Abstract
Asthma is a heterogeneous disease, usually characterized by chronic airway inflammation. Various clinical conditions can mimic asthma, such as foreign body aspiration, subglottic stenosis, congestive heart failure, diffuse panbronchiolitis, aortic arch anomalies, reactive airway dysfunction syndrome, chronic obstructive pulmonary disease, retrosternal goiter, vocal cord tumors, other airway tumors, and vocal cord dysfunction. Upper airway obstruction can be a life-threatening emergency. Here, we present the case of a 58-year-old female with recurrent hospital visits for wheezing and exacerbations of asthma, who was later found to have a vocal cord nodule confirmed to be squamous cell carcinoma, which was mimicking like asthma.
Keywords: Vocal cord mass, asthma mimic, wheeze
Introduction
Asthma is a heterogeneous disease, usually characterized by chronic airway inflammation. It can be present with wheezing, chest tightness, cough, and shortness of breath, all of which may vary in intensity and over time.1 The diagnosis of asthma requires an appropriate history, consisting of respiratory symptoms, diurnal variation of symptoms, and exposure to triggers, as well as demonstration of variable expiratory airflow obstruction.2
Wheezing is a common manifestation of respiratory illness in adults. Wheezing is not always indicative of asthma, and not all asthma produces wheezing.3 Causes of wheezing can be divided into three categories: extrathoracic upper airway obstruction, intrathoracic upper airway obstruction, and lower airway obstruction.
Upper airway obstruction can be a life-threatening emergency. The most common causes of upper airway obstruction are paroxysmal vocal cord motion, retropharyngeal abscess, benign airway tumors, anaphylaxis, bilateral vocal cord paralysis, foreign body aspiration, tracheal stenosis, intrathoracic goiter, tracheomalacia, and a right-sided aortic arch.4,5
The vocal cord abnormality that most commonly mimics asthma is vocal cord dysfunction. However, the differential diagnosis includes other disorders that should also be kept in mind, such as vocal cord polyps, vocal cord granulomas, unilateral or bilateral vocal cord paralysis, and vocal cord tumors.6
Vocal cord tumors can produce asthma-like symptoms at the time of presentation. These tumors are relatively common. Approximately 13,430 new cases of laryngeal cancer are identified each year in United States. The number of new cases of larynx cancer is 3.2 per 100,000 men and women per year.
Case report
A 58-year-old Hispanic woman arrived at our emergency department with a chief complaint of wheezing and dry cough for 2 days. She had no fever, sore throat, chest pain, hemoptysis, night sweats, odynophagia, no hoarseness of voice, abdominal pain, hematemesis, or melena. Her past medical history was significant for hypertension, diabetes mellitus type II, hyperlipidemia, and gastroesophageal reflux disease. She was recently discharged from the emergency department after management of shortness of breath and wheeze 1 week prior to the current visit. Our patient had four emergency room visits in past 6 months before this hospitalization. Patient also visited her primary care physician twice for similar complaints. All her symptoms started 6 months ago. Prior to this emergency room visit, she was seen at a pulmonary clinic for predominant symptoms of wheezing.
The patient’s surgical history was significant for a cesarean section 20 years ago. Her mother died of breast carcinoma. She had 15-pack-year history of smoking, and she consumed alcohol socially. She denied illicit drug use and reported no allergies. She was taking metformin, lisinopril, chlorthalidone, metoprolol, atorvastatin, aspirin, omeprazole, albuterol inhaler as needed. She lived with her family and was a home-maker with no known occupational exposure to toxic substances.
Physical examination on presentation to the emergency department revealed an emaciated woman with these findings: temperature, 97.6°F; pulse, 102 beats/min; respiratory rate, 18 breaths/min; blood pressure, 112/69 mm Hg; pulse oxygen saturation, 98% on ambient air; and body mass index, 15 kg/m2. Her oral mucosa was moist, and skin turgor was normal. She had no palpable lymphadenopathy. She had equal air entry bilaterally with inspiratory wheezes on lung auscultation. She had a sinus tachycardia but normal heart sounds. She had no organomegaly on abdominal examination, and her neurological examination was unremarkable.
Initial laboratory results which included hematology profile, serum chemistry, liver function blood tests, and serum calcium levels were within normal limits. Chest radiography showed no pulmonary infiltrates. She was subsequently discharged from hospital after her wheeze subsided. Spirometry done in pulmonary clinic revealed flattening of the inspiratory flow loop (Figure 1).
Figure 1.
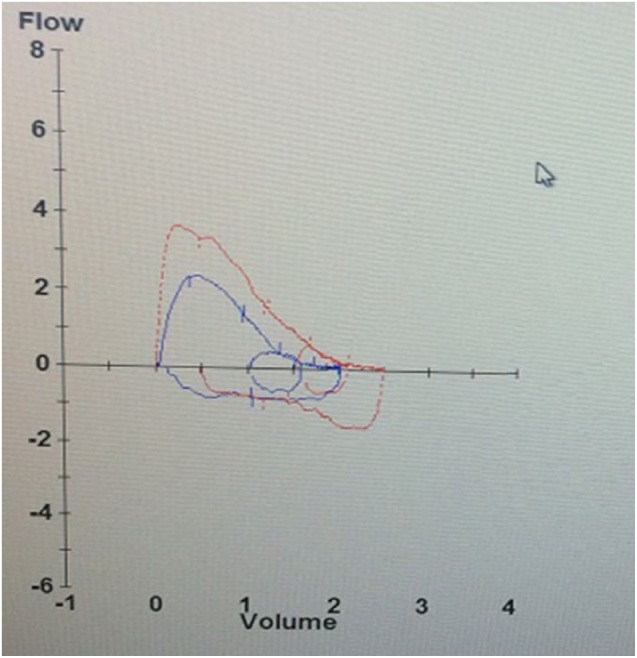
Spirometry showing flattening of the inspiratory flow–volume loop.
Computed tomography (CT) of the neck performed showed a 1.4 × 1.4 cm2 right vocal cord mass causing airway narrowing (Figure 2).
Figure 2.
CT of the neck showing a 1.4 × 1.4 cm2 exophytic right vocal cord nodules: (a) sagittal view and (b) coronal view.
Members of the otolaryngology consultation service performed fiberoptic laryngoscopy, which showed a large exophytic mass arising from the right true vocal cord but normal vocal cord mobility (Figure 3).
Figure 3.

Fiberoptic laryngoscopy showing a large exophytic mass attached to the right true vocal cord.
Subsequently, she underwent excisional biopsy of the vocal cord nodules and underwent emergency tracheostomy to secure the airway. Histopathology of the mass showed moderately differentiated invasive squamous cell carcinoma T3N0M0. The patient’s postoperative hospital course was unremarkable, and she was discharged home with plans for outpatient chemoradiation therapy.
Discussion
Asthma is a common respiratory illness, which is managed with inhaled and oral agents such as bronchodilators, corticosteroids, and leukotriene receptor antagonists. Patients with chronic symptoms suggestive of asthma, normal spirometry, poor response to asthma medications, and frequent medical visits should be evaluated for the presence of other conditions that mimic asthma.
True vocal cord carcinoma is the most common of all laryngeal cancers. Most of these tumors occur on the anterior two-thirds of the cord, although a small percentage is located on the anterior commissure. They rarely occur on the posterior commissure. The growth characteristics of true vocal cord carcinomas are determined by the unique anatomy of the vocal cords. The sparsity of lymphatic drainage in all areas of the vocal cord except the posterior commissure makes metastasis of early lesions extremely unlikely.7 The first reported case of head and neck squamous cell carcinoma was in 1868.8
Various conditions can mimic asthma; common mimics include foreign body aspiration, vocal cord dysfunction, vocal cord abnormalities, exercise-induced bronchospasm, and gastroesophageal reflux disease. Vocal fold paresis from prolonged intubation, idiopathic vocal fold paralysis, recurrent laryngeal nerve damage during surgery, and vocal fold paralysis caused by head and neck malignancy can all cause abnormal vocal fold movement and thereby produce symptoms of vocal cord dysfunction that mimic asthma.9 The other uncommon conditions which may mimic asthma-like symptoms are subglottic stenosis, congestive heart failure, diffuse panbronchiolitis, reactive airway dysfunction syndrome, chronic obstructive pulmonary disease.
Psychogenic respiratory distress mimicking asthma can be a conversion reaction that causes paradoxical vocal cord dysfunction.10 Non-asphyxiating foreign body aspiration usually presents as a cough, but it may also cause wheezing, shortness of breath, and hemoptysis. The wheezing in these patients mimics asthma.11 Laryngotracheal stenosis is a rare condition, which can present as a complication of granulomatosis with polyangiitis; it can also produce wheezing that mimics asthma.12 As reported by Özgül et al.,13 an ectopic parathyroid adenoma at the distal part of the trachea can also produce asthma-like wheezing. Endobronchial lipomas, which are rare benign tumors of the lung, can likewise present with asthma-like wheezing.14 In addition, endobronchial tuberculosis presenting as a polypoid, necrotic endobronchial lesion has been reported to produce symptoms mimicking asthma.15
In the herein described case, a true vocal cord nodules, which was found to be squamous cell cancer on biopsy, produced symptoms mimicking asthma that led to recurrent office and emergency room visits. Among carcinomas of the head and neck, 45% are laryngeal cancer. These cancers are most often found in males over 50 years of age. Common risk factors for laryngeal and hypopharyngeal cancers are male sex; tobacco use and alcohol consumption; human papilloma virus infection; genetic predilection; and exposure to wood dust, paint fumes, and certain chemicals used in metal-working, petroleum, plastics, and asbestos textile industries.16,17 A study by Zhao et al.18 suggests that an association exists between overexpression of histone deacetylase 1 and the clinical characteristics of laryngeal squamous cell carcinoma.
Symptoms of vocal cord cancer vary, depending on the structures involved by the malignancy and the accompanying inflammatory reaction. The symptoms may include wheezing, stridor, dyspnea, dysphagia, dysphonia, pain, halitosis, blood-tinged sputum, and a neck mass. Investigations that can be performed include direct laryngoscopy, CT of the neck and chest, plain chest radiography, positron emission tomography, and pulmonary function tests (PFT) (Figure 4). Inspection of the larynx is best accomplished using a flexible laryngoscope, and direct laryngoscopy also provides an opportunity to obtain biopsies of the tumor.
Figure 4.

An algorithm for diagnosis of inspiratory wheeze.
PFT, starting with spirometry before and after the administration of inhaled bronchodilator, can be performed for patients who have wheezing. The flow–volume loop helps determine whether airflow obstruction is caused by an intrathoracic or extrathoracic obstruction and whether the obstruction is variable or fixed. Variable extrathoracic obstruction caused by vocal cord paralysis is typically apparent only during maximum inspiration. The maximal expiratory flow–volume curve and expiratory spirometry are usually normal in this setting because the extrathoracic airway will be pushed open during expiration. In addition to visual inspection of the graph, the ratio of inspiratory to expiratory flow rates can help distinguish a variable extrathoracic lesion from an intrathoracic upper airway lesion.19,20 In our case, patient had spirometry that showed inspiratory loop flattening suggesting extrathoracic obstruction.
CT with contrast of the chest and neck can identify various structures that cause extrinsic compression of the trachea, such as a mediastinal mass, lymphadenopathy, an aneurysm, airway stenosis, a central airway neoplasm, congenital airway disorders, tracheobronchomalacia, and vascular rings. These conditions may all cause wheezing.21
The National Comprehensive Cancer Network22 Practice Guidelines in Oncology currently recommend concurrent radiation therapy and cisplatin chemotherapy to achieve laryngeal preservation in cases of locally advanced laryngeal cancer. There are various surgical options, including transoral laser microsurgery, open partial laryngectomy, and total laryngectomy.23 Our case emphasizes on the fact that different etiologies can mimic asthma and recognizing vocal cord nodules causing obstruction of upper airway as an emergency.
Conclusion
Various conditions may mimic asthma, and patients with poor response to asthma medications and frequent office or hospital visits should be further evaluated for the presence of an asthma mimic. Awareness of vocal cord nodules and its appropriate evaluation is critical in patients presenting with hoarseness, stridor, and/or wheezing. Timely PFT and direct laryngoscopy, as performed for the patient described in this report, can aid in the identification of vocal cord nodules and lead to a definitive diagnosis.
Acknowledgments
M.Kh. and M.Ka. searched the literature and wrote the manuscript. M.Kh. conceived and edited the manuscript. M.Kh. supervised the patient treatment, critically revised and edited the manuscript. T.S. and A.A. were involved in patient care along with M.Kh. All authors have made significant contributions to the manuscript and have reviewed it before submission. All authors have confirmed that the manuscript is not under consideration for review at any other Journal. All authors have read and approved the final manuscript.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our hospital does not require IRB approval for case reports. Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from patient and is with corresponding author.
References
- 1.National asthma education and prevention program: expert panel report III: guidelines for the diagnosis and management of asthma. Bethesda, MD: National Heart, Lung, and Blood Institute, 2007, https://www.nhlbi.nih.gov/health-pro/guidelines/current/asthma-guidelines/full-report (accessed 4 December 2014). [Google Scholar]
- 2. Global initiative for Asthma. Global strategy for asthma management and prevention, 2016, http://ginasthma.org/2016-gina-report-global-strategy-for-asthma-management-and-prevention
- 3. Bohadana A, Izbicki G, Kraman SS. Fundamentals of lung auscultation. N Engl J Med 2014; 370: 744–751. [DOI] [PubMed] [Google Scholar]
- 4. Gehlbach B, Kress JP. Upper airway obstruction. In: Hall JB, Schmidt GA, Wood LDH. (eds) Principles of critical care. 3rd ed. New York: McGraw-Hill, 2005, pp. 455–464. [Google Scholar]
- 5. Khosh MM, Lebovics RS. Upper airway obstruction. Parillo JE, Dellinger RP. (eds) Critical care medicine. 2nd ed. St Louis, MO: Mosby, 2001, pp. 808–825. [Google Scholar]
- 6. Campainha S, Ribeiro C, Guimarães M, et al. Vocal cord dysfunction: a frequently forgotten entity. Case Rep Pulmonol 2012; 2012: 525493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sessions DG, Ogura JH, Fried MP. Laryngeal carcinoma involving anterior commissure and subglottis. Can J Otolaryngol 1975; 4(4): 666–670. [PubMed] [Google Scholar]
- 8. Rehn H. Cancer of the vestibule and vocal cords in a 3 years old boy. Arch Pathol Anat Physiol Klin Med 1868; 43: 129. [Google Scholar]
- 9. Christopher KL, Morris MJ. Vocal cord dysfunction, paradoxic vocal fold motion, or laryngomalacia? Our understanding requires an interdisciplinary approach. Otolaryngol Clin North Am 2010; 43(1): 43–66. [DOI] [PubMed] [Google Scholar]
- 10. Leo RJ, Konakanchi R. Psychogenic respiratory distress: a case of paradoxical vocal cord dysfunction and literature review. Prim Care Companion J Clin Psychiatry 1999; 1(2): 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chen CH, Lai CL, Tsai TT, et al. Foreign body aspiration into the lower airway in Chinese adults. Chest 1997; 112(1): 129–133. [DOI] [PubMed] [Google Scholar]
- 12. Nunn AC, Nouraei SA, George PJ, et al. Not always asthma: clinical and legal consequences of delayed diagnosis of laryngotracheal stenosis. Case Rep Otolaryngol 2014; 2014: 325048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Özgül MA, Seyhan EC, Özgül G, et al. Endotracheal ectopic parathyroid adenoma mimicking asthma. Respir Med Case Rep 2014; 13: 28–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rooijakkers M, Wynants J, Aumann J. Endobronchial lipoma, an extremely rare benign tumour of the lung, mimicking asthma bronchiale. Acta Clin Belg 2014; 69(1): 74–75. [DOI] [PubMed] [Google Scholar]
- 15. Argun Baris S, Onyilmaz T, Basyigit I, et al. Endobronchial tuberculosis mimicking asthma. Tuberc Res Treat 2015; 2015: 781842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kapil U, Singh P, Bahadur S, et al. Assessment of risk factors in laryngeal cancer in India: a case-control study. Asian Pac J Cancer Prev 2005; 6(2): 202–207. [PubMed] [Google Scholar]
- 17. Marchiano E, Patel DM, Patel TD, et al. Subglottic squamous cell carcinoma: a population-based study of 889 cases. Otolaryngol Head Neck Surg 2016; 154(2): 315–321. [DOI] [PubMed] [Google Scholar]
- 18. Zhao R, Chen K, Cao J, et al. A correlation analysis between HDAC1 over-expression and clinical features of laryngeal squamous cell carcinoma. Acta Otolaryngol 2016; 136(2): 172–176. [DOI] [PubMed] [Google Scholar]
- 19. Miller RD, Hyatt RE. Obstructing lesions of the larynx and trachea: clinical and physiologic characteristics. Mayo Clin Proc 1969; 44(3): 145–161. [PubMed] [Google Scholar]
- 20. Bolliger CT, Sopko J, Maurer P, et al. The flow-volume loop in bilateral vocal cord paralysis. Chest 1993; 104(4): 1302–1304. [DOI] [PubMed] [Google Scholar]
- 21. Lee KS, Boiselle PM. Update on multidetector computed tomography imaging of the airways. J Thorac Imaging 2010; 25(2): 112–124. [DOI] [PubMed] [Google Scholar]
- 22. National Comprehensive Cancer Network. NCCN practice guidelines in oncology—head and neck cancers, version 2.2013, http://face2facehealing.org/wp-content/uploads/2015/11/NCCN-Guidelines-Multidisciplinary-Team-Approach.pdf
- 23. Wen WP, Su ZZ, Zhu XL, et al. Supracricoid partial laryngectomy with cricothyroidopexy: a treatment for anterior vocal commissure laryngeal squamous carcinoma. Head Neck 2013; 35(3): 311–315. [DOI] [PubMed] [Google Scholar]



