Abstract
Background and objectives
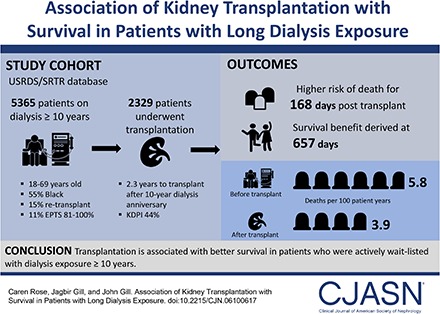
Evidence that kidney transplantation is associated with better survival compared to dialysis stems from data in populations with short durations of dialysis exposure. Recent changes in allocation policy increase access to transplantation for patients with longer dialysis exposure. The objective of this study was to determine the association of transplantation with survival in patients with ≥10 years of dialysis treatment.
Design, setting, participants, & measurements
Our study of n=5365 patients in the Scientific Registry of Transplant Recipients determined the adjusted relative risk of death in recipients of a deceased donor kidney transplant after ≥10 years of dialysis treatment compared with waitlisted patients with the same dialysis exposure in a time-dependent nonproportional hazards analysis.
Results
The adjusted relative risk of death in n=2320 transplant recipients compared with patients on dialysis who had equal lengths of follow-up from their 10-year dialysis anniversary was 0.60 (95% confidence interval, 0.53 to 0.68), and this benefit was observed in a variety of patient subgroups, including patients ≥65 years of age and patients with diabetes. However, transplant recipients were at higher risk of death for 180 days after transplantation and did not derive survival benefit until 657 days after transplantation, despite receiving good-quality kidneys. The study patients were younger and had higher expected post-transplant survival than patients currently waitlisted with ≥10 years of dialysis.
Conclusions
Transplantation is associated with better survival in patients who were actively waitlisted with dialysis exposure ≥10 years. Whether transplantation is associated with better survival in currently waitlisted patients with similar dialysis exposure and whether transplantation of lower-quality deceased donor kidneys is associated with better survival are uncertain.
Keywords: cadaver organ transplantation, survival, kidney transplantation, Risk, Transplant Recipients, Confidence Intervals, Follow-Up Studies, Graft Survival, Tissue Donors, kidney, Registries, diabetes mellitus, Humans, renal dialysis
Introduction
Kidney transplantation is the preferred treatment for patients with ESRD, because it is associated with better survival, better quality of life, and lower use of health care resources compared with treatment with dialysis (1–3). The better survival associated with kidney transplantation compared with treatment with dialysis extends to patients of advanced age and patients with comorbid disease conditions, such as diabetes and cardiovascular disease, leading to an increased need for this treatment that has outpaced increases in the availability of deceased donor kidneys (1,4). The resulting discrepancy between the need and supply of transplantable kidneys remains the dominant issue in kidney transplantation, with the recent national data showing a threefold increase in the number of patients removed from the waiting list because of deteriorating health status between 2010 and 2015 (5). Currently, 13% of the nearly 10,000 waitlisted kidney transplant candidates in the United States have had ESRD for >11 years (5).
Patients with prolonged exposure to dialysis before transplantation are known to have inferior post-transplant outcomes (6–8). However, most of the information regarding the association of kidney transplantation with better survival is derived from studies during an era in which patients received transplants relatively rapidly, typically within the first few years after the development of ESRD (1,4). Therefore, whether patients in the current era who receive transplants after prolonged treatment with dialysis continue to derive a similar survival benefit remains uncertain.
Recent changes to the kidney allocation system (KAS) have increased access to transplantation for patients with longer durations of pretransplant dialysis exposure. Specifically, in the new KAS, waiting time among patients not waitlisted before the initiation of dialysis is now calculated from the date of first chronic dialysis treatment rather than the date of waitlist activation (9). This policy change presents an opportunity to consider the option of transplantation in patients who have not accessed transplantation and have been treated with dialysis for prolonged periods of time. If referred and waitlisted for transplantation, these patients would be backdated to their initial dialysis start date, and many would rapidly receive deceased donor transplants ahead of currently waitlisted patients with shorter durations of dialysis treatment (10). We hypothesized that transplantation may not be associated with better survival in patients who have prolonged exposure to dialysis because of a survivor effect and the fact that longer pretransplant dialysis exposure is associated with a higher increased risk of allograft failure (6–8). Accordingly, we undertook this study to determine the association of deceased donor kidney transplantation with survival in a cohort of patients with prolonged dialysis exposure defined as ≥10 years.
Materials and Methods
Our local hospital research ethics board approved this study. The clinical and research activities being reported are consistent with the principles of the Declaration of Istanbul as outlined in the Declaration of Istanbul on Organ Trafficking and Transplant Tourism.
Data Source and Study Population
Data from the US Renal Data System (USRDS) and the Scientific Registry of Transplant Recipients (SRTR) were used for this analysis. The SRTR data system includes data on all donors, waitlisted candidates, and transplant recipients in the United States submitted by the members of the Organ Procurement and Transplantation Network (OPTN). The Health Resources and Services Administration, US Department of Health and Human Services provides oversight of the activities of the OPTN and the SRTR contractors.
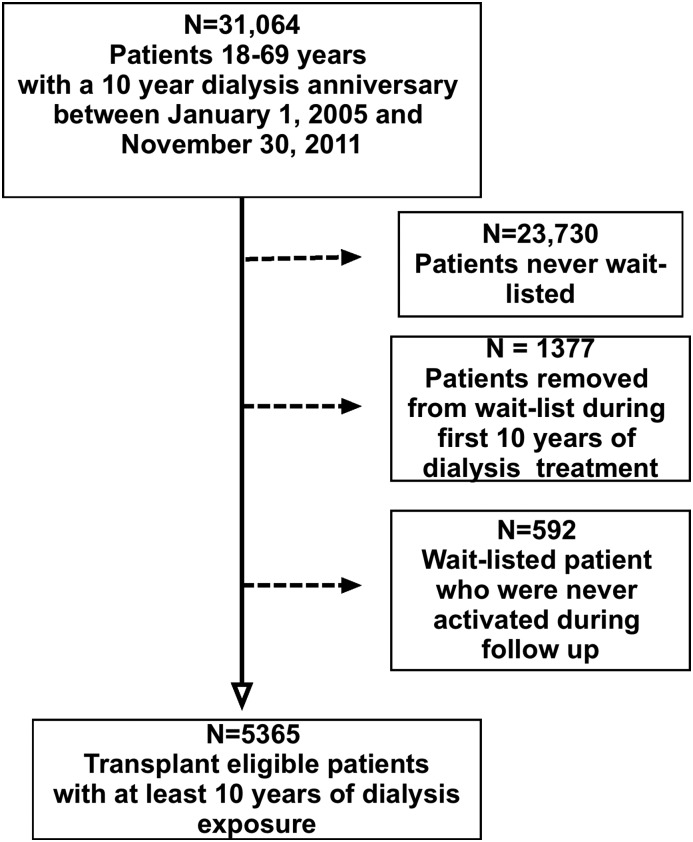
The study population included patients with ESRD (≥18 years old) with a 10-year dialysis anniversary between January 1, 2005 and November 30, 2011. This time period was chosen to allow for a minimum of 5 years of potential follow-up after the 10-year dialysis anniversary in all patients (the last date of follow-up in study data files was November 30, 2016). The final study cohort of 5365 patients was identified after excluding patients ≥70 years of age, in whom transplantation remains infrequent, patients who were never waitlisted before their 10-year dialysis anniversary or during study follow-up, waitlisted patients who were permanently removed from the waiting list before their 10-year dialysis anniversary, and patients who were waitlisted in inactive status but never activated to the waiting list before the end of study follow-up (November 30, 2016) as shown in Figure 1.
Figure 1.
Flow chart describing the identification of the study cohort.
Statistical Methods
Characteristics of study patients were described using the median and quartiles for continuous variables or frequencies and proportions for categorical variables. The characteristics of study patients were compared with those of waitlisted patients with ≥10 years of dialysis exposure on November 30, 2016 (the most recent waitlist data in our SRTR files) using the chi-squared and Kruskal–Wallis test as appropriate. The expected post-transplant survival (EPTS) of study patients was calculated at the time of the 10-year dialysis anniversary in study patients and comparator patients currently waitlisted. The EPTS score is calculated using four variables (age, prior organ transplant, diabetic status, and dialysis time), and the scores range from 0% to 100% (11). The score represents the percentage of transplant candidates in the reference population (all adult patients on the waiting list on December 31, 2015) with a higher post-transplant survival. Therefore, lower scores are associated with a higher EPTS. The kidney donor profile index (KDPI) was determined by calculating the ten-variable Kidney Donor Risk Index. Cutpoints for KDPI quartiles were based on the standardized 2015 Kidney Donor Risk Index values of deceased kidney donors recovered for transplantation (12).
Survival Analyses
Patients were followed from the date of their 10-year dialysis anniversary to the date of death or end of study follow-up, with follow-up censored at the time of transplantation from a living donor. The primary analysis was designed as intention to treat and did not censor patients in the event of removal from the waiting list or allograft failure. A secondary analysis, censored patients at the time of waitlist removal. The cumulative 5-year patient survival from the date of the 10-year dialysis anniversary was determined using the Kaplan–Meier method. Death rates per 100 patient-years were determined during dialysis treatment and after transplantation in all patients and subgroups defined by EPTS determined on each patient’s 10-year dialysis anniversary. The primary study outcome was the relative risk of death in recipients of a deceased donor transplant compared with waitlisted patients with the same duration of dialysis treatment who remained on the waiting list. The primary outcome was determined using a nonproportional hazards model. The model treated deceased donor transplantation as a time-dependent covariate to account for the fact that patients switched from dialysis to transplantation at different times during follow-up. We calculated the number of days remaining on dialysis until equal death rates were observed between patients who did and did not receive a transplant as well as the number of days until both groups had equal survival as previously described (1,4,13). Survival models were adjusted for variables commonly associated with survival in waitlisted patients and available in the SRTR dataset: patient age on their 10-year dialysis anniversary, sex, race, cause of ESRD, body mass index, comorbid conditions recorded at the time of waitlisting, peak panel reactive antibody, and year of first chronic dialysis treatment. The association of deceased donor transplantation with long-term survival was determined in subgroups defined by age, sex, race, diabetes, panel reactive antibody, and EPTS.
Variables with missing data were assigned a category of missing to allow inclusion of all patients in the models.
Finally, to inform the potential implications of study findings, a cross-sectional analysis was performed by cause of ESRD to determine the number and characteristics of patients ages 18–69 years old who had never received a transplant and were never waitlisted despite ≥10 years of continuous dialysis treatment on September 9, 2015 (the latest date included in our USRDS data files).
All analyses were performed in SAS 9.4 (SAS, Cary, NC).
Results
The study cohort included n=5365 adult patients on dialysis activated to the deceased donor transplant waiting list before (n=1038) or after (n=4327) their 10-year dialysis anniversary (Figure 1). Among patients waitlisted before their 10-year dialysis anniversary, the median (Q1-Q3) time to waitlist activation was 7.2 (5.1–8.8) years. Among patients waitlisted after their 10-year dialysis anniversary, the median (Q1,Q3) time to waitlist activation was 12.6 (11.1–14.6) years after the date of first dialysis treatment. Study patients were younger, were less likely to have diabetes as the cause of ESRD were less obese, and had greater EPTS than contemporary waitlisted patients with the same duration of pretransplant dialysis exposure (Table 1). Study patients were also less likely to have a previous transplant and had lower panel reactive antibodies. Study patients had lower median household incomes, were more likely to be of nonwhite race, and were more likely to have Medicare insurance than contemporary waitlisted patients with the same duration of pretransplant dialysis exposure (Table 1). During the median (Q1,Q3) follow-up of 6.5 (5.0–8.5) years, n=2320 study patients received a deceased donor kidney transplant (the median [Q1–Q3] time to transplantation was 2.3 [0.91–4.24] years after the 10-year dialysis anniversary date). The median (Q1–Q3) KDPI of the kidneys transplanted was 44% (25–65), and only 6% of kidneys had a KDPI>85%. There were n=1815 (34%) total deaths, and the 5-year cumulative survival probability of the study cohort was 78%. Table 2 shows the death rate per 100 patient-years during treatment with dialysis and after transplantation. Among dialysis-treated patients, the death rate increased with increasing durations of dialysis treatment after the 10-year dialysis anniversary. In contrast, the death rate was highest in the first year after transplantation and then decreased with increasing time after transplantation. The overall death rates before and after transplantation varied by EPTS, but patients in all EPTS groups had lower death rates after transplantation.
Table 1.
Characteristics of study patients and waitlisted patients on the deceased donor kidney transplant waiting list as of November 30, 2016
| Characteristic | n=5365 Study Patients | n=3112a Waitlisted Patients with ≥10 yr of Dialysis Exposure on November 30, 2016 | P Value |
|---|---|---|---|
| Duration of dialysis exposure, yr | |||
| Median (Q1–Q3) | 12.6 (11.1–14.6)b | 11.8 (10.7–13.6) | <0.001 |
| Age at 10-yr anniversary, yr | |||
| Median (Q1,Q3) | 48 (40–57) | 53 (43–60) | <0.001 |
| Age categories, yr | |||
| 18–39 | 25 | 15 | <0.001 |
| 40–49 | 30 | 27 | |
| 50–59 | 28 | 34 | |
| 60–64 | 11 | 14 | |
| 65–69 | 6 | 10 | |
| Women | 46 | 46 | 0.51 |
| Race | |||
| White non-Hispanic | 20 | 19 | 0.001 |
| White Hispanic | 17 | 21 | |
| Black | 55 | 52 | |
| Other | 8 | 8 | |
| Cause of kidney disease | |||
| Diabetes | 13 | 19 | <0.001 |
| Glomerular | 19 | 24 | |
| Hypertension | 33 | 32 | |
| Polycystic | 4 | 4 | |
| Other | 31 | 21 | |
| Body mass index, kg/m2 | |||
| <25 | 39 | 32 | <0.001 |
| 25–29.9 | 30 | 29 | |
| 30–34.9 | 19 | 19 | |
| ≥35 | 12 | 20 | |
| Comorbid conditions | |||
| Angina | 4 | 3 | 0.07 |
| Cerebrovascular disease | 2 | 3 | 0.19 |
| Peripheral vascular disease | 4 | 4 | 0.10 |
| Cancer | 4 | 3 | 0.07 |
| ABO blood group | |||
| A | 25 | 23 | 0.07 |
| B | 18 | 20 | |
| AB | 3 | 2 | |
| O | 54 | 55 | |
| Peak PRA % | |||
| 0 | 27 | 19 | <0.001 |
| 1–29 | 19 | 11 | |
| 30–79 | 13 | 10 | |
| 80–89 | 4 | 3 | |
| 90–94 | 3 | 2 | |
| 95–97 | 4 | 4 | |
| 98 | 2 | 3 | |
| 99 | 15 | 26 | |
| 100 | 13 | 22 | |
| OPTN region | |||
| 1 | 3 | 4 | <0.001 |
| 2 | 10 | 11 | |
| 3 | 18 | 20 | |
| 4 | 11 | 11 | |
| 5 | 19 | 21 | |
| 6 | 2 | 2 | |
| 7 | 7 | 8 | |
| 8 | 4 | 3 | |
| 9 | 9 | 8 | |
| 10 | 7 | 5 | |
| 11 | 10 | 9 | |
| Median household income (Q1–Q3) | $42,891 ($33,193–$57,003) | $44,714 ($34,252–$59,633) | <0.001 |
| Insurance | |||
| Private | 15 | 21 | <0.001 |
| Medicare | 72 | 63 | |
| Medicaid | 11 | 13 | |
| Other | 2 | 3 | |
| Education | <0.001 | ||
| Less than high school | 50 | 55 | |
| Postsecondary | 29 | 33 | |
| Unknown | 21 | 12 | |
| Previous transplant | 15 | 25 | <0.001 |
| Expected post-transplant survival, % | |||
| 1–20 | 26 | 11 | <0.001 |
| 21–40 | 31 | 26 | |
| 41–60 | 18 | 20 | |
| 61–80 | 14 | 22 | |
| 81–100 | 11 | 21 |
Income could not be calculated in 8% of the study patients and 7% of current waitlisted patients. Body mass index is missing in 2% of study patients and 2% of current waitlisted patients. Percentages are shown unless otherwise indicated. Q1,Q3, first and third quartile; PRA, panel reactive antibody; OPTN, Organ Procurement and Transplantation Network.
Excludes n=562 study patients who were on the waiting list on November 30, 2016.
Duration of dialysis exposure before waitlisting (years). Patients waitlisted before the start of dialysis treatment were assigned a value of zero.
Table 2.
Death rates (per 100 patient-years) before and after transplantation
| Patient Subgroup | On Dialysis | After Transplantation |
|---|---|---|
| All patients | ||
| Overalla | 5.8 | 3.9 |
| First yearb | 3.5 | 5.9 |
| Second year | 5.8 | 3.3 |
| Greater than or equal to third year | 6.6 | 3.6 |
| Overall death rates before and after transplantation in subgroups defined by EPTS,c % | ||
| EPTS | 3.3 | 1.7 |
| 1–20 | 4.7 | 2.8 |
| 21–40 | 6.4 | 4.9 |
| 41–60 | 9.1 | 6.7 |
| 61–80 | 13.4 | 11.0 |
| 81–100 |
EPTS, expected post-transplant survival.
Per 100 patient-years.
First year refers to the 11th year in dialysis-treated patients and the first post-transplant year in those who received a transplant. Similarly, second year refers to the 12th year in dialysis-treated patients and the second post-transplant year in those who received a transplant. Third year refers to the 13th year in dialysis-treated patients and the third post-transplant year in those who received a transplant.
EPTS was calculated at time of the 10-year dialysis anniversary.
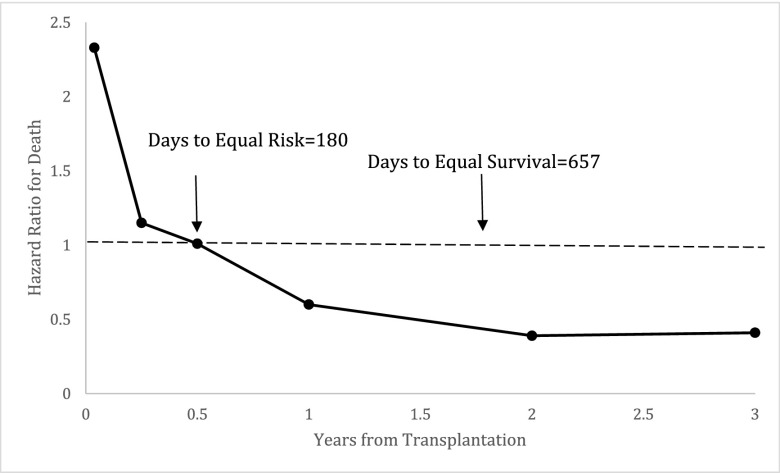
Figure 2 shows the adjusted relative risk of death among patients who received a first deceased donor kidney transplant compared with patients with equivalent durations of dialysis treatment. Deceased donor transplant recipients were at higher risk of death for a period of 180 days after the date of transplant surgery and then had lower risk of death. Because of this higher risk of death early after transplantation, survival between transplant recipients and patients who continued treatment with dialysis did not equalize until 657 days after transplantation.
Figure 2.
Deceased donor transplant recipients were at higher risk of death for a period of 180 days after the date of transplant surgery and then, had a lower risk of death. Because of this higher risk of death early after transplantation, survival between transplant recipients and patients who conitnued treatment with dialysis duid not equalize until 657 days after transplantation. The figure shows the adjusted relative risk of death in n=2320 kidney transplant recipients compared with waitlisted patients who had the same duration of dialysis treatment. The reference group (relative risk, 1.0) included the n=5365 waitlisted patients with at least 10 years of dialysis exposure. Patients in both groups had the same length of follow-up from the date of their 10-year dialysis anniversary. Values were adjusted for differences in patient age, sex, race, cause of kidney failure, body mass index, comorbid conditions, sensitization, and year of first chronic dialysis treatment.
Table 3 shows that transplant recipients had a 40% lower long-term risk of death compared with patients who continued dialysis (hazard ratio, 0.60; 95% confidence interval, 0.53 to 0.68) after adjustment for differences in patient age, sex, race, cause of kidney disease, body mass index in kilograms per meter2, comorbid conditions, sensitization, and year of first chronic dialysis treatment. Transplantation was consistently associated with lower risk of death compared with treatment with dialysis in subgroups defined by age, sex, race, cause of ESRD, sensitization to HLA antigens, and EPTS (Table 3). In a secondary analysis, in which patient follow-up was censored at the time of removal from the waiting list, transplantation was still associated with lower risk of death (hazard ratio, 0.75; 95% confidence interval, 0.66 to 0.86).
Table 3.
Subgroup analyses: Adjusted risk of death in transplant recipients compared with patients who remained on dialysis
| Subgroup | Hazard Ratio for Transplant within Subgroup (95% CI) |
|---|---|
| All patients | 0.60 (0.53 to 0.68) |
| Age, yr | |
| <40 | 0.44 (0.32 to 0.61) |
| 40–49 | 0.49 (0.38 to 0.63) |
| 50–59 | 0.49 (0.39 to 0.61) |
| 60–64 | 0.52 (0.38 to 0.70) |
| 65–69 | 0.60 (0.40 to 0.91) |
| Women | 0.38 (0.31 to 0.46) |
| Men | 0.58 (0.50 to 0.68) |
| Race | |
| White non-Hispanic | 0.51 (0.39 to 0.67) |
| White Hispanic | 0.46 (0.34 to 0.62) |
| Black | 0.46 (0.34 to 0.63) |
| Diabetes as cause of kidney failure | 0.73 (0.58 to 0.93) |
| Other causes | 0.56 (0.49 to 0.65) |
| Panel reactive antibody, % | |
| 0 | 0.61 (0.49 to 0.75) |
| 1–79 | 0.60 (0.49 to 0.72) |
| 80–89 | 0.74 (0.42 to 1.32) |
| 90–98 | 0.96 (0.60 to 1.52) |
| 99–100 | 0.60 (0.53 to 0.68) |
| Expected post-transplant survival, % | |
| 1–20 | 0.49 (0.35 to 0.67) |
| 21–40 | 0.51 (0.39 to 0.65) |
| 41–60 | 0.69 (0.53 to 0.90) |
| 61–80 | 0.60 (0.46 to 0.78) |
| 81–100 | 0.75 (0.58 to 0.97) |
Multivariate model adjusted for differences in patient age, sex, race, cause of kidney disease, body mass index in kilograms per meter2, comorbid conditions, sensitization, and year of first chronic dialysis treatment. 95% CI, 95% confidence interval.
There were n=22,169 patients (including 64% under the age of 60 years old and 27% with diabetes as the cause of ESRD) recorded in the USRDS data files who had never been waitlisted or received a transplant despite ≥10 years of dialysis treatment who may be eligible for deceased donor kidney transplantation as of September 9, 2015 (Table 4). Patients with diabetes as the cause of ESRD were older, were more likely to be men and white non-Hispanic, and had more comorbidities than patients with other causes of ESRD.
Table 4.
Characteristics of adult patients ages 18–69 years old with ≥10 years of dialysis exposure who have never been waitlisted and never received a transplant (n=22,169)
| Characteristic | All Patients,a n=22,169 | Patients with Diabetes as Cause of ESRD, n=6067 | Patients with Other Cause of ESRD, n=16,102 | P Value |
|---|---|---|---|---|
| Age at time of 10-yr dialysis anniversary, yr | ||||
| Median (quartile 1, quartile 3) | 56 (47, 63) | 61 (55, 66) | 53 (45, 61) | <0.001 |
| 18–39 | 12 | 3 | 16 | <0.001 |
| 40–49 | 20 | 10 | 24 | |
| 50–59 | 32 | 31 | 32 | |
| 60–64 | 18 | 26 | 15 | |
| 65–70 | 18 | 30 | 13 | |
| Women | 43 | 51 | 40 | <0.001 |
| Race | ||||
| White non-Hispanic | 25 | 19 | 10 | <0.001 |
| White Hispanic | 13 | 19 | 27 | |
| Black | 50 | 47 | 51 | |
| Other | 12 | 15 | 12 | |
| Comorbid conditionsb | 7 | |||
| Ischemic heart disease | 7 | 13 | 4 | <0.001 |
| Cerebrovascular disease | 4 | 6 | 3 | <0.001 |
| Peripheral Vascular disease | 5 | 12 | 2 | <0.001 |
| Cancer | 2 | 1 | 3 | <0.001 |
Percentages are shown unless otherwise indicated.
Cross-sectional analysis of data captured in the US Renal Data System on September 9, 2015.
Comorbid conditions determined from the Medevid Form recorded at the start of first dialysis treatment.
Discussion
Given the scarcity of transplantable kidneys, examination of the rationale for considering different patient subgroups for transplantation is a relevant clinical and policy issue. Improving the survival of patients with ESRD is the most compelling reason to treat patients with kidney transplantation rather than dialysis (2). Prolonged exposure to dialysis is associated with lower patient and allograft survival (6–8), and to our knowledge, previous work has not documented the survival benefit of transplantation in patients with prolonged dialysis exposure ≥3 years who are increasingly encountered in current clinical practice due to the long-standing shortage of suitable deceased donor kidneys for transplantation (4). The relevance of this analysis is highlighted by the fact that there are n=3112 patients with similar duration of dialysis exposure currently waitlisted for transplantation as well as a potential group of over 22,000 patients on dialysis ages 18–69 years old with ≥10 years of dialysis exposure who have never been waitlisted and could rapidly receive a deceased donor transplant if referred and found suitable for waitlisting under the new KAS (10).
The finding that transplantation was associated with a substantially better survival among patients with ≥10 years of dialysis exposure was surprising. We hypothesized that transplantation may not be associated with better survival in such patients because of a survivor effect and because pretransplant dialysis exposure is associated with inferior post-transplant allograft survival (6–8). The association of transplantation with better survival was preserved in subgroups of patients, including those with diabetes as the cause of ESRD, those of older age, and patients sensitized to human leukocyte antigens. Compared with the seminal analyses of Wolfe et al. (1), patients with prolonged dialysis exposure in this study required a much longer time to achieve the survival benefit associated with transplantation. In that study, transplant recipients had an equal risk of death 106 days after transplantation and derived a survival benefit 244 days after transplantation compared with 180 and 657 days, respectively, in these study patients. These differences are primarily the result of the fact that study patients were dialysis survivors and had a lower overall death rate during dialysis treatment (5.8/100 patient-years) compared with patients included in the analysis of Wolfe et al. (1) (6.3/100 patient-years). In addition, study patients also had a slightly higher rate of death after transplantation (3.9/100 patient-years) compared with 3.8/100 patient-years in the analysis of Wolfe et al. (1). This information may be useful when counseling patients who are clinically stable and have been on long-term dialysis about the benefits of kidney transplantation.
Examination of the death rates in study patients during dialysis treatment also provides information that may be important for the management of similar patients currently on the waiting list. There was a relatively large increase in the death rate with increasing time on dialysis in study patients after the 10-year dialysis anniversary. Of note, 80% of the study patients were waitlisted after their 10-year dialysis anniversary, and it is likely that some patients were evaluated by transplant centers relatively close to the time of deceased donor transplantation, suggesting the importance of close surveillance of such patients during the waitlisting period.
Despite our efforts to identify a contemporary cohort of patients with sufficient potential follow-up to inform current clinical practice, the extent to which the study findings can be applied to the over 25,000 dialysis-treated patients with similar durations of pretransplant exposure is uncertain. The study patients were younger and had higher EPTS than the over 3000 patients currently waitlisted with a similar duration of pretransplant dialysis exposure. Only a minority (n=528; 9.8%) of the study patients were waitlisted after the implementation of the new KAS, and 267 of these patients received a transplant. Therefore, the majority of study patients were likely not waitlisted with the expectation of rapid transplantation, which may be the primary motivation to refer patients not currently waitlisted for transplantation after the implementation of the new KAS.
It is notable that most study patients received relatively low KDPI kidneys, and only 6% received kidneys with KDPI>85%. Given the higher risk of perioperative morbidity in transplants using high KDPI kidneys (14–16), patients with prolonged dialysis exposure may not derive a survival benefit from transplantation from a high-KDPI donor. The main consideration in selecting patients for a high KDPI donor kidney is to avoid the additional exposure to dialysis required to receive a better-quality kidney (15,16). This consideration may not be relevant for most patients with prolonged dialysis exposure under current allocation rules, because such patients may gain rapid access to better-quality deceased donor kidneys. The duration of dialysis exposure (i.e., ≥10 years) was arbitrarily chosen but is justified by the fact that a substantial proportion (13%) of currently waitlisted patients have had ESRD (including treatment with dialysis or transplantation) for 11 years or longer (5). This study is subject to the well known limitations of observational studies and did not examine other important considerations, including improvements in quality of life and cost-savings associated with transplantation, compared with treatment with dialysis (2).
In summary, kidney transplantation with good-quality deceased donor kidneys was associated with a long-term survival benefit in selected patients with pretransplant dialysis exposure ≥10 years. However, survival was not achieved until nearly 2 years after the date of transplantation, despite the fact that most of the transplants were performed with relatively low KDPI kidneys. Although these findings support consideration of patients with similar durations of dialysis exposure for transplantation, further studies are needed to inform the selection of such patients for transplantation and determine whether such patients also benefit from transplantation with lower-quality deceased donor kidneys.
Disclosures
None.
Acknowledgments
J.S.G. is supported by a foundation grant from the Canadian Institutes of Health Research.
The data reported here have been supplied by the Minneapolis Medical Research Foundation as the contractor for the Scientific Registry of Transplant Recipients (SRTR) and the US Renal Data System. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the SRTR or the US Government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, Held PJ, Port FK: Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med 341: 1725–1730, 1999 [DOI] [PubMed] [Google Scholar]
- 2.Tonelli M, Wiebe N, Knoll G, Bello A, Browne S, Jadhav D, Klarenbach S, Gill J: Systematic review: Kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant 11: 2093–2109, 2011 [DOI] [PubMed] [Google Scholar]
- 3.Laupacis A, Keown P, Pus N, Krueger H, Ferguson B, Wong C, Muirhead N: A study of the quality of life and cost-utility of renal transplantation. Kidney Int 50: 235–242, 1996 [DOI] [PubMed] [Google Scholar]
- 4.Gill JS, Tonelli M, Johnson N, Kiberd B, Landsberg D, Pereira BJ: The impact of waiting time and comorbid conditions on the survival benefit of kidney transplantation. Kidney Int 68: 2345–2351, 2005 [DOI] [PubMed] [Google Scholar]
- 5.Hart A, Smith JM, Skeans MA, Gustafson SK, Stewart DE, Cherikh WS, Wainright JL, Kucheryavaya A, Woodbury M, Snyder JJ, Kasiske BL, Israni AK: OPTN/SRTR 2015 annual data report: Kidney. Am J Transplant 17[Suppl 1]: 21–116, 2017 [DOI] [PMC free article] [PubMed]
- 6.Meier-Kriesche HU, Port FK, Ojo AO, Rudich SM, Hanson JA, Cibrik DM, Leichtman AB, Kaplan B: Effect of waiting time on renal transplant outcome. Kidney Int 58: 1311–1317, 2000 [DOI] [PubMed] [Google Scholar]
- 7.Cosio FG, Alamir A, Yim S, Pesavento TE, Falkenhain ME, Henry ML, Elkhammas EA, Davies EA, Bumgardner GL, Ferguson RM: Patient survival after renal transplantation. I. The impact of dialysis pre-transplant. Kidney Int 53: 767–772, 1998 [DOI] [PubMed] [Google Scholar]
- 8.Schold JD, Sehgal AR, Srinivas TR, Poggio ED, Navaneethan SD, Kaplan B: Marked variation of the association of ESRD duration before and after wait listing on kidney transplant outcomes. Am J Transplant 10: 2008–2016, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Israni AK, Salkowski N, Gustafson S, Snyder JJ, Friedewald JJ, Formica RN, Wang X, Shteyn E, Cherikh W, Stewart D, Samana CJ, Chung A, Hart A, Kasiske BL: New national allocation policy for deceased donor kidneys in the United States and possible effect on patient outcomes. J Am Soc Nephrol 25: 1842–1848, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stewart DE, Kucheryavaya AY, Klassen DK, Turgeon NA, Formica RN, Aeder MI: Changes in deceased donor kidney transplantation one year after KAS implementation. Am J Transplant 16: 1834–1847, 2016 [DOI] [PubMed] [Google Scholar]
- 11.Organ Procurement and Transplantation Network. United Network for Organ Sharing Policy 8.5 Kidney Allocation Classifications and Rankings. (Richmond) 2013. Available at: http://optn.transplant.hrsa.gov/PoliciesandBylaws2/policies/pdfs/policy_7.pdf. Accessed August 10, 2017
- 12.OPTN : A Guide to Calculating and Interpreting the Kidney Donor Profile Index, 2014. Available at: https://optn.transplant.hrsa.gov/media/1512/guide_to_calculating_interpreting_kdpi.pdf. Accessed March 7, 2016
- 13.Mauger EA, Wolfe RA, Port FK: Transient effects in the Cox proportional hazards regression model. Stat Med 14: 1553–1565, 1995 [DOI] [PubMed] [Google Scholar]
- 14.Massie AB, Luo X, Chow EK, Alejo JL, Desai NM, Segev DL: Survival benefit of primary deceased donor transplantation with high-KDPI kidneys. Am J Transplant 14: 2310–2316, 2014 [DOI] [PubMed] [Google Scholar]
- 15.Schold JD, Meier-Kriesche HU: Which renal transplant candidates should accept marginal kidneys in exchange for a shorter waiting time on dialysis? Clin J Am Soc Nephrol 1: 532–538, 2006 [DOI] [PubMed] [Google Scholar]
- 16.Merion RM, Ashby VB, Wolfe RA, Distant DA, Hulbert-Shearon TE, Metzger RA, Ojo AO, Port FK: Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA 294: 2726–2733, 2005 [DOI] [PubMed] [Google Scholar]