Abstract
Background and objectives
Uremic pruritus in patients on hemodialysis is associated with depression, lower quality of life, and mortality. We studied the prevalence, awareness, and treatment of pruritus to assess how well this important condition is currently managed internationally.
Design, setting, participants, & measurements
Data from 35,452 patients on hemodialysis in up to 17 countries from the Dialysis Outcomes and Practice Patterns Study were analyzed to describe pruritus prevalence from 1996 to 2015. Data from 6256 patients and 268 medical directors in 17 countries in 2012–2015 were analyzed to describe predictors, effects, medical directors’ awareness, and treatment of pruritus.
Results
Patients very much or extremely bothered by itching declined from 28% in 1996 to 18% in 2015. In 2012–2015, among patients nearly always or always bothered by itching, pruritus had a major effect on work and social life; 18% used no treatment for pruritus, and 17% did not report itching to health care staff. In total, 69% of medical directors underestimated the prevalence of pruritus in their unit. Managing high serum phosphorus and low Kt/V was ranked as the most important intervention, but no relationship was found between these factors and pruritus; 57% of medical directors used oral antihistamines for first-line chronic treatment of pruritus. Gabapentin was used by 45% as first-, second-, or third-line treatment. Nalfurafine was only used in Japan.
Conclusions
The prevalence of pruritus in people on hemodialysis is decreasing but remains underestimated. Large numbers of patients on hemodialysis with severe pruritus do not receive treatment. There is wide variation in the use of unlicensed medications for the treatment of pruritus. These data provide a benchmark for initiatives to improve the management of uremic pruritus.
Multimedia
This article contains multimedia at https://vimeo.com/49458473
This article contains multimedia at vimeo.com/49455976
Keywords: dialysis, hemodialysis, outcomes, gabapentin, Phosphorus, renal dialysis, Prevalence, depression, Benchmarking, Physician Executives, quality of life, Cyclohexanecarboxylic Acids, gamma-Aminobutyric Acid, Histamine Antagonists
Introduction
Uremic pruritus is common in people with CKD (1), including in those on maintenance hemodialysis (HD) (2). It is associated with substantially reduced quality of life, depression, poor sleep quality, and increased mortality (2) (Supplemental Movie 1) but has been under-recognized by health care providers (3–5). Research into pruritus is a high priority for patients (6).
Treatment of pruritus can be graded according to the severity of symptoms. Patients with mild or localized symptoms may prefer topical treatment, whereas more severe or generalized itching may require systemic treatment (7).
Four randomized, controlled trials of a total of 138 patients with severe pruritus have shown gabapentin to reduce itch by between 4.6 and 6.4 cm more than placebo on a 10-cm visual analog scale (8,9) (Supplemental Movie 2). Pregabalin (n=67) reduced itch severity by 4.6 cm more than placebo (n=57) and also improved sleep quality and health-related quality of life (10). In a case series of 71 patients with severe pruritus, 85% were relieved of itching with gabapentin or pregabalin (11). Use of these agents is supported by European dermatology guidelines (7) and a Cochrane systematic review (12).
Nalfurafine, a κ-opioid receptor agonist, reduced the severity of itch by 0.95 cm more than placebo on a 10-cm visual analog scale score in one randomized, controlled trial (13) and by 0.9 and 1.0 cm more than placebo in a second using two doses (14). Single randomized, controlled trials of turmeric, montelukast, and zinc sulfate have shown a significant reduction in itch compared with placebo and warrant further study (15–17).
We have conducted a pruritus-related survey in 17 countries in the Dialysis Outcomes and Practice Patterns Study (DOPPS) to assess how pruritus is currently managed and to provide a benchmark for quality improvement initiatives.
Materials and Methods
Patients and Data Collection
The DOPPS is an international prospective cohort study of patients on HD ≥18 years of age. Study patients are enrolled randomly from a representative sample of randomly selected HD facilities within each nation at the start of each study phase as described previously (18,19). Study approval was obtained by a central institutional review board. Additional study approval and patient consent were obtained as required by national and local ethics committee regulations.
To study changes in pruritus prevalence over time, we analyzed data from 51,062 patients on HD enrolled in the DOPPS at the beginning of DOPPS phases 1–5 (i.e., 1996–2015) from up to 21 countries (Figure 1). All patients were offered a questionnaire about their health, care, quality of life, and symptoms; 39,553 returned their questionnaires, and of those, 35,452 answered the question regarding how bothered they were by itchy skin.
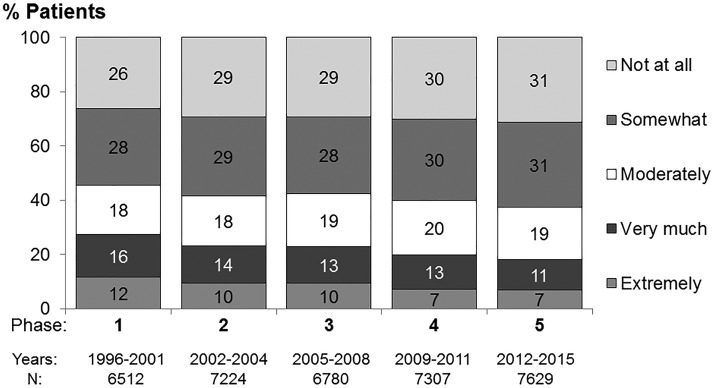
Figure 1.
The percentage of patients very much or extremely bothered by itchy skin declined between 1996 and 2015 from 28% to 18%. Question wording: “To what extent were you bothered by itchy skin during the past 4 weeks?” Australia, Belgium, Canada, China, France, the six Gulf Cooperation Council (GCC) countries (Bahrain, Qatar, Kuwait, Oman, Saudi Arabia, and United Arab Emirates), Germany, Italy, Japan, New Zealand, Russia, Spain, Sweden, Turkey, the United Kingdom, and the United States were analyzed. The DOPPS phase 1 collected data from 1996 to 2001, the DOPPS phase 2 collected data from 2002 to 2004, the DOPPS phase 3 collected data from 2005 to 2008, the DOPPS phase 4 collected data from 2009 to 2011, and the DOPPS phase 5 collected data from 2012 to 2015. Data collection in Australia, Belgium, Canada, New Zealand, and Sweden did not begin until phase 2; data collection in China began in phase 4 and started in the GCC countries, Russia, and Turkey in phase 5. Australia, China, France, and New Zealand were excluded in phase 5.
To study current awareness and treatment of pruritus, we studied 8621 patients enrolled at the start of the DOPPS phase 5 (i.e., 2012–2015); 6256 (73%) indicated how much they were bothered by itchy skin.
During the second year of the DOPPS phase 5 (i.e., 2013), additional questions were asked of patients in 17 countries (excluding Australia, China, France, and New Zealand) about the effect of itchy skin. Of 5884 patients who returned their questionnaires, 5436 patients indicated whether they were bothered by itchy skin, and 4219 patients (in 278 facilities) responded to at least one of the eight additional questions; 268 medical directors of 337 participating study sites in these 17 countries completed a survey about their treatment practices for patients with pruritus. The majority of nonresponders (41 of 69) were in the United States.
Demographic data, comorbid conditions, laboratory values, and medications were abstracted from patient records. In the DOPPS phase 5, medication lists were ascertained at study entry and updated during study follow-up. Patient self-reported health measures were collected through questionnaires provided at enrolment and annually thereafter.
Definitions
In each DOPPS phase from 1996 to 2015, patients indicated how much they were bothered by itchy skin by responding to the question: “During the past 4 weeks, to what extent were you bothered by: itchy skin?” Response options were (1) not at all bothered, (2) somewhat bothered, (3) moderately bothered, (4) very much bothered, and (5) extremely bothered. In the second year of the DOPPS phase 5 (2013–2014), a section about the effect of itch on patients’ lives was added to the survey, including questions on feelings of depression and embarrassment and the effect on work and social interactions, from the Skindex-10 (20). All questions in this section were worded as follows: “During the past week, how often have you been bothered by,” with responses ranging from zero (never) to six (always) on a seven-point Likert scale. Scores of five or six were interpreted as being “nearly always or always” bothered.
In 2013, medical directors were asked to estimate the prevalence of pruritus among their patients and describe their typical treatment practices. Questions asked whether the following medications were for first-, second-, or third-line chronic use therapy, for acute use, or never prescribed for pruritus: intravenous corticosteroids, gabapentin, antidepressants, antianxiolytics/sedatives, or opioids for patients who are not referred to a specialist. Patient medications were checked for prescriptions of gabapentin, pregabalin, or nalfurafine during the entire DOPPS phase 5 study period (2012–2015). The timing of prescription was not linked to the timing of the patient survey.
Data Analyses
Associations of patient characteristics presented in Supplemental Table 1 were tested in adjusted multivariate logistic regression with odds of being at least moderately bothered by itching. Models were adjusted for age, sex, dialysis vintage, 13 summary comorbidity measures (coronary artery disease, cancer, other cardiovascular disease, cerebrovascular disease, congestive heart failure, diabetes mellitus, gastrointestinal bleeding, hypertension, lung disease, neurologic disorder, psychological disorder, peripheral vascular disease, and recurrent cellulitis), and country and accounted for facility clustering for the DOPPS phase 5 enrolment cross-section sample. Data summary and analyses were conducted with SAS software, version 9.4 (SAS Institute, Cary, NC).
Results
Prevalence and Severity of Pruritus
The percentage of patients very much or extremely bothered by itchy skin declined between 1996 and 2015 from 28% to 18% (Figure 1). Similar results were seen in countries participating in all five DOPPS phases (data not shown).
In the DOPPS phase 5 (2012–2015), the percentage of patients at least moderately bothered by itchy skin ranged from 26% in Germany to 48% in the United Kingdom; 13% (Germany) to 26% (the United Kingdom) were very much or extremely bothered (Figure 2).
Figure 2.
The percentage of patients at least moderately bothered by itchy skin ranged from 26% in Germany to 48% in the United Kingdom in the DOPPS phase 5 (2012–2015). Results are ranked by the proportion of patients who were moderately to extremely bothered by itchy skin. Question wording: “To what extent were you bothered by itchy skin during the past 4 weeks?” In total, 96% of patients answered this question among patients who completed a patient questionnaire. ANZ, Australia and New Zealand; Bel, Belgium; Can, Canada; Chi, China; GCC, the six Gulf Cooperation Council countries (Bahrain, Qatar, Kuwait, Oman, Saudi Arabia, and United Arab Emirates); Ger, Germany; Ita, Italy; Jpn, Japan; Rus, Russia; Spa, Spain; Swe, Sweden; Tur, Turkey; UK, the United Kingdom; US, the United States.
In the DOPPS phase 5 cross-sectional sample, mean values or prevalence of nearly all patient characteristics were similar across the categories of pruritus severity (Table 1). Patients not responding to the questionnaire differed slightly in age and ferritin.
Table 1.
Patient characteristics according to the extent to which patients were bothered by itchy skin
| Variable | To What Extent Were You Bothered by Itchy Skin during the Past 4 wk? | |||||
|---|---|---|---|---|---|---|
| No Response | Not at All | Somewhat | Moderately | Very Much | Extremely | |
| Total sample, N | 2365 | 2111 | 1840 | 1188 | 692 | 425 |
| Total sample, % | 27 | 20 | 17 | 11 | 6 | 4 |
| Patient characteristics | ||||||
| Men | 60 | 60 | 59 | 60 | 60 | 59 |
| Age, yr | 66 (15) | 62 (15) | 62 (15) | 63 (15) | 63 (15) | 64 (15) |
| Time on dialysis, yr | 5.1 (5.6) | 5.4 (6.2) | 5.8 (6.2) | 5.3 (5.7) | 4.9 (5.4) | 5.1 (6) |
| BMI, kg/m2 | 26 (6) | 26 (6) | 25 (6) | 26 (7) | 26 (6) | 26 (7) |
| Treatment time, min | 231 (37) | 237 (34) | 237 (35) | 235 (32) | 232 (32) | 232 (29) |
| Hemodiafiltration,a % | 22 | 20 | 16 | 17 | 16 | 17 |
| Smokerb | 22 | 19 | 21 | 22 | 24 | 21 |
| Hepatitis B/C | 5 | 6 | 8 | 9 | 9 | 9 |
| Laboratory values | ||||||
| Hemoglobin, g/dl | 10.9 (1.4) | 11 (1.4) | 11 (1.4) | 11 (1.4) | 11 (1.4) | 10.9 (1.5) |
| Parathyroid hormone, pg/ml | 355 (379) | 355 (416) | 348 (449) | 346 (496) | 322 (345) | 349 (430) |
| White blood cell count | 6.9 (2.3) | 6.7 (2.1) | 6.7 (2.2) | 6.7 (2.2) | 6.8 (2.4) | 7 (2.5) |
| Albumin, g/dl | 3.7 (0.5) | 3.8 (0.5) | 3.7 (0.5) | 3.7 (0.5) | 3.7 (0.5) | 3.7 (0.5) |
| Ferritin, ng/ml | 486 [228–806] | 410 [159–754] | 344 [105–672] | 394 [156–715] | 382 [155–680] | 401 [141–704] |
| Calcium, mg/dl | 8.9 (0.8) | 8.9 (0.8) | 8.9 (0.8) | 8.9 (0.8) | 8.9 (0.8) | 8.9 (0.8) |
| Phosphorus, mg/dl | 4.9 [4–5.9] | 4.9 [4.1–5.9] | 5.1 [4.2–6.0] | 5 [4–5.9] | 5 [4.1–6] | 5 [4.1–6.1] |
| Calcium × phosphorus product, mg2/dl2 | 43 (35, 53) | 43 (36, 52) | 45 (36, 55) | 44 (35, 52) | 44 (36, 53) | 44 (36, 54) |
| Single-pool Kt/V | 1.5 (0.3) | 1.5 (0.3) | 1.5 (0.3) | 1.5 (0.3) | 1.5 (0.3) | 1.5 (0.3) |
| CRP, mg/Lc | 4.7 [1.5–13.2] | 3 [1–8] | 2.7 [1–7] | 4 [1–9.7] | 4 [1–10.5] | 5.3 [1.7–15.8] |
| Patient-reported measures, % | ||||||
| Bothered by dry skind | 14 | 21 | 68 | 81 | 87 | |
| Have restless sleepe | 29 | 36 | 46 | 57 | 66 | |
Data are from patients enrolled at the start of the Dialysis Outcomes and Practice Patterns Study phase 5 (i.e., 2012–2015). Data are shown as mean (SD), median [interquartile range], or column percentage. Nonresponse rate was 27% overall, varying from 9% in Turkey to 46% in Canada. BMI, body mass index; CRP, C-reactive protein.
Hemodiafiltration excludes the United States and Canada due to lack of use (n=6024).
Smoker is defined as someone indicating being a current smoker or who stopped smoking within past year; this measure was missing for all patients from United States large dialysis organizations (n=5871).
CRP is restricted to facilities that reported measurement in at least 50% of patients (excludes the United States; n=2607).
Measure shows the percentage of patients who selected moderately, very much, or extremely bothered (versus not at all or somewhat) in response to the question on the Patient Questionnaire: “During the past 4 weeks, to what extent were you bothered by each of the following: dry skin?” (n=6152); this measure was missing for most “no response” patients, because they did not return the questionnaire.
Measure shows the percentage of patients who selected “3= Occasionally or a moderate amount of the time (3–4 days)” or “4= Most or all of the time (5–7 days)” versus “1= Rarely or none of the time (<1 day)” or “2= Some or little of the time (1–2 days)” in response to the question on the Patient Questionnaire: “During the past 4 weeks, my sleep was restless” (n=6025); this measure was missing for most “no response” patients, because they did not return the questionnaire.
Patients at least moderately bothered by itchy skin were slightly older and had a higher median C-reactive protein. Multivariable logistic regression analyses confirmed associations of older age and higher C-reactive protein with worse pruritus (Supplemental Table 1). Serum albumin was negatively associated with pruritus severity, and patients with hepatitis B or C were more likely to be bothered as found previously (2). However, no association was observed with serum phosphorus, calcium, calcium-phosphorus product, parathyroid hormone (PTH), Kt/V, and hemodiafiltration.
Symptom Burden Due to Pruritus
Patients very much or extremely bothered by itchy skin were also bothered by dry skin (84%), and 60% frequently had restless sleep (Table 1). Patients who were nearly always or always bothered by itching in the past week were much more often (1) bothered by the appearance of their skin; (2) frustrated, annoyed, and depressed by their itching; (3) bothered by the effects of itching on interactions or the desire to interact with others; and (4) bothered by itching so as to make it hard to work (Table 2).
Table 2.
Effects of pruritus on daily living in patients who were nearly always or always bothered by itchy skin
| Among Patients Nearly Always Bothered by Itchy Skin during the Past Week, Frequency of Being Bothered by | 0 (Never) | 1–3 | 4–6 (Always) |
|---|---|---|---|
| Being annoyed about your itching | 3 | 15 | 81 |
| Frustration about your itching | 6 | 17 | 77 |
| Appearance of your skin from scratching | 9 | 22 | 69 |
| Feeling depressed about your itching | 13 | 29 | 58 |
| Feeling embarrassed about your itching | 22 | 33 | 45 |
| Effect of itching making it hard to work | 23 | 33 | 45 |
| Effects of itching on desire to be with people | 32 | 33 | 35 |
| Effects of itching on interactions with others | 29 | 37 | 34 |
Data are from the second year of the Dialysis Outcomes and Practice Patterns Study phase 5 (i.e., 2013) in 17 countries. The table shows percentages of responses to questions among patients who said “yes” to “Are you bothered at all by itchy skin?” and selected five or six (“nearly always or always bothered”) on the zero to six scale in response to the question: “During the past week, how often have you been bothered by: your itching?” (n=1023); the number of responders to each question was within 6%.
Approximately one third of patients bothered by itchy skin were most bothered by itching at night, and nearly 50% were bothered either at all times throughout the day or not at any specific time (Supplemental Table 2). There was no relation of itching with the timing of the dialysis treatment for most patients (61%); however, 15% indicated that itching was worst during the dialysis session, 9% indicated that itching was worst soon after a session, and 14% indicated that itching was worst on nondialysis days.
Nephrologists’ Awareness of Pruritus
Overall, 65% of medical directors estimated that <5% of their patients suffered from severe pruritus. Medical directors underestimated the prevalence of pruritus in 69% of facilities. In the large fraction of facilities, where 21%–50% of patients reported having severe pruritus, only 1% of medical directors estimated the same prevalence of pruritus in their facility. Facilities with the lowest prevalence of patient-reported itching tended to have a higher medical director estimate of the prevalence of severe pruritus (Supplemental Figure 1).
Overall, patients bothered by itchy skin were most likely to report symptoms of itching to a nephrologist (42%) followed by a nurse or other dialysis staff member (32%), a dermatologist (18%), or a primary care doctor (16%; categories not exclusive). However, 17% of patients nearly always or always bothered by itchy skin had not reported their symptoms to any health care provider. This varied from 8% in Italy and 12% in the Gulf Cooperation Council countries to 21% in Sweden and 33% in the United States (Supplemental Table 3).
Treatment of Uremic Pruritus
Health Care Providers Treating Pruritus.
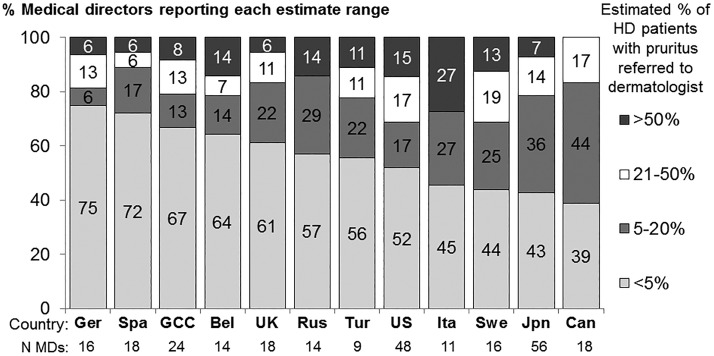
In Germany, pruritus treatment was largely determined by nephrologists, with the majority of medical directors referring <5% of patients (Figure 3). In the United States, Sweden, and Italy, approximately 30% of medical directors referred >20% of patients with pruritus to a dermatologist compared with 11%–14% of medical directors in Spain and Russia.
Figure 3.
There was wide variation between countries in the percentage of patients with pruritus referred to a skin specialist or dermatologist. Data are from 262 medical directors who returned their survey in 2013 (total n=337). Question text: “Among patients with pruritus, estimate the percent of patients you refer to a dermatologist or other specialist.” Bel, Belgium; Can, Canada; GCC, the six Gulf Cooperation Council countries (Bahrain, Qatar, Kuwait, Oman, Saudi Arabia, and United Arab Emirates); Ger, Germany; HD, hemodialysis; Ita, Italy; Jpn, Japan; Rus, Russia; Spa, Spain; Swe, Sweden; Tur, Turkey; UK, the United Kingdom; US, the United States.
Overall, a little over one half of patients reported that treatments were most often prescribed by a nephrologist; prescription by other health care providers ranged from 19% by a primary care doctor to 24% by a dermatologist. Percentages were similar for patients who were nearly always or always bothered by itchy skin (Supplemental Table 4).
Therapeutic Options for Severe Pruritus.
Medical directors ranked five therapeutic options for patients with severe pruritus in order of importance (Supplemental Table 5). Phosphorus control in patients with high serum phosphorus was ranked as most important in every DOPPS country and overall by 60% of medical directors. Increasing dialysis dose in patients with low Kt/V, increasing prescribed treatment time in patients with short treatment time, and lowering PTH levels in patients with high PTH were ranked second to fourth. Use of prescription medications for pruritus was ranked as least important by 45% of medical directors.
Use of Medication for Pruritus.
Sixty-eight percent of patients nearly always or always bothered by itchy skin reported using topical treatments, 28% used oral medications, and 18% reported taking no treatment to relieve their itching. The latter varied from 8% in Japan and 9% in the Gulf Cooperation Council countries to 29% in the United States and 45% in Russia (Supplemental Table 6). Ultraviolet light therapy was rarely used.
In patients with pruritus not referred to a skin specialist, antihistamines were most commonly used in all countries (Supplemental Table 7). Overall, 57% of medical directors used oral antihistamines (prescription or over the counter), and 23% used topical antihistamines as first-line chronic treatment of pruritus; 9% reported using topical corticosteroids as first-line treatment.
Gabapentin was used as first-line treatment in some facilities in the Gulf Cooperation Council countries, the United States, the United Kingdom, and Germany (Supplemental Figure 2). All nephrologists in Germany and a majority in the United Kingdom and Turkey reported using gabapentin for chronic itching as first-, second-, or third-line therapy. In all other countries, the majority of nephrologists never used gabapentin, ranging from 100% in Japan and Russia to 55% in the United States.
Patient-level data indicated that, among all patients bothered by itching, 7% were prescribed gabapentin, 4% were prescribed pregabalin, 5% were prescribed nalfurafine, and 85% were prescribed none of these agents during the DOPPS phase 5 follow-up. Overall, gabapentin prescription, for any indication, varied from 0% in Japan and Russia to 21% in the United States during the DOPPS phase 5 follow-up. Pregabalin was only prescribed, for any indication, in the United Kingdom, Germany, Canada, and Spain. Nalfurafine was only used in Japan, where 15% of patients bothered by itchy skin were prescribed nalfurafine.
Discussion
Pruritus continues to be common among people on HD, although there has been a decline in prevalence of severe pruritus over the last 20 years. Although mild pruritus may be a nuisance, severe pruritus has a major negative effect on patients’ lives. They are often bothered by the dryness and appearance of their skin, and they are frustrated, annoyed, and depressed by their itching, which have major effects on their social and working lives. The majority also suffers restless sleep, which is associated with depression and increased mortality (2).
Nephrologists in all DOPPS countries underestimated the prevalence of itching in their patients. Although reporting bias may have affected medical directors’ estimates, these findings extend previous reports (3–5). Medical directors may have interpreted the prevalence of pruritus to refer to the percentage of patients with either a diagnosis of pruritus or with currently severe itching, the latter being a lower figure if pruritus is treated effectively. Facilities with the lowest prevalence of patient-reported itching tended to have a higher medical director estimate of the prevalence of severe pruritus, suggesting that those more aware of pruritus were more likely to give effective treatment.
Many patients did not report symptoms of itching to clinicians. Even among those who were nearly always or always bothered by itchy skin, 17% had not reported their symptoms to any health care provider. Studies in renal (4) and nonrenal populations (21) suggest that reporting of itch may rely on patients’ resilience to symptoms, language ability, available time, opportunity during the consultation, and whether they expect health professionals to accept itch as a problem. This emphasizes the need for the renal team to inquire routinely about itching rather than to wait for patients to volunteer this symptom. Systematic use of tools that collect subjective and objective patient-generated data on pruritus (22) may prompt and inform discussions about itch and support treatment decisions.
Wide variation between countries was found in the percentage of patients with pruritus referred to a skin specialist. In a recent German study, 19% of patients on HD with chronic itch primarily had diseased skin, and such patients may benefit from a specialist evaluation (23).
The treatment ranked most important by a large majority of nephrologists was dietary counseling and/or a change in the phosphate binder regimen. This suggests most nephrologists believe that high serum phosphorus is a major cause of pruritus. In earlier DOPPS data, Pisoni et al. (2) showed strong associations between the likelihood of being moderately, very much, or extremely bothered by itchy skin and having a serum phosphorus ≥5.5 mg/dl (1.8 mmol/L) or an increased calcium/phosphorus product. However, large differences in the odds of patients having pruritus remained after extensive covariate adjustment, indicating that serum phosphorus and calcium/phosphorus product did not explain a large proportion of pruritus.
Furthermore, an association between these measures and pruritus is no longer observed in the 2012–2015 data, a finding supported by other recent studies (11,20,24). There is no published interventional study showing that lowering serum phosphorus improves pruritus. Emphasizing restriction of phosphate intake in patients with pruritus may lead to inadequate nutrition and inappropriately burden patients with responsibility for their own symptoms (Supplemental Movie 1).
The intervention ranked next most important was increasing dialysis dose (Kt/V). In a study from 1995, increasing Kt/V from a mean of 1.05 to 1.24 led to an improvement in pruritus (25). However, no association between Kt/V and pruritus was found in this study, where the mean Kt/V was 1.5, consistent with other recent studies (2,24).
Many nephrologists would change the vitamin D or cinacalcet regimen to lower an elevated serum PTH in patients with severe pruritus. The link between hyperparathyroidism and pruritus originates from early reports of improvement in itching after parathyroidectomy (26,27). However, many patients with severe pruritus do not have elevated PTH levels (11), and no association has been shown between pruritus and PTH in this study and other studies (2,20,24).
The finding that patients with more severe pruritus have lower serum albumin suggests an association between pruritus and malnutrition-inflammation complex syndrome. An association between pruritus and C-reactive protein was reported in two studies (28,29) as in this study. Another study showed an association between pruritus and IL-2 but not with C-reactive protein or other cytokines (30).
Use of prescription medications was ranked lowest out of the five treatment interventions. Topical treatments were the most commonly used medication and may be preferred by patients bothered by dry skin. Most nephrologists in all countries use antihistamines as first-line drug treatment. Treatment with the antihistamine ketotifen has been shown to reduce pruritus compared with conventional therapy (31), but in a comparative trial without a placebo arm, ketotifen was less effective than gabapentin (32). Another uncontrolled trial of ketotifen showed no effect on pruritus, and uncontrolled trials of hydroxyzine and chlorphenamine showed a partial effect or no effect (32). Plasma histamine levels are not associated with the severity of pruritus (33), and patients frequently report that antihistamines are ineffective (11,21,34). It has been suggested that antihistamines should be tried first, because they are unlikely to be harmful. However, the side effects of drowsiness and dizziness were found to be the same with ketotifen and hydroxyzine as with gabapentin (28). The lack of a consistent effect of antihistamines is consistent with the findings of functional magnetic resonance imaging brain imaging studies in patients on HD with pruritus that show normal responses evoked by histamine itch but abnormal responses evoked by cowhage itch (35).
Gabapentin and pregabalin have effects on pruritus, insomnia, and restless legs syndrome, possibly mediated by reducing the excessive resting brain activation shown on functional magnetic resonance imaging scans (35). Their use for pruritus is unlicensed and varies widely between countries. Nalfurafine, an oral κ-opioid receptor agonist, is currently only approved for use in Japan. It may have a direct effect on the brain and/or provide positive feedback from the skin at the level of the spinal cord. Its effect on itching in randomized trials was less than gabapentin, and its most common side effect is insomnia (14). There remains a need for a more robust evidence base for these and other agents, such as turmeric, montelukast, zinc sulfate, and nalbuphine (15–17,36).
The current model of clinical practice is failing to identify and treat many patients severely affected by itching. There is a major opportunity to improve the health and wellbeing of patients with CKD through increased awareness of pruritus and the greater use of effective treatments. This could be achieved by systematic efforts to (1) develop and implement treatment guidelines, (2) include pruritus monitoring and treatment in performance management schemes (37), and (3) routinely collect itch prevalence and severity data in registries.
This study has a number of limitations. The patient response rate was 73%. The medical director response rate was 80%, with 59% of nonresponders being in the United States. The prevalence of itch may be affected by reporting bias; patients who are bothered by itchy skin may be more or less likely to respond to the survey. Similarly, medical directors unaware of the true prevalence of pruritus may be more or less likely to respond. Cross-sectional associations between pruritus and patient characteristics do not imply causation, and we did not study the effect of characteristics over time on the development of pruritus.
Although there has been a reduction in the proportion of patients on HD affected by itching over the last 20 years, in 2012–2015, nearly one in five patients on HD was very much or extremely bothered by itching. Nephrologists substantially underestimate the number of patients affected by itching. Of patients who were nearly always or always bothered by itching, 17% did not report their symptoms to a health care professional, and 18% were not receiving treatment for their itching. Medical directors ranked phosphorus control and increasing Kt/V as the most important therapeutic options for patients with severe pruritus, but neither phosphorus nor Kt/V were associated with itching. There is wide variation in the use of gabapentin and pregabalin for the treatment of pruritus. There is a major opportunity to improve the health and wellbeing of patients on HD through increased awareness of pruritus and the greater use of effective treatments.
Disclosures
F.T. has received consulting fees from MedScape. B.M.R. has received lecture fees from Kyowa Hakko Kirin. The other authors have no disclosures to declare.
Supplementary Material
Acknowledgments
S.N.v.d.V. is supported by Health e-Research Centre Medical Research Council Research grant MR/K006665/1. The Dialysis Outcomes and Practice Patterns Study (DOPPS) Program is supported by Amgen, Kyowa Hakko Kirin, and Baxter Healthcare. Additional support for specific projects and countries is provided by Amgen, AstraZeneca, the European Renal Association-European Dialysis and Transplant Association, the German Society of Nephrology, Hexal AG, Janssen, the Japanese Society for Peritoneal Dialysis, Keryx, Proteon, Relypsa, Roche, the Società Italiana di Nefrologia, the Spanish Society of Nephrology, and Vifor Fresenius Medical Care Renal Pharma. Public funding and support provided for specific DOPPS projects, ancillary studies, or affiliated research projects are as follows: Australia: the National Health and Medical Research Council; Canada: the Canadian Institutes of Health Research and the Ontario Renal Network; France: Agence Nationale de la Recherche; Thailand: Thailand Research Foundation, the Chulalongkorn University Matching Fund, the King Chulalongkorn Memorial Hospital Matching Fund, and the National Research Council of Thailand; the United Kingdom: the National Institute for Health Research via the Comprehensive Clinical Research Network; and the United States: the National Institutes of Health and the Patient-Centered Outcomes Research Institute. All grants are made to Arbor Research Collaborative for Health and are not to coauthors directly.
All support is provided without restrictions on publications.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.09590916/-/DCSupplemental.
References
- 1.Abdel-Kader K, Unruh ML, Weisbord SD: Symptom burden, depression, and quality of life in chronic and end-stage kidney disease. Clin J Am Soc Nephrol 4: 1057–1064, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pisoni RL, Wikström B, Elder SJ, Akizawa T, Asano Y, Keen ML, Saran R, Mendelssohn DC, Young EW, Port FK: Pruritus in haemodialysis patients: International results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant 21: 3495–3505, 2006 [DOI] [PubMed] [Google Scholar]
- 3.Weisbord SD, Fried LF, Mor MK, Resnick AL, Unruh ML, Palevsky PM, Levenson DJ, Cooksey SH, Fine MJ, Kimmel PL, Arnold RM: Renal provider recognition of symptoms in patients on maintenance hemodialysis. Clin J Am Soc Nephrol 2: 960–967, 2007 [DOI] [PubMed] [Google Scholar]
- 4.Feldman R, Berman N, Reid MC, Roberts J, Shengelia R, Christianer K, Eiss B, Adelman RD: Improving symptom management in hemodialysis patients: Identifying barriers and future directions. J Palliat Med 16: 1528–1533, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weisshaar E, Matterne U, Mettang T: How do nephrologists in haemodialysis units consider the symptom of itch? Results of a survey in Germany. Nephrol Dial Transplant 24: 1328–1330, 2009 [DOI] [PubMed] [Google Scholar]
- 6.Manns B, Hemmelgarn B, Lillie E, Dip SC, Cyr A, Gladish M, Large C, Silverman H, Toth B, Wolfs W, Laupacis A: Setting research priorities for patients on or nearing dialysis. Clin J Am Soc Nephrol 9: 1813–1821, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weisshaar E, Szepietowski JC, Darsow U, Misery L, Wallengren J, Mettang T, Gieler U, Lotti T, Lambert J, Maisel P, Streit M, Greaves M, Tschachler E, Ring J, Ständer S; the European Dermatology Forum (EDF); the European Academy of Dermatology and Venereology (EADV): European Guideline on Chronic Pruritus, 2014 Available at: http://www.euroderm.org/edf/index.php/edf-guidelines/category/5-guidelines-miscellaneous. Accessed January 16, 2017
- 8.Lau T, Leung S, Lau W: Gabapentin for uremic pruritus in hemodialysis patients: A qualitative systematic review. Can J Kidney Health Dis 3: 14, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nofal E, Farag F, Nofal A, Eldesouky F, Alkot R, Abdelkhalik Z: Gabapentin: A promising therapy for uremic pruritus in hemodialysis patients: A randomized-controlled trial and review of literature. J Dermatolog Treat 27: 515–519, 2016 [DOI] [PubMed] [Google Scholar]
- 10.Yue J, Jiao S, Xiao Y, Ren W, Zhao T, Meng J: Comparison of pregabalin with ondansetron in treatment of uraemic pruritus in dialysis patients: A prospective, randomized, double-blind study. Int Urol Nephrol 47: 161–167, 2015 [DOI] [PubMed] [Google Scholar]
- 11.Rayner H, Baharani J, Smith S, Suresh V, Dasgupta I: Uraemic pruritus: Relief of itching by gabapentin and pregabalin. Nephron Clin Pract 122: 75–79, 2012 [DOI] [PubMed] [Google Scholar]
- 12.Xander C, Meerpohl JJ, Galandi D, Buroh S, Schwarzer G, Antes G, Becker G: Pharmacological interventions for pruritus in adult palliative care patients. Cochrane Database Syst Rev 6: CD008320, 2013 [DOI] [PubMed] [Google Scholar]
- 13.Wikström B, Gellert R, Ladefoged SD, Danda Y, Akai M, Ide K, Ogasawara M, Kawashima Y, Ueno K, Mori A, Ueno Y: Kappa-opioid system in uremic pruritus: Multicenter, randomized, double-blind, placebo-controlled clinical studies. J Am Soc Nephrol 16: 3742–3747, 2005 [DOI] [PubMed] [Google Scholar]
- 14.Kumagai H, Ebata T, Takamori K, Muramatsu T, Nakamoto H, Suzuki H: Effect of a novel κ-receptor agonist, nalfurafine hydrochloride, on severe itch in 337 haemodialysis patients: A Phase III, randomized, double-blind, placebo-controlled study. Nephrol Dial Transplant 25: 1251–1257, 2010 [DOI] [PubMed] [Google Scholar]
- 15.Pakfetrat M, Basiri F, Malekmakan L, Roozbeh J: Effects of turmeric on uremic pruritus in end stage renal disease patients: A double-blind randomized clinical trial. J Nephrol 27: 203–207, 2014 [DOI] [PubMed] [Google Scholar]
- 16.Nasrollahi AR, Miladipour A, Ghanei E, Yavari P, Haghverdi F: Montelukast for treatment of refractory pruritus in patients on hemodialysis. Iran J Kidney Dis 1: 73–77, 2007 [PubMed] [Google Scholar]
- 17.Najafabadi MM, Faghihi G, Emami A, Monghad M, Moeenzadeh F, Sharif N, Davarpanah Jazi AH: Zinc sulfate for relief of pruritus in patients on maintenance hemodialysis. Ther Apher Dial 16: 142–145, 2012 [DOI] [PubMed] [Google Scholar]
- 18.Young EW, Goodkin DA, Mapes DL, Port FK, Keen ML, Chen K, Maroni BL, Wolfe RA, Held PJ: The Dialysis Outcomes and Practice Patterns Study (DOPPS): An international hemodialysis study. Kidney Int 57[Suppl 74]: S74–S81, 2000 [Google Scholar]
- 19.Pisoni RL, Gillespie BW, Dickinson DM, Chen K, Kutner MH, Wolfe RA: The Dialysis Outcomes and Practice Patterns Study (DOPPS): Design, data elements, and methodology. Am J Kidney Dis 44[Suppl 2]: 7–15, 2004 [DOI] [PubMed] [Google Scholar]
- 20.Mathur VS, Lindberg J, Germain M, Block G, Tumlin J, Smith M, Grewal M, McGuire D; ITCH National Registry Investigators : A longitudinal study of uremic pruritus in hemodialysis patients. Clin J Am Soc Nephrol 5: 1410–1419, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bathe A, Weisshaar E, Matterne U: Chronic pruritus--more than a symptom: A qualitative investigation into patients’ subjective illness perceptions. J Adv Nurs 69: 316–326, 2013 [DOI] [PubMed] [Google Scholar]
- 22.Price A, Cohen DE: Assessment of pruritus in patients with psoriasis and atopic dermatitis: Subjective and objective tools. Dermatitis 25: 334–344, 2014 [DOI] [PubMed] [Google Scholar]
- 23.Hayani K, Weiss M, Weisshaar E: Clinical findings and provision of care in haemodialysis patients with chronic itch: New results from the german epidemiological haemodialysis itch study. Acta Derm Venereol 96: 361–366, 2016 [DOI] [PubMed] [Google Scholar]
- 24.Weisshaar E, Weiss M, Passlick-Deetjen J, Tschulena U, Maleki K, Mettang T: Laboratory and dialysis characteristics in hemodialysis patients suffering from chronic itch--results from a representative cross-sectional study. BMC Nephrol 16: 184, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hiroshige K, Kabashima N, Takasugi M, Kuroiwa A: Optimal dialysis improves uremic pruritus. Am J Kidney Dis 25: 413–419, 1995 [DOI] [PubMed] [Google Scholar]
- 26.Massry SG, Popovtzer MM, Coburn JW, Makoff DL, Maxwell MH, Kleeman CR: Intractable pruritus as a manifestation of secondary hyperparathyroidism in uremia. Disappearance of itching after subtotal parathyroidectomy. N Engl J Med 279: 697–700, 1968 [DOI] [PubMed] [Google Scholar]
- 27.Chou FF, Ho JC, Huang SC, Sheen-Chen SM: A study on pruritus after parathyroidectomy for secondary hyperparathyroidism. J Am Coll Surg 190: 65–70, 2000 [DOI] [PubMed] [Google Scholar]
- 28.Chen HY, Chiu YL, Hsu SP, Pai MF, Lai CF, Yang JY, Peng YS, Tsai TJ, Wu KD: Elevated C-reactive protein level in hemodialysis patients with moderate/severe uremic pruritus: A potential mediator of high overall mortality. QJM 103: 837–846, 2010 [DOI] [PubMed] [Google Scholar]
- 29.Malekmakan L, Malekmakan A, Sayadi M, Pakfetrat M, Sepaskhah M, Roozbeh J: Association of high-sensitive C-reactive protein and dialysis adequacy with uremic pruritus. Saudi J Kidney Dis Transpl 26: 890–895, 2015 [DOI] [PubMed] [Google Scholar]
- 30.Fallahzadeh MK, Roozbeh J, Geramizadeh B, Namazi MR: Interleukin-2 serum levels are elevated in patients with uremic pruritus: A novel finding with practical implications. Nephrol Dial Transplant 26: 3338–3344, 2011 [DOI] [PubMed] [Google Scholar]
- 31.Francos GC, Kauh YC, Gittlen SD, Schulman ES, Besarab A, Goyal S, Burke JF Jr: Elevated plasma histamine in chronic uremia. Effects of ketotifen on pruritus. Int J Dermatol 30: 884–889, 1991 [DOI] [PubMed] [Google Scholar]
- 32.Amirkhanlou S, Rashedi A, Taherian J, Hafezi AA, Parsaei S: Comparison of gabapentin and ketotifen in treatment of uremic pruritus in hemodialysis patients. Pak J Med Sci 32: 22–26, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mettang T, Fritz P, Weber J, Machleidt C, Hübel E, Kuhlmann U: Uremic pruritus in patients on hemodialysis or continuous ambulatory peritoneal dialysis (CAPD). The role of plasma histamine and skin mast cells. Clin Nephrol 34: 136–141, 1990 [PubMed] [Google Scholar]
- 34.Mettang T, Kremer AE: Uremic pruritus. Kidney Int 87: 685–691, 2015 [DOI] [PubMed] [Google Scholar]
- 35.Papoiu AD, Emerson NM, Patel TS, Kraft RA, Valdes-Rodriguez R, Nattkemper LA, Coghill RC, Yosipovitch G: Voxel-based morphometry and arterial spin labeling fMRI reveal neuropathic and neuroplastic features of brain processing of itch in end-stage renal disease. J Neurophysiol 112: 1729–1738, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hawi A, Alcorn H Jr, Berg J, Hines C, Hait H, Sciascia T: Pharmacokinetics of nalbuphine hydrochloride extended release tablets in hemodialysis patients with exploratory effect on pruritus. BMC Nephrol 16: 47, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van der Veer SN, van Biesen W, Couchoud C, Tomson CR, Jager KJ: Measuring the quality of renal care: Things to keep in mind when selecting and using quality indicators. Nephrol Dial Transplant 29: 1460–1467, 2014 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.