopathologic correlates (panels e – f). Superficial confocal videomosaic showing normal epithelial cells with prominent nucleoli (panel a, white rectangle and inset), and a focal area of epithelial disarray (panel b). Confocal videomosaic obtained at the epithelial junction showing increased vascularity (arrowheads, panel c) and an area with numerous large atypical dendritic cells (panel d). Hematoxylin and eosin stain of the lesion showed fine black granular pigment within the stroma in the dermis (panel e, original magnification × 40). Immunohistochemical stain for A103 showed scattered melanocytes in the basal layer and in the epidermis (panel g, original magnification × 20). Immunohistochemical stain for CD1a highlighted numerous Langerhans cells throughout the epidermis (panel f, original magnification × 20). [Copyright: ©2017 Yélamos et al.]
Conclusions
In the last decade, RCM imaging has expanded its use beyond the skin and has been applied to the oral and genital mucosa, specifically to distinguish mucosal melanomas from benign lesions [1,6,7]. Indeed, RCM features suggesting mucosal melanomas include suprabasal dendritic or large round cells, dendritic cells in the epithelial-connective tissue junction, and epithelial disarray [1,6,7]. In our case, RCM showed numerous suprabasilar dendritic cells along with epithelial disarray. However, these findings occurred focally, and we also noted numerous bright dots and plump cells suggesting a reactive lymphohistiocytic infiltrate. To better characterize these findings, immunohistochemical stains for melanocytes and Langerhans cells were performed. These showed normal numbers of melanocytes within the basal and suprabasilar epithelium (Figure 2f) and numerous Langerhans cells extending into the upper epithelium (Figure 2g).
Langerhans cells are difficult to distinguish from melanocytes on RCM [8], and have a low specificity on the oral mucosa since they occur in normal mucosa and in reactive processes such as amalgam tattoos [1]. Histologically amalgam tattoos reveal small granules deposited between the collagen fibers and can present with a foreign-body reaction [2]. No previous studies have reported the RCM findings of amalgam tattoos. Although the presence of amalgam granules may not be visible with RCM since they are located deeper than 200–300 μm, the presence of bright dots (lymphocytes) and plump cells (macrophages), with suprabasal dendritic cells, is suggestive of a reactive process, such as an amalgam tattoo.
To conclude, we have presented the first case of amalgam tattoo imaged with RCM using a new telescopic probe. Although the presence of epidermal disarray and suprabasilar dendritic cells on RCM was suggestive of melanoma, the coexisting presence of bright dots and plump cells brings into consideration the differential diagnosis a reactive process such as an amalgam tattoo. However, since the RCM features of mucosal melanomas and other mucosal conditions are limited, larger studies are needed to increase the meaning of using this new probe with high-resolution images.
Acknowledgements
We would like to thank Dr. Marco Ardigò for his thoughtful feedback regarding this case.
Footnotes
Competing interests/Disclosures: Milind Rajadhyaksha is a former employee of and owns equity in Caliber Imaging and Diagnostics (formerly Lucid Inc.), the company that manufactures and sells the Vivascope confocal microscope. The Vivascope is the commercial version of an original laboratory prototype that he had developed at Massachusetts General Hospital, Harvard Medical School. The other authors have no disclosures or conflicts of interest to report.
All authors have contributed significantly to this publication.
Funding: This research was funded in part by NIH/NCI grant R01CA156773, NIH/NCI grant R01CA199673, NIH/NIBIB grant R01EB020029, the NIH/NCI Cancer Center Support Grant P30 CA008748 and the Beca Excelencia Fundación Piel Sana.
References
- 1.Maher NG, Solinas A, Scolyer RA, Guitera P. In vivo reflectance confocal microscopy for evaluating melanoma of the lip and its differential diagnoses. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;123(1):84–94. doi: 10.1016/j.oooo.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 2.Lundin K, Schmidt G, Bonde C. Amalgam tattoo mimicking mucosal melanoma: a diagnostic dilemma revisited. Case Rep Dent. 2013;2013:787294. doi: 10.1155/2013/787294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pellacani G, Guitera P, Longo C, Avramidis M, Seidenari S, Menzies S. The impact of in vivo reflectance confocal microscopy for the diagnostic accuracy of melanoma and equivocal melanocytic lesions. J Invest Dermatol. 2007;127(12):2759–2765. doi: 10.1038/sj.jid.5700993. [DOI] [PubMed] [Google Scholar]
- 4.Peterson G, Zanoni DK, Migliacci J, Cordova M, Rajadhyaksha M, Patel S. Progress in reflectance confocal microscopy for imaging oral tissues in vivo. Proceedings of SPIE Photonics West. 2016:9689. [Google Scholar]
- 5.Kose K, Cordova M, Duffy M, Flores ES, Brooks DH, Rajadhyaksha M. Video-mosaicing of reflectance confocal images for examination of extended areas of skin in vivo. Br J Dermatol. 2014;171(5):1239–1241. doi: 10.1111/bjd.13050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Debarbieux S, Perrot JL, Erfan N, et al. Reflectance confocal microscopy of mucosal pigmented macules: a review of 56 cases including 10 macular melanomas. Br J Dermatol. 2014;170(6):1276–1284. doi: 10.1111/bjd.12803. [DOI] [PubMed] [Google Scholar]
- 7.Uribe P, Collgros H, Scolyer RA, Menzies SW, Guitera P. In vivo reflectance confocal microscopy for the diagnosis of melanoma and melanotic macules of the lip. JAMA Dermatol. 2017 doi: 10.1001/jamadermatol.2017.0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hashemi P, Pulitzer MP, Scope A, Kovalyshyn I, Halpern AC, Marghoob AA. Langerhans cells and melanocytes share similar morphologic features under in vivo reflectance confocal microscopy: a challenge for melanoma diagnosis. J Am Acad Dermatol. 2012;66(3):452–462. doi: 10.1016/j.jaad.2011.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]