Abstract
The present study tested the role of FKBP5 binding protein 5 (FKBP5) genetic variation in an internalizing pathway from child maltreatment to emerging adult problem drinking among a sample of African-American youth (N = 280) followed prospectively from ages 11 to 20. Specifically, whether childhood internalizing symptoms and emerging adult tension reduction alcohol expectancies sequentially mediate the effect of child maltreatment on emerging adult problem drinking and whether FKBP5 moderates these associations were investigated. Results indicate that individuals with at least one copy of the FKBP5 CATT haplotype (minor alleles) are more vulnerable to traversing the hypothesized internalizing pathway of risk than individuals without this genotypic profile. Taken together our findings 1) highlight the importance of FKBP5 genetic variation in the context of early adversity; 2) support the role of two prospective sequential mechanisms of an internalizing pathway to problematic drinking, namely childhood internalizing symptoms and emerging adult tension reduction alcohol expectancies; 3) identify a subgroup of maltreated children most susceptible to progressing along this less common pathway of risk.
Keywords: child maltreatment, problem drinking, FKBP5 binding protein 5, alcohol expectancies, internalizing pathway
Child maltreatment is considered among the most severe childhood adversities and is marked by serious disturbances in the caregiving environment (Cicchetti & Lynch, 1995; Cicchetti & Toth, 2016). Children who experience maltreatment are at heightened risk for a number of negative psychological and biological consequences not only in childhood, but throughout the life course (Cicchetti & Toth, 2015; Masten & Cicchetti, 2010). Among the myriad negative developmental sequelae, child maltreatment has been associated with emotion dysregulation, difficult peer relations, neuroendocrine dysfunction, internalizing and externalizing symptomatology, and disrupted parent-child relationships (see Cicchetti & Toth, 2016 for review). Additionally, child maltreatment increases risk for the development of substance use problems (e.g., Buckingham & Daniolos, 2013; Dube, Felitti, Dong, Chapman, Giles, & Anda, 2003; Hamburger, Leeb, & Swahn, 2008; Huang, Trapido, Fleming, Arheart, Crandall, et al., 2011; Rogosch, Oshri, & Cicchetti, 2010; Shin, Hong, & Hazen, 2010; Tonmyr, Thornton, Draca, & Wekerle, 2010; Wilsnack, Vogeltanz, Klassen, & Harris, 1997). For instance, over and above other forms of childhood adversities (e.g., parental death, parental incarceration, parental divorce), child maltreatment uniquely predicted persistent alcohol dependence in adulthood (Elliot, Stohl, Wall, Keyes, Goodwin, Skodol, et al., 2014). Moreover, adult men with a maltreatment history were found to be 1.74 times as likely to meet criteria for an alcohol disorder compared to men without child maltreatment experience. Elucidating why maltreated children may develop problematic substance use, and which maltreated children may be at greatest risk are important for advancing our understanding of the consequences of child maltreatment and the etiology of substance use disorders, as well as for designing effective preventive interventions for children and families.
Within the broader literature on the development of substance use disorders (SUDs), there is robust support for an externalizing or antisocial pathway (Chassin, Hussong, & Beltran, 2009; Chassin, Sher, Hussong, & Curran, 2013; Sher, 1991; Zucker, Heitzeg & Nigg, 2011; Zucker 2006). This pathway to problematic substance use is theorized to begin in infancy with a difficult temperament, and is marked by aggressive and rule-breaking behaviors in childhood, a behaviorally disinhibited or undercontrolled temperamental style, affiliation with deviant and substance using peers, maladaptive parenting practices and an early onset of substance use (Chassin, Hussong, & Beltran, 2009; Chassin, Sher, Hussong, & Curran, 2013; Costello, 2007; Sher, 1991; Zucker, Heitzeg, & Nigg, 2011). Given the vast empirical support for this pathway, it has been described as the “dominant pathway of risk for SUDs” (Hussong, Jones, Stein, Baucom, & Boeding, 2011).
Consistent with this assertion is growing evidence for an externalizing pathway by which maltreated children are at risk for the development of substance use disorders (Handley, Rogosch, & Cicchetti, 2015; Jones, Lewis, Litrownik, Thompson, Proctor, Isbell et al., 2013; Mezquita, Ibanez, Moya, Villa, & Ortet, 2014; Oshri, Rogosch, Burnette, & Cicchetti, 2011; Rogosch et al., 2010). For instance, Oshri and colleagues (2011) demonstrated that maltreated children were more likely to display a behaviorally undercontrolled temperament style in childhood, which in turn predicted a higher level of externalizing behaviors during pre-adolescence, which resulted in more marijuana abuse and dependence symptoms in adolescence. Similarly, Mezquita and colleagues (2014) found that childhood physical abuse was associated with young adult disinhibition which was related to antisocial behavior which prospectively predicted later problem drinking. Therefore, there is accumulating evidence, consistent with the broader developmental psychopathology literature, for an externalizing pathway of risk from child maltreatment to SUDs that is marked by a snowballing of risk including disinhibition, the development of externalizing behaviors, and the further development of problem substance use.
A lesser researched pathway to the development of SUDs is the internalizing pathway which is characterized by stress and negative affect regulation. Individuals traversing this pathway may use substances as a method of coping or self-medication. As with the externalizing pathway, the internalizing pathway to SUDs is best understood with a developmental lens (Zucker, 2006). Individuals who traverse an internalizing pathway may exhibit an inhibited temperament in infancy and internalizing symptoms throughout childhood, adolescence, and beyond. Additionally, throughout late childhood and adolescence, individuals following this risk pathway may develop positive beliefs about the effects of substances. These beliefs, often termed substance use expectancies, may include beliefs that substance use can reduce tension and negative affect. Once individuals initiate substance use, their personal experiences with the effects of substances function to shape their motivations for using (see Cooper, Kuntsche, Levitt, Barber & Wolf, 2016 for review). Individuals on an internalizing trajectory may develop strong coping motives, or motivations to use substances to cope with distress (Hussong et al., 2011; Sher, 1991). It is important to emphasize that the externalizing and internalizing pathways to problematic substance use are not mutually exclusive, and there are individuals for whom elements of both pathways may, at least at certain periods throughout development, contribute to SUDs (Hussong et al., 2011). Given the dominance of the externalizing pathway, to properly isolate the unique effects of the internalizing pathway, it is critical to control for externalizing symptoms.
Although there is some evidence within the broader developmental psychopathology literature for an internalizing pathway to SUD, results are decidedly mixed, especially among studies which controlled for co-occurring externalizing symptoms (Hussong, Ennett, Cox, & Haroon, 2017; Leve, Harold, Van Ryzin, Elam, & Chamberlain, 2012; McCarty, Wymbs, King, Mason, Vander Stoep, McCauley, & Baer, 2012; O’Neil, Conner, & Kendall, 2011; Pesola, Shelton, Munafo, Hickman, Maughan, van den Bree, 2015). For example, Menary, Corwin, and Chassin (2017) showed that, controlling for adolescent externalizing symptoms, greater internalizing symptoms during adolescence predicted an earlier age of first drink and a faster transition from first drink to first alcohol dependence symptom. Moreover, Pesola and colleagues (2015) found that depressive symptoms during adolescence were predictive of problematic drinking in emerging adulthood, over and above adolescent conduct problems. However, a number of studies have failed to find evidence for an association between internalizing symptoms during adolescence and later substance use (Chassin, Pitts, DeLucia, & Todd, 1999; King & Chassin, 2008), and some have demonstrated a protective effect of internalizing symptoms, particularly anxiety and social withdrawal (Edwards, Latendresse, Heron, Bin Cho, Hickman, Lewis, Dick, & Kendler, 2014; Rogosch et al., 2010). Hussong and colleagues (2017) asserted that inconsistencies across studies may be due to variations in the developmental timing of the associations, the particular measure or type of internalizing symptom, and the specific substance type (e.g., alcohol versus marijuana use).
Within the child maltreatment literature specifically there is also some emerging support for an internalizing pathway that explains, at least in part, why maltreated children are at-risk for SUDs. For example, in a cross-sectional study, retrospectively reported childhood sexual abuse among girls was associated with adolescent problem drinking by way of increased anxiety, but not depressive, symptoms (Hudson, Wekerle, Goldstein, Ellenbogen, Waechter, Thompson, & Stewart, 2017). Moreover, Mezquita and colleagues (2014) found that childhood emotional abuse was associated with higher levels of young adult negative emotionality, which was associated with alcohol coping motives, which prospectively predicted alcohol-related problems. Similarly, Lewis et al., (2011) showed that adolescent internalizing symptoms at age 14 mediated the effect of child maltreatment prior to age 12 on age 16 smoking. Mirroring the broader developmental psychopathology literature, support for the internalizing pathway from child maltreatment to substance use problems has not been consistent. For instance, Jones and colleagues (2013) did not find evidence for an indirect effect of childhood sexual abuse on adolescent drinking via internalizing symptoms. Moreover, although Rogosch, Oshri, and Cicchetti (2010) found that child maltreatment predicted increased internalizing symptoms in childhood, with continuity throughout early adolescence, higher levels of internalizing symptoms at age 13–15 predicted fewer marijuana disorder symptoms. Differences among the types of substances and specific internalizing symptoms measured by prior studies may contribute to these disparate findings.
As described above, the internalizing pathway is theorized to include tension reduction substance use expectancies and coping motivations for using alcohol and drugs (e.g., Hussong et al 2011; Sher, 1991). There is emerging evidence to suggest that these cognitive components of the risk trajectory may partially explain the developmental progression from child maltreatment to problem substance use. For example, Jester, Steinberg, Heitzeg, and Zucker (2015) demonstrated that childhood exposure to interparental violence predicted distress in early adolescence which was associated with stronger expectances of alcohol use for coping which then predicted problem drinking in emerging adulthood. A similar pattern of results, albeit later in development and with a different form of child maltreatment, was found by Grayson and Nolan-Hoeksema (2005) who showed that among adult women, retrospectively reported childhood sexual assault was related to adult distress, which was associated with stronger motivations to drink to cope, which were related to alcohol problems. Finally, Goldstein, Flett, and Wekerle (2010) also found evidence for the role of drinking motives in this pathway. Specifically, among college students, the effect of retrospectively reported child maltreatment on current alcohol-related consequences was mediated by coping-depression motives for drinking for women and motives related to enhancing positive mood for men.
Therefore, there is increasing evidence for an internalizing pathway from child maltreatment to problem substance use which may be mediated by negative affect or internalizing symptoms and beliefs about substance use for stress regulation. However, this emerging literature is marked by a number of limitations such as retrospective reporting of child maltreatment or an exclusive focus on a single type of maltreatment (i.e. sexual abuse), cross-sectional methodology, and the lack of the appropriate statistical control of the robust externalizing pathway. Moreover, not all children who experience maltreatment develop problems with substance use. The moderating role of individual factors such as genotypic variation has yet to be adequately investigated within these pathways. It is critical to understand not only why maltreated children may be at risk for substance use problems, but also to elucidate which maltreated children may be especially vulnerable.
FKBP5
The FKBP5 binding protein (FKBP5) gene is associated with the stress-response system and therefore has been studied in association with a number of adversities and the development of various forms of psychopathology. FKBP5 is responsive to stress exposure, induced by cortisol, and is an important modulator of the glucocorticoid receptor (GR) activity. More specifically, it is involved in an intracellular, ultra-short negative feedback loop that regulates GR sensitivity. This negative feedback loop is marked by the rapid induction of FKBP5 in response to GR activation and the inhibitory effect of FKBP5 on GR activity and is critical for recovery from stress exposure (Binder, 2009; Galat, 2013; Zannas & Binder, 2014).
FKBP5 is located on chromosome 6 (chromosome 6p21.31) and contains a number of single nucleotide polymorphisms (SNPs) that are implicated in the differential ability of FKBP5 to be induced by cortisol and to bind to the GR (see Zannas & Binder, 2014 for review). Variants of SNPs spanning the 103 kb of the FKBP5 gene have been linked with functional differences at the GR (e.g., rs3800373, rs9296158, rs1360780, and rs9470080), that during exposure to stress result in prolonged cortisol responses. Minor alleles are associated with greater expression of FKBP5 and increased binding at the GR. Major alleles, on the other hand, are associated with weaker induction of cortisol (Binder et al., 2004; Binder, 2009; Zannas & Binder, 2014).
A number of studies have demonstrated that variation in FKBP5 SNPs or haplotypes interacts with childhood adversity resulting in various negative outcomes including limbic system irritability (Dackis, Rogosch, Oshri, & Cicchetti, 2012), poor working memory (Lovallo, Enoch, Acheson, Cohoon, Sorocco, Hodgkinson, Vincent, & Goldman, 2016), heightened amygdala reactivity (White, Bogdan, Fisher, Munoz, Williamson, & Hariri, 2012), depression (Appel, Schwahn, Mahler, Schulz, Spitzer, Fenske, et al., 2011; Zimmerman, Bruckl, Nocon, Pfister, Binder, Uhr, et al., 2011) suicide attempts (Roy, Gorodetsky, Yuan, Goldman, & Enoch, 2010; Roy, Hodgkinson, DeLuca, Goldman, & Enoch, 2012), post-traumatic stress disorder and dissociative symptoms (Xie, Kranzler, Poling, Stein, Anton, Farrer, Gelernter, 2010; Yaylaci, Cicchetti, Rogosch, & Bulut, 2016) and aggressive and violent behaviors (Bevilacqua, Carli, Sarchiapone, George, Goldman, Dory, & Enoch, 2012). The majority of these prior studies point to minor alleles or minor haplotypes as interacting with environmental adversity to confer risk; however, a few have found interactive risk from the major alleles or haplotypes (e.g., Roy et al., 2010; Roy et al., 2012; Yaylaci et al., 2016). Importantly, prior research on FKBP5 and interaction with stress and adversity exposure points to the importance of careful consideration of the developmental timing of the adversity. Specifically, in their review, Zannas and Binder (2014) concluded that FKBP5 by adversity interactions are robust for childhood traumatic experiences, but not for adult traumas.
Recently, researchers have begun to examine the role of FKBP5 genotypic variation in the development of problematic substance use. Specifically, Huang and colleagues (2014) found FKBP5 genotype and haplotype variation affected the severity of alcohol withdrawal symptoms among adults with alcohol use disorder. Moreover, among a sample of college students, Lieberman and colleagues (2016) demonstrated that FKBP5 interacted with retrospectively reported early life trauma, but not adult trauma or stress, to predict current heavy drinking. Nylander and colleagues (2016) also tested the effect of FKBP5 by environmental adversity on problem drinking behavior among young adults. Participants retrospectively reported on their childhood relationship with their parents. Results indicated that the effect of a poor parent-child relationship on young adult problem drinking depended on FKBP5 variation. These studies provide promising evidence that FKBP5 interacts with early adversity to affect problem drinking. They are limited however by the reliance on retrospective reports of varying forms of adversity and the lack of investigation of underlying mechanisms.
Among a sample of children with substantiated child maltreatment documented through Child Protective Services (CPS) records, and demographically matched comparisons, Handley, Rogosch, and Cicchetti (2015) found evidence for moderated mediation such that child externalizing behavior mediated the effect of child maltreatment on adolescent marijuana dependence symptoms only for individuals with the FKBP5 CATT haplotype (minor alleles). The authors did not find evidence for FKBP5 moderation of an internalizing pathway to adolescent marijuana dependence however. To our knowledge, this study provided the first evidence of genetically moderated mediation of the externalizing pathway to SUDs among maltreated children. Although prior studies lay critical groundwork toward the understanding of not only why maltreated children are at risk for SUDs, but also which maltreated children may be at greatest risk, many questions remain unanswered.
Current study
The aim of the present study was to investigate an internalizing pathway from child maltreatment to emerging adult problem drinking, and to determine whether FKBP5 genotypic variation moderates the pathway. Specifically, we sought to prospectively test whether child maltreatment may progress to problematic alcohol use in emerging adulthood by way of internalizing symptoms in childhood and tension-reducing alcohol expectancies in emerging adulthood. To examine the uniqueness of this pathway, over and above the robust externalizing pathway, we included childhood externalizing symptoms in our developmental model. We selected emerging adulthood as a developmental period for investigation of problem alcohol use given that this time period is marked by peak levels of heavy drinking and alcohol dependence (Chassin et al., 2013; Jackson & Sartor, 2016; Sher, Grekin, & Williams, 2005). We hypothesized that children who experienced maltreatment would evidence increased internalizing symptoms during childhood which would affect stronger beliefs about the tension reduction benefits of drinking during emerging adulthood, which would be related to more problematic drinking behavior. We further hypothesized that youth with at least 1 copy of the FKBP5 CATT haplotype (minor alleles) would be at increased risk to traverse this internalizing pathway.
Method
Participants
Participants (N=280) were from a longitudinal follow-up study of emerging adults who participated in a research summer camp program as children. The original study (wave 1) included 680 low-income maltreated (n=360) and nonmaltreated (n=320) children aged 10 to 12 (M=11.28, SD= .97). The original sample was racially and ethnically diverse (71.6% African-American, 11.8% Caucasian, 12.6% Hispanic, 4.0% biracial/other race) and evenly distributed by gender (50.1% male). The majority of children were from single parent families (68.7%) with a history of receiving public assistance (96.1%).
Participants for the present investigation consisted of 280 of the original study participants. Of the original 680 participants assessed in childhood, 420 completed the wave 2 emerging adult assessment. Of these, only the African-American participants were included in this current study (N=280). This was done because genetic variation can differ across ancestral groups, making interpretation of gene by environment interactions more difficult. At wave 2, emerging adults were on average 20.16 years old (SD=1.37), 46.8% male, 58.2% with a history of childhood maltreatment.
Analyses (chi-square and t-tests) were conducted comparing the 280 included African-American youth in the present study to the 207 excluded African-American participants on demographic variables and wave 1 study variables. There were no differences between included and excluded participants on child maltreatment status, family income, maternal marital status at wave 1, child gender, and age at wave 1. Moreover, there were no differences between included and excluded participants on self-report of childhood physiological anxiety, depressive symptoms, worry/oversensitivity, or conduct problems.
Informed consent was obtained from parents of maltreated and nonmaltreated children for their child’s participation in the summer camp program and for examination of any Department of Human Services (DHS) records pertaining to the family. Children in the maltreated group were recruited through a DHS liaison who examined Child Protective Services reports to identify children who had been maltreated and/or were part of a family with a history of maltreatment. Children living in foster care often experience early and extreme maltreatment. They were not recruited for the current investigation to reduce heterogeneity among the maltreated sample. The DHS liaison contacted eligible families and explained the study. Parents who were interested in having their child participate provided signed permission for their contact information to be shared with project staff. These families were representative of those receiving services through DHS. Comprehensive reviews of all DHS records for each family were conducted. Maltreatment information was coded by trained research staff and a clinical psychologist, using the Barnett, Manly, and Cicchetti (1993) nosological system for classifying child maltreatment. Coding is based on all available information and does not rely on DHS determinations.
Because maltreating families primarily have low socioeconomic status (National Incidence Study – NIS-4; Sedlak et al., 2010), nonmaltreating families were recruited from those receiving Temporary Assistance to Needy Families (TANF) in order to ensure socioeconomic comparability between maltreated and nonmaltreated families. A DHS liaison contacted eligible nonmaltreating families and described the project. Parents who were interested in participating signed a release allowing their contact information to be given to project staff for recruitment. The families were recruited as nonmaltreated families after comprehensive DHS record searches confirmed the absence of any documented child maltreatment. Families who received preventative DHS services due to concerns over risk for maltreatment were not included within the nonmaltreated comparison group. Mothers of children recruited for both the maltreatment and nonmaltreatment groups were interviewed by trained research assistants using the Maternal Child Maltreatment Interview (Cicchetti, Toth & Manly, 2003). This was used to further verify a lack of DHS involvement among the children recruited for the nonmaltreatment group. Moreover, for the nonmaltreatment group, records were reviewed in the year following camp participation to assure that all information had been assessed. Maltreated and nonmaltreated children included in the present study were compared on a number of demographic characteristics. Groups did not differ in terms of maternal marital status, maternal age, child age, and child gender.
A range of strategies were used to relocate and recruit participants at wave 2. Records of last known addresses, extensive public internet searches (e.g., LexisNexis), contact information from medical records and neighborhood canvasing were part of a comprehensive recruitment design. Additionally, the DHS liaison was again utilized to locate participants through access to DHS records. The living situation of participants was varied and the developmental timing (i.e., 18–20 years of age) created unique challenges within this sample. Many participants were in a transitory period, either living with their families of origin or just beginning to live independently, which resulted in fewer participants registering in public databases.
Procedures
At wave 1, children attended a weeklong day camp from 9:00 a.m. to 4:00 p.m. and participated in both traditional camp activities and research assessments (for detailed descriptions of camp procedures see Cicchetti & Manly, 1990). At camp, children were assigned to groups of eight (four maltreated and four nonmaltreated children) same-age and same-sex peers. Each group was led by three trained camp counselors who were unaware of the maltreatment status of the children and the hypotheses of the study. The intensive staff to child ratio allowed for counselors to closely interact with children. During the 35 hours of interaction throughout the camp week, counselors got to know children well. In addition to recreational activities, after providing assent, children participated in research assessments. Trained research assistants conducted these individual research sessions in which questionnaires and other research measures were administered.
At wave 2, emerging adult participants were individually interviewed in private interview rooms by trained research assistants who were unaware of the participant’s maltreatment group status and the research hypotheses. The participants completed a variety of assessments including self-report measures and a diagnostic clinical interview.
Measures
Childhood conduct problems
Childhood conduct problems were assessed using the Pittsburgh Youth Survey (PYS; Loeber, Farrington, Stouthamer-Loeber, & Van Kammen, 1998). The PYS is a self-report measure that examines a range of delinquent behaviors and substance use in childhood. Reporters indicate both the lifetime prevalence of behaviors, as well as the occurrence in the past six months. A total of the 25 conduct disorder symptoms (e.g., stealing, cheating on school tests, damaging property) endorsed in the past 6 months, excluding the 6 substance use items, was used to determine childhood conduct problems. The mean number of symptoms endorsed was 2.21 (SD=2.80). Reliability was adequate for the 25 items (α = .83).
Childhood internalizing symptoms
Child depressive symptoms were measured using child self-report of the Child Depression Inventory (CDI; Kovacs, 1982; 2004). The CDI is 27 item questionnaire measure of depressive symptoms designed for school-age children. Children were asked to select the response option that best describes them within the past two weeks. The CDI is a well-established measure of child depressive symptoms with good psychometric properties (Kovacs, 2004). A summary score of the 27 items was calculated to index self-reported depressive symptoms. Participants in this study reported a mean of 8.01 (SD = 6.76). A total score greater than, or equal to 19 is indicative of clinical level depressive symptoms (Kovacs, 2004). In the current sample, 8.6% of children met this threshold for clinically elevated depressive symptoms.
Child physiological anxiety and child worry/oversensitivity were assessed by child self-report on the Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds & Richmond, 1997). The RCMAS asks children to respond “yes” or “no” to a total of 37 items. The RCMAS is a well-validated measure (Muris, Merckelbach, Ollendick, King, & Bogie, 2002) with good psychometric properties (Reynolds & Richmond, 1997). Scaled scores are calculated based on gender and age. The physiological anxiety subscale includes 10 items such as “Often I feel sick in my stomach,” “Often I have trouble catching my breath,” and “I have bad dreams.” The mean physiological anxiety scaled score in this study was 8.98 (SD=3.03). The worry/oversensitivity subscale is comprised of 11 items including “I am nervous,” “I worry when I go to bed at night,” “I worry about what is going to happen.” Children reported a mean worry/oversensitivity scaled score of 8.46 (SD=3.07).
As described in detail below, the above three indicators of child internalizing symptomatology (i.e., depressive symptoms, physiological anxiety, and worry/oversensitivity) were subsequently modeled as indicators of a child internalizing latent factor.
Emerging adult alcohol expectancies
At wave 2, emerging adult participants self-reported their alcohol expectancies using the Mann and colleagues’ (1987) adaptation of the Alcohol Expectancies Questionnaire (Christiansen et al., 1982). Response options ranged from 1 (Strongly Disagree) to 5 (Strongly Agree). The three items from the tension reduction subscale were used for the present study. Items included “Drinking alcohol helps me when I’m tense and nervous,” “Drinking alcohol relaxes me,” and “Drinking alcohol helps me forget my worries.” A mean score was calculated such that higher scores indicated stronger tension reduction alcohol expectancies. The mean score for this sample was 3.43 (SD = 1.10). There was adequate reliability among the items in this study (α=.78).
Emerging adult problem drinking
Problem drinking in emerging adulthood (wave 2) was assessed using 4 alcohol consumption items. Two items asked participants to self-report their quantity and frequency of consumption of hard liquor in the past year. These items were multiplied to index the consumption of hard liquor in the past year. Because this consumption variable was non-normality distributed, and given that modeling techniques are sensitive to non-normality, a square root transformation was used to reduce skewness and kurtosis. Participants also self-reported the frequency of their binge drinking of beer, wine, wine coolers, or hard liquor within the past year (defined as 3 or more drinks for women and 5 or more drinks for men) and the frequency of getting drunk on alcohol (not just lightheaded) within the past year. As described in detail below, these three variables (i.e., consumption of hard liquor, binge drinking, and drunkenness) were modeled as indicators of an emerging adult problem drinking latent construct in subsequent analyses. In this sample, 68.6% of emerging adult participants indicated drinking alcohol in the past year.
DNA collection, extraction, and genotyping
Using an established protocol, trained research assistants obtained DNA samples from children by collecting buccal cells with the Epicentre Catch-All Collection Swabs. Subsequently, using the conventional method, DNA was extracted with the Epicentre BuccalAmp DNA Extraction Kit, in order to prepare DNA for PCR amplification. Genotyping was conducted following previously published protocols. DNA was whole-genome amplified using the Repli-g kit (Qiagen, Chatsworth, CA, Catalog No. 150043) per the kit instructions to ensure the availability of data over the long term for this valuable sample. Amplified samples were then diluted to a working concentration.
All DNA samples were genotyped in duplicate for quality control. In addition, human DNA from cell lines was purchased from Coriell Cell Respositories for all representative genotypes in duplicate and genotypes confirmed by sequencing using DTCS chemistry on an ABI 3130×1. These and a no template control were run alongside study samples representing 9% of the total data output. Any samples that were not able to be genotyped to a 95% or greater confidence level were repeated under the same conditions.
FKBP5 was genotyped using assays for SNPs rs3800373, rs9296158, rs1360780, and rs9470080 purchased from Applied Biosystems, Inc. (ABI, Bedford, MA) as C27489960_10, C1256775_10, C8852038_10, and C92160_10 respectively. Individual allele discriminations were made using Taq Man Genotyping Master Mix (ABI Catalog No. 4371357) with amplification in an ABI 9700 thermal cycler and analyzing the endpoint fluorescence using a Tecan M200. If a genotype for either gene or SNP could not be determined after the first run, then it was repeated up to four times. The call rates for the four FKBP5 SNPs ranged from 99.8%–100%. Genotype distributions were in Hardy-Weinberg equilibrium (HWE; all p>.05). Haplotypes for the four FKBP5 SNPs were determined using Arlequin v3.5.1.3, which employs a pseudo-Bayesian approach to estimate phase (Excoffier & Lischer, 2010). Arlequin was able to estimate haplotypes for every participant with a posterior probability higher than 0.97, which allowed us to assign a score of zero, one, or two copies of the CATT haplotype to participants with a high degree of certainty (See Table 1 for distributions of SNPs and CATT haplotype). 37.9% (n=106) of participants had 0 copies of the CATT haplotype, 46.8% (n=131) had 1 copy, and 15.4% (n=43) had 2 copies of the haplotype. Because of the small number of participants with 2 copies, individuals with 1 or 2 copies of the haplotype were combined. Therefore, for genetic moderation analyses, a binary variable was used such that 37.9% of the sample was coded 0 (no CATT haplotype) and 62.1% were coded 1 (1 or 2 copies of the haplotype).
Table 1.
Description of FKBP5 SNPs and CATT haplotype by maltreatment groups
| SNP | Overall sample | Maltreated (n=163) |
Nonmaltreated n=117) |
|
|---|---|---|---|---|
| rs3800373 | χ2 (2)=.17, p>.05 | |||
| AA | 34.6% | 33.7% | 35.9% | |
| AC | 47.5% | 48.5% | 46.2% | |
| CC | 17.9% | 17.8% | 17.9% | |
| rs9296158 | χ2 (2)=.34, p>.05 | |||
| GG | 30.7% | 29.4% | 32.5% | |
| AG | 46.8% | 47.2% | 46.2% | |
| AA | 22.5% | 23.3% | 21.4% | |
| rs1360780 | χ2 (2)=.22, p>.05 | |||
| CC | 36.1% | 35.0% | 37.6% | |
| CT | 47.9% | 48.5% | 47.0% | |
| TT | 16.1% | 16.6% | 15.4% | |
| rs9470080 | χ2 (2)=.31, p>.05 | |||
| CC | 31.8% | 31.3% | 32.5% | |
| CT | 46.1% | 45.4% | 47.0% | |
| TT | 22.1% | 23.3% | 20.5% | |
| CATT haplotype | χ2 (1)=.03, p>.05 | |||
| no copies | 47.2% | 37.4% | 38.5% | |
| 1–2 copies | 52.8% | 62.6% | 61.5% |
African ancestry
To validate self-reported race, ancestral proportion testing was conducted. DNA from study participants was subjected to SNP genotyping of the Burchard et al panel of 106 SNPs (Lai et al., 2009; Yaeger et al., 2008), known to be informative for ancestry from Africa, Europe, and Native America. The SNPs were genotyped using the iPLEX platform from Sequenom Bioscience, Inc which uses the Sequenom MassArray. Samples are subjected to single base primer extension (SBE) with fluorophore labeled nucleotides from primers designed for SNPs of interest. The samples including the SBE products were placed on the iPLEX platform and MALDI-TOF was used to identify the allele based on the fluorophore passing the detector at the expected time associated with the mass of the SBE primer. The SNP genotyping results were then recoded and uploaded into STRUCTURE v2.3.4 which uses algorithms developed by Pritchard and colleagues (Falush Stephens, & Pritchard, 2003; 2007; Hubisz, Falush, Stephens, & Pritchard, 2009). Three SNP tests were excluded based on high allele call rates of the non-DNA containing wells. The data from remaining 103 loci were uploaded into the software and set to analyze with an Admixture model of ancestry and initialization of the simulation on the GALA cohort (initialize of POPINFO). The simulation was set to run with a Burn-in of 10,000, MCMC Reps of 1,000 and assuming 3 populations within the group. The results of the simulations were subsequently identified as percent association to each ancestry group based on the known ancestry of the GALA cohort. Among this sample of self-identified African-American participants, the mean proportion of African-Ancestry was .90, thus validating the self-report measure of race and supporting genotypic homogeneity.
Data Analytic Plan
Descriptive data analyses were conducting using SPSS 23, and structural equation models (SEMs) were performed using Mplus Version 7.4 (Muthén & Muthén, 1998–2015) with maximum likelihood (ML) estimator. First, measurement modeling was conducted to confirm the factor structure of the 3 proposed indicators of child internalizing symptoms (i.e. physiological anxiety, depressive symptoms, and worry/oversensitivity) and the factor structure of the 3 proposed indicators of problem drinking (i.e. consumption of hard liquor, binge drinking, and drunkenness). Next, measurement invariance testing was done to examine factor loading invariance for both latent factors across FKBP5 CATT haplotype variation. Results of measurement modeling informed model specification in the subsequent SEMs.
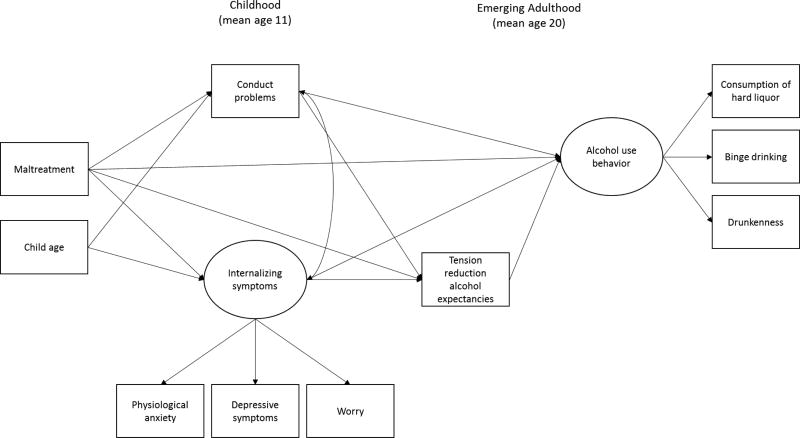
The first SEM was specified as illustrated in Figure 1. Child maltreatment (yes/no) and child age at wave 1 were included as exogenous variables. Wave 1 childhood conduct problems and the latent child internalizing symptoms factor (indicators: physiological anxiety, depressive symptoms, and worry/oversensitivity) were specified as mediators with correlated residuals. Wave 2 emerging adult tension reduction alcohol expectancies manifest variable was predicted by the childhood internalizing symptoms latent factor, child maltreatment, and childhood conduct problems. Finally, the emerging adult problem drinking latent factor (indicators: consumption of hard liquor, binge drinking, and drunkenness) was modeled as an endogenous variable predicted by emerging adult tension reduction alcohol expectancies, childhood internalizing symptoms latent factor, child maltreatment, and childhood conduct problems.
Figure 1.
Conceptual model
Missing data for endogenous variables were handled using full information maximum likelihood (FIML). Model fit for confirmatory factor analyses (CFAs) and structural equation models (SEMs) was evaluated using the comparative fit index (CFI), root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). CFI values greater than .95, RMSEA values less than .06, SRMR values less than .06, and a non-significant χ2 statistic were considered evidence of good model fit (Hu and Bentler, 1999; Yu and Muthen, 2002). Mediation was tested using 95% bias-corrected bootstrapped confidence intervals (CIs). CIs which do not include the value zero are considered statistically significant.
Next, genetic moderation was tested using the multiple-group method. Moderation of the internalizing path by FKBP5 CATT haplotype was assessed at the following two paths: 1) child maltreatment➔child internalizing latent factor and 2) child internalizing latent factor➔emerging adult tension reduction alcohol expectancies. Moderation of the externalizing path by FKBP5 CATT haplotype was assessed at the following two paths: 1) child maltreatment➔child conduct problems, and 2) child conduct problems➔emerging adult drinking. Moderated mediation was also tested using 95% bias-corrected bootstrapped confidence intervals (CIs). CIs which do not include the value zero are considered statistically significant.
Results
Preliminary Analyses
Overall, maltreated and nonmaltreated youth did not differ in childhood depressive symptoms (t(276)=−1.37, p>.05) and childhood worry/oversensitivity (t(274)=−1.23, p>.05). Maltreated children reported marginally significantly higher levels of physiological anxiety (t(274)=−1.72, p=.09) and significantly higher levels of conduct problems (t(278)=−2.19, p=.03) at wave 1. Maltreated and nonmaltreated children did not differ in their self-reported emerging adult alcohol expectancies (t(269)=−.02, p>.05), hard liquor consumption (t(278)=.37, p=n.s), binge drinking (t(278)=.58. p>.05), or drunkenness (t(278)=.71, p>.05).
SNP and haplotype frequencies for the overall sample, and comparing maltreated and nonmaltreated children are presented in Table 1. The groups did not differ on distributions of any of the 4 FKBP5 SNPs (rs3800373: χ2 (2)=.17, p>.05, rs9296158: χ2 (2)=.34, p>.05, rs1360780: χ2 (2)=.22, p>.05, rs9470080: χ2 (2)=.31, p>.05) and groups did not differ on CATT haplotype frequency (χ2 (1)=.03, p>.05). Therefore, results do not support gene-environment correlation (rGE) such that FKBP5 genotype did not affect the likelihood that children would be maltreated.
Table 2 provides the zero-order correlations among study variables for both haplotype groups. Notably, child maltreatment was related to higher levels of child physiological anxiety and depressive symptoms for individuals with at least one copy of the FKBP5 CATT haplotype (r = .15–.19, p<.05) but not for individuals with zero copies of the CATT haplotype (r = −.03–−.04, p>.05). Moreover, child internalizing symptom indicators (e.g., physiological anxiety, depressive symptoms, and worry) were related more strongly to emerging adult alcohol expectancies for those individuals with the CATT haplotype (r=.15–.16, ps =.04 – .06) than for those with zero copies of the haplotype (r=−.06–−.02, ps>.05).
Table 2.
Zero-order correlations among study variables by FKBP5 haplotype group
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Maltreatment status | − | −.07 | −.04 | −.03 | −.01 | −.02 | .01 | −.07 | −.10 | −.15 |
| 2. | Wave 1 age | .02 | − | .18 | .09 | .05 | .21* | .04 | .09 | .04 | .03 |
| 3. | Physiological anxiety | .19* | .16* | − | .62*** | .60*** | .15 | −.02 | .12 | .05 | .11 |
| 4. | Depressive symptoms | .15* | .09 | .56*** | − | .65*** | .23* | −.06 | −.01 | −.08 | .04 |
| 5. | Worry | .12 | .13 | .64*** | .61*** | − | .03 | −.04 | .03 | −.01 | .14 |
| 6. | Conduct problems | .21** | .21** | .13 | .10 | −.01 | − | .13 | .06 | .09 | .12 |
| 7. | Alcohol expectancies | −.01 | .11 | .15t | .15t | .16* | .02 | − | .25* | .26** | .27** |
| 8. | Hard liquor | .01 | .09 | .02 | −.09 | −.04 | .10 | .34*** | − | .81*** | .76*** |
| 9. | Binge | −.01 | .12 | .04 | .01 | .03 | .19 | .33*** | .72*** | − | .72*** |
| 10. | Drunk | .02 | .15 | .04 | −.02 | −.03 | .18* | .31*** | .77*** | .79*** | − |
Note: Correlations presented above the diagonal are for individuals with zero copies of the FKBP5 CATT haplotype and correlations presented below the diagonal are for individuals with at least 1 copy of the FKBP5 CATT haplotype. Maltreatment status is coded such that 0=nonmaltreated, 1=maltreated. All continuous variables are coded such that higher values indicted higher levels of the construct.
p<.07
p<.05
p<.01
p<.001.
Measurement Modeling
Confirmatory factor analysis (CFA) was conducted to determine the factor structure of the three childhood internalizing symptomatology measured variables (i.e., physiological anxiety, depressive symptoms, and worry/oversensitivity) and the three emerging adult alcohol use measured variables (i.e., hard liquor, binge drinking, drunkenness). Results confirmed a two factor model (χ2 (8, n = 280) = 8.20, p=.41, CFI = .99, RMSEA = .01, SRMR=.03), with statistically significant factor loadings (λ =.76–.82) for the childhood internalizing factor, and (λ =.87–.88) for the emerging adult alcohol use factor. The correlation between the two factors was non-significant (β=.03, p>.05).
Next, measurement invariance testing was conducting to determine whether the factor loadings varied by FKBP5 variation. Results of a model which constrained factors loadings to equality across groups evidenced good model fit (χ2 (24, n = 280) = 29.02, p=.05, CFI = .99, RMSEA = .04, SRMR=.04). Results of a model which allowed factor loadings to vary across FKBP5 groups was tested next and also evidenced good model fit (χ2 (20, n = 280) = 23.99, p=.24, CFI = .99, RMSEA = .04, SRMR=.04). Because the unconstrained model was not a significantly better fit to the data than the constrained model (Δχ2 (4) = 5.03, p>.05), there was evidence of metric measurement invariance across FKBP5 variation. Therefore, the factor structure and factor loadings for both child internalizing and emerging adult drinking did not vary by FKBP5 variation. These results informed the model specification of the multiple-group structural equation models described below.
Structural Equation Model
First, an SEM was estimated as depicted in Figure 1. The model evidenced good fit to the data (χ2 (26, n = 280) = 26.69, p = .42, CFI = .99, RMSEA = .01, SRMR = .02). Children who experienced maltreatment self-reported higher levels of conduct problems (β= .13, p = .01), as did older children (β = .21, p<.001). Child maltreatment was not a significant predictor of child internalizing symptoms (latent factor: (β = .10, p>.05); however, older children self-reported higher levels of internalizing symptoms (β = .15, p=.03). Emerging adult alcohol expectancies were not significantly predicted by child conduct problems (β = .06, p>.05), maltreatment status (β = −.02, p>.05), or internalizing symptoms (β = .09, p>.05). Finally, higher levels of emerging adult alcohol use was predicted by higher levels of tension reduction alcohol expectancies (β = .34, p<.001) and higher levels of childhood conduct problems (β =. 13, p = .04). Child maltreatment was not a significant unique predictor of emerging adult drinking (β = −.05, p >.05), nor was child internalizing symptoms (β = −.01, p >.05). The residual correlation between child internalizing symptoms and child conduct problems was non-significant.
The 95% bias-corrected bootstrap method was used to test the significance of the mediated effect of child maltreatment on emerging adult drinking by way of child conduct problems. This method was selected because it has been shown to provide more accurate confidence intervals (MacKinnon, 2008) and to be more highly powered for testing mediation effects in samples of this size (Fritz & MacKinnon, 2007). Confidence intervals that do not include the value zero are considered statistically significant. Results indicated that the effect of child maltreatment on emerging adult alcohol use was significantly mediated by child conduct symptoms (LCL=.005, UCL=.115), thus supporting an externalizing pathway of child maltreatment to emerging adult alcohol use.
Multiple Group Structural Equation Models
To examine moderation by FKBP5 genotype variation, two sets of multiple-group SEMs were tested: 1) moderation of the internalizing pathway, 2) moderation of the externalizing pathway. Models were specified as shown in Figure 1 with factor loadings and all structural paths constrained to equality across FKBP5 groups. This fully constrained model fit the data well (χ2 (71, n = 280) = 74.77, p=.36, CFI = .99, RMSEA = .02, SRMR=.06). Next, a partially unconstrained model to test for moderation of the internalizing pathway was estimated which relaxed constraints between FKBP5 CATT haplotype groups for the following two paths of interest: 1) maltreatment➔child internalizing latent factor, and 2) child internalizing latent factor➔emerging adult alcohol expectancies but maintained all other model constraints. This partially unconstrained model evidenced good model fit (χ2 (69, n = 280) = 68.58, p=.49, CFI = .99, RMSEA = .01, SRMR=.05), and was a significantly better fit to the data than the fully constrained model (Δχ2 (2) = 6.19, p<.05) supporting moderation by FKBP5.
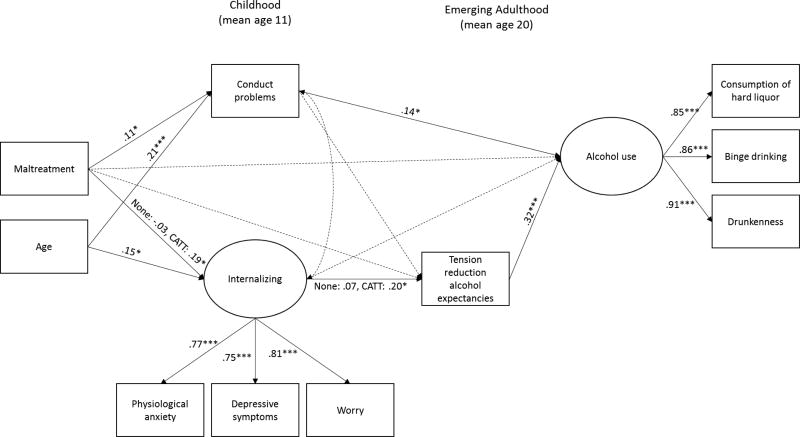
An examination of the unconstrained standardized path coefficients for each group revealed that child maltreatment significantly predicted higher levels of child internalizing symptoms for those children with at least one copy of the FKBP5 CATT haplotype (β=.19, p=.02) but not for those children without a copy of the haplotype (β=−.03, p>.05). Moreover, child internalizing symptoms predicted stronger emerging adult tension reduction alcohol expectancies for those individuals with at least one copy of the FKBP5 haplotype (β=.20, p=.03), but not for those without the haplotype (β=−.07, p>.05). See Figure 2 for results of the partially unconstrained SEM.
Figure 2.
Results of moderated mediation model.
Note: Standardized factor loadings and path coefficients are presented. “None” indicates results for the FKBP5 CATT haplotype group without any copies of the haplotype. “CATT” indicates results for the FKBP5 CATT haplotype group with at least 1 copy of the haplotype. *p<.05, ***p<.001.
Moderated mediation was also tested using the 95% bias-corrected bootstrap method. The sequential two mediator chain of child maltreatment ➔ child internalizing symptoms ➔ emerging adult alcohol expectancies ➔ emerging adult drinking was also significant for individuals with the FKBP5 CATT haplotype (LCL=.003, UCL=.095), but not for individuals without the CATT haplotype (LCL=−.015, UCL=.046). Thus, results support moderated mediation of the internalizing pathway from child maltreatment to emerging adult drinking. Specifically, for individuals with at least one copy of the FKBP5 CATT haplotype, child maltreatment predicted higher levels of internalizing symptoms in childhood, which in turn predicted stronger tension reduction alcohol expectancies in emerging adulthood, which predicted more emerging adult drinking. This mediational pathway was non-significant for individuals without a copy of the FKBP5 CATT haplotype.
Finally, a partially unconstrained model to test for moderation of the externalizing pathway was estimated which relaxed constraints between FKBP5 CATT haplotype groups for the following two paths of interest: 1) maltreatment➔child conduct problems, and 2) child conduct problems➔emerging adult drinking but maintained all other model constraints. This partially unconstrained model evidenced good model fit (χ2 (69, n = 280) = 71.05, p=.41, CFI = .99, RMSEA = .02, SRMR=.05), but was not a significantly better fit to the data than the fully constrained model (Δχ2 (2) = 3.71, p>.05). Thus, although there was support for the externalizing pathway, there was no evidence for moderation of this pathway by FKBP5.
Discussion
The aim of the present study was to investigate whether internalizing symptoms and tension reduction alcohol expectancies sequentially mediate the effect of child maltreatment on emerging adult problem drinking and to determine whether certain maltreated children may be especially vulnerable to traversing this internalizing pathway of risk based on FKBP5 genotypic variation. In doing so, this is the first study to prospectively test a stress and negative affect regulation pathway of child maltreatment risk for SUDs incorporating two critical consecutive mediators (internalizing symptoms and alcohol expectancies), while controlling for the robust externalizing pathway, and also including genotypic moderation of this progression.
First, our results are consistent with a number of prior studies showing that early childhood adversity interacts with FKBP5 variation to affect internalizing symptoms (e.g., Appel et al., 2011; Binder et al., 2009; Zimmerman et al., 2011). Specifically, we found that maltreatment leads to the development of internalizing symptoms during childhood (as measured by child report of physiological anxiety, depressive symptoms, and worry) only for those individuals with at least one copy of the FKBP5 CATT haplotype (minor alleles). Although a prior study failed to find evidence that FKBP5 moderated the effect of child maltreatment on child internalizing symptoms (Handley et al., 2015), the current study differs from that work in terms of our reliance on diverse measures of self-reported internalizing symptoms and our sample of exclusively African-American youth. On the contrary, Handley et al. (2015) employed observer report measures of various internalizing symptoms with a racially and ethnically diverse sample of children. It is possible that differing perceptions of the child’s internalizing symptoms between observers and children themselves, as well as sampling differences may explain these disparate results.
With regards to the development of alcohol expectancies, our findings indicate that whether child internalizing symptoms prospectively predict stronger tension reduction alcohol expectancies approximately nine years later, also depends on FKBP5 genotypic variation. We found that higher levels of internalizing symptoms in childhood affect stronger beliefs regarding the stress-reducing properties of alcohol in emerging adulthood only for those individuals with at least one copy of the FKBP5 CATT haplotype. Even before children initiate drinking, they hold beliefs about the effects of alcohol (e.g., Zucker, Kincaid, Fitzgerald, & Bingham, 1995). Parental drinking behavior and parental alcohol expectancies influence an individual’s own alcohol expectancies, as do one’s experience with alcohol effects once he or she begins drinking (e.g., Brown, Creamer, & Stetson, 1987; Donovan, Molina, & Kelly, 2009; Handley & Chassin, 2009; Jester, Wong, Cranford, Buu, Fitzgerald, & Zucker, 2015; Sher et al., 1996). Given the consistent and well-documented relation between alcohol expectancies and drinking behavior, a link the current study also supports (e.g., Handley et al., 2009; Jones, Corbin, & Fromme, 2001; Mann, Chassin, & Sher, 1987; Montes, Witkiewitz, Andersson, Fosses-Wong, Pace, Berglund, & Larimer, 2017; Sher et al., 1996; Jester et al., 2015), understanding how various developmental factors shape alcohol expectancies, and who is at greatest risk for tension-reduction alcohol expectancies, is critical to informing our knowledge of the development of SUDs. We advance the extant literature by showing that for certain vulnerable youth with a specific FKBP5 genotypic profile, childhood internalizing symptoms also shape beliefs regarding the tension reducing benefits of drinking later in development. These results are consistent with developmental theory regarding the internalizing pathway of risk for SUDs by demonstrating that alcohol expectancies, particularly those related to stress and negative affect regulation, are indeed affected by childhood experiences of depression and anxiety for some susceptible individuals (Hussong et al., 2011; Sher, 1991).
Taken together our results provide evidence for an internalizing pathway by which maltreated children are at risk for developing problem drinking that is distinct from an externalizing pathway and is moderated by FKBP5 genotypic variation. More specifically, the central finding of this study is that child maltreatment affects childhood internalizing symptoms which in turn affects stronger tension reduction alcohol expectancies in emerging adulthood, which results in higher levels of problem drinking behavior. Critically, we found that this is not a universal pathway; rather FKBP5 genotypic variation is an important moderator of this risk trajectory. These findings are consistent with the growing body of work highlighting FKBP5 as an important gene to study in relation to early adversity (see Zannas & Binder, 2014 for review). Given its role in the stress response system and as a regulator of the glucocorticoid receptor (GR; Binder, 2009; Galat, 2013; Zannas et al., 2014), polymorphisms in FKPB5 warrant continued research attention, especially among studies of early stress exposure. Thus, our results extend prior research on the interactive effects of FKBP5 variation and early adversity by being the first to document its role in an internalizing pathway of risk from child maltreatment to emerging adult problem drinking.
These findings are consistent with the extant literature showing that maltreated children are at risk for developing problems with substances (e.g., Buckingham et al., 2013; Dube et al., 2003; Hamburger et al., 2008; Handley et al., 2015; Huang et al., 2011; Rogosch et al., 2010; Shin et al., 2010; Tonmyr et al., 2010; Wilsnack et al., 1997). Although we did not find evidence for a direct effect of child maltreatment on emerging adult problem drinking, our results support two distinct mediated pathways of risk. In accordance with the well documented externalizing pathway to SUD (see Chassin et al., 2009; Chassin et al., 2013; Sher, 1991; Zucker 2006; Zucker, et al., 2011 for reviews), we found that maltreated children self-report higher levels of childhood conduct problems, which, over and above childhood internalizing problems, predict higher levels of emerging adult problem drinking. This pathway was not moderated by FKBP5 genotypic variation. Importantly, our results show a more nuanced and complex internalizing pathway that is mediated by child internalizing symptoms and emerging adult alcohol expectancies, exists over and above the robust externalizing pathway, and is moderated by FKBP5 genotype. Hussong and colleagues (2011) described an internalizing pathway to SUDs marked by an inhibited temperament in infancy, internalizing symptoms throughout development, positive substance use expectancies and interpersonal skills deficits, as well as coping motivations for substance use. Our findings support this stress and negative affect pathway to problem substance use and expand on this model by showing the relevance of FKBP5 to these associations. It is important to highlight that without the inclusion of FKBP5 moderation, results would have pointed only to an externalizing pathway. It was not until we considered FKBP5 genotypic variation that an internalizing pathway emerged.
To date only one prior study has examined an internalizing and externalizing pathway of child maltreatment risk to substance use while also considering FKBP5. Specifically, among a sample of adolescents, Handley, Rogosch, and Cicchetti (2015) found that individuals with the FKBP5 CATT haplotype were more likely to traverse an externalizing pathway from child maltreatment to adolescent marijuana dependence than individuals without the haplotype. Handley and colleagues (2015) did not find evidence for an internalizing pathway, nor did they find support for FKBP5 moderation of this pathway. A number of methodological differences between the studies are worth noting when considering the differing findings. First, as described above, the sample for the present study included African-American individuals only. This was done to minimize difficulties related to population stratification. The Handley et al. (2015) sample was racially and ethnically diverse. Second, the two studies differ in their developmental period under investigation. The present study focused on problem drinking behavior among emerging adults, whereas the Handley et al. (2015) study examined marijuana dependence symptoms among adolescents. In this way, the Handley et al. (2015) paper investigated pathways from child maltreatment to a more clinical outcome during an earlier period of development. The current study focused exclusively on self-report childhood symptomatology whereas Handley et al. (2015) measured childhood symptomatology using camp counselor and peer ratings. Finally, we included both internalizing and externalizing pathways within the same model in order to examine the unique effects of each mechanism, compared to testing each model separately as was done in the Handley et al. (2015) paper. That these notable methodological differences may contribute to disparate findings is consistent with the results of a recent review of the internalizing pathway of risk for SUD which suggests that the substance under investigation, as well as the developmental period, and the type of internalizing symptom may all contribute to differing findings (Hussong et al., 2017).
Although this study makes important new contributions to the literature on child maltreatment, the development of substance use disorders, and the role of FKBP5 in these associations, limitations are worth noting. First, we relied on a binary measure of child maltreatment experiences occurring prior to the first wave of assessment. Given accumulating evidence that FKBP5 interacts with early adversity, and not later traumatic experiences, it will be important to further elucidate this interactive effect with more specific measures of the developmental timing of the maltreatment experience throughout childhood. Moreover, although we selected an FKBP5 haplotype with robust empirical support for its role in stress-regulation (Zannas & Binder, 2014), it is only one gene among many involved in this complex process. Polygenic risk scores which incorporate multiple genes related to the stress-response system will be important to incorporate into future research. Finally, we selected a sample of exclusively African-American youth for this investigation because genetic variation can differ across ancestral groups and thus challenge interpretations of gene by environment interactions. However, this limits the generalizability of our findings and calls for future studies with other samples from other ancestral groups.
In conclusion, the present study sheds light on a lesser studied and complex pathway of risk from child maltreatment to emerging adult drinking that is mediated by internalizing symptoms in childhood and tension-reduction alcohol expectancies in emerging adulthood, and is moderated by FKBP5 genotypic variation. These findings provide important directions for preventive intervention design for maltreated children and their families by showing that for vulnerable youth with the minor alleles of the FKBP5 CATT haplotype, early internalizing symptoms may set the course for problematic beliefs about drinking which in turn may elevate risk for problem drinking. Thus, several points of intervention are implicated (e.g., depressive and anxiety symptoms in childhood and alcohol expectancies in adolescence/emerging adulthood) which may alter the trajectory of SUD risk for maltreated children.
Acknowledgments
We are grateful to the Jacobs Foundation (to Dante Cicchetti) and the National Institute on Drug Abuse (R01-DA01774 to Fred A. Rogosch and Dante Cicchetti) for their support of this work.
References
- Appel K, Schwahn C, Mahler J, Schulz A, Spitzer C, Fenske K. Moderation of adult depression by a polymorphism in the FKBP5 gene and childhood physical abuse in the general population. Neuropsychopharmacology. 2011;36:1982–1991. doi: 10.1038/npp.2011.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett D, Manly JT, Cicchetti D. Defining child maltreatment: The interface between policy and research. In: Cicchetti D, Toth SL, editors. Child Abuse, Child Development, and Social Policy. Norwood, NJ: Ablex; 1993. pp. 7–74. [Google Scholar]
- Bevilacqua L, Carli V, Sarchiapone M, George DK, Goldman D, Roy A. Interaction between FKBP5 and childhood trauma and risk of aggressive behavior. Archives of General Psychiatry. 2012;69:62–70. doi: 10.1001/archgenpsychiatry.2011.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binder EB. The role of FKBP5, a co-chaperone of the glucocorticoid receptor in the pathogenesis and therapy of affective and anxiety disorders. Psychoneuroendocrinology. 2009;34:S186–S195. doi: 10.1016/j.psyneuen.2009.05.021. [DOI] [PubMed] [Google Scholar]
- Binder EB, Bradley RG, Liu W, Epstein MP, Deveau TC, Mercer KB, Tang Y, Ressler KJ. Association of FKBP5 polymorphisms and childhood abuse with risk of posttraumatic stress disorder symptoms in adults. Journal of the American Medical Association. 2008;299(11):1291–1305. doi: 10.1001/jama.299.11.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binder EB, Salyakina D, Lichtner P, Wochnik GM, Ising M, Pütz B. Polymorphisms in FKBP5 are associated with increased recurrence of depressive episodes and rapid response to antidepressant treatment. Nature Genetics. 2004;36:1319–1325. doi: 10.1038/ng1479. [DOI] [PubMed] [Google Scholar]
- Brown SA, Creamer VA, Stetson BA. Adolescent alcohol expectancies in relation to personal and parental drinking patterns. Journal of Abnormal Psychology. 1987;96(2):117–121. doi: 10.1037/0021-843X.96.2.117. [DOI] [PubMed] [Google Scholar]
- Buckingham ET, Daniolos P. Longitudinal outcomes for victims of child abuse. Current Psychiatry Reports. 2013;15:342. doi: 10.1007/s11920-012-0342-3. [DOI] [PubMed] [Google Scholar]
- Chassin L, Hussong A, Beltran I. Adolescent substance use. In: Lerner RM, Steinberg L, editors. Handbook of Adolescent Psychology: Vol. 1. Individual bases of adolescent development. 3. Hoboken, NJ: Wiley; 2009. [Google Scholar]
- Chassin L, Pitts SC, DeLucia C, Todd M. A longitudinal study of children of alcoholics: Predicting young adult substance use disorders, anxiety, and depression. Journal of Abnormal Psychology. 1999;108(1):106–119. doi: 10.1037/0021-843X.108.1.106. [DOI] [PubMed] [Google Scholar]
- Chassin L, Sher KJ, Hussong A, Curran P. The developmental psychopathology of alcohol use and alcohol disorders: Research achievements and future directions. Development and Psychopathology. 2013;25(4):1567–1584. doi: 10.1017/S0954579413000771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christiansen BA, Goldman MS, Inn A. Development of alcohol-related expectancies in adolescents: Separating pharmacological from social-learning influences. Journal of Consulting and Clinical Psychology. 1982;50:336–344. doi: 10.1037/0022-006X.50.3.336. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Lynch M. Failures in the expectable environment and their impact on individual development: The case of child maltreatment. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology: Risk, Disorder, and Adaptation. Vol. 2. New York, NY: John Wiley & Sons, Inc.; 1995. pp. 32–71. [Google Scholar]
- Cicchetti D, Toth SL. Child maltreatment and developmental psychopathology: A multilevel perspective. In: Cicchetti D, editor. Developmental Psychopathology. 3. Vol. 3. New York: Wiley; 2016. pp. 457–512. Maladaptation and Psychopathology) [Google Scholar]
- Cicchetti D, Toth SL. Child Maltreatment. In: Lamb M, editor. Handbook of Child Psychology and Developmental Science. 7. Vol. 3. New York: Wiley; 2015. pp. 513–563. Socioemotional Process. [Google Scholar]
- Cicchetti D, Toth SL, Manly JT. Unpublished manuscript. Mt. Hope Family Center, Rochester; NY: 2003. Maternal maltreatment classification interview. [Google Scholar]
- Cooper ML, Kuntsche E, Levitt A, Barber LL, Wolf S. Motivational models of substance use: A review of theory and research on motives for using alcohol, marijuana, and tobacco. The Oxford Handbook of Substance Use and Substance Use Disorders: Two-Volume Set. 2016:375. [Google Scholar]
- Costello EJ. Psychiatric predictors of adolescent and young adult drug use and abuse: What have we learned? Drug and Alcohol Dependence. 2007;88S:S97–S99. doi: 10.1016/j.drugalcdep.2006.12.027. [DOI] [PubMed] [Google Scholar]
- Dackis MN, Rogosch FA, Oshri A, Cicchetti D. The role of limbic systemirritability in linking history of childhood maltreatment and psychiatric outcomes in low- income, high-risk women: Moderation by FK506 binding protein 5 haplotype. Development and Psychopathology. 2012;24:1237–1252. doi: 10.1017/S0954579412000673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan JE, Molina BS, Kelly TM. Alcohol outcome expectancies as socially shared and socialized beliefs. Psychology of Addictive Behaviors. 2009;23(2):248–259. doi: 10.1037/a0015061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk for illicit drug use: The adverse childhood experiences study. Pediatrics. 2003;111:564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- Edwards AC, Latendresse SJ, Heron J, Cho SB, Hickman M, Lewis G, Kendler KS. Childhood internalizing symptoms are negatively associated with earlyadolescent alcohol use. Alcoholism: Clinical and Experimental Research. 2014;38(6):1680–1688. doi: 10.1111/acer.12402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott JC, Stohl M, Wall MM, Keyes KM, Goodwin RD, Skodol AE, Hasin DS. The risk for persistent adult alcohol and nicotine dependence: the role ofchildhood maltreatment. Addiction. 2014;109(5):842–850. doi: 10.1111/add.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Excoffier L, Lischer HEL. Arlequin suite ver 3.5: A new series of programs to perform population genetics analyses under Linux and Windows. Molecular Ecology Resources. 2010;10:564–567. doi: 10.1111/j.1755-0998.2010.02847.x. [DOI] [PubMed] [Google Scholar]
- Falush D, Stephens M, Pritchard JK. Inference of population structure using multilocus genotype data: Dominant markers and null alleles. Molecular Ecology Notes. 2007;7:574–578. doi: 10.1111/j.1471-8286.2007.01758.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falush D, Stephens M, Pritchard JK. Inference of population structure using multilocus genotype data: Linked loci and correlated allele frequencies. Genetics. 2003;164(4):1567–87. doi: 10.1093/genetics/164.4.1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychological Science. 2007;18(3):233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galat A. Functional diversity and pharmacological profiles of the FKBPs and theircomplexes with small natural ligands. Cellular and Molecular Life Sciences. 2013;70(18):3243–3275. doi: 10.1007/s00018-012-1206-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein AL, Flett GL, Wekerle C. Child maltreatment, alcohol use and drinking consequences among male and female college students: An examination of drinking motives as mediators. Addictive Behaviors. 2010;35(6):636–639. doi: 10.1016/j.addbeh.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Grayson CE, Nolen-Hoeksema S. Motives to drink as mediators between childhoodsexual assault and alcohol problems in adult women. Journal of Traumatic Stress. 2005;18:137–145. doi: 10.1002/jts.20021. [DOI] [PubMed] [Google Scholar]
- Hamburger ME, Leeb RT, Swahn MH. Childhood maltreatment and earlyalcohol use among high-risk adolescents. Journal of Studies on Alcohol and Drugs. 2008;69:291–295. doi: 10.15288/jsad.2008.69.291. [DOI] [PubMed] [Google Scholar]
- Handley ED, Chassin L. Intergenerational transmission of alcohol expectancies in ahigh-risk sample. Journal of Studies on Alcohol and Drugs. 2009;70(5):675–682. doi: 10.15288/jsad.2009.70.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handley ED, Rogosch FA, Cicchetti D. Developmental pathways from childmaltreatment to adolescent marijuana dependence: Examining moderation by FK506binding protein 5 gene (FKBP5) Development and Psychopathology. 2015;27(4):1489–1502. doi: 10.1017/S0954579415000899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler P. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Huang MC, Schwandt ML, Chester JA, Kirchhoff AM, Kao CF, Liang T, Goldman D. FKBP5 moderates alcohol withdrawal severity: Human genetic association and functional validation in knockout mice. Neuropsychopharmacology. 2014;39(8):2029–2038. doi: 10.1038/npp.2014.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang S, Trapido E, Fleming L, Arheart K, Crandall L, French M. The long-termeffects of childhood maltreatment experiences on subsequent illicit drug use and drug- related problems in young adulthood. Addictive Behaviors. 2011;36:95–102. doi: 10.1016/j.addbeh.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubisz MJ, Falush D, Stephens M, Pritchard JK. Inferring weak population structure with the assistance of sample group information. Molecular Ecology Resources. 2009;9:1322–32. doi: 10.1111/j.1755-0998.2009.02591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson A, Wekerle C, Goldstein AL, Ellenbogen S, Waechter R, Thompson K, Stewart SH. Gender differences in emotion-mediated pathways from childhoodsexual abuse to problem drinking in adolescents in the child welfare system. Journal of Child and Adolescent Trauma. 2017;10:19–28. doi: 10.1007/s40653-016-0125-9. [DOI] [Google Scholar]
- Hussong AM, Ennett ST, Cox MJ, Haroon M. A systematic review of theunique prospective association of negative affect symptoms and adolescent substance usecontrolling for externalizing symptoms. Psychology of Addictive Behaviors. 2017;31(2):137. doi: 10.1037/adb0000247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychology of Addictive Behaviors. 2011;25:390–404. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Sartor CE. The natural course of substance use and dependence. The Oxford Handbook of Substance Use and Substance Use Disorders. 2016;1(29):67. [Google Scholar]
- Jester JM, Steinberg DB, Heitzeg MM, Zucker RA. Coping expectancies, notenhancement expectancies, mediate trauma experience effects on problem alcohol use: Aprospective study from early childhood to adolescence. Journal of Studies on Alcohol and Drugs. 2015;76(5):781–789. doi: 10.15288/jsad.2015.76.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jester JM, Wong MM, Cranford JA, Buu A, Fitzgerald HE, Zucker RA. Alcohol expectancies in childhood: Change with the onset of drinking and ability topredict adolescent drunkenness and binge drinking. Addiction. 2015;110(1):71–79. doi: 10.1111/add.12704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones BT, Corbin W, Fromme K. A review of expectancy theory and alcoholconsumption. Addiction. 2001;96(1):57–72. doi: 10.1046/j.1360-0443.2001.961575.x. [DOI] [PubMed] [Google Scholar]
- Jones DJ, Lewis T, Litrownik A, Thompson R, Proctor LJ, Isbell P, Runyan D. Linking childhood sexual abuse and early adolescent risk behavior: The intervening role of internalizing and externalizing problems. Journal of Abnormal Child Psychology. 2013;41(1):139–150. doi: 10.1007/s10802-012-9656-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King KM, Chassin L. Adolescent stressors, psychopathology, and young adultsubstance dependence: A prospective study. Journal of Studies on Alcohol and Drugs. 2008;69(5):629–638. doi: 10.15288/jsad.2008.69.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. The Children’s Depression Inventory: A self-rated depression scale for school-aged youngsters. Unpublished manuscript 1982 [Google Scholar]
- Kovacs M. Children’s depression inventory (CDI) Toronto: Multi-Health Systems Inc; 2004. [Google Scholar]
- Lai CQ, Tucker KL, Choudhry S, Parnell LD, Mattei J, García-Bailo B, et al. Population admixture associated with disease prevalence in the Boston Puerto Rican health study. Human Genetics. 2009;125:199–209. doi: 10.1007/s00439-008-0612-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Harold GT, Van Ryzin MJ, Elam K, Chamberlain P. Girls’ tobaccoand alcohol use during early adolescence: Prediction from trajectories of depressivesymptoms across two studies. Journal of Child & Adolescent Substance Abuse. 2012;21(3):254–272. doi: 10.1080/1067828X.2012.700853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TL, Kotch J, Wiley TR, Litrownik AJ, English DJ, Thompson R, Dubowitz H. Internalizing problems: A potential pathway from childhood maltreatment to adolescent smoking. Journal of Adolescent Health. 2011;48(3):247–252. doi: 10.1016/j.jadohealth.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman R, Armeli S, Scott DM, Kranzler HR, Tennen H, Covault J. FKBP5 genotype interacts with early life trauma to predict heavy drinking in collegestudents. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics. 2016;171(6):879–887. doi: 10.1002/ajmg.b.32460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovallo WR, Enoch M, Acheson A, Cohoon AJ, Sorocco KH, Hodgkinson CA, Vincent AS, Goldman D. Early-life adversity interacts with FKBP5 genotypes: Altered working memory and cardiac stress reactivity in the Oklahoma Family Health Patterns Project. Neuropsychopharmacology. 2016;78:1–9. doi: 10.1038/npp.2015.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to Statistical Mediation Analysis. New York, NY: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- Mann LM, Chassin L, Sher KL. Alcohol expectancies and the risk for alcoholism. Journal of Counseling and Clinical Psychology. 1987;55(3):411–417. doi: 10.1037/0022-006X.55.3.411. [DOI] [PubMed] [Google Scholar]
- Masten AS, Cicchetti D. Developmental cascades. Development and Psychopathology. 2010;22(3):491–495. doi: 10.1017/S0954579410000222. [DOI] [PubMed] [Google Scholar]
- McCarty CA, Wymbs BT, King KM, Mason WA, Stoep AV, McCauley E, Baer J. Developmental consistency in associations between depressive symptoms and alcohol use in early adolescence. Journal of Studies on Alcohol and Drugs. 2012;73(3):444–453. doi: 10.15288/jsad.2012.73.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezquita L, Ibáñez MI, Moya J, Villa H, Ortet G. A longitudinal examinationof different etiological pathways to alcohol use and misuse. Alcoholism: Clinical and Experimental Research. 2014;38(6):1770–1779. doi: 10.1111/acer.12419. [DOI] [PubMed] [Google Scholar]
- Montes KS, Witkiewitz K, Andersson C, Fossos-Wong N, Pace T, Berglund M, &Larimer ME. Trajectories of positive alcohol expectancies and drinking: Anexamination of young adults in the US and Sweden. Addictive Behaviors. 2017;73:74–80. doi: 10.1016/j.addbeh.2017.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, Ollendick T, King N, Bogie N. Three traditional and three new childhood anxiety questionnaires: Their reliability and validity in a normal adolescent sample. Behaviour Research and Therapy. 2002;40(7):753–772. doi: 10.1016/s0005-7967(01)00056-0. http://doi.org/10.1016/S0005-7967(0100056-0) [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. Seventh Edition. Los Angeles, CA: Muthen & Muthen; 1998–2015. [Google Scholar]
- Nylander I, Todkar A, Granholm L, Vrettou M, Bendre M, Boon W, Comasco E. Evidence for a link between Fkbp5/FKBP5, early life social relations and alcoholdrinking in young adult rats and humans. Molecular Neurobiology. 2016:1–10. doi: 10.1007/s12035-016-0157-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neil KA, Conner BT, Kendall PC. Internalizing disorders and substance usedisorders in youth: Comorbidity, risk, temporal order, and implications for intervention. Clinical Psychology Review. 2011;31(1):104–112. doi: 10.1016/j.cpr.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Oshri A, Rogosch FA, Burnette ML, Cicchetti D. Developmental pathways toadolescent cannabis abuse and dependence: Child maltreatment, emerging personality, and internalizing versus externalizing psychopathology. Psychology of Addictive Behaviors. 2011;25:634–644. doi: 10.1037/a0023151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesola F, Shelton KH, Heron J, Munafò M, Maughan B, Hickman M, van den Bree MB. The mediating role of deviant peers on the link between depressed mood and harmful drinking. Journal of Adolescent Health. 2015;56(2):153–159. doi: 10.1016/j.jadohealth.2014.10.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds CR, Richmond BO. What I think and feel: A revised measure of children’s manifest anxiety. Journal of Abnormal Child Psychology. 1997;25(1):15–20. doi: 10.1023/a:1025751206600. http://doi.org/10.1023/A:1025751206600. [DOI] [PubMed] [Google Scholar]
- Rogosch FA, Oshri A, Cicchetti D. From child maltreatment to adolescent cannabis abuse and dependence: A developmental cascade model. Development and Psychopathology. 2010;22:883–897. doi: 10.1017/S0954579410000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy A, Gorodetsky E, Yuan Q, Goldman D, Enoch MA. Interaction of FKBP5, a stress-related gene, with childhood trauma increases the risk for attempting suicide. Neuropsychopharmacology. 2010;35:1674–1683. doi: 10.1038/npp.2009.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy A, Hodgkinson CA, DeLuca V, Goldman D, Enoch MA. Two HPA axisgenes, CRHBP and FKBP5, interact with childhood trauma to increase the risk for suicidal behavior. Journal of Psychiatric Research. 2012;46:72–79. doi: 10.1016/j.jpsychires.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedlak AJ, Mettenburg J, Basena M, Petta I, McPherson K, Greene A. Fourth National Incidence Study of Child Abuse and Neglect (NIS-4): Report to Congress. Washington, DC: US Department of Health and Human Services, Administration for Children, Youth and Families; 2010. [Google Scholar]
- Sher KJ. Children of alcoholics: A critical appraisal of theory and research. Chicago, IL: University of Chicago Press; 1991. [Google Scholar]
- Sher KJ, Grekin ER, Williams NA. The development of alcohol use disorders. Annu. Rev. Clin Psychol. 2005;1:493–523. doi: 10.1146/annurev.clinpsy.1.102803.144107. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Wood MD, Wood PK, Raskin G. Alcohol outcome expectancies and alcohol use: A latent variable cross-lagged panel study. Journal of abnormal psychology. 1996;105(4):561–574. doi: 10.1037/0021-843X.105.4.561. [DOI] [PubMed] [Google Scholar]
- Shin SH, Hong HG, Hazen AL. Childhood sexual abuse and adolescent substance use: A latent class analysis. Drug and Alcohol Dependence. 2010;109:226–235. doi: 10.1016/j.drugalcdep.2010.01.013. [DOI] [PubMed] [Google Scholar]
- Tonmyr L, Thornton T, Draca J, Wekerle C. A review of childhood maltreatment and adolescent substance use relationship. Current Psychiatry Reviews. 2010;6:223–234. doi: 10.2174/157340010791792581. [DOI] [Google Scholar]
- White MG, Bogdan R, Fisher PM, Munoz KE, Williamson DE, Hariri AR. FKBP5 and emotional neglect interact to predict individual differences in amygdala reactivity. Genes, Brain, and Behavior. 2012;11:869–878. doi: 10.1111/j.1601-183X.2012.00837.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilsnack SC, Vogeltanz ND, Klassen AD, Harris TR. Childhood sexual abuse and women’s substance abuse: National survey findings. Journal of Studies on Alcohol. 1997;58(3):264–271. doi: 10.15288/jsa.1997.58.264. [DOI] [PubMed] [Google Scholar]
- Xie P, Kranzler HR, Poling J, Stein MB, Anton RF, Farrer LA. Interaction of FKBP5 with childhood adversity on risk for post-traumatic stress disorder. Neuropsychopharmacology. 2010;35:1684–1692. doi: 10.1038/npp.2010.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaeger R, Avila-Bront A, Abdul K, Nolan PC, Grann VR, Birchette MG, Ziv E. Comparing genetic ancestry and self-described race in African Americans born in the United States and in Africa. Cancer Epidemiology Biomarkers & Prevention. 2008;17(6):1369–1338. doi: 10.1158/1055-9965.EPI-07-2505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaylaci FT, Cicchetti D, Rogosch FA, Bulut O, Hetzel SR. The interactive effects of child maltreatment and the FKBP5 binding protein 5 gene (FKBP5) on dissociative symptoms in adolescence. Development and Psychopathology. 2016:1–13. doi: 10.1017/S095457941600105X. [DOI] [PubMed] [Google Scholar]
- Yu CY, Muthén BO. Evaluation of model fit indices for latent variable models with categorical and continuous outcomes (Technical Report) Los Angeles, CA: University of California at Los Angeles, Graduate School of Education and Information Studies; 2002. [Google Scholar]
- Zannas AS, Binder EB. Gene-environment interactions at the FKBP5 locus: Sensitive periods, mechanisms and pleiotropism. Genes, Brain and Behavior. 2014;13(1):25–37. doi: 10.1111/gbb.12104. [DOI] [PubMed] [Google Scholar]
- Zimmermann P, Brückl T, Nocon A, Pfister H, Binder EB, Uhr M, Ising M. Interaction of FKBP5 gene variants and adverse life events in predicting depression onset: Results from a 10-year prospective community study. American Journal of Psychiatry. 2011;168(10):1107–1116. doi: 10.1176/appi.ajp.2011.10111577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker RA. Alcohol use and alcohol use disorders: A developmental-biopsychosocial systems formulation covering the life course. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology. 2. Vol. 3. New York: Wiley; 2006. pp. 620–656. Risk, Disorder, and Adaptation) [Google Scholar]
- Zucker RA, Heitzeg MM, Nigg JT. Parsing the undercontrol-disinhibition pathway to substance use disorders: A multilevel developmental problem. Child Development Perspectives. 2011;5:248–255. doi: 10.1111/j.1750-8606.2011.00172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker RA, Kincaid SB, Fitzgerald HE, Bingham CR. Alcohol schema acquisition in preschoolers: Differences between children of alcoholics and children of nonalcoholics. Alcoholism: Clinical and Experimental Research. 1995;19(4):1011–1017. doi: 10.1111/j.1530-0277.1995.tb00982.x. [DOI] [PubMed] [Google Scholar]