Abstract
Objective
Internet-based physical activity (PA) interventions have shown promise, although findings remain equivocal. We used formative research to enhance a previously demonstrated program (Step into Motion) with the goal of developing an Internet program poised for dissemination.
Methods
We conducted focus groups to identify Internet features targeted to theoretical constructs (social cognitive theory) predictive of PA behavior and rated as “useful for increasing PA.” We identified 5 theory-targeted Internet features as useful for increasing PA: (1) a PA tracking/logging calendar targeting self-monitoring and goal setting; (2) geographic mapping tools targeting perceived environment; (3) a discussion forum targeting social support; (4) exercise videos targeting observational learning; and (5) regular updates of peer PA progress targeting situation. We then tested the efficacy of the enhanced program (enhanced Internet, EI; N = 25) in relation to publicly available PA Websites (standard Internet, SI; N = 28) among 53 participants in a randomized controlled trial.
Results
The EI arm increased PA in relation to the SI arm at 3 months (18.4 to 186.0 min/wk vs. 20.9 to 57.3 min/wk; p = .03) but between-groups differences were not observed at 6 months (176.8 vs. 133.5 min/wk; p = .44). EI participants maintained PA from 3 to 6 months (186.0 to 176.8 min/wk), and the SI group increased PA (57.3 to 133.5 min/wk).
Conclusion
The EI program was efficacious at improving PA levels in relation to publicly available Websites initially, but differences in PA levels were not maintained at 6 months. Future research should identify Internet features that promote long-term maintenance.
Keywords: physical activity, sedentary, non-face-to-face
Physical inactivity has been identified as one of the leading preventable causes of death and all-cause mortality (Mokdad, Marks, Stroup, & Gerberding, 2004) and has been cited as the biggest public health problem of the 21st century (Blair, 2009). The U.S. Department of Health and Human Services recently issued the first comprehensive set of federal guidelines for physical activity (PA; U.S. Department of Health & Human Services, 2008), which state that all asymptomatic healthy adults should accumulate at least 150 minutes of moderate-intensity PA per week for health benefits. Despite these recommendations and the known benefits of regular PA, only 49% of U.S. adults are achieving these guidelines (National Center for Chronic Disease Prevention and Health Promotion, 2007), supporting a need for evidence-based PA interventions. Although face-to-face interventions are known to be successful in promoting PA (Dunn et al., 1999a), they are plagued with numerous barriers to participation, including participant transportation needs, time requirements, and high cost of delivery. Non-face-to-face interventions, including those delivered via the Internet, address many of these participation barriers through remote delivery and by emphasizing home-based, lifestyle activities (Marcus et al., 1998; Marcus, Napolitano, et al., 2007b).
Recent data indicate 77% of the U.S. population (231 million) uses the Internet (Pew Internet, 2008). Internet use is independent of age (92% of 18-year-olds online; 72% of 64-year-olds online), gender (76% of men and 74% of women), and race/ethnicity (76% of non-Hispanic Whites, 60% of African Americans, and 56% of Hispanics online) (Pew Internet, 2009). A study found that 8 of 10 Internet users look for health information online (Rees, 2005), and the number of those seeking exercise specific information online has increased dramatically from 36% in 2002 to 52% in 2008 (Pew Internet, 2008). The widespread use of the Internet suggests it to be a cost-effective way to reach large populations for the purpose of health promotion. In a recent study by Lewis et al., the Internet was shown to be a more cost-effective channel for delivering physical activity intervention materials to large populations (>352 people) when compared with print materials (B. A. Lewis, Williams, Neighbors, Jakicic, & Marcus, 2010). Therefore, because of its potential for non-face-to-face delivery, interactivity, wide reach, and cost-effectiveness, the Internet may be an ideal channel for delivering PA interventions designed for widespread dissemination (Mummery, Schofield, Hinchliffe, Joyner, & Brown, 2006).
Evidence-based PA interventions delivered via the Internet are highlighted as a specific strategy for improving public health in the recently released National Physical Activity Plan (National Physical Activity Plan, 2009). Thus far, Internet-based PA interventions have shown promise for increasing PA; however, the findings remain equivocal (Marcus, Ciccolo, & Sciamanna, 2008; Vandelanotte, Spathonis, Eakin, & Owen, 2007; Webb, Joseph, Yardley, & Michie, 2010). Although previous Internet PA studies have demonstrated modest effect sizes for increasing PA within groups across time (Webb et al., 2010), others have not found significant differences between groups. For example, in our Step into Motion (Marcus, Lewis, Williams, Whiteley, et al., 2007) trial, a motivationally tailored, theory-based individualized feedback intervention delivered via the Internet (tailored Internet) led to significant increases in moderate to vigorous PA of 141 minutes/week (min/wk) at month 6 and 105 min/wk at month 12; however, the intervention did not outperform our tailored print (same content delivered via print) or standard Internet (six reputable publicly available PA promotion Websites) arms (Marcus, Lewis, Williams, Dunsiger, et al., 2007). Although between-groups differences were not observed, the number of Website logins among the tailored Internet arm over 12 months was positively associated with greater PA at 12 months (B. Lewis et al., 2008). Additionally, constructs from social– cognitive theory (SCT; Bandura, 1997) that were measured but not targeted in the tailored Internet intervention—including self-monitoring, perceived environment (Ries, Dunsiger, & Marcus, 2009), outcome expectations, social support, and enjoyment—were predictive of increased PA at 12 months. As it is related to the behavior of physical activity, SCT suggests self-regulatory skills (e.g., tracking PA behavior via step logs) mediate an individual's self-efficacy and outcome expectations for PA behavior. SCT also supports implementing an element of social support to enhance the process of PA behavior change (Baranowski, Perry, & Parcel, 2002).
Overall, there have been too few clinical trials showing differences in lifestyle PA behavior when comparing intervention and control groups; and the majority of past Internet PA studies have been limited by approaches that require at least one face-to-face visit (Jenkins, Christensen, Walker, & Dear, 2009), limiting the potential reach of the Internet channel of delivery. Of the few Internet PA studies that have used non-face-to-face delivery to date, only two have demonstrated improvements in PA over a wait-list control group (Napolitano et al., 2003; Plotnikoff, McCargar, Wilson, & Loucaides, 2005). We are not aware of any published non-face-to-face Internet PA studies showing between-groups differences when using a contact control group (Jenkins et al., 2009). Therefore, little is known about whether Internet approaches delivered in a completely non-face-to-face format that require no in-person visits can instill positive changes in PA behavior when compared to publicly available programs. Evidence from other behavior change fields (e.g., weight management, smoking cessation, stress reduction, blood glucose control, reducing alcohol consumption) suggests that utilization of technologically advanced, low-cost, non-face-to-face Internet-delivered programs can be effective for behavior change (Graham, Cobb, Raymond, Sill, & Young, 2007; Petersen, Sill, Lu, Young, & Edington, 2008).
Few Internet PA interventions have used formative-based approaches such as focus groups for informing intervention development (Ferney & Marshall, 2005). Few Internet PA studies have used Internet features targeted specifically to theoretical constructs known to predict PA behavior (Marcus et al., 2008). To develop effective strategies for increasing PA via the Internet, it is critical to identify specific Internet features that have the greatest potential for increasing PA in both the short and long term. Recently, Anderson-Bill et al. tested whether SCT constructs were predictive of PA behavior in an online, SCT-based intervention program known as Guide to Health. The authors demonstrated that program user's perceived social support, use of self-regulatory behaviors, and self-efficacy were predictive of physical activity levels (Anderson-Bill, Winett, & Wojcik, 2011), and in a longitudinal model, improvements in the same constructs strongly predicted improved PA levels (Anderson-Bill, Winett, Wojcik, & Winett, 2011). This work illustrates the importance of identifying Internet features that are both appealing to users and based on theoretical constructs known to predict PA behavior (Hawkins, Kreuter, Resnicow, Fishbein, & Dijkstra, 2008; van den Berg et al., 2007).
The present study sought to address specific limitations of our past study by using formative data to enhance a previously demonstrated Internet PA program (Step into Motion). The aim of this study was to test the efficacy of the newly enhanced Internet (EI) intervention in relation to six reputable, publicly available PA promoting Websites (standard Internet, SI), which have been demonstrated to increase PA and successfully retain participants in our previous trial (Marcus, Lewis, Williams, Whiteley, et al., 2007), for improving PA behavior in previously sedentary adults. We hypothesized that the EI arm would increase their PA levels in relation to the SI group at both 3 and 6 months.
Method
Focus Groups
We conducted three focus groups using a nominal group technique (Stewart, Shamdasani, & Rook, 2007) with a convenience sample of 17 participants (41.7 ± 10.4 years of age, 91% female, 91% White, 68% married, 55% with an income of at least $50,000 per year). The goals of these focus groups was to identify Internet features rated as “useful for improving PA” by the participants. Internet features that targeted social cognitive theory (SCT) constructs found to predict PA adoption in two previous clinical PA trials were reviewed (Marcus, Lewis, Williams, Dunsiger, et al., 2007; Marcus, Napolitano, et al., 2007b). Interested participants were first e-mailed a link to prototypes of the Internet features 1 week prior to the focus group and asked to become familiar with the features. Participants then took part in a 90-min focus group discussing likes and dislikes of several identified Internet features. Participants then rank-ordered the features that they felt would be “most useful for increasing their PA.” We then added the highest-rated features to our EI Website: (1) an interactive logging feature targeting self-monitoring and goal setting in which participants logged their PA minutes into a calendar and set goals; (2) a geographic mapping tool targeting the perceived environment; (3) an “Ask the Expert” question-and-answer forum targeting social support; (4) exercise videos targeting observational learning; and (5) regular updates of peer PA progress targeting situation. All experimental protocols were approved by the Institutional Review Board for projects involving human subjects at Life Span/Miriam Hospital and Brown University in Providence, Rhode Island.
Intervention Design and Recruitment
To test the efficacy of our newly created EI Website in relation to six publicly available PA Websites, we recruited healthy, sedentary (achieving less than 60 min of moderate-to-vigorous physical activity per week) men and women between the ages of 18 and 65 years who had access to an Internet-connected computer. Participants across three different states (Rhode Island, Massachusetts, and Connecticut) were passively recruited through Internet advertisements posted on Craigslist. Exclusion criteria included the following: (1) ambulatory/exercise limitations; (2) any overt, complicated, or acute cardiovascular, metabolic, respiratory, or neurological diseases as assessed by medical history; (3) current or planned pregnancy; (4) hospitalization from any physical or mental disorder in the past 6 months; (5) taking medication that may impair PA tolerance or performance (e.g., beta blockers); (6) participation in any of our previous PA trials; and (7) lack of access to an Internet connected computer. Eligibility was assessed on the basis of a standardized telephone interview. Individuals willing to participate in the study read and signed an electronic informed consent document approved by the Brown University and Life Span institutional review boards.
A total of 527 individuals responded to our advertisements of which 461 were deemed ineligible to participate. Of the 461 participants deemed ineligible, 60 were excluded for either non-responsiveness (N = 35) or declining to participate (N = 25). The remaining 401 participants were deemed ineligible for being too active (N = 341) or for medical reasons (N = 52) including high body mass index (BMI), ambulatory limitations, asthma, stroke, pregnancy, and contraindicated medications. Eight participants were excluded for other reasons including lack of computer access and participation in a previous study. A total of 66 eligible people agreed to participate and were randomized to one of two groups: (1) enhanced Internet (EI; N = 32) or (2) standard Internet (SI; N = 34). However, 13 of the 66 participants were deemed ineligible after randomization for reasons of lack of providing necessary medical clearance (N = 6) and cross-contamination (N = 7) (see Figure 1). Specifically, a subgroup of participants mistakenly received one e-mail message directed at the opposite study arm during Week 1 of the intervention resulting in cross-contamination. These messages, though not substantive, introduced participants to group-specific details of the opposite study arm, and thus these participants were removed from the final data analysis. In summary, our study sample consisted of 53 participants with 25 randomized to the EI arm (80.0% women; age = 38.5 ± 13.1 years; BMI = 31.4 ± 1.1 kg/m2) and 28 randomized to the SI arm (71.4% women; age = 36.8 ± 11.1 years; BMI = 31.0 ± 0.7 kg/m2) (see Table 1). A total of 22 EI participants and 26 SI participants completed the 6-month assessment. Overall, more than half of all participants were college educated, and more than 80% reported being non-Hispanic/White. Participants were enrolled and completed all testing sessions between February 2010 and February 2011. We did not observe differential drop-out between the two groups. Although sample sizes were too small to statistically test for differences between dropouts and completers, exploratory analyses did not detect any meaningful differences between these samples.
Figure 1.
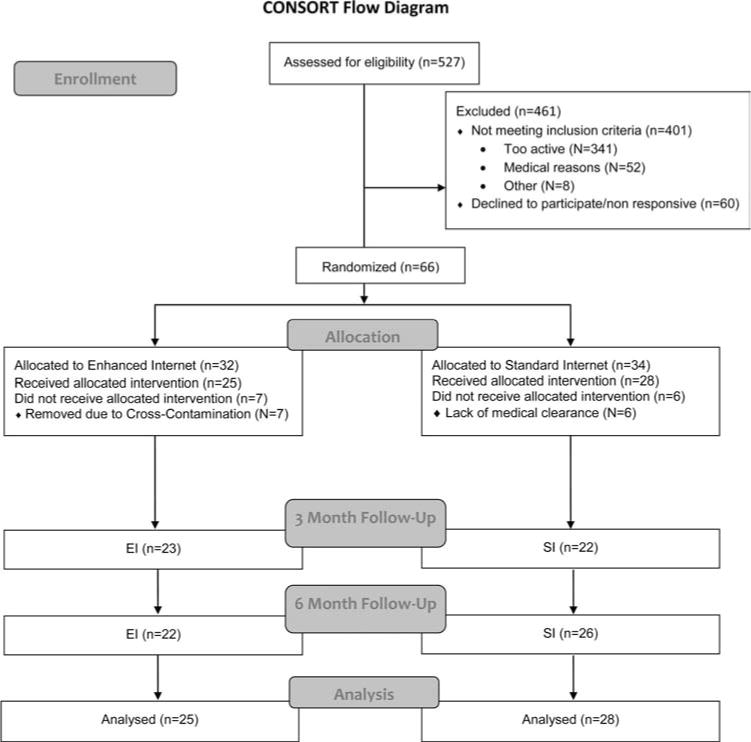
Sequence of events and recruitment/enrollment schematic. Study was coordinated at Brown University, Providence, Rhode Island, from February 2010through February 2011.
Table 1. Baseline Participant Characteristics by Treatment Condition (N = 53).
| EI (n = 25), no. (%) or M (SD) | SI (n = 28), no. (%) or M (SD) | P value | |
|---|---|---|---|
| Age, years | 38.5 (13.1) | 36.8 (11.1) | 0.61 |
| Percentage women | 80.0% | 71.4% | 0.47 |
| Body mass index (kg/m2) | 31.4 + 1.1 | 31.0 + 0.7 | 0.12 |
| Non-Hispanic White | 92.0% | 82.1% | 0.29 |
| College graduate | 52.0% | 64.3% | 0.36 |
| Household income <$40,000 | 56.0% | 57.1% | 0.93 |
| Married | 36.0% | 50.0% | 0.30 |
| Baseline PA (minutes/week) | 18.4 (27.0) | 20.9 (28.6) | 0.74 |
Note. EI = enhanced Internet; SI = standard Internet; PA = physical activity.
Measures
The primary outcome for this study was PA behavior as assessed by the 7-day Physical Activity Recall (PAR; Blair et al., 1985; Sallis et al., 1985). The PAR has been used in numerous studies that have demonstrated its reliability and validity (Pereira et al., 1997), and there is substantial evidence that the PAR is sensitive to change in PA interventions trials (Dunn et al., 1999b; Marcus, Lewis, Williams, Dunsiger, et al., 2007; Marcus, Napolitano, et al., 2007a). The 7-day PAR was administered over the telephone, by the same, certified interviewer at baseline, 3 months, and 6 months. Participants in the EI arm completed monthly Internet questionnaires assessing Self-Efficacy (Marcus, Selby, Niaura, & Rossi, 1992) Decisional Balance (Marcus, Rakowski, & Rossi, 1992), Behavioral/Cognitive Processes of Change (Marcus, Rossi, Selby, Niaura, & Abrams, 1992), and Outcome Expectations for Exercise (Resnick, Zimmerman, Orwig, Furstenberg, & Magaziner, 2000). Data from these questionnaires were used to generate automated motivationally targeted (TTM) feedback reports addressing specific barriers to PA. Participants randomized to the SI arm completed monthly questionnaires focused on non-PA related health topics (e.g., nutrition, health screens) to control for the number of contacts between the participants and the research staff between the two conditions. Participants in both groups were given a $10 incentive for completing monthly questionnaires and $25 incentives for completing the 3-month and 6-month assessments. The study Web developers provided Webuse data that objectively monitored participants' use (e.g., logins) of the Website. At 3 months, participants randomized to the EI arm completed a questionnaire designed to assess participant's perception of each Internet feature's helpfulness for increasing his or her PA. This questionnaire was based on a 5-point Likert scale (1 = not at all useful; 2 = a little useful; 3 = moderately useful; 4 = quite useful; 5 = extremely useful).
Intervention Arms
We used a block randomization procedure with random-sized blocks (2– 6) to assign participants to treatment arms. The randomization scheme was developed using MATLAB R2008b. On the basis of the randomization schedule, we created sequentially numbered envelopes that included treatment assignments. Envelopes were signed and sealed to ensure confidentiality. A research assistant who was unaware of the randomization schedule opened the envelopes at the time of enrollment and informed each participant his or her treatment assignment. Immediately following group assignment, participants were sent an e-mail with a URL address to the study homepage as well as a username and password to enter their group-specific Website. Participants were explained their study responsibilities and received training in navigating their group-specific Websites. A separate research assistant remained unaware of participant treatment assignment and was responsible for all primary and secondary data collection.
Enhanced Internet (EI)
Participants randomized to the EI arm were given a long-term goal of accumulating a minimum of 150 min of moderate intensity PA each week in continuous bouts of at least 10 min in duration. Participants were educated on how to assess the intensity of their PA through monitoring their rating of perceived exertion (RPE; Borg, 1982) and heart rate. EI group participants were given access to our newly developed Website, which was an enhanced version of our previously demonstrated Step into Motion Website. As a carry-over component of the Step into Motion Website, EI participants received immediate, individually tailored, motivational (TTM) PA messages generated by a computerized expert system after completing monthly online questionnaires (Marcus, Lewis, Williams, Whiteley, et al., 2007). The reports provided information consisting of preplanned counseling messages written by doctoral-level psychologists who have experience in health behavior change. The messages targeted participants' barriers to and expected benefits from PA in addition to reinforcing successful use of strategies for PA adoption. These materials were matched to the individual's Stage of Motivational Readiness for PA adoption.
In addition to the feedback reports, the EI Website included the five SCT-influenced Internet features identified as most useful by participants in the focus groups (see Table 2). For example, participants were able to access the geographic mapping tool, which allowed participants to create, save, and print local online walking/biking paths. Several features were updated regularly in order to model the dynamic nature of the Internet by providing users with new and engaging content to promote increased logins throughout the 6-month intervention period. New answers to participant questions related to PA were posted weekly through an online Ask the Expert question-and-answer forum and regular updates were provided regarding participant's peer PA progress (e.g., “Participants reported an average of 85 minutes of moderate intensity PA this week.”).
Table 2. Description of Theory-Targeted Internet Feature Enhancements.
| Internet feature | Targeted SCT construct | Description of feature |
|---|---|---|
| Physical activity tracking & goal-setting calendar | Self-monitoring | The PA tracking calendar promoted self-monitoring of daily PA (e.g., activity type, minutes of activity, intensity of activity, number of steps taken). Participants were encouraged to set goals by choosing one of many enjoyable, short-term challenges (e.g., walk 15 min per day for 30 days). Participants were mailed a pedometer to assist in steps monitoring. Users received real-time progress feedback (% completed) each time a new daily activity was logged. |
| Regular peer activity updates | Situation | Regular updates of user-generated summary data were provided on the home page to inform participants on how they were doing in relation to others in the study, thereby educating participants on “healthful norms” PA behavior (e.g., average number of daily steps logged). |
| Ask the Expert Q&A forum | Social support | Participants were able to post exercise- and health-related questions on a threaded discussion forum that was monitored by a doctoral level research team member with expertise in exercise science and PA promotion. Responses were posted anonymously on a public bulletin board system, which all participants were able to view and respond to. |
| Exercise videos | Observational learning | A library of online videos modeling moderate intensity physical activities (i.e., step aerobics, yoga, Pilates, home-based resistance training) was posted to encourage the targeted behavior of moderate intensity PA. |
| Geographic mapping functions | Environment & situation | A geographic mapping tool was provided to target participants' perceptions about their PA environment, which allowed users to find, create, save, print, and share local walking/biking paths. Contextual information about local PA facilities was also posted to educate participants about available/local PA resources. |
Note. SCT = social–cognitive theory; PA = physical activity; Q&A = question and answer.
From the homepage, participants were able to access all Internet features and were encouraged to access these features on a regular basis. EI participants were e-mailed regular prompts (e.g., weekly during Month 1, biweekly during Months 2–3, and monthly during Months 4 – 6), reminding them to access the Website. Participants were asked to record their PA on the Website daily by logging the number of minutes of moderate intensity PA or daily steps that they had completed. Participants were mailed a pedometer to assist in step monitoring. These data were summarized in an interactive tracking calendar that provided feedback on individual progress.
When examining Website use (e.g., number of unique days with at least one login), the EI group logged on an average of 18.3 times over the first 3 months and a total of 32.3 times over the entire 6-month intervention. When asked to rate the helpfulness of each of the newly added Internet features for increasing his or her PA on a 5-point Likert scale at Month 6, EI participants (N = 21) rated the geographic mapping feature targeting perceived environment (M = 3.67) and the PA tracking calendar (3.52) as moderately to quite helpful, and rated the discussion forum (2.81), peer updates (2.74), and exercise videos (2.53) as little to moderately helpful.
Standard Internet (SI)
Participants randomized to the SI arm received access to a list of six reputable, publicly available PA-promoting Websites that have been demonstrated to increase PA and successfully retain participants in one of our previous trials (Marcus, Lewis, Williams, Whiteley, et al., 2007). The six Websites included the following: (1) the American Heart Association; (2) Shape Up America; (3) the Mayo Clinic; (4) American Academy of Family Physicians; (5) American Council on Exercise (ACE); and (6) American College of Sports Medicine (ACSM) (see Table 3). We selected these six Websites on the basis of the following criteria: (1) no cost to the participant; (2) easily accessible; (3) operational for at least 5 years; and (4) included accurate and useful information regarding PA promotion. In order to track Website use of the SI arm, participants were asked to access the six Websites by first logging onto the study homepage, which contained links to the Websites. The SI arm received regular e-mail prompts on the same schedule and for the same period of time as did those in the EI arm. Participants were provided unlimited access to the SI Website throughout the 6 months of the study.
Table 3. Description of Theory-Targeted Internet Features of Control Group Websites.
| Organization | Website address | Interactive features | SCT theory |
|---|---|---|---|
| American Heart Association | http://www.startwalkingnow.org | Walking path finder | Environment |
| PA tracker | Monitoring | ||
| Find a walking buddy | Social support | ||
| Shape Up America | http://www.shapeup.org | Body fat calculator | Monitoring |
| Mayo Clinic Fitness Center | http://www.mayoclinic.com/health/fitness/MY00396 | Exercise videos | Observational learning |
| Expert feedback | Social support | ||
| American Academy of Family Physicians | http://familydoctor.org/healthfacts/059/ | Exercise videos | Observational learning |
| American Council on Exercise | http://www.acefitness.org/getfit/default.aspx | Exercise videos | Observational learning |
| Calorie calculator | Monitoring | ||
| Ask the expert | Social Support | ||
| Discussion boards | Social support | ||
| American College of Sports Medicine | http://www.acsm.org | Exercise videos | Observational learning |
| Self-assessment log | Goal setting |
Note. SCT = social–cognitive theory; PA = physical activity.
When examining SI Website use, the SI group logged on an average of 5.3 times over the first 3 months and a total of 9.4 times over the entire 6-month intervention. However, because of the use of external and publicly available Websites, we may have been unable to accurately track SI participant's login frequency.
Statistical Analyses
To assess potential between-groups differences in baseline characteristics, we used analysis of variance (ANOVA) for continuous outcomes and chi-squared test for categorical variables. Data analysis focused on the primary hypothesis of testing PA differences between the EI and SI arms at 3 and 6 months. The number of minutes of at least moderate intensity activity (as measured by the 7-day PAR) was considered the primary variable of interest. Analysis was conducted on the intent to treat (ITT). To test for between-groups differences, we used a repeated-measures regression model implemented with generalized estimating equations (GEE) with robust standard errors, which adjusts standard errors to account for repeated measurements (Zeger & Liang, 1986). GEE's make use of all available data without directly imputing the missing outcomes. Using a similar model, we assessed within-group changes in minutes per week of PA from baseline to 3 months and baseline to 6 months. In addition, we compared percentage meeting national PA guidelines using chi-squared tests at both 3 months and 6 months. We assumed that those with missing outcomes did not meet PA guidelines.
Results
Participants assigned to the EI and SI conditions did not differ in demographic or behavioral characteristics (see Table 3). At baseline, participants randomized to the EI arm reported an average of 18.4 min/wk of PA (SD = 27.0), in comparison with 20.9 min/wk (SD = 28.6) among SI participants. Estimated marginal mean minutes of weekly PA at 3 and 6 months are presented in Table 4. Results suggest that the treatment effect was significant at 3 months, c2(1, 53) = 4.78, p = .03, but not at 6 months, c2(1, 53) = 0.61, p = .44. However, within-group changes from 3 to 6 months were not significant for EI participants (Z = 0.11, p = .91) but were significant for SI participants (Z = 2.38, p = .02). More EI participants were meeting the PA guidelines of 150 min of moderate-intensity PA at 3 months in relation to SI participants (40.0% vs. 10.7%), c2(1, 53) = 6.11, p = .01, but no between-groups difference was observed at 6 months (48.0% vs. 35.7%), c2(1, 53) = 0.82, p = .36.
Table 4. Estimated Weekly Minutes of Physical Activity at 3 and 6 Months by Treatment Condition, Adjusted for Baseline PA.
| Intervention period | EI | SI |
|---|---|---|
| 3-month PA (minutes/week) | 180.4 (57.5) | 46.3 (17.1) |
| 6-month PA (minutes/week) | 171.4 (46.9) | 121.8 (33.0) |
Note. Means and standard errors are reported. EI = enhanced Internet; SI = standard Internet; PA = physical activity.
Discussion
Our findings suggest that a non-face-to-face, user- and theory-guided Internet PA program is more efficacious for producing immediate increases in PA among sedentary adults than what is currently available to the public. For instance, more EI participants were meeting the federal PA guidelines of 150 min of moderate intensity PA per week at 3 months (40% vs. 10%) and nearly half of all EI participants (48%) were meeting guidelines at 6 months. This finding is clinically important because few randomized controlled Internet PA interventions have demonstrated differences in PA levels over a control group (Ciccolo, Lewis, & Marcus, 2008). However, the difference in PA levels at 3 months did not persist through 6 months. The lack of between-groups differences at 6 months appears to be due to gains in PA levels within the SI group from 3 months to 6 months rather than decreased PA among the EI group. The delayed increase in PA among the SI group was unexpected because no previous studied to our knowledge have reported such findings in a similar group. It is possible that the observed gain in PA among the SI group was due to increased Website use, although as previously noted, we were unable accurately track SI Website use because of the use of external Websites. It is also plausible that the EI Website provided the adequate tools for participants to jump-start their PA behavior, change that took longer among a group of comparably motivated Web users.
The volume of change in moderate-intensity PA observed in the EI group from baseline to 6 months (158 min/wk) has been repeatedly shown to result in improvements in risk for chronic disease and functional capacity (Haskell, Blair, & Hill, 2009). In past Internet PA studies, change in PA has consistently been correlated to measures of user engagement as measured by logins (Carr et al., 2008; Marcus, Lewis, Williams, Dunsiger, et al., 2007). On the basis of our Website-use data, EI participants accessed the Website an average of 32.3 times over 6 months or 1.3 times per week. Although we asked SI participants to access only the publicly available Websites via our homepage, it was possible for SI participants to bookmark the external Websites and log on to them directly; therefore this is a limitation of the study.
This study contributes to the field in multiple ways. First, we delivered this program remotely from our facilities in Providence, Rhode Island, to residents of three different states using a completely non-face-to-face format. Few completely non-face-to-face Internet PA interventions have demonstrated positive findings. Recently, Anderson-Bill et al. conducted a large scale, purely online Internet trial (Web-Based Guide to Health) targeting nutrition, PA, and weight-gain prevention (Anderson-Bill, Winett, & Wojcik, 2011; Anderson-Bill, Winett, Wojcik, & Winett, 2011). We believe the Guide to Health trial and our study can serve as models for future non-face-to-face Internet PA interventions.
Second, the present study used formative research methods to identify and include interactive Internet features rated as appealing and targeted to specific theoretical constructs shown to predict PA in our previous trials (Anderson-Bill, Winett, Wojcik, & Winett, 2011). Although our group had preconceived notions of features that would be rated as most useful for improving PA (e.g., social networking features) on the basis of our work in previous trials, this process was beneficial in identifying features that were perceived as most useful for our specific population. Participants of this study rated the geographic features targeting perceived environment the highest followed by the PA Tracking Calendar. Few Internet PA trials of this kind have demonstrated this level of examination. One such study that has conducted such examination is the previously mentioned study by Anderson-Bill et al., which demonstrated improvements in PA behavior and weight loss that were shown to be associated with improvements in various SCT constructs including social support, self-efficacy, outcome expectations, and self-regulation (Anderson-Bill, Winett, Wojcik, & Williams, 2011; Anderson-Bill, Winett, Wojcik, & Winett, 2011). The present data warrant further exploration as to why the added features were rated highest and whether specific features were more helpful in the short term or the long term.
Third, our findings indicate that this completely non-face-to-face intervention can increase PA among previously sedentary adults. Given the equivocal findings of previous studies, this is important in moving the field forward. Although most Internet PA trials have failed to observe between-groups differences in PA behavior, our study demonstrated between-groups differences at Month 3, suggesting that the EI intervention facilitated quicker increases in PA behavior than did the SI comparison arm. It is now necessary to identify the specific features that had the largest impact in improving PA behavior in the EI arm from baseline to 3 months. It would also be helpful to explore which features participants in the EI arm were using, when they were using those features, and how specific feature use overlapped with increases in PA behavior. Such a pattern analysis would help decipher whether specific Internet features were responsible for the early improvements in PA, which is necessary for long-term adherence.
Equally important questions remain in identifying ways to continue the increase in PA from Month 3 to Month 6. Although the present study was limited by sample size prohibiting such analyses, these findings support a larger trial to test: (1) whether participant use of theory-guided Internet features impacts the targeted theoretical constructs and whether this relates to change in PA behavior; (2) whether our program can sustain behaviors long term (e.g., 12 months posttreatment); and (3) which Internet features predict long-term behavior. It is also necessary to explore possible reasons for the lagged improvement among the SI participants from Month 3 to Month 6. It is possible that there were specific features offered within the SI Websites that participants used, and given the lagged but pronounced response in PA among SI participants, these features could be useful to include in future Internet PA trials.
The findings of this study should be read with caution because the associations between participant perceptions of individual features and change in PA behaviors is not sufficient to suggest a causal relationship. Also, the generalizability of our findings is limited because of the primarily female, middle-aged and non-Hispanic White population of adults included. Such demographic characteristics are typical of participants in Internet PA studies. However, only slightly more than half of all participants were college educated, and more than half reported a household income of less than $40,000 per year, indicating that the sample had less education and a lower income than did typical populations in this area of study. Further mediator analyses focusing on use of each theory-targeted feature is also warranted. It is likely that a program targeting a different population such as younger or older adults would require different features for successful behavior change, and researchers are encouraged to explore such features. Finally, the present study is limited by a relatively small sample size and self-report PA data.
Conclusions
The Internet has the potential to make a significant public health impact on sedentary behavior through wide-scale dissemination (Bennett & Glasgow, 2009). However, in order to develop successful, dissemination ready Internet PA interventions, it is necessary that future studies continue to test the ever-evolving Internet technologies. Future studies must include cell phone technology as a means of increasing intervention reach and allowing users to access materials and through multiple channels (Webb et al., 2010). Interactive and engaging features of Web 2.0 sites have changed the expectations of Internet users; thus public health intervention Websites must adhere to the new Web 2.0 design principles, including dynamic designs in which the content adapts on the basis of user input. Consistently, as has been proposed previously (Collins, Murphy, & Strecher, 2007), future Internet PA interventions should explore multiphase optimization strategies (MOST) in which systems-based approaches are used to adapt intervention content and delivery based on participant input.
Acknowledgments
We would like to sincerely thank Jaime Longval, Santina Horowitz, Michele Ruttenberg, and Rachelle Edgar for their contributions to this study.
Contributor Information
Lucas J. Carr, Department of Kinesiology, East Carolina University, Centers for Behavioral and Preventive Medicine, Miriam Hospital, Providence, RI, and Warren Alpert Medical School at Brown University
Beth Lewis, School of Kinesiology, University of Minnesota.
Sheri Hartman, Department of Family and Preventive Medicine, University of California, San Diego.
Gregory Dominick, Department of Behavioral Health and Nutrition, University of Delaware.
Shira I. Dunsiger, Centers for Behavioral and Preventive Medicine, Miriam Hospital, Providence, RI, and Warren Alpert Medical School at Brown University
Joseph T. Ciccolo, Centers for Behavioral and Preventive Medicine, Miriam Hospital, Providence, RI, and Warren Alpert Medical School at Brown University
Beth Bock, Centers for Behavioral and Preventive Medicine, Miriam Hospital, Providence, RI, and Warren Alpert Medical School at Brown University.
Bess H. Marcus, Department of Family and Preventive Medicine, University of California, San Diego
References
- Anderson-Bill ES, Winett RA, Wojcik JR. Social cognitive determinants of nutrition and physical activity among Web-health users enrolling in an online intervention: The influence of social support, self-efficacy, outcome expectations, and self-regulation. Journal of Medical Internet Research. 2011;13:147. doi: 10.2196/jmir.1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson-Bill ES, Winett RA, Wojcik JR, Williams DM. Aging and the social cognitive determinants of physical activity behavior and behavior change: Evidence from the guide to health trial. Journal of Aging Research. 2011;2011:505928. doi: 10.4061/2011/505928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson-Bill ES, Winett RA, Wojcik JR, Winett SG. Web-based guide to health: Relationship of theoretical variables to change in physical activity, nutrition and weight at 16-months. Journal of Medical Internet Research. 2011;13:124. doi: 10.2196/jmir.1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York, NY: W. H. Freeman; 1997. [Google Scholar]
- Baranowski T, Perry CL, Parcel GS. Social ccognitive theory. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: Theory research and practice. 3. San Francisco, CA: Jossey-Bass; 2002. pp. 165–181. [Google Scholar]
- Bennett GG, Glasgow RE. The delivery of public health interventions via the Internet: Actualizing their potential. Annual Review of Public Health. 2009;30:273–292. doi: 10.1146/annurev.publhealth.031308.100235. [DOI] [PubMed] [Google Scholar]
- Blair SN. Physical inactivity: The biggest public health problem of the 21st century. British Journal of Sports Medicine. 2009;43:1–2. [PubMed] [Google Scholar]
- Blair SN, Haskell WL, Ho P, Paffenbarger RS, Jr, Vranizan KM, Farquhar JW, Wood PD. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. American Journal of Epidemiology. 1985;122:794–804. doi: 10.1093/oxfordjournals.aje.a114163. [DOI] [PubMed] [Google Scholar]
- Borg G. Ratings of perceived exertion and heart rates during short-term cycle exercise and their use in a new cycling strength test. International Journal of Sports Medicine. 1982;3:153–158. doi: 10.1055/s-2008-1026080. [DOI] [PubMed] [Google Scholar]
- Carr LJ, Bartee RT, Dorozynski C, Broomfield JF, Smith ML, Smith DT. Internet-delivered behavior change program increases physical activity and improves cardiometabolic disease risk factors in sedentary adults: Results of a randomized controlled trial. Preventive Medicine. 2008;46:431–438. doi: 10.1016/j.ypmed.2007.12.005. [DOI] [PubMed] [Google Scholar]
- Ciccolo JT, Lewis B, Marcus BH. Internet-based physical activity interventions. Current Cardiovascular Risk Reports. 2008;2:299–304. [Google Scholar]
- Collins LM, Murphy SA, Strecher V. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): New methods for more potent eHealth interventions. American Journal of Preventive Medicine. 2007;32(5, Suppl. 1):S112–S118. doi: 10.1016/j.amepre.2007.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, III, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: A randomized trial. Journal of the American Medical Association. 1999a;281:327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, III, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: A randomized trial. Journal of the American Medical Association. 1999b;281:327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- Ferney SL, Marshall AL. Website physical activity interventions: Preferences of potential users. Health Education Research. 2005;21:560–566. doi: 10.1093/her/cyl013. [DOI] [PubMed] [Google Scholar]
- Graham AL, Cobb NK, Raymond L, Sill S, Young J. Effectiveness of an Internet-based worksite smoking cessation intervention at 12 months. Journal of Occupational and Environmental Medicine. 2007;49:821–828. doi: 10.1097/JOM.0b013e3180d09e6f. [DOI] [PubMed] [Google Scholar]
- Haskell WL, Blair SN, Hill JO. Physical activity: Health outcomes and importance for public health policy. Preventive Medicine. 2009;49:280–282. doi: 10.1016/j.ypmed.2009.05.002. [DOI] [PubMed] [Google Scholar]
- Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Education Research. 2008;23:454–466. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins A, Christensen H, Walker JG, Dear K. The effectiveness of distance interventions for increasing physical activity: A review. American Journal of Health Promotion. 2009;24:102–117. doi: 10.4278/ajhp.0801158. [DOI] [PubMed] [Google Scholar]
- Lewis B, Williams D, Dunsiger S, Sciamanna C, Whiteley J, Napolitano M, … Marcus BH. User attitudes towards physical activity Websites in a randomized controlled trial. Preventive Medicine. 2008;47:508–513. doi: 10.1016/j.ypmed.2008.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis BA, Williams DM, Neighbors CJ, Jakicic JM, Marcus BH. Cost analysis of an internet and print intervention for physical activity promotion. Psychology of Sport & Exercise. 2010;11:246–249. doi: 10.1016/j.psychsport.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus BH, Bock BC, Pinto BM, Forsyth LH, Roberts MB, Traficante RM. Efficacy of an individualized, motivationally tailored physical activity intervention. Annals of Behavioral Medicine. 1998;20:174–180. doi: 10.1007/BF02884958. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Ciccolo JT, Sciamanna CN. Using electronic/computer interventions to promote physical activity. British Journal of Sports Medicine. 2008;43:102–105. doi: 10.1136/bjsm.2008.053744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus BH, Lewis BA, Williams DM, Dunsiger S, Jakicic JM, Whiteley JA, Parisi AF. A comparison of Internet and print-based physical activity interventions. Archives of Internal Medicine. 2007;167:944–949. doi: 10.1001/archinte.167.9.944. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Lewis BA, Williams DM, Whiteley JA, Albrecht AE, Jakicic JM, … Bock BC. Step into motion: A randomized trial examining the relative efficacy of Internet vs. print-based physical activity interventions. Contemporary Clinical Trials. 2007;28:737–747. doi: 10.1016/j.cct.2007.04.003. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Napolitano MA, King AC, Lewis BA, Whiteley JA, Albrecht A, et al. Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project STRIDE. Health Psychology. 2007a;26:401–409. doi: 10.1037/0278-6133.26.4.401. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Napolitano MA, King AC, Lewis BA, Whiteley JA, Albrecht AE, et al. Examination of print and telephone channels for physical activity promotion: Rationale, design, and baseline data from Project STRIDE. Contemporary Clinical Trials. 2007b;28:90–104. doi: 10.1016/j.cct.2006.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus BH, Rakowski W, Rossi JS. Assessing motivational readiness and decision making for exercise. Health Psychology. 1992;11:257–261. doi: 10.1037/0278-6133.11.4.257. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychology. 1992;11:386–395. doi: 10.1037/0278-6133.11.6.386. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Research Quarterly for Exercise and Sport. 1992;63:60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Mummery WK, Schofield G, Hinchliffe A, Joyner K, Brown W. Dissemination of a community-based physical activity project: The case of 10,000 steps. Journal of Science and Medicine in Sport. 2006;9:424–430. doi: 10.1016/j.jsams.2006.06.015. [DOI] [PubMed] [Google Scholar]
- Napolitano MA, Fotheringham M, Tate D, Sciamanna C, Leslie E, Owen N, … Marcus BH. Evaluation of an Internet-based physical activity intervention: A preliminary investigation. Annals of Behavioral Medicine. 2003;25:92–99. doi: 10.1207/S15324796ABM2502_04. [DOI] [PubMed] [Google Scholar]
- National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP). Behavioral risk factor surveillance system: Prevalence and trends data for physical activity in 2007. 2007 Retrieved March 17, 2009, from http://apps.nccd.cdc.gov/brfss.
- National Physical Activity Plan; Paper presented at the National Physical Activity Plan Conference; Washington, DC. 2009. Jul, [Google Scholar]
- Pereira MA, FitzerGerald SJ, Gregg EW, Joswiak ML, Ryan WJ, Suminski RR, … Zmuda JM. A collection of Physical Activity Questionnaires for health-related research. Medicine and Science in Sports and Exercise. 1997;29(6, Suppl):S1–S205. [PubMed] [Google Scholar]
- Petersen R, Sill S, Lu C, Young J, Edington DW. Effectiveness of employee Internet-based weight management program. Journal of Occupational and Environmental Medicine. 2008;50:163–171. doi: 10.1097/JOM.0b013e31815c6cf6. [DOI] [PubMed] [Google Scholar]
- Pew Internet. Internet and American Life Project: Fall tracking survey. 2008 Retrieved from http://www.pewinternet.org/Reports/2009/8-The-Social-Life-of-Health-Information/3-Exercise-or-fitness/1-Information-about-exercise-or-fitness.aspx?r=1.
- Pew Internet. Internet and American Life Project. 2009 Oct 30; Retrieved November 12, 2009, from http://www.pewinternet.org/Trend-Data.
- Plotnikoff RC, McCargar LJ, Wilson PM, Loucaides CA. Efficacy of an E-mail intervention for the promotion of physical activity and nutrition behavior in the workplace context. American Journal of Health Promotion. 2005;19:422–439. doi: 10.4278/0890-1171-19.6.422. [DOI] [PubMed] [Google Scholar]
- Rees T. More Americans going online looking for health information. Healthcare Marketing. 2005;21:2. [PubMed] [Google Scholar]
- Resnick B, Zimmerman SI, Orwig D, Furstenberg AL, Magaziner J. Outcome expectations for exercise scale: Utility and psychometrics. Journals of Gerontology: Series B Psychological Sciences and Social Sciences. 2000;55B:S352–S356. doi: 10.1093/geronb/55.6.S352. [DOI] [PubMed] [Google Scholar]
- Ries AV, Dunsiger S, Marcus BH. Physical activity interventions and changes in perceived home and facility environments. Preventive Medicine. 2009;49:515–517. doi: 10.1016/j.ypmed.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, Paffenbarger RS., Jr Physical activity assessment methodology in the Five-City Project. American Journal of Epidemiology. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- Stewart DW, Shamdasani PN, Rook DW. Focus groups: Theory and practice. Vol. 20. Thousand Oaks, CA: Sage; 2007. [Google Scholar]
- U.S. Department of Health and Human Services. Physical Activity Guidelines Advisory Committee Report to the Secretary of Health and Human Services. 2008 Retrieved June 1, 2009, from http://www.health.gov/PAGuidelines/committeereport.aspx.
- Vandelanotte C, Spathonis KM, Eakin EG, Owen N. Website-delivered physical activity interventions a review of the literature. American Journal of Preventive Medicine. 2007;33:54–64. doi: 10.1016/j.amepre.2007.02.041. [DOI] [PubMed] [Google Scholar]
- van den Berg B, Yzermans CJ, van der Velden PG, Stellato RK, Lebret E, Grievink L. Are physical symptoms among survivors of a disaster presented to the general practitioner? A comparison between self-reports and GP data. BMC Health Services Research. 2007;7:150. doi: 10.1186/1472-6963-7-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb TL, Joseph J, Yardley L, Michie S. Using the Internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research. 2010;12:e4. doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. doi: 10.2307/2531248. [DOI] [PubMed] [Google Scholar]


