Abstract
Men who have sex with men (MSM) can reduce their risk of acquiring human immunodeficiency virus (HIV) by using various prevention strategies and by understanding the effectiveness of each option over the short- and long-term. Strategies examined were: circumcision; insertive anal sex only; consistent, 100% self-reported condom use; and pre-exposure prophylaxis (PrEP). PrEP efficacy was based on three levels of adherence. The cumulative HIV acquisition risk among MSM over periods of 1 year and 10 years were estimated with and without single and combinations of prevention strategies. A Bernoulli process model was used to estimate risk.
In the base case with no prevention strategies, the 1-year risk of HIV acquisition among MSM was 8.8%. In contrast, the 1-year risk associated with circumcision alone was 6.9%; with insertive sex only, 5.5%; with 100% self-reported condom use, 2.7%; and with average, high, and very high PrEP adherence, 5.1%, 2.5%, and 0.7%, respectively. The 10-year risk of HIV acquisition among MSM with no prevention strategy was 60.3%. In contrast, that associated with circumcision alone was 51.1%; with insertive sex only, 43.1%; with 100% self-reported condom use, 24.0%; and with average, high, and very high PrEP adherence, 40.5%, 22.2%, and 7.2%, respectively. While MSM face substantial risk of HIV, there are now a number of prevention strategies that reduce risk. Very high adherence to PrEP alone or with other strategies appears to be the most powerful tool for HIV prevention.
Keywords: HIV, HIV infections, prevention & control, pre-exposure prophylaxis, condoms, unsafe sex, risk reduction behavior, United States
An estimated 1.2 million people in the United States were living with human immunodeficiency virus (HIV) at the end of 2013; of these, 55% were men who have sex with men (MSM) (1). Of the new HIV diagnoses among adults in 2013, about 68% were in MSM, some of whom were also injection drug users (2). Furthermore, while the annual number of HIV diagnoses for all other groups decreased in 2009 – 2013, it increased among MSM, from 27 394 to 30 689 (2).
The majority of HIV infections among MSM occur through sexual transmission. Among males living with HIV, more than 70% of infections were attributable to male-to-male sexual contact (1). A previous analysis (3) reported on the effectiveness of single and combination prevention strategies over time on reducing the risk of HIV transmission among serodiscordant MSM and heterosexual couples. It found relatively high levels of HIV acquisition risk over time, unless prevention strategies were combined.
This analysis evaluated how MSM who are at risk for acquiring HIV and are unaware of their partner’s serostatus can reduce their risk by using single and combination prevention strategies. Four strategies were assessed, both singly and combined with the others: circumcision; insertive anal sex only, i.e., no receptive anal sex; consistent (100% adherence) condom use; and pre-exposure prophylaxis (PrEP). For PrEP efficacy, three levels were evaluated—average, high, and very high—based on observed adherence in clinical trials (4). Because HIV prevalence may vary widely in the communities from which MSM choose their partners, the analysis also examined the effectiveness of prevention strategies among varying prevalence rates.
MATERIALS AND METHODS
The cumulative risk of HIV acquisition among MSM over 1 year and 10 years was estimated. A Bernoulli process model was used to estimate HIV risk without a prevention strategy in the base case (see Supplementary Materials; 3, 5); then the base case estimate was adjusted with each risk-reduction strategy separately and in combination. Risk ratios were assumed to be independent and multiplicative in assessing risk reduction with combination strategies (3, 6). The key input parameters used in the model included per-act HIV transmission probabilities with insertive and receptive anal sex, HIV risk-reduction strategies or risk modifiers, number of sex acts, and HIV prevalence among MSM partners (see Supplementary Materials). The analyses were conducted with Microsoft Excel™ (Microsoft Corp., Redmond, Washington, United States).
The input values used in the analysis for the per-act HIV transmission probability associated with unprotected (no condom use) insertive and receptive anal sex, the average number of sex acts per month (three insertive and three receptive anal sex acts per month), and the efficacy of male circumcision applied to only insertive anal acts have been described by Lasry and colleagues (3). An 18% (3% – 43%) HIV prevalence among sex partners was used—based on anonymous HIV testing of MSM in the 2011 National HIV Behavioral Surveillance System, a survey of MSM recruited through venue-based sampling in metropolitan statistical areas of the United States (7). The analysis assumed that 30% of MSM living with HIV would adhere to antiretroviral therapy (ART) and have a suppressed HIV ribonucleic acid (RNA) viral load, conferring on this model a 96% reduction in HIV transmission (8, 9).
An efficacy of 70% (95% Confidence Interval [95%CI]: 58% – 79%) was applied to 100% condom use, based on analyses of data from two HIV prevention trials in the United States that enrolled HIV- uninfected MSM (10). No efficacy was assumed if condoms were used less than 100% of the time, based on results from the same study. Three levels of adherence to PrEP were used based on the iPrEX trial results (4): average, as reported in an intention-to-treat analysis; high, based on pill count; and very high, based on study drug (emtricitabine and tenofovir disoproxil fumarate [FTC/TDF]) detection in blood samples. The corresponding efficacies were 44% (95% CI: 15% – 63%), 73% (95% CI: 41% – 88%), and 92% (95% CI: 40% – 99%), respectively (4).
Univariate sensitivity analysis on two parameters were conducted to explore potential variation in the risk estimates (see Supplementary Materials). The possibly wide variation in prevalence among the communities from which MSM may select their partners was explored. In addition, previous analyses have demonstrated that the number of HIV exposures—sex acts in this analysis—has a large effect on the risk of acquiring HIV. Therefore, similar to Lasry and colleagues (3), in this study the number of sex acts was assumed to vary from 2 – 20 per month, compared to the base case value of 6.
RESULTS
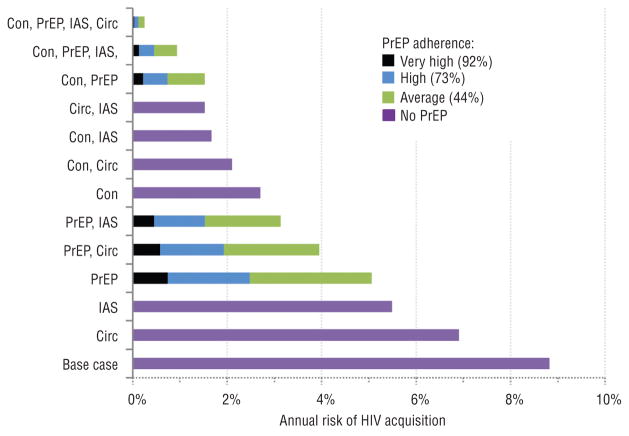
In the base case with no prevention strategies, the 1-year risk of HIV acquisition among MSM was 8.8% (Figure 1). In contrast, the 1-year risk associated with circumcision alone was 6.9%; with insertive sex only, 5.5%; with 100% self- reported condom use, 2.7%; and with average, high, and very high PrEP adherence, 5.1%, 2.5%, and 0.7%, respectively.
FIGURE 1.
Annual risk of Human Immunodeficiency Virus (HIV) acquisition among HIV-uninfected males who have sex with males, using combinations of prevention strategies—condom (CON), pre-exposure prophylaxis (PrEP), circumcision (Circ), insertive anal sex only (IAS)—or no strategy (base case), United States of America, 2015
Source: Prepared by the authors from the study data.
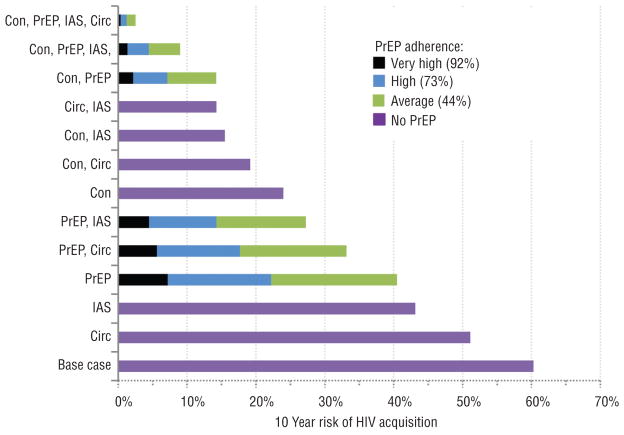
In the base case with no prevention strategies, the 10-year risk of HIV acquisition among MSM was 60.3% (Figure 2). In contrast, the 10-year risk associated with circumcision alone was 51.1%; with insertive sex only, 43.1%; with 100% self-reported condom use, 24.0%; and with average, high, and very high PrEP adherence, 40.5%, 22.2%, and 7.2%, respectively.
FIGURE 2.
The 10-year risk of Human Immunodeficiency Virus (HIV) acquisition among HIV-uninfected males who have sex with males, using combinations of prevention strategies—condom (CON), pre-exposure prophylaxis (PrEP), circumcision (Circ), insertive anal sex only (IAS)—or no strategy (base case), United States of America, 2015
Source: Prepared by the authors from the study data.
The most effective prevention combination—very high PrEP adherence, 100% condom use, circumcision, and insertive sex only—reduced 1-year acquisition risk to 0.04% and 10-year risk to 0.4%. The efficacy of other combinations of prevention strategies are presented in Figures 1 and 2.
When the adjusted HIV prevalence varied from 3% – 43% (base case: 18%), the 1-year HIV acquisition risk without prevention strategies ranged from 1.5% – 19.9% (base case risk: 8.8%; data not shown). With high adherence to PrEP, the 1-year acquisition risk ranged from 0.4% – 5.8% (base case risk: 2.5%).
When the number of sex acts per month varied from 2 – 20 (base case: 6), the 1-year HIV acquisition risk without prevention strategies ranged from 3.1% – 25.7% (base case risk: 8.8%). With high adherence to PrEP, the 1-year acquisition risk ranged from 0.8% – 8.0% (base case risk: 2.5%).
DISCUSSION
The risk of HIV acquisition was high among MSM in this analysis when no prevention strategies were employed, reaching 60% after 10 years of continuous exposure. At the highest level of adherence, PrEP was the single most protective strategy. However, at the average level of adherence—the level of adherence associated with the modified intention-to-treat analysis in the iPrEX trial (4)—PrEP was less protective than condoms alone when condoms were used to cover all sex acts. Combinations of strategies also were usually very protective, even among those not based on PrEP; for instance, circumcision among men who also practiced only insertive sex, decreased risk substantially.
High levels of adherence can be difficult to achieve. In the iPrEX trial on pre-exposure prophylaxis among MSM in several countries, only 51% of participants had a detectable level of the study drug in their blood sample, and for that group, PrEP was 92% efficacious (4). The overall efficacy of PrEP in iPrEX was 44% among participants with and without detectable drug in their blood sample. An iPrEX subgroup analysis evaluated adherence to the study drug among 510 participants. Of the 56 participants from the United States, 95% had any detectable levels of the study drug, and 57% had drug levels associated with consistent dosing (11). A multi-site demonstration project implemented in sexually-transmitted disease and community health clinics in the United States found 65% of the study participants had drug levels consistent with taking four or more doses per week, at all visits (12).
Furthermore, MSM frequently report less than 100% condom use. In the 2011 National HIV Behavioral Surveillance System (13), 57% of MSM who reported being HIV-negative or of unknown status, also reported having had anal sex in the prior 12 months without a condom and with a partner of any HIV status, i.e., positive, negative, or unknown (13). Among MSM who considered themselves HIV-negative, but tested positive, 33% reported that their most recent sex act was anal sex, unprotected by a condom and with a male partner of HIV-negative or unknown status. Among MSM who tested HIV-negative, 12% reported that their most recent sex act was anal sex unprotected by a condom with a male partner of HIV-positive or unknown status. Smith and colleagues found in their analyses of condom use and efficacy in 3 490 HIV-negative MSM, 35% of those having anal sex with a male partner of any HIV status reported sex without a condom at least once during any 6-month interval, as did 84% over all 6-month intervals assessed (10). In theory, use of condoms for some, even if not all sex acts should provide some protection from HIV. However, trials of condom effectiveness, where adherence can only be measured through self-report, have not demonstrated partial effectiveness.
Sensitivity analyses showed that the study results would be affected by the prevalence of HIV in the communities from which men choose partners, and the average number of sex acts. Higher prevalence and more sex acts both resulted in greater risk.
Limitations
This analysis has several limitations. Although the relative magnitude of effect would remain unchanged for the single and combination strategies assessed, a number of factors could alter absolute risk levels, including a change in the proportion of MSM in a community who have achieved viral load suppression and the increase or decrease in number and type of sex acts over time. In assessing combination strategies, we assumed that risk ratios were independent and multiplicative (3, 6). While it is possible that the efficacy of combined interventions would not be multiplicative, insufficient data were available to assess other possibilities. Furthermore, we assumed no change in risk behavior for the individual base case when estimating 10-year HIV acquisition risks under single or combinations of prevention strategies.
We attributed the protective effect of male circumcision to insertive sex acts, assuming a biological equivalence with insertive vaginal sex. However, because none of the randomized controlled trials of male circumcision included many MSM, definitive statements regarding the effect of male circumcision on the risk of acquiring HIV or other sexually transmitted infections cannot be made. In this analysis, where 50% of anal sex acts were assumed to be insertive and 50% receptive, the greater per-act transmission risk associated with receptive anal sex dwarfed the effect of circumcision, and circumcision alone reduced the 10-year risk of HIV acquisition from 60.3% to only 51.1%.
Lastly, this analysis does not factor in access, affordability, or cost differences between the different strategies, which could affect uptake among MSM. This analysis was designed to provide MSM with a measure of the potential benefits of HIV prevention strategies. However, individual decisions regarding these strategies could also be shaped by perceptions and understandings of HIV risk, potential stigma associated with engaging in HIV prevention efforts, perceived side effects, and adherence challenges.
Conclusions
In conclusion, while MSM face a substantial risk of acquiring HIV, they also may be able to access a number of prevention strategies to reduce that risk. Combinations of strategies generally work better than single strategies. Very high adherence to PrEP, either alone or combined with other strategies, may be the most powerful tool for HIV prevention. Analyses such as this one improve our understanding of HIV acquisition risk over the short- and long-term, and assist MSM in choosing prevention strategies best suited to personal preferences and circumstances.
Supplementary Material
Footnotes
Conflict of interests. None declared.
Disclaimer. Authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of the RPSP/PAJPH and/or PAHO. Likewise, the findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
References
- 1.United States Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2014. [Accessed on 28 May 2015];HIV/AIDS surveillance supplemental report. Available from: www.cdc.gov/hiv/library/reports/surveillance/
- 2.United States Centers for Disease Control and Prevention. [Accessed on 28 May 2015];HIV surveillance report. 2013 25 Available from: www.cdc.gov/hiv/library/reports/surveillance/ [Google Scholar]
- 3.Lasry A, Sansom SL, Wolitski RJ, Green TA, Borkowf CB, Patel P, et al. HIV sexual transmission risk among serodiscordant couples: assessing the effects of combining prevention strategies. AIDS. 2014;28(10):1521–9. doi: 10.1097/QAD.0000000000000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pinkerton SD, Abramson PR. The Bernoulli-process model of HIV transmission. In: Holtgrave D, editor. Handbook of economic evaluation of HIV prevention programs. New York: Springer; 1998. pp. 13–32. [Google Scholar]
- 6.Fox J, White PJ, Weber J, Garnett GP, Ward H, Fidler S. Quantifying sexual exposure to HIV within an HIV-serodiscordant relationship: development of an algorithm. AIDS. 2011;25(8):1065–82. doi: 10.1097/QAD.0b013e328344fe4a. [DOI] [PubMed] [Google Scholar]
- 7.Wejnert C, Le B, Rose CE, Oster AM, Smith AJ, Zhu J, et al. HIV infection and awareness among men who have sex with men-20 cities, United States, 2008 and 2011. PLoSOne. 2013;8(10):e76878. doi: 10.1371/journal.pone.0076878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bradley H, Hall HI, Wolitski RJ, Van Handel MM, Stone AE, LaFlam M, et al. Vital signs: HIV diagnosis, care, and treatment among persons living with HIV--United States, 2011. MMWR. 2014;63(47):1113–7. [PMC free article] [PubMed] [Google Scholar]
- 9.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith DK, Herbst JH, Zhang X, Rose CE. Condom effectiveness for HIV prevention by consistency of use among men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2015;68(3):337–44. doi: 10.1097/QAI.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 11.Amico KR, Marcus JL, McMahan V, Liu A, Koester KA, Goicochea P, et al. Study product adherence measurement in the iPrEx placebo-controlled trial: concordance with drug detection. J Acquir Immune Defic Syndr. 2014;66(5):530–7. doi: 10.1097/QAI.0000000000000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu A. Adherence, sexual behavior and HIV/STI incidence among men who have sex with men (MSM) and transgender women (TGW) in the US PrEP demonstration (Demo) project. IAS Conference on HIV Pathogenesis, Treatment, and Prevention; 19 – 22 July 2015; Vancouver, Canada. [Accessed on 14 August 2015]. Available from: www.ias2015.org/ [Google Scholar]
- 13.United States Centers for Disease Control and Prevention. HIV testing and risk behaviors among gay, bisexual, and other men who have sex with men - United States. MMWR. 2013;62(47):958–62. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.