Abstract
Psychotherapists routinely use both specific and non-specific strategies to deliver empirically supported treatments (ESTs). Psychotherapy adherence monitoring has traditionally focused on assessing therapist use of EST-specific strategies (to distinguish between ESTs), paying less attention to non-specific techniques common to multiple psychotherapies. This study used the Collaborative Study Psychotherapy Rating Scale (CSPRS) to evaluate therapist use of both specific and non-specific techniques in two affect-focused ESTs for depression. Blinded raters evaluated 180 recorded sessions of interpersonal psychotherapy (IPT) and brief supportive psychotherapy (BSP). Because IPT and BSP both emphasize attention to affective states and developing a warm therapy relationship, we expected overlap across scales measuring therapist warmth, empathy, and focus on feelings. In contrast, we expected differences in scales measuring therapist directiveness, as well as IPT- and BST-specific interventions. Results showed raters displayed good inter-rater reliability on primary subscales and could discriminate between two treatments with considerable overlap. Both IPT and BSP therapists used similarly high levels of non-specific, facilitative interventions. Expectedly, IPT therapists were more directive and used more IPT-specific strategies, while BSP therapists utilized more non-directive, supportive strategies. Unexpectedly, BSP therapists showed greater focus on feelings than IPT therapists. Exploratory analyses suggested that greater focus on feelings in early sessions was associated with greater depressive symptom reduction in the first eight weeks of treatment for both ESTs. Additional treatment adherence research is needed to investigate both shared and distinctive features of ESTs, as well as the effect of the relative use of specific versus non-specific interventions on psychotherapy outcomes.
Keywords: psychotherapy adherence, Interpersonal Psychotherapy, Brief Supportive Psychotherapy, evidence-based psychotherapy, common factors of psychotherapy
Psychotherapeutic techniques are often divided into “specific” and “non-specific” factors. Specific factors refer to techniques based on the theoretical orientation of a particular empirically-supported treatment (EST) and typifying its approach: for example, a transference interpretation in psychoanalysis or weighing the evidence for and against automatic thoughts in cognitive behavior therapy (CBT). Non-specific or common factors refer to elements not unique to a particular theoretical orientation (Butler & Strupp, 1986) but shared across many psychotherapies (Frank & Frank, 1993). Examples of common factors include developing a warm and confiding relationship with the therapist, establishing a healing setting in which the therapist facilitates the patient’s emotional arousal (Frank, 1971), problem confrontation (Weinberger, 1995), affective experiencing, and behavioral regulation (Karasu, 1986). A literature review of the common factors found that two of the most agreed-upon common techniques across studies were developing a therapeutic alliance and providing opportunity for emotional catharsis (Grencavage & Norcross, 1990). Although non-specific interventions are shared across most ESTs, the extent or frequency with which clinicians use particular common-factor techniques may differ substantially across treatments (Markowitz & Milrod, 2011) and may account for considerable variability in depression treatment outcome (e.g., Wampold, 2001). Too little research has attempted to assess simultaneously the extent to which therapists use both treatment-specific and common factors techniques within and across ESTs.
Systematic adherence monitoring is a key component of evaluating and delivering ESTs in research trials. ESTs, defined as “clearly specified psychological treatments shown to be efficacious in controlled research with a delineated population” (Chambless & Hollon, 1998, p. 7), are defined in structured treatment manuals that delineate specific techniques to use or avoid. Because treatment manuals alone cannot assure adherent treatment delivery (Miller & Binder, 2002), investigators have developed standardized measures of the extent to which therapists perform techniques prescribed by, and avoid techniques proscribed by, EST treatment manuals (Waltz, Addis, Koerner, & Jacobson, 1993). Without confirming that patients receive the treatments allegedly being delivered, researchers cannot evaluate therapeutic efficacy or ensure that ESTs, once deemed efficacious, are reliably delivered outside research settings. Further, therapists’ proportional use of defined psychotherapy strategies in sessions is unknown without psychotherapy adherence monitoring.
Despite the importance of adherence monitoring in understanding psychotherapy process and outcome, the number of published studies providing detailed psychotherapy adherence data in depression treatment trials is small relative to published outcome studies. Most published treatment adherence studies use assessment instruments that focus on EST-specific techniques and thus have relevance only to certain types of therapy (Barber & Crits-Christoph, 1996; Barber, Crits-Christoph, & Luborsky, 1996; Butler, Henry, & Strupp, 1995; Segal et al., 2002; Weck et al., 2011; Weck et al., 2013), thereby limiting meaningful comparison across different ESTs. In contrast, a very limited number of investigators have used broad-spectrum adherence measures to compare multiple EST-specific and common-factor techniques across treatment modalities (e.g., Dimidjian et al., 2006; Hill, O’Grady, & Elkin, 1992; Markowitz et al., 1998; Markowitz et al., 2000; Ogrodniczuk & Piper, 1999).
The most highly developed, broad spectrum measure of cross-treatment psychotherapy adherence is the Collaborative Study Psychotherapy Rating Scale (CSPRS), created for the multisite National Institute of Mental Health Treatment of Depression Collaborative Research Program (TDCRP). Its sixth and final version (CSPRS-6) evolved through extensive psychometric testing (Hollon, 1984) and by design assessed both non-specific psychotherapy factors and treatment-specific factors associated with cognitive-behavioral therapy (CBT), interpersonal psychotherapy (IPT), and clinical medication management. To date, little psychometric research has evaluated the ability of broad-spectrum adherence scales such as the CSPRS-6 to measure the relative use of both specific and non-specific strategies across ESTs. Although DeRubeis and colleagues examined the roles of both therapeutic alliance and therapy-specific techniques in the process of change during CBT (DeRubeis & Feeley, 1990; Feeley, DeRubeis, & Gelfand, 1999; Strunk et al., 2012), only two studies have examined the use of treatment-specific versus common factors strategies in IPT (Hill, O’Grady, & Elkin, 1992; Markowitz et al., 2000). Evidence showing that common factors techniques can have significant influence on treatment outcome (e.g., Wampold, 2001), and the difficulty EST therapists often face in balancing specific versus non-specific techniques within time-limited therapy sessions, make further research on the relative use of common and therapy-specific strategies in ESTs sorely needed. Addressing this gap in the literature, the current report examines how therapists used specific and non-specific strategies in two evidence-based, affect-focused, depression treatments, IPT and brief supportive psychotherapy (BSP), using the CSPRS-6 and a brief scale developed to assess key strategies of BSP. One challenge was: how discriminable are these two therapies? Only one previous study examined this, finding IPT and BSP were distinguishable in a randomized controlled trial treating depressed HIV-positive patients (Markowitz et al., 2000).
IPT (Weissman, Markowitz & Klerman, 2007) is a structured, time-limited, efficacious treatment for major depressive disorder (Cuijpers et al., 2011). IPT focuses on the reciprocal relationship between mood states and interpersonal problems that commonly trigger or exacerbate depressive episodes. Treatment focuses on one of four defined IPT problem areas: grief (complicated bereavement), social role transitions (a major change in life circumstances), role disputes (conflicts with a significant other), or interpersonal deficits (global difficulties establishing or maintaining relationships) (Swartz & Markowitz, 2009). IPT therapists help patients to understand the relationship between their symptoms and their current life stressors, to more effectively manage their interpersonal problems, and increase social support as ways to resolve depressive symptoms (Weissman, Markowitz & Klerman, 2007). IPT therapists work to develop a warm, supportive, trusting therapeutic alliance with patients. An affect-focused therapy, IPT attends to, and explores, both positive and negative affective states (Swartz, 2015), and the relationship of affect to interpersonal situations and events. Thus IPT should, in theory, rely heavily on such common psychotherapeutic techniques as facilitating a warm therapeutic relationship, providing support, and maintaining a strong emphasis on feeling states. Its semi-structured, time-limited model, however, leads IPT therapists to take a moderately directive stance, explicitly guiding in-session discussion of interpersonal issues and using IPT-specific techniques, including ‘coaching’ patients to improve specific aspects of interpersonal communication and function, in order to resolve identified interpersonal problems associated with their depressive symptoms.
Like IPT, BSP is a time-limited, affect-focused therapy. Rooted in Rogers’ Client-Centered Therapy, it relies primarily on the psychotherapeutic common factors as treatment strategies (Markowitz, 2014). BSP therapists maintain a warm, supportive stance but do not direct the content of therapy sessions—except to pursue and explore patients’ affective responses. Thus, BSP therapists allow patients to select the topic of conversation. They focus on listening carefully, reflecting, and clarifying patients’ feelings, while providing supportive comments that emphasize patients’ strengths (Markowitz, 2014). This limited, non-directive treatment focus has led to the increasing use of BSP as an active psychotherapy comparator condition to control for common therapy factors such as therapist attention, personal warmth and support, and a focus on the patient’s feeling states. As potential testament to the power of such non-specific factors, BSP has yielded similar outcomes when compared to several other ESTs for mood disorders (Markowitz, 2014). For example, BSP matched the outcome of IPT in a study of dysthymic patients (Markowitz et al., 2005) and CBT in a study of depressed HIV-positive patients (Markowitz et al., 1998). In a large, twelve-week study comparing pharmacotherapy alone or combined with BSP or with Cognitive Behavioral Analysis System of Psychotherapy (CBASP), chronically depressed treatment-resistant patients in the BSP and CBASP treatment arms displayed comparable remission and response rates (Kocsis et al., 2009).
Using the CSPRS-6 and a BSP-specific scale described below, we evaluated whether we could reliably assess therapist use of specific and non-specific factors in IPT and BSP. We hypothesized that IPT therapists would be more directive than BSP therapists and that the EST-specific scales would discriminate between the treatment-specific aspects of IPT and BSP. Additionally, we expected IPT and BSP therapists to use comparably low levels of CBT strategies. In contrast, we hypothesized that IPT and BSP therapists would receive similarly high scores for promoting the discussion of feeling states and for using common-factors techniques including therapist warmth and empathy. Finally, we conducted post hoc analyses to explore whether use of BSP-specific, IPT-specific, and non-specific affect-focused strategies assessed in weeks 2–4 of treatment were associated with depressive symptom change at treatment week 8.
Method
Study Participants and Treatment Trials
The University of Pittsburgh Institutional Review Board approved all research procedures and all patients provided written informed consent. We randomly selected recorded sessions of IPT and BSP from two randomized controlled trials completed in the same University of Pittsburgh research clinic between August 2009 and June 2013. In both trials, adults meeting current DSM-IV criteria for a non-psychotic major depressive disorder (MDD) episode of sufficient severity (documented by Structured Clinical Interview for DSM-IV [SCID; First, et al., 1995] and score ≥15 on the 25-item Hamilton Rating Scale for Depression [HRSD; Thase, Carpenter, Kupfer, & Frank, 1991]) were randomly assigned to receive either BSP or an adapted version of IPT. The adaptations of IPT did not alter underlying IPT theory or basic strategies. Change in depressive symptoms was measured using the HRSD administered in each week of active treatment by clinicians blinded to treatment assignment.
In Study 1 (R01MH085874; Cyranowski, P.I.), adult males and females (N=50) meeting the above MDD criteria and having significant co-occurring anxiety (score ≥7 on the past-month Panic and Agoraphobic Spectrum Self-Report [PAS-SR, Cassano et al., 1997; Shear et al., 2001]) were randomly assigned to 16 sessions of either BSP or IPT-PS (interpersonal psychotherapy for depression with co-occurring panic symptoms) in addition to adjunctive pharmacotherapy (citalopram). IPT-PS adapts IPT to target not only depression, but also cooccurring panic, anxiety, and avoidance symptoms that may interfere with the proactive interpersonal problem-solving techniques of IPT (Cyranowski et al., 2005). In addition to using primary IPT strategies for depression, IPT-PS therapists identify anxiety or avoidance symptoms that interfere with interpersonal problem solving related to the identified IPT problem area. They incorporate, in limited fashion, simple cognitive strategies (identify and replace dysfunctional anxiety-related cognitions) or behavioral strategies (reduce dysfunctional patterns of avoidance) within the IPT treatment framework.
In Study 2 (R01 MH083647; Swartz, P.I.), depressed mothers (N=173) of psychiatrically ill children were randomly assigned to nine sessions of either BSP or IPT-MOMS. IPT-MOMS adapts IPT to address the needs of mothers of psychiatrically-ill children, focusing on mother-child communication and the role transition of parenting an ill child (Swartz et al., 2008). Mothers taking stable doses of antidepressants were eligible for study inclusion, assuming medications remained stable throughout the trial.
The 10 therapists (9 female, 1 male) were psychologists, social workers, and a psychiatrist trained in working with depressed patients. Five therapists participated in both studies. Therapists provided only IPT or BSP, excepting the two primary trainers (H.S. & J.C.) who provided both IPT and BSP at separate time points (Falkenström, Markowitz, Jonker, Philips, & Holmqvist, 2013). All IPT therapists were trained by recognized IPT expert trainers (H.S. or Ellen Frank, Ph.D.); all BSP therapists either received a two-day initial training directly from a BSP expert (J.M.) or watched a recorded BSP training and received ongoing supervision from a BSP supervisor (J.C. or Allan Zuckoff, Ph.D.). Across both trials, three IPT therapists were highly experienced therapists (>10 years of experience), one moderately experienced (5–10 years of experience), and one was an early-career therapist (1–5 years of experience); three highly experienced, one moderately experienced, and three early-career therapists delivered BSP. Throughout the trials, all therapists participated in weekly treatment supervision (separate supervision for IPT and BSP), in which they presented cases, reviewed session video recordings, and received expert supervisor feedback. Efforts were made to provide comparable experiences for the two therapist teams.
Treatment Adherence Measure
Raters used the Collaborative Study Psychotherapy Rating Scale (CSPRS-6; Hollon, 1984) to evaluate recorded psychotherapy sessions. The original instrument contained 96 items divided into scales measuring specific techniques of IPT (28 items), CBT (28 items), and clinical (pharmacotherapeutic) management (20 items), as well as nonspecific therapeutic strategies (12 items). Guided by specific anchor points in the raters’ manual, raters score items on a Likert-type scale to measure the extent to which certain therapist behaviors occurred during the observed session, with item scores ranging from one (not at all) to seven (extensively). Raters consider both the frequency and intensity of observed therapist behaviors; thus, items assess whether and how often therapists use specific and common factors therapeutic techniques during the session. Although items are not designed to measure the quality or effectiveness of techniques, Waltz and colleagues (1993) remark that raters are asked to make inferences about the quality of interventions in some instances (e.g., to consider the thoroughness of exploration in examining evidence for automatic thoughts). Although raters completed all CSPRS-6 items, the current report focused on subscales relevant to IPT and BSP. As the CSPRS-6 was not originally developed to measure BSP adherence, the current study used a brief version of the Markowitz and colleagues (2000) addendum BSP scale described below.
The IPT scale originally developed for the CSPRS-6 comprises seven subscales: Interpersonal Rationale (3 items), Focus on Feelings (4 items), Assessing Interpersonal Relationships and Tendencies (5 items), Assisting Changes in Interpersonal Functioning (4 items), Role Transitions (4 items), Interpersonal Disputes (4 items), and Interpersonal Deficits (4 items). Because IPT and BSP both rely heavily on affect-focused strategies that may be considered ‘common factors,’ we elected to remove the Focus on Feelings subscale from the IPT-specific measure and analyze this scale separately (described below). The remaining six IPT subscales were used to assess therapist use of IPT-specific techniques. IPT-specific items assess, for example, the extent to which the therapist “related the client’s depression… to difficulties in the client’s interpersonal relationships”; “focused on the client’s interpersonal relationships”; or “explored changes the client would like to see in an important relationship.”
The BSP scale for this study was a shortened version of a 10-item BSP scale designed by Markowitz and colleagues (2000) for a study of depression treatment among HIV-positive patients. Although this scale did not receive the elaborate psychometric testing of the original CSPRS, previous trials have successfully used the full BSP subscale (Markowitz et al., 1998; Markowitz et al., 2000; Markowitz et al., 2005; Markowitz et al., 2008; Kocsis et al., 2009), and one formal report showed that the CSPRS-6 plus the BSP subscale discriminated between IPT and BSP (Markowitz et al., 2000). The current study omitted several BSP items specific to HIV-positive patients, leaving a shortened, three-item BSP scale measuring the extent to which therapists: (1) “facilitated discussion but did not provide any theoretical framework,” (2) “conveyed the sense that he/she was a non-judgmental helper…,” and (3) “echoed the patient’s concerns ….” Scoring conventions for the BSP scale follow the CSPRS-6 format. (Complete items are available from the authors upon request.)
Because both IPT and BSP are affect-focused psychotherapies, we elected to separate therapist use of this key common-factors strategy and assess the Focus on Feelings subscale separately. The 4-item Focus on Feeling scale measured the extent to which therapists help the client to: (1) “acknowledge affect that she/he was not expressing…”; (2) “accept feelings of which the client is aware but which are painful or uncomfortable”; (3) “explore her/his feelings related to an interpersonal relationship…” and (4) “identify and explore feelings the client had about a deceased person…”
Finally, we evaluated three CSPRS-6 subscales to compare and contrast techniques therapists used across the two treatments. Two non-specific subscales included the 4-item Explicit Directiveness scale, measuring how much the therapist actively guides session discussion (e.g., “how much did the therapist direct or guide the session in an explicit way?”) and the 8-item Facilitative Conditions scale, assessing non-specific therapist qualities such as warmth and empathy (e.g., “was the therapist empathic toward the client [i.e., did she/he convey an intimate understanding of and sensitivity to the client’s experiences and feelings]?). The CBT scale, included to demonstrate discriminant validity, has six subscales: Cognitive Rationale (3 items), Assessing Cognitive Processes (5 items), Evaluating and Changing Beliefs (7 items), Behavioral Focus (4 items), Homework (3 items), and Collaborative Structure (6 items). Analyses used mean scores for each subscale. CBT-specific items assess, for example, how much the therapist helped the client to “relate affective states…to the client’s ongoing thoughts”; “report specific thoughts (as verbatim as possible)…”; and “identify specific types of cognitive distortions or errors….”
Session Recordings
We selected two sets of therapy sessions for adherence ratings: (1) early sessions (defined as sessions 2–4 in Study 1; sessions 3–4 in Study 2), and (2) late sessions (defined as sessions 13–15 in Study 1; sessions 5–7 in Study 2). By a priori design, approximately 25% of all available session recordings in each category were selected using a computer-generated program that chose every seventh recording on a list of consecutively numbered available sessions. Separate lists were maintained for each therapy modality and each study. When a session recording proved inaudible, the recording immediately following it was chosen. Raters evaluated 180 recordings: 32 Study 1 recordings (16 per therapy) and 148 Study 2 recordings (77 IPT, 71 BSP). Approximately half of the recordings rated in each study comprised early sessions, half late sessions.
Recordings were randomly assigned to raters blinded to treatment modality and early versus late session status. Most (88%) recorded sessions were videotaped, with only the patients visible; the remainder were audiorecorded based on participant request or because the session was conducted via telephone (n = 7). Raters listened to each tape and transcribed the session, focusing on therapist verbalizations rather than patient responses. The average time spent rating each session was 2.5 hours.
Adherence Raters
Independent raters were two master’s level students without previous IPT or BSP experience. They were trained by S.M., who participated in a two-day training session in the laboratory of J.C.M. with extensively experienced CSPRS-6 and BSP raters. Raters developed reliability after approximately 80 hours of training, including independent reading of IPT and BSP treatment manuals, participation in didactic sessions provided by experts in both treatments, extensive discussion of each CSPRS-6 and BSP item, and rating and discussing 10 pilot session recordings. To be deemed eligible to begin study ratings, raters needed to score within one point of each other on each individual CSPRS-6 and BSP item. Following the initial training and co-rating phase, a subset (N=27) of the recordings selected for adherence ratings were randomly chosen for independent coding by both raters to calculate inter-rater reliability. The raters met regularly with the trainer to discuss the recordings and to prevent drift. At each meeting, the raters were assigned seven individual and three reliability recordings. One rater’s scores for each reliability tape were then randomly chosen to be included in analyses.
Statistical Analysis
Mixed effects models, in which raters were considered fixed effects and session recordings considered random effects, were used to obtain intraclass correlation (ICC) estimates of interrater reliability. To begin, single-measure intraclass correlations, ICC (3,1) were calculated to assess interrater reliability for each scale. These estimates represent the degree of between-rater consistency in ratings and generalize to the session recordings rated by only one rater. In addition, given the frequent use of multiple adherence raters on large-scale adherence measurement projects, average-measures of intraclass correlations, ICC (3,k), were calculated to examine the impact that averaging the two raters’ ratings would have on reliability (Hallgren, 2012). Internal consistency of each CSPRS-6 and BSP scale was evaluated using Cronbach’s alpha statistic, and t-tests compared mean CSPRS-6 and BSP scale ratings obtained between the IPT and BSP session recordings. For post hoc analyses exploring the relationship between adherence scores and treatment outcome, linear regression models were used to calculate standardized residual scores representing the variance in HRSD scores at the eighth week of treatment that could not be explained by HRSD scores at the first week of treatment. Week 8 scores were used to standardize outcomes across two studies of different durations. Linear regressions were then used to predict residualized change in depressive symptoms by ratings on the early session (week 2–4) IPT, BSP, and Focus on Feelings scales.
Results
Study Patients
Clinical and demographic characteristics of the 112 depressed patients whose session recordings were used for analyses appear in Table 1. Most patients were women (97.2%), white (77.8%), had at least some college education (80.4%) and a mean age of 42.6 years (SD= 10.1). Study 2 included greater percentages of African American and married patients than Study 1. On average, patients in Study 2 were older than those in Study 1; patients in Study 1 not unexpectedly entered the trial with more lifetime anxiety diagnoses and more severe depressive symptoms than those in Study 2.
Table 1.
Participant Demographic Information
| Total (n=112) |
Study 1 (n=25) |
Study 2 (n=87) |
Statistic | ||
|---|---|---|---|---|---|
| Gender (female) | n (%) | 109 (97.3) | 22 (88.0) | 87 (100.0) | χ2 = 10.727, p = 0.001 |
| Age | M (SD) | 42.6 (10.1) | 30.8 (10.2) | 46.0 (7.1) | t = −8.509, p = 0.000 |
| Race | χ2 = 11.831, p= 0.037 | ||||
| Caucasian | n (%) | 88 (78.6) | 19 (76.0) | 69 (79.3) | |
| African American | n (%) | 17 (15.2) | 3 (12.0) | 14 (16.1) | |
| Mixed/Other | n (%) | 7 (6.3) | 3 (12.0) | 4 (4.6) | |
| Education | χ2 = 7.705, p = 0.261 | ||||
| No high school diploma | n (%) | 4 (3.6) | 1 (4.0) | 3 (3.4) | |
| High school diploma/GED | n (%) | 18 (16.1) | 3 (12.0) | 15 (17.2) | |
| Partial/Full undergraduate | n (%) | 70 (62.5) | 19 (76.0) | 51 (58.6) | |
| Graduate degree | n (%) | 20 (17.9) | 2 (8.0) | 18 (20.7) | |
| Income | χ2 = 11.640, p = 0.168 | ||||
| Less than $10,000 | n (%) | 44 (39.3) | 14 (56.0) | 30 (34.5) | |
| $10,000 – $29,999 | n (%) | 29 (25.9) | 4 (16.0) | 25 (28.7) | |
| $30,000 – $74,999 | n (%) | 28 (25.0) | 6 (24.0) | 22 (26.2) | |
| Greater than $75,000 | n (%) | 11 (9.8) | 1 (4.0) | 10 (11.5) | |
| Marital status | χ2 = 19.239, p = 0.002 | ||||
| Married/Living with partner | n (%) | 49 (43.8) | 4 (16.0) | 45 (51.7) | |
| Never married | n (%) | 32 (28.6) | 15 (60.0) | 17 (19.5) | |
| Separated/Divorced | n (%) | 26 (23.2) | 6 (24.0) | 20 (23.0) | |
| Widowed | n (%) | 5 (4.5) | 0 (0.0) | 5 (5.7) | |
| Comorbid anxiety disorder (all) | n (%) | 72 (64.3) | 20 (80.0) | 52 (59.8) | χ2 = 3.462, p = 0.063 |
| Comorbid Panic Disorder | n (%) | 15 (13.4) | 4 (16.0) | 11 (12.6) | |
| Lifetime anxiety disorder (all) | n (%) | 81 (72.3) | 23 (92.0) | 58 (66.7) | χ2 = 6.226, p = 0.013 |
| Lifetime Panic Disorder | n (%) | 30 (26.8) | 7 (28.0) | 23 (26.4) | |
| HRSD-17 | M (SD) | 16.7 (4.0) | 18.4 (3.2) | 16.2 (4.0) | t = 2.499, p = 0.014 |
| HRSD-25 | M (SD) | 20.6 (5.5) | 22.7 (4.4) | 20.0 (5.6) | t = 2.214, p = 0.029 |
Note: HRSD = Hamilton Rating Scale for Depression.
Interrater Reliability and Internal Consistency of CSPRS Scales
Table 2 describes intraclass correlations and Cronbach’s alpha internal reliability estimates for each CSPRS-6/BSP scale. Except for the four-item Explicit Directiveness scale (Cronbach’s α = 0.34), internal consistency of the scales ranged from acceptable (Cronbach’s α= 0.66 for the 4-item Focus on Feelings scale) to excellent (Cronbach’s α= 0.90 for the modified 24-item IPT scale). Interrater reliability estimates were excellent for the BSP scale (ICC= 0.91) and good for the IPT (ICC=0.62) and Focus on Feelings scales (ICC=0.68) (Cicchetti, 1994). Interrater reliability for other therapeutic technique scales ranged from fair (CBT, Facilitative Conditions) to good (Explicit Directiveness). Unsurprisingly, average-measures ICC’s (3,k) were uniformly higher than single-measures ICC’s (3,1), with average-measures ICC’s ranging from 0.60 to 0.95.
Table 2.
CSPRS-6 and BSP Scale Intraclass Correlations and Internal Consistency
| ICC (3,1) | ICC (3,k) | Cronbach’s alpha | |
|---|---|---|---|
| IPT | 0.62 | 0.76 | 0.90 |
| BSP | 0.91 | 0.95 | 0.87 |
| FF | 0.68 | 0.81 | 0.66 |
| CBT | 0.56 | 0.71 | 0.75 |
| FC | 0.43 | 0.60 | 0.70 |
| ED | 0.62 | 0.77 | 0.34 |
Note: CSPRS-6 = Collaborative Study Psychotherapy Rating Scale, sixth version; IPT = interpersonal psychotherapy; BSP = brief supportive psychotherapy; FF = focus on feelings; CBT = cognitive-behavioral therapy; FC = facilitative conditions; ED = explicit directiveness.
Adherence Scores Obtained Across BSP and IPT Therapy Recordings
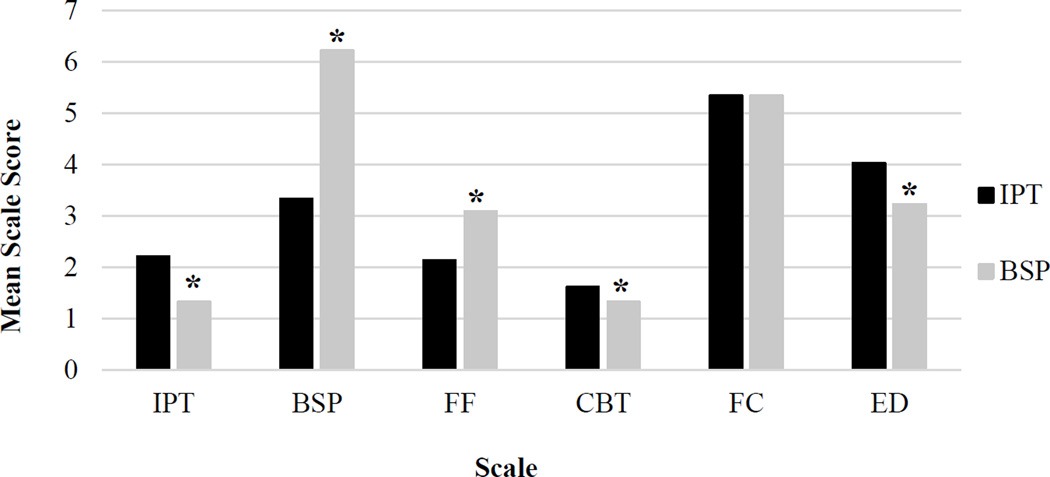
Table 3 and Figure 1 present average scores across the six CSPRS-6/BSP scales, separated by treatment. As hypothesized, IPT therapists provided higher levels of IPT-specific interventions and greater explicit direction than BSP therapists (p’s < .0001), and BSP therapists had higher levels of BSP-specified interventions. Unexpectedly, BSP therapists also displayed a greater focus on feelings than IPT therapists (p’s < .0001).
Table 3.
Mean CSPRS-6 and BSP Subscale Scores for Early and Late Sessions by Treatment
| IPT |
BSP |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Early | Late | t | df | p | Early | Late | t | df | p | |
| IPT | 2.15 | 2.27 | −1.05 | 91 | 0.2985 | 1.37 | 1.29 | 1.71 | 85 | 0.0918 |
| BSP | 3.23 | 3.43 | −1.10 | 91 | 0.2757 | 6.34 | 6.09 | 2.22 | 85 | 0.0293 |
| FF | 2.08 | 2.19 | −0.67 | 91 | 0.5024 | 3.23 | 2.95 | 1.93 | 85 | 0.0568 |
| CBT | 1.61 | 1.61 | 0.02 | 91 | 0.9834 | 1.32 | 1.32 | 0.17 | 85 | 0.8651 |
| FC | 5.20 | 5.49 | −2.42 | 91 | 0.0176 | 5.33 | 5.35 | −0.19 | 85 | 0.8488 |
| ED | 4.15 | 3.91 | 1.58 | 91 | 0.1176 | 3.16 | 3.31 | −1.31 | 85 | 0.1953 |
Figure 1.
Comparison of IPT and BSP treatments on Adherence Scores.
IPT = interpersonal psychotherapy; BSP = brief supportive psychotherapy; FF = focus on feelings; CBT = cognitive-behavioral therapy; FC = facilitative conditions; ED = explicit directiveness.
* p<0.0001
Raters scored IPT and BSP therapy sessions as having comparable levels of Facilitative Conditions such as therapist warmth and empathy. Both sets of sessions scored very low on levels of explicit CBT strategies, although IPT therapists were statistically more likely than BSP therapists to include these interventions (p < .0001). In IPT, mean Facilitative Conditions scores were significantly higher in later sessions (p = .018) and in BSP, BSP scale scores were significantly lower in later sessions (p = .029). No other significant differences in mean CSPRS-6/BSP scores emerged between early and late session recordings (p’s > .05).
After rating each session, raters were asked to decide which therapy they thought the therapist was conducting. They judged 174 recordings (96.7%) correctly, including 100% of BSP recordings and 95.9% of IPT recordings, indicating high levels of global adherence to the respective therapies.
Post Hoc Analyses
Early session (week 2–4) adherence ratings for BSP-specific and IPT-specific interventions were not associated with change in depressive symptoms (as reflected by residualized HRSD change scores from the first to the eighth week of treatment) in the full sample (IPT scale: β −0.19, p = 0.88; BSP scale: β −0.40, p = 0.32), nor within the separate IPT or BSP treatments (all p’s > 0.06). In contrast, higher early session scores on the Focus on Feelings scale were associated lower week 8 HRSD scores (β −1.79, p = 0.02), a finding that appeared to be stronger in IPT (β −2.84, p = 0.06) than BSP (β −0.297, p = 0.829).
Discussion
The recent Institute of Medicine (IOM) report, “Psychosocial Interventions for Mental and Substance Use Disorders” (http://iom.nationalacademies.org/Reports/2015/Psychosocial-Interventions-Mental-Substance-Abuse-Disorders.aspx), highlights the importance of improving the evidence base for psychosocial interventions. The IOM report, however, contains a worrisome call to break therapies into component parts or “elements” in order to investigate components that are specific to (versus shared across) interventions. Although we support the IOM’s encouragement to evaluate the roles of both specific and non-specific factors in mediating treatment outcomes—especially as growing evidence points to the importance of non-specific factors in psychotherapy outcomes (Wampold 2001) —little evidence supports the IOM’s assertion that psychotherapies can or should be disassembled into stand-alone components (cf., Ahn & Wampold, 2001). Indeed, we have argued that affect-focused psychotherapies like IPT and BSP would be endangered were an “elements” framework adopted; unlike a more neatly divisible (e.g., cognitive behavioral) treatment, IPT and BSP employ strategies that are woven together over time to create an affectively meaningful experience for patients (Swartz, 2015). The current report demonstrates that it is possible to evaluate the relative use of both specific and non-specific interventions in two affect-focused therapies without deconstructing the interventions.
In the current study, blinded raters were able to identify and discriminate between two relatively similar affect-focused ESTs using CSPRS-6/BSP ratings, despite considerable expected overlap in use of non-specific therapy techniques. Results demonstrated that therapists in the research protocols adhered closely to their assigned psychotherapy modality. We observed significant differences between IPT and BSP on both specific and non-specific CSPRS-6/BSP items according with the respective treatments’ guidelines. BSP sessions received high mean scores on the BSP scale and IPT sessions received moderate scores on the IPT scale. These scores resemble results found by Markowitz and colleagues (2000) comparing IPT and BSP, and may reflect that during an individual session, BSP therapists repeatedly use a few general behaviors whereas IPT therapists employ some but not all of IPT’s various techniques. For example, because IPT therapists are required to choose a single treatment focus, an IPT therapist receiving a high score on a specific IPT technique (e.g., focus on grief) would likely receive a low score on an alternative treatment focus (e.g., focus on role transition). Because of this level of treatment specificity related to each of the IPT problem areas, note that commonly-reported mean IPT item scores may underestimate the frequency with which IPT therapists utilized targeted IPT interventions overall. Examination of summary scores of the IPT scale revealed that on average, IPT therapists had scores 20 points higher than BSP therapists (52.98 v. 32.01, respectively).
Findings confirmed most hypotheses regarding the differential use of EST-specific versus non-specific techniques. IPT therapists provided higher levels of IPT-specific interventions and greater explicit direction than BSP therapists, while BSP therapists avoided specific IPT techniques, using more non-directive, supportive strategies. IPT therapists did display some general BSP behaviors (such as nonjudgemental reflection), which is unsurprising: IPT therapists were expected to use common factor techniques -- which comprise BSP -- in addition to specific IPT techniques. Also as hypothesized, IPT and BSP therapists displayed similarly high levels of warmth and empathy, as their identical Facilitative Conditions scores indicate. Expectedly, both sets of therapists displayed relatively low scores on CBT subscales. IPT therapists did, however, score higher than BSP therapists on the CBT scale, which is understandable given the expected integration of some cognitive strategies within IPT-PS. The highest scoring CBT subscales among IPT therapists were ‘Evaluating and Changing Beliefs,’ which is consistent with the IPT-PS adaptation; and ‘Collaborative Structure,’ which arguably should also arise in other directive therapies such as IPT. Indeed, selecting and maintaining a focus on the chosen IPT problem area are well-described components of IPT and require in-session collaboration and structuring (Weissman, Markowitz & Klerman, 2007).
This study replicates and extends previous findings of Markowitz and colleagues (2000) demonstrating that blinded raters can discriminate between two therapies that have many overlapping elements. Such a task carries greater difficulty than comparing more disparate treatments, as in the original TDCRP trial (Hill, O’Grady, & Elkin, 1992). Although the current study did not evaluate the quality of the therapies provided, it established that both sets of therapists generally adhered to their respective treatment modalities and eschewed proscribed techniques, a sound validation for the two trials described.
We did not hypothesize differences in use of techniques in early and late sessions; however, we observed an increase in Facilitative Conditions scores in IPT in late sessions and a decrease in BSP scale scores in BSP from early to late sessions. The observed increase in Facilitative Conditions scores in later IPT sessions suggests that the balance of IPT interventions may shift toward non-specific strategies as treatment progresses because therapists spend less time structuring the session (e.g., choosing the IPT focus, encouraging the patient to discuss interpersonal issues) whereas more time is spent offering non-specific support as the patient improves. Similarly, in BSP, lower BSP scale scores in later sessions suggests that as patients improve, the therapist uses fewer specific BSP techniques such as echoing patients concerns. These findings suggest that therapists use more treatment-specific interventions early in the course of therapy and rely more on non-specific factors over time. Alternatively, the findings may reflect that patients learn the structure and techniques of the therapy in early sessions and need less therapist guidance in later sessions (Markowitz et al., 2000). However, lacking conservative control of family-wise error rate and prior hypotheses regarding early versus late sessions, these findings need replication.
Other study limitations are the total of only two raters, and that not all sessions were co-rated. Our results corroborate that deploying additional raters per recording and using their average ratings increases interrater reliability (Hallgren, 2012). While this mutli-rater approach is less often used, future cost-benefit analyses may find it advantageous in effort and cost, considering the positive trade-off that might result from training more raters simultaneously with less time-intensive procedures and then using averaged rater scores.
Another limitation is the very low internal consistency of the Explicit Directiveness scale, similar to the findings of Hill, O’Grady, and Elkin (1992), suggesting that the scale items do not measure the same construct. In fact, post hoc analyses indicated that removal of the therapists’ subtle guidance item (as opposed to explicit guidance) increased the Cronbach’s alpha from 0.34 to 0.50. We chose to use the scale in its original form, however, to allow comparison with the extant literature. Despite the low internal consistency, raters displayed good interrater reliability on the scale. In addition, interrater reliability scores were lower than expected for some CSPRS-6 subscales (see Hill, O’Grady, & Elkin, 1992; Markowitz et al., 2000). Previous research found similarly low ICCs for the Facilitative Conditions scale (Hill, O’Grady, & Elkin, 1992), likely secondary to the inevitably looser anchors intrinsic to a somewhat subjective subscale relative to more easily operationalized components of the EST-specific CSPRS-6 scales.
Although we had originally hypothesized that both IPT and BSP therapists would score similarly on Focus on Feelings (originally one of the seven IPT subscales), we found, to our surprise, that BSP therapists had higher Focus on Feelings scores. Potential explanations for this include the key role that ‘following the client’s affect’ plays in BSP and that BSP therapists had a limited number of alternative techniques available. Because BSP interventions are limited to focusing on patients’ affective states and providing general support, BSP therapists may spend more session time exploring feeling states. In contrast, IPT therapists have at their disposal multiple specific interpersonal strategies that vie for session time, which may function to decrease time spent explicitly focusing on feelings. Indeed, Figure 1 suggests that IPT therapists distribute their work almost evenly between focusing on feelings and utilizing specific interpersonal interventions of IPT. In contrast, BSP therapists allocate most of their time to focusing on feelings and providing non-directive support (as indicated by high BSP scale scores).
We were similarly surprised by post hoc results indicating that while early use of BSP- and IPT-techniques were not related to week-8 symptom change, a higher Focus on Feelings score was associated with lower week-8 depression scores in the full sample, and perhaps more so for patients randomized to IPT. One might have hypothesized that the use of more directive IPT problem-solving strategies should increase the efficacy of IPT. But because identification and exploration of emotional responses are crucial to any successful psychotherapy (Markowitz & Milrod, 2011), a diminished focus on feelings in early IPT sessions (necessitated by focus on IPT-specific strategies) might plausibly decrease the effectiveness of IPT. For example, premature introduction of directive interventions might not allow the patient sufficient time to build an alliance or experience relevant affective states (Markowitz & Milrod, 2011). Our experience suggests that premature use of directive IPT strategies, without sufficient focus on feelings, may be particularly common among early-career therapists, who may feel less comfortable tolerating patients’ negative affect. Indeed, it may benefit novice therapists to begin their psychotherapy training by developing experience and comfort in providing foundational components of psychotherapy with BSP, “psychotherapy stripped down to its basics” (Markowitz, 2014, p. 287), before graduating to more multi-faceted, directive therapeutic techniques (e.g., Plankun, Sudak, & Goldberg, 2009). Thus, it is plausible that the ultimate effectiveness of ESTs lies not only in their specific strategies, but in the therapist’s ability to optimally balance use of key common-factors interventions (such as an affective focus) with more directive, EST-specific change strategies.
The current trial was not explicitly designed to evaluate the relationship between treatment adherence and outcome. Hence whether the use of EST-specific versus non-specific strategies influences IPT and BSP treatment outcome remains an empirically testable question. These exploratory post hoc analyses require confirmation in future research that evaluates the likely reciprocal temporal relationships between therapists’ use of treatment strategies and patients’ symptom changes over time. The above discussion does, however, illustrate the potential importance of future process research that simultaneously assesses use of both EST-specific and non-specific factors. As a first critical step, this report supports the feasibility and potential utility of simultaneously assessing therapist use of key nonspecific and EST-specific interventions, using a broad-spectrum adherence scales.
To date, too little research has examined psychotherapy adherence in detail, and virtually none has assessed how EST therapists utilize both common-factor strategies and EST-specific interventions within the therapeutic encounter. As the field moves to consider the advantages of strategic treatment integration approaches to identify active ingredients of psychosocial treatments, future research is needed to assess therapist use of both specific and non-specific techniques delivered in the context of ESTs, and to determine the optimal balance of the two on depression treatment outcomes.
Acknowledgments
The authors wish to thank the many individuals who contributed to this project: psychotherapy supervisors (Ellen Frank, Ph.D.; Allan Zuckoff, Ph.D.), adherence raters (Leah Boisen and Susan Wright), adherence trainers (Angelo Boccia Cedeño, M.A. and Brian Jo, M.A.), staff, and participants of the treatment trials.
Source of Funding: This research was supported by grants from the National Institute of Mental Health R01 MH085874 and R01 MH083647.
References
- Ahn HN, Wampold BE. Where oh where are the specific ingredients? A meta-analysis of component studies in counseling and psychotherapy. Journal of Counseling Psychology. 2001;48(3):251. [Google Scholar]
- Barber J, Crits-Christoph P. Development of a therapist adherence/competence rating scale for supportive-expressive dynamic psychotherapy: a preliminary report. Psychotherapy Research. 1996;6(2):81–94. doi: 10.1080/10503309612331331608. [DOI] [PubMed] [Google Scholar]
- Barber JP, Crits-Christoph P, Luborsky L. Effects of therapist adherence and competence on patient outcome in brief dynamic therapy. Journal of Consulting and Clinical Psychology. 1996;64(3):619. doi: 10.1037//0022-006x.64.3.619. [DOI] [PubMed] [Google Scholar]
- Butler SF, Henry WP, Strupp HH. Measuring adherence in time-limited dynamic psychotherapy. Psychotherapy: Theory, Research, Practice, Training. 1995;32(4):629. [Google Scholar]
- Butler SF, Strupp HH. Specific and nonspecific factors in psychotherapy: A problematic paradigm for psychotherapy research. Psychotherapy: Theory, Research, Practice, & Training. 1986;23(1):30. [Google Scholar]
- Cassano GB, Michelini S, Shear MK, Coli E, Maser JD, Frank E. The panic-agoraphobic spectrum: a descriptive approach to the assessment and treatment of subtle symptoms. The American Journal of Psychiatry. 1997;154(4):27–38. doi: 10.1176/ajp.154.6.27. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Hollon SD. Defining empirically supported therapies. Journal of Consulting and Clinical Psychology. 1998;66(1):7. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment. 1994;6(4):284. [Google Scholar]
- Cuijpers P, Geraedts AS, van Oppen P, Andersson G, Markowitz JC, van Straten A. Interpersonal psychotherapy for depression: a meta-analysis. American Journal of Psychiatry. 2011;168(6):581–592. doi: 10.1176/appi.ajp.2010.10101411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyranowski JM, Frank E, Shear MK, Swartz HA, Fagiolini A, Scott J, Kupfer DJ. Interpersonal psychotherapy for depression with panic spectrum symptoms: a pilot study. Depression and Anxiety. 2005;21(3):140–142. doi: 10.1002/da.20069. [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Feeley M. Determinants of change in cognitive therapy for depression. Cognitive Therapy and Research. 1990;14(5):469–482. [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, Jacobson NS. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology. 2006;74(4):658. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Falkenström F, Markowitz JC, Jonker H, Philips B, Holmqvist R. Can psychotherapists function as their own controls? Meta-analysis of the crossed therapist design in comparative psychotherapy trials. Journal of Clinical Psychiatry. 2013;74(5):482–491. doi: 10.4088/JCP.12r07848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feeley M, DeRubeis RJ, Gelfand LA. The temporal relation of adherence and alliance to symptom change in cognitive therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67(4):578. doi: 10.1037//0022-006x.67.4.578. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition. New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- Frank JD. Therapeutic factors in psychotherapy. American Journal of Psychotherapy. 1971;25(3):350–361. doi: 10.1176/appi.psychotherapy.1971.25.3.350. [DOI] [PubMed] [Google Scholar]
- Frank JD, Frank JB. Persuasion and healing: A comparative study of psychotherapy. Baltimore, MD: JHU Press; 1993. [Google Scholar]
- Grencavage LM, Norcross JC. Where are the commonalities among the therapeutic common factors? Professional Psychology: Research and Practice. 1990;21(5):372–378. [Google Scholar]
- Hallgren KA. Computing inter-rater reliability for observational data: An overview and tutorial. Tutorials in Quantitative Methods for Psychology. 2012;8(1):23. doi: 10.20982/tqmp.08.1.p023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill CE, O'Grady KE, Elkin I. Applying the Collaborative Study Psychotherapy Rating Scale to rate therapist adherence in cognitive-behavior therapy, interpersonal therapy, and clinical management. Journal of Consulting and Clinical Psychology. 1992;60(1):73. doi: 10.1037//0022-006x.60.1.73. [DOI] [PubMed] [Google Scholar]
- Hollon SD. Final report: System for rating psychotherapy audiorecordings. Bethesda, MD US Department of Health and Human Services. 1984 [Google Scholar]
- Karasu TB. The specificity versus nonspecificity dilemma: Toward identifying therapeutic change agents. The American Journal of Psychiatry. 1986;143(6):687–695. doi: 10.1176/ajp.143.6.687. [DOI] [PubMed] [Google Scholar]
- Kocsis JH, Gelenberg AJ, Rothbaum BO, Klein DN, Trivedi MH, Manber R, Keller … Thase ME. Cognitive behavioral analysis system of psychotherapy and brief supportive psychotherapy for augmentation of antidepressant nonresponse in chronic depression: the REVAMP Trial. Archives of General Psychiatry. 2009;66(11):1178–1188. doi: 10.1001/archgenpsychiatry.2009.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz JC, Kocsis JH, Christos P, Bleiberg K, Carlin A. Pilot study of interpersonal psychotherapy versus supportive psychotherapy for dysthymic patients with secondary alcohol abuse or dependence. The Journal of Nervous and Mental Disease. 2008;196(6):468–474. doi: 10.1097/NMD.0b013e31817738f1. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Kocsis JH, Fishman B, Spielman LA, Jacobsberg LB, Frances AJ, Perry SW. Treatment of depressive symptoms in human immunodeficiency virus-positive patients. Archives of General Psychiatry. 1998;55(5):452–457. doi: 10.1001/archpsyc.55.5.452. [DOI] [PubMed] [Google Scholar]
- Markowitz JC. What is supportive psychotherapy? Focus. 2014;12(3):285–289. [Google Scholar]
- Markowitz JC, Kocsis JH, Bleiberg KL, Christos PJ, Sacks M. A comparative trial of psychotherapy and pharmacotherapy for “pure” dysthymic patients. Journal of Affective Disorders. 2005;89(1):167–175. doi: 10.1016/j.jad.2005.10.001. [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Milrod BL. The importance of responding to negative affect in psychotherapies. Perspectives. 2011;168(2) doi: 10.1176/appi.ajp.2010.10040636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz JC, Spielman LA, Scarvalone PA, Perry SW. Psychotherapy adherence of therapists treating HIV-positive patients with depressive symptoms. Journal of Psychotherapy Practice and Research. 2000;9(2):75–80. [PMC free article] [PubMed] [Google Scholar]
- Miller SJ, Binder JL. The effects of manual-based training on treatment fidelity and outcome: A review of the literature on adult individual psychotherapy. Psychotherapy: Theory, Research, Practice, Training. 2002;39(2):184–198. [Google Scholar]
- Ogrodniczuk JS, Piper WE. Measuring therapist technique in psychodynamic psychotherapies. Journal of Psychotherapy Practice and Research. 1999;8(2):143. [PMC free article] [PubMed] [Google Scholar]
- Plakun EM, Sudak DM, Goldberg D. The Y model: an integrated, evidence-based approach to teaching psychotherapy competencies. Journal of Psychiatric Practice. 2009;15(1):5–11. doi: 10.1097/01.pra.0000344914.54082.eb. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Teasdale JD, Williams JM, Gemar MC. The mindfulness-based cognitive therapy adherence scale: inter-rater reliability, adherence to protocol and treatment distinctiveness. Clinical Psychology & Psychotherapy. 2002;9(2):131–138. [Google Scholar]
- Shear MK, Frank E, Rucci P, Fagiolini DA, Grochocinski VJ, Houck PR, Banti S. Panic-agoraphobic spectrum: reliability and validity of assessment instruments. Journal of Psychiatric Research. 2001;35(1):59–66. doi: 10.1016/s0022-3956(01)00002-4. [DOI] [PubMed] [Google Scholar]
- Strunk DR, Cooper AA, Ryan ET, DeRubeis RJ, Hollon SD. The process of change in cognitive therapy for depression when combined with antidepressant medication: Predictors of early intersession symptom gains. Journal of Consulting and Clinical Psychology. 2012;80(5):730. doi: 10.1037/a0029281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz HA, Frank E, Zuckoff A, Cyranowski JM, Houck PR, Cheng Y, Shear MK. Brief interpersonal psychotherapy for depressed mothers whose children are receiving psychiatric treatment. American Journal of Psychiatry. 2008;165(9):1155–1162. doi: 10.1176/appi.ajp.2008.07081339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz HA, Markowitz JC. Techniques of individual interpersonal psychotherapy. In: Gabbard GO, editor. Textbook of psychotherapeutic treatments in psychiatry. Washington, D.C.: American Psychiatric Publishing; 2009. pp. 309–338. [Google Scholar]
- Swartz HA. IOM report on psychosocial interventions for mental and substance use disorders: the interpersonal psychotherapy perspective. Depression and Anxiety. 2015;32(11):793–795. doi: 10.1002/da.22426. [DOI] [PubMed] [Google Scholar]
- Thase ME, Carpenter L, Kupfer DJ, Frank E. Clinical significance of reversed vegetative subtypes of recurrent major depression. Psychopharmacology Bulletin. 1991;27:17–22. [PubMed] [Google Scholar]
- Waltz J, Addis ME, Koerner K, Jacobson NS. Testing the integrity of a psychotherapy protocol: assessment of adherence and competence. Journal of Consulting and Clinical Psychology. 1993;61(4):620. doi: 10.1037//0022-006x.61.4.620. [DOI] [PubMed] [Google Scholar]
- Wampold BE. The great psychotherapy debate: Models, methods, and findings. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. [Google Scholar]
- Weck F, Hilling C, Schermelleh-Engel K, Rudari V, Stangier U. Reliability of adherence and competence assessment in cognitive behavioral therapy: influence of clinical experience. The Journal of Nervous and Mental Disease. 2011;199(4):276–279. doi: 10.1097/NMD.0b013e3182124617. [DOI] [PubMed] [Google Scholar]
- Weck F, Rudari V, Hilling C, Hautzinger M, Heidenreich T, Schermelleh-Engel K, Stangier U. Relapses in recurrent depression 1 year after maintenance cognitive-behavioral therapy: The role of therapist adherence, competence, and the therapeutic alliance. Psychiatry Research. 2013;210(1):140–145. doi: 10.1016/j.psychres.2013.05.036. [DOI] [PubMed] [Google Scholar]
- Weinberger J. Common factors aren't so common: The common factors dilemma. Clinical Psychology: Science and Practice. 1995;2(1):45–69. [Google Scholar]
- Weissman MM, Klerman GL, Prusoff BA, Sholomskas D, Padian N. Depressed outpatients: results one year after treatment with drugs and/or interpersonal psychotherapy. Archives of General Psychiatry. 1981;38(1):51–55. doi: 10.1001/archpsyc.1981.01780260053005. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Markowitz JC, Klerman G. Clinicians’ Quick Guide to Interpersonal Psychotherapy. New York NY: Oxford University Press; 2007. [Google Scholar]