Abstract
We report the largest experience, to our knowledge, of home cardiorespiratory monitoring in 47,495 newborns using the novel Owlet Smart Sock (OSS) technology (October 2015 to May 2017). On average, 47,495 newborns were monitored for 6 months, 4.5 d/wk, 9.9 h/d. Continuous readings of oxygen saturation and heart rate were obtained from 39,626 full-term newborns. OSS users were likely first-time parents in their 30s with at least a college degree; 37% had a healthcare professional in the family; and 28% were at or below median income level per the US Census Bureau. “Peace of mind” was the reason to own an OSS in 75%, and 82% of parents followed Safe Sleep Guidelines. A total of 94% of parents reported a better quality of sleep. The fast and continuous pace of device adoption and reported experience suggest excellent parental acceptance of the OSS. Prospective studies are warranted to further evaluate its applications in the high-risk newborn population.
Keywords: neonatology, general pediatrics, cardiorespiratory monitoring, pulse oximetry
Objective
Development in biomedical and computer sciences, wireless communication techniques, and low-energy consumption microprocessors with sophisticated algorithms led to the recent widespread innovation of wearable monitoring systems.1 Continuous monitoring and transmission of physiological parameters in infants are not limited to alerting for and prevention of life-threatening events. It also represents an opportunity for physicians and scientists to identify or predict various pathological conditions and provide insights into the behavioral and physical development of a child.
However, the utility of home-based continuous monitoring, especially in healthy, term newborns, remains a controversial topic in the clinical community. Proponents suggest that this type of monitoring can provide parents and physicians valuable information about infant health, potentially alerting when an infant is in crisis and enabling timely intervention.2 Critics expressed concerns about frequent false alarms, high cost of monitors, increase in parental anxiety, and the risk of overdiagnosis.3,4 Currently, limited comprehensive, contemporary data exist to support or reject the usefulness of home-based continuous monitoring in infants.
The objective of this report is to describe the initial experience with home use of the Owlet Smart Sock (OSS), a novel, miniaturized, wireless, vital signs monitoring device in 47,495 newborns between October 2015 and June 2017 and to share insights into the largest reported series. With known limitations of current reports (descriptive statistics vs randomized clinical study, parent-reported prematurity, events retrospectively verified by physicians), the unique home use patterns, normative physiological reference ranges for oxygen saturation (SpO2) and heart rate (HR) for various newborn age groups, and a case study on apnea of prematurity (AOP) detection while using the OSS are presented in this article.
Importantly, we point out the utility of the OSS in regard to the future opportunities that it may offer to improve access to outpatient and at-home physiological monitoring of infants with specific medical conditions.5,6
Materials and Methods
Study Population
Owlet Baby Care, Inc., to the best of our knowledge, has amassed the largest data set on home use of the OSS vital signs monitor in newborns up to 12 months of age. The study population described includes 47,495 newborns (“active users”) between the commercial launch of the device in October 2015 and May 2017, when additional demographic surveys were conducted.
Active users were defined as those who activated the OSS for their newborns between 1 and 12 months of age, with total monitoring time ≥24 hours. Individual monitoring sessions <2 hours in duration and newborns with inconclusive or missing age were excluded from the current analysis. The newborns were predominantly located in the United States and Canada.
The continuous variables SpO2 and HR were obtained from 39,626 full-term newborns. OSS usage statistics were collected from all 47,495 active users. Demographic data self-reported by parents of newborns were available from 5125 users (24.2% response rate) who participated in a survey of all active users in May 2017.
It is important to note the following points: (1) only experience with the commercially available version of the OSS is the subject of the current report; the medical grade version of the OSS (class II) is currently under review by the Food and Drug Administration (FDA) and is not commercially available in the United States or Canada; (2) no claims or representations were made on the use of the current version of the device in clinical settings; (3) continuous variables (SpO2, HR) and alerts information (rates and types) were obtained via direct output during monitoring.
Device Description
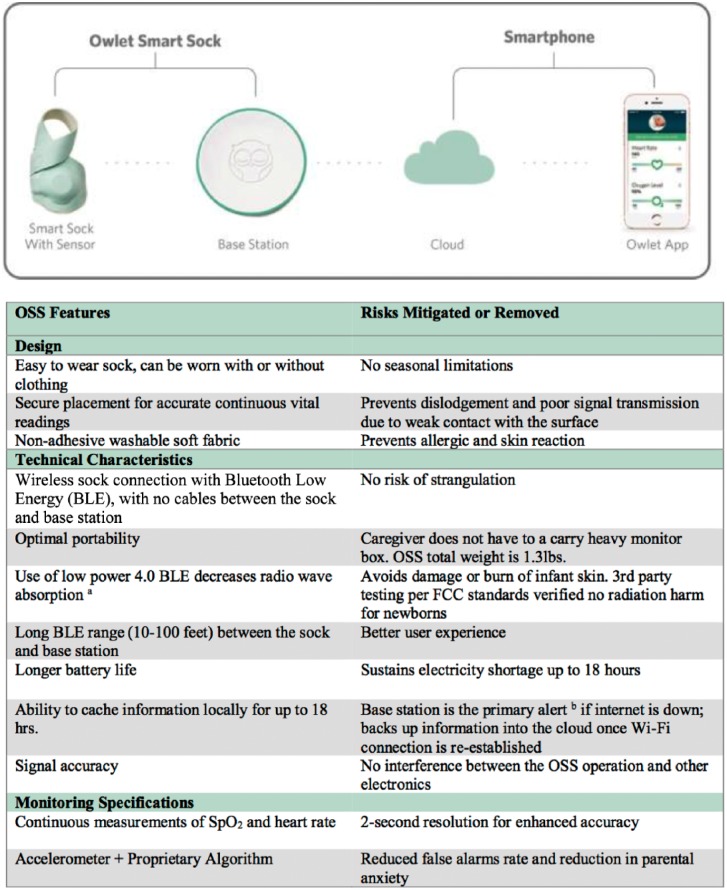
The OSS (Lehi, UT) is designed to provide continuous monitoring of vital signs (SpO2 and HR) in newborns via a sensor-embedded sock during their sleep in home settings. The OSS kit includes a base station, pulse oximeter, charging cords, and socks in 3 sizes (designed to fit newborns to children 15 to 18 months of age). The materials used for the OSS are durable, hypoallergenic, and safety tested for infant use. The key differentiating features and advantages of the OSS are depicted in Figure 1.
Figure 1.
Owlet Smart Sock System (OSS) and its key differentiating features.
a Industry standard measurement for radio wave absorption is known as specific absorption rate (SAR) and is measured in watts per kilogram of flesh (W/kg). The maximum safe SAR level set by the Federal Communications Commission (FCC) for transmitters on a human appendage is 4.0 W/kg. The OSS level is 0.0005 W/kg, which is 8000 times below the maximum safe threshold and more than 2000 times less than that of common cellular phones.
b Base station sounds an 80-decibel alarm [dB(A)/10 cm], which is in accordance with Food and Drug Administration standards that requires no less than 75 dB(A) for in-home monitors and no less than 70 dB(A) for hospital monitors.
The sensor is powered by a small rechargeable battery and sends the acquired data via Bluetooth Low Energy (BLE) to a base station. The battery can last for up to 18 hours without charging. The BLE radio waves generated are considered safe for the infant as verified by a mandatory third-party testing.
The Wi-Fi–enabled base station serves as the primary notification system, emitting both visual and audible signals when changes in SpO2 occur and/or the HR becomes too high or too low. The OSS smartphone application allows parents to receive alerts on their phone (iPhones iOS 9 or later) and monitor their infant’s vital signs remotely (see Figure 1). In a case of a Red Alert, parents can immediately view the exact cause of the alert (ie, low oxygen or high or low HR).
The OSS stores recorded SpO2 levels and HR data in a secure cloud-based system. If the Wi-Fi or electricity becomes unavailable, the monitoring continues and stores vitals data locally, for up to 18 hours, until the connection is restored and the data are loaded into the cloud. Home alarms, cell phones, or other electronics do not interfere with the OSS.
Accuracy and reliability of the OSS have been tested against hospital-grade pulse oximeters as well as arterial blood gas samples according to standard FDA guidance. Using hospital-grade pulse oximeters as a reference, the OSS has the SpO2 accuracy of ±3% (70%-100% range) and HR accuracy of ±5 beats per minute (bpm; 30-300 bpm range).
Vitals Data Collection
All Owlet Care users consented for data collection relevant to the OSS, and strict data confidentiality was maintained. HR, SpO2, and movement data in the 2-second resolution were collected and stored in a secure cloud database throughout the monitor use. All data related to alerts are preserved in the cloud database for retrospective analysis.
Description of OSS Alerts and Notifications System
A combination of an accelerometer and a proprietary algorithm of noise detection reduces the frequency of false alarms. The OSS notifications allow users to differentiate between alerts caused by device malfunction and notifications caused by changed preset vital readings. There are 5 types of alerts, each represented by a specific color that displays on the base station (see the appendix). The base station also sounds an 80-dB alarm [dB(A)/10 cm].
The Red Alert is the most critical and immediate of the OSS alarms. When the infant’s average HR dips below 60 bpm or exceeds 220 bpm or when the SpO2 value drops below the 80% threshold, a Red Alert is issued. The processing algorithm limits the oxygen value to changing by no more than 1% SpO2 per second and the HR to changing by no more than 8 bpm/s, which is in accordance with physiological limits.
Results
Continuous readings of HR and SpO2 with a 2-s resolution were obtained from 39,626 full-term consecutive active OSS users between October 2015 and May 2017. Version 1.0 of the OSS was used in 65.6% of newborns; V2.0 became available in March 2017.
In addition, because of limitations in the initial data collection methodology, a survey to describe demographics and OSS user demographics was conducted among all active OSS users in May 2017. The response rate was 24.2%, and data on 5,125 users are summarized in Table 1.
Table 1.
Newborn, Parent, and OSS Usagea Characteristics.
| Demographic Survey Data Set (n = 5125)a | Percentage |
|---|---|
| Newborn profile | |
| Full-term newborns | 85% |
| Preterm newborns | 15% |
| Parent profile | |
| Parent age category | |
| • 30-39 Years old | 61% |
| • 21-29 Years old | 31% |
| • 40+ Years old | 7% |
| College-educated household | 70% |
| Household with at least 1 healthcare industry professional | 37% |
| Households at or below median incomeb | 28% |
| Reasons for using OSSc | |
| History of SIDS (parent or someone close to the parent) | 8% |
| Infant diagnosed with a breathing problem or heart condition | 12% |
| Newborn post NICU | 13% |
| First-time parent | 30% |
| “Peace of mind” feeling | 44% |
| Parental outcome of using OSS | |
| Following Safe Sleep Guidelines | 82% |
| Better quality sleep for parents | 94% |
| Feeling less anxiety | 96% |
Abbreviations: OSS, Owlet Smart Sock System; SIDS, sudden infant death syndrome; NICU, neonatal intensive care unit.
Parent reported data.
US median income is $56,516 per 2015 US Census Bureau.
Some parents indicated >1 reason.
Most parents (85%) used OSS for healthy full-term newborns, and 15% of monitored newborns were preterm children. Although data describe an early adopter of the OSS as likely being a first-time parent in their 30s with at least 1 college degree (“digital natives”), there were a few surprising findings. About 37% of Owlet users had at least 1 parent working in the health care industry. Importantly, about a third of families using OSS were at or below the median income level, per US Census Bureau.7
A parental desire to know more about their child as well as a feeling of peace of mind accounted for 75% of the reasons to own the OSS. According to the survey results, parents felt significantly less anxious and reported better quality of sleep (96% and 94% of users, respectively). Safe Sleep Guidelines were followed by 82% of parents. Per the survey, parent-reported history of SIDS (with the previous pregnancy or in the family) accounted for 8% of reasons for owning the OSS, and 15% of parents used the OSS on their infants discharged from the neonatal intensive care unit (NICU).
Normative Physiological Readings
Because the accuracy of the self-reported gestational age of preterm infants was not verified, we report normative findings for SpO2 and HR in 39,626 full-term newborns only. The sock was worn primarily by infants in their sleep per the OSS user manual.
The normal average HR in full-term babies while sleeping is 136 bpm in the first month of postnatal life and 106 bpm at 12 months, consistent with reported physiological findings (see Table 2). The average SpO2 in full-term babies varied slightly by months of age, with 96% in the first month of life and 97% at 12 months.
Table 2.
Heart Rate and Oxygen Saturation (SpO2) Averages by Age for Full-Term Monitored Newborns (n = 39,626).a
| Postnatal Age (n) | Heart Rate (bpm) ± SD) | SpO2 (%) ± SD |
|---|---|---|
| 1 Month (15 372) | 136 ± 9.0 | 96 ± 1.7 |
| 2 Months (19 729) | 131 ± 8.2 | 97 ± 1.6 |
| 3 Months (20 443) | 122 ± 7.5 | 97 ± 1.6 |
| 4 Months (20 168) | 116 ± 7.4 | 97 ± 1.6 |
| 5 Months (19 357) | 114 ± 7.5 | 97 ± 1.9 |
| 6 Months (18 103) | 112 ± 7.2 | 97 ± 1.5 |
| 7 Months (16 268) | 111 ± 7.1 | 97 ± 1.4 |
| 8 Months (13 806) | 110 ± 7.1 | 97 ± 1.4 |
| 9 Months (10 917) | 109 ± 7.2 | 98 ± 1.4 |
| 10 Months (8357) | 108 ± 7.2 | 98 ± 1.4 |
| 11 Months (6166) | 107 ± 7.2 | 98 ± 1.4 |
| 12 Months (4459) | 106 ± 7.6 | 97 ± 1.4 |
This population included activated users between 1 and 12 months of age, whose total time monitored was at least 24 hours.
Average OSS Usage
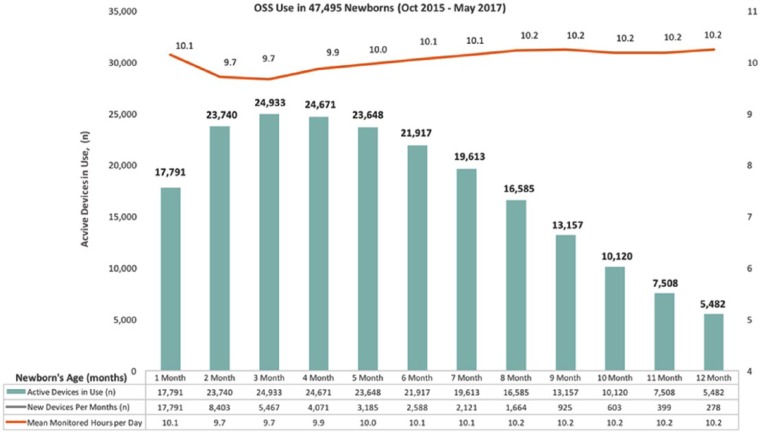
OSS usage data were obtained from 47,495 active users (full-term infants and parent-reported premature infants). According to our observation series, on average, a child was monitored for 6 months, 4.5 d/wk, and 9.9 h/d. The OSS smartphone app was utilized 64% of the time.
Figure 2 demonstrates the total number of devices used at 1 point of time at each month of the infant’s life and average use of OSS per day throughout first 12 months of life. The highest number of devices were activated between 0 and 1, and between 1 and 2 months of postnatal age. The total number of new devices activated each month is shown at the bottom of the data table.
Figure 2.
Owlet Smart Sock System (OSS) usage patterns: hours of daily use and number of devices used in 47,495 newborns.
Overall, OSS use started to decline between 5 and 6 months of age; however, as the overall number of users decreased, the average duration of daily monitoring remained relatively constant. This may suggest overall positive parental experience with the OSS and/or possibly exaggerated negative impact of the false alarm fatigue in the home setting.
False-Positive Alerts
For a typical night, most of the Red Alerts were for low oxygen (71%); fewer alerts were emitted for high HRs (18%) and low HRs (10%). For low oxygen events, artifacts usually lasted <20 s. For true alerts, the maximum raw SpO2 average value for the previous 20 s must have been less than 90 s, and the device must be transmitting at least 8 valid data points (out of 11) in the last 20 s. True bradycardias were associated with low oxygen levels below 80% saturation.
In our experience, clinically significant alerts tended to be clustered and repeated. For instance, a child would have been alert-free for 6 months, but 10 alerts may occur during the first days of a respiratory syncytial virus (RSV) infection.
User-Reported Clinically Significant Red Alerts
Whereas the OSS registers all types of alerts for users, the company encourages caregivers to report experiences related to clinically relevant Red Alerts. Also, Owlet reaches out to the caregivers and their physicians to gather and verify all relevant medical information associated with the Red Alert event when and if possible.
Since October 2015, Owlet has accumulated more than 80 parent-reported cases that led to either prevention of a critical event or helped diagnose an overlooked condition. Of these, 49 events (61%) appeared clinically significant after verification with the health care provider and analysis of matching waveforms. The remaining 39% of events were indeterminate (possible motion artifact, incorrect usage, or sparse data). The most common self-reported conditions that led to seeking medical advice and/or a hospitalization were the following: Respiratory syncytial virus (n = 23), Supraventricular tachycardia (n = 7), breathing disturbances (laryngomalacia, n = 7), obstructed airways caused by unsafe sleep practices (n = 5), congenital heart defect (n = 3), and apnea (n = 3).
Case Report: Apnea of Prematurity (AOP) in a 4-Day-Old Premature Infant
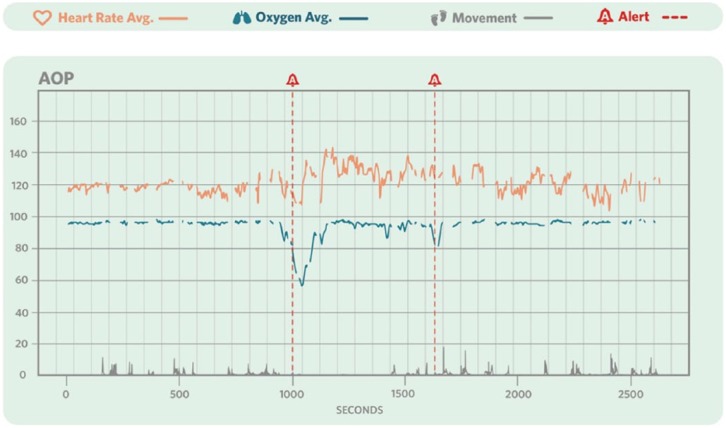
The following case report describes a preterm infant with AOP that led to a Red Alert. This case was verified with the neonatologist, and the clinical manifestation was matched with waveform readings from the OSS.
Description
A 4-day-old premature infant presented to the NICU with increasing apneas after birth (5 apnea episodes and 4 bradycardia/desaturation episodes with the need for a moderate stimulation or self-resolved) and was treated for AOP in the NICU for 8 days. Although the exact gestational age of the child was unclear, the prematurity of the newborn was confirmed by radiological findings and was suspected to be at 36 weeks (late premature infant). The parents purchased the OSS before the child’s birth to allow for a smoother care transition at home.
After the OSS issued 5 low oxygen Red Alerts during the night, the newborn’s vital signs were checked by a nurse with a hospital monitor. The hospital monitor confirmed the OSS readings and that the child was experiencing significant desaturation events while sleeping (Figure 3). The infant was treated with caffeine and moderate continuous positive airway pressure therapy support.
Figure 3.
Apnea of prematurity (AOP) registration and waveform tracing the Owlet Smart Sock System in a 4-day-old premature infant.
Potential Role of OSS in AOP Detection and Surveillance
AOP is a common problem affecting premature infants. The long-term consequences of severe, recurrent apnea-associated bradycardia and desaturation resulting in intermittent hypoxemia are not known; however, some authors have linked it8,9 with delayed mental development.
The potential uses of the OSS in premature infants are not limited to monitoring for AOP and bradycardia episodes; it may be a useful tool for studying the pathogenesis and consequences of AOP, long-term risks, and optimization of the treatment regimens.
Discussion
Use of pulse oximetry and cardiorespiratory monitors in the home setting has been long debated and has been a controversial topic ever since the introduction of such monitors in early 1970s.6 The history is well summarized in a recent article by Freed and Martinez.6
The most common sentiment toward home-based cardiorespiratory monitoring was supported by the National Institutes of Health Development Conference in 1982 and later by the American Academy of Pediatrics (AAP) guidelines based mostly on results from the CHIME study conducted in 1998 and published in 2001.5,10 In addition, the AAP Committee on the Fetus and Newborn presented recommendations related to the use of home cardiorespiratory monitoring in 2003 that discouraged its use for SIDS prevention or in healthy full-term infants, because of lack of proven benefits, and focused on the high-risk newborn population (high-risk premature and technology-dependent infants using monitors equipped with event recorder).5 The committee encouraged pediatricians to continue to promote proven practices that decrease the risk of SIDS, per recommendations.
Freed and Martinez6 provided data from a comprehensive home cardiorespiratory monitoring program of more than 35,000 infants from August 1998 to December 2016. Their most recent hypothesis about the utility of cardiorespiratory monitoring suggests that the monitoring of a select group of infants who are at risk for episodes of intermittent hypoxemia has merit and bears serious consideration.6 Other investigators have also demonstrated the utility of home pulse oximetry in at-risk infants,11 including late preterm infants.9 A study by Seddon et al12 using plethysmography recorded by pulse oximetry demonstrated the feasibility of this technique for monitoring of preterm infants in the home.
The purpose of this article was to present large reported experience with the OSS device as suggested in a recent viewpoint feature by Bonafide et al3 in January 2017. Authors warned that the commercial marketing of home cardiorespiratory monitors and pulse oximeters such as the OSS “may cause unnecessary fear, uncertainty, and self-doubt in parents.” Since the introduction of home monitors as summarized by Freed and Martinez,6 there has been concern that the false alarms would cause anxiety and psychological stress in parents. More recent technology such as pulse oximetry is very sensitive, and close attention needs to be paid to how these monitors’ limits are set.
Readings, registration, and storage of the data on SpO2 and HR in 2-s resolution with continuously evolving proprietary algorithms that reduce false alarms represents a significant opportunity to explore benefits of the home-based monitoring as part of comprehensive home-based care programs.
As Owlet continues to work on the application as a class-II medical device, we believe that multiparameter monitoring of basic vital signs in infants has applications for daily life management, clinical practice, and biomedical research. This strategy of the OSS is in keeping with the suggestion also made by Bonafide et al3 regarding the standardization of these devices. Contemporary health monitoring systems represents tools that provide an early indication of changing patient status, thus allowing for quick and timely intervention.
The key to this discussion is to highlight the capabilities that modern technology like the OSS offer, as well as the plethora of unanswered questions and implications for medical management and public health.
Conclusions
A fast and continuous pace of OSS adoption (>100 000 units used to date) suggests excellent parental acceptance and experience. When combined with technological advances of the system for continuous nonobtrusive monitoring in newborns, overall advantages of the OSS could be leveraged into solving important clinical and public health problems. Future prospective randomized clinical trials are warranted to further validate the impact of the OSS technology in healthy and high-risk newborns in clinical and home settings.
Limitations
Limitations of the current publication include the following:
it was a retrospective descriptive analysis of a self-selected population of early adopters of the OSS technology; and
incomplete and missing data on the key demographic and other characteristics at the initial stages of the OSS adoption significantly reduced the analyzed sample from the overall OSS user base.
Future Goals
In September 2017, Owlet Baby Care, Inc. launched the Connected Care accessory platform that will allow historical data tracking and trending, such as a 24-hour, 1-week, and 1-month view of HR and SpO2, sleep patterns, and detailed Red Alerts information. Parents may share this information with their physicians.
A broad clinical program has been set up to validate the OSS technology and assess its value in enabling insights into diagnosis and postdischarge surveillance for newborns at high risk for SIDS, Apparent Life-Threatening Events (ALTEs), and other conditions. The company collaborates with established investigators in prospective studies with FDA-approved pulse oximetry devices.
Acknowledgments
The authors would like to thank Dr. Joseph Hageman for his critical review of this article. Dr. Hageman is editor-in-chief, Pediatric Annals; Director of Quality Improvement, Section of Neonatology, Comer Children’s Hospital; a Senior Clinician Educator, The University of Chicago Pritzker School of Medicine; and an Emeritus Attending Pediatrician, North Shore University Health System.
Appendix
OSS Alerts Description.
| Base Station Color Indicator | Significance |
|---|---|
| Green | Blinking green: system is recording initial heart rate and oxygen vitals. Slow pulsing green: system is operational, and the baby is being actively monitored. Both heart rate and oxygen levels are in the preset range |
| White | Static white: sensor package is plugged in and charging |
| Yellow | Flashing yellow: system is reporting a warning; sock is not connected to the base station or sock fit is incorrect and unable to receive a high-integrity read |
| Blue | Flashing blue: sock has disconnected from the base station |
| Red | Flashing red: system is reporting a critical alert, which indicates heart rate is either high or low according to preset range or oxygen saturation is at a critical low level |
Footnotes
Author Contributions: MID: Contributed to acquisition, analysis and interpretation; drafted the manuscript; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
KW: Contributed to conception and design; contributed to the data acquisition; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
LD: Contributed to conception; contributed to acquisition and analysis; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
MA: Contributed to conception and design; contributed to acquisition, analysis, and interpretation; critically revised the manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Michelle I. Dangerfield, Luke Davidson, and Milena Adamian are employees of Owlet Care, Inc. Kenneth Ward is a consultant and medical advisor to Owlet Care, Inc, and owns stock options in the company.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: All authors of the manuscript have financial disclosures related to Owlet Care, Inc.
References
- 1. Zhu Z, Liu T, Li G, Li T, Inoue Y. Wearable sensor systems for infants. Sensors (Basel). 2015;15:3721-3749. doi: 10.3390/s150203721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Freed GE, Meny R, Glomb WB, Hageman JR. Effect of home monitoring on a high-risk population. J Perinatol. 2002;22:165-167. doi: 10.1038/sj.jp.7210662 [DOI] [PubMed] [Google Scholar]
- 3. Bonafide CP, Jamison DT, Foglia EE. The emerging market of smartphone-integrated infant physiologic monitors. JAMA. 2017;317:353-354. doi: 10.1001/jama.2016.19137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Carlin RF, Moon RY. Risk factors, protective factors and current recommendations to reduce sudden infant death syndrome. JAMA Pediatr. 2017;171:175-180. doi: 10.1001/jamapediatrics.2016.3345 [DOI] [PubMed] [Google Scholar]
- 5. American Academy of Pediatrics Committee of the Fetus and Newborn. Apnea, Sudden Infant Death Syndrome, and home monitoring. J Pediatr. 2003;111:914-917. [PubMed] [Google Scholar]
- 6. Freed GE, Martinez FM. The history of home cardiorespiratory monitoring. Pediatr Ann. 2017;46:303-308. doi: 10.3928/19382359-20170725-01 [DOI] [PubMed] [Google Scholar]
- 7. Proctor BD, Semega JL, Kollar MA. Income and poverty in the United States: 2015. https://www.census.gov/library/publications/2016/demo/p60-256.html. Accessed November 2, 2017.
- 8. Ramanathan R, Corwin MJ, Hunt CE, et al. Cardiorespi-ratory events recorded in the home: comparison of healthy infant with those at increased risk for SIDS. JAMA. 2001;285:2199-2207. doi: 10.1001/jama.285.17.2199 [DOI] [PubMed] [Google Scholar]
- 9. Montenegro BL, Amberson M, Veit L, Freiberger C, Dukhovny D, Rhein LM. Economics of home monitoring for apnea in late preterm infants. Respir Care. 2017;62:42-48. doi: 10.4187/respcare.04954 [DOI] [PubMed] [Google Scholar]
- 10. National Institutes of Health Consensus Development Conference on Infantile Apnea and Home Monitoring, Sept 29 to Oct 1, 1986. Pediatrics. 1987;79:292-299. [PubMed] [Google Scholar]
- 11. Gélinas J, Davis GM, Arlegui C, Côté A. Prolonged, documented home-monitoring of oxygenation in infants and children. Pediatr Pulmonol. 2008;43:288-296. doi: 10.1002/ppul.20776 [DOI] [PubMed] [Google Scholar]
- 12. Seddon P, Sobowiec-Kouman S, Wertheim D. Infant home respiratory monitoring using pulse oximetry [published online July 7, 2016]. Arch Dis Child. doi: 10.1136/archdischild-2016-310712 [DOI] [PubMed] [Google Scholar]