Abstract
US Latinos are less likely to utilize mental health services than non-Latino Whites, and to take antidepressant medication. This mixed-method study followed a subset (N=28) of a research sample of depressed Latino immigrant primary care patients with a telephone interview to study their knowledge about and experiences with antidepressant medications. Most (82%) reported taking medication for two months or more, and 75% reported feeling better, while over half reported side effects. Most (61%) agreed that antidepressants are generally safe, and helpful in treating depression (68%); however, many believed they could be addictive (39%). Fifty percent of patients who discontinued their medication did not inform their providers. Twelve of the 28 patients also participated in focus groups about interactions with providers and made suggestions for conveying information about antidepressants. Patients suggested videos as a format to disseminate medication information since they do not require written comprehension. Other patient recommendations are presented.
Keywords: antidepressants, primary care, low-income patients, Latinos, focus groups
Latinos in the United States suffer from more physical health problems than non-Latino Whites (Blackwell et al., 2014; U.S. Department of Health and Human Services [USDHHS], 2000); and these problems are associated with worse mental health problems (Bandiera et al., 2008). Latinos are also at increased risk for posttraumatic stress disorder (PTSD) due to high violence exposure (Clark et al., 2008; Eisenman et al., 2003; Fortuna et al., 2008). Despite these risk factors, Latinos in the US are less likely to utilize mental health services than non-Latino Whites (Alegria et al., 2002; Cabassa et al., 2006; Dobalian and Rivers, 2008; SAMHSA, 2015), and they are also less likely to utilize antidepressant medication (Interian et al., 2011). System barriers to mental health treatment for Latinos include cost of care/lack of health insurance coverage, limited time with providers, low knowledge about resources, and lack of linguistic and culturally competent services (Anastasia and Bridges, 2015; Kessler et al., 2001; Rubenstein et al., 1999; Ruiz et al., 2013; SAMSHA, 2015; Shattell et al., 2008; Uebelacker et al., 2012; USDHHS, 2001; Vargas et al., 2015). Latinos are less likely to receive care that meets best practice guidelines (Alexandre et al., 2009; Cabassa et al., 2006; Lagomasino et al., 2005; Quinones et al., 2014), and are more likely to drop out early or discontinue care (La Roche, 2002; Lanouette et al., 2006; Sue, 1998; USDHHS, 1999), highlighting the need to understand characteristics of acceptable and accessible interventions.
Psychiatric medications are often viewed negatively by the public in general, and even as harmful (Jorm, 2012). Research examining treatment preferences for depression among Latinos has generally found a strong preference for individual psychotherapy, while medications are viewed less favorably (Cabassa et al., 2007; Dwight-Johnson et al., 2000; Eisenman et al., 2008; Kaltman et al., 2014). Complementary and alternative medications, including herbal medicines, are frequently used for depression among underserved U.S. Latinos, and these therapies are among preferred treatment methods (Bazargan et al., 2008; Hirai et al., 2015; Sorrell, 2014).
Very little research exists about knowledge, and sources of knowledge, regarding antidepressants in the general population, and among Latinos in particular. In one study, Chandra et al. (2009) found that Latino and African American teens and their parents had lower levels of knowledge than their White counterparts. A qualitative study of mostly Puerto Ricans and Dominicans showed that use of antidepressants was seen as indicative of a severe illness and a weakness or failure to cope (Interian et al., 2007).
In non-Latino groups, perceived necessity for taking medications is associated with more severe and longer anticipated duration of symptoms, while perceived harmfulness of medications is associated with an unclear understanding of depression (Aikens et al., 2008). Poor antidepressant adherence has been associated with less knowledge about depression and medication side effects, as well as concerns about dependence (Bauer et al., 2013; Fawzi et al., 2012; Woodward et al., 2016). In situations where necessity (e.g., health depends on the medications) outweighs concerns, medication adherence is better (Fawzi et al., 2012; Russell and Kazantzis, 2008). Yet several studies have found greater adherence among patients prescribed antidepressants compared to those referred for psychotherapy, including among Latino patients (Ishiwaka et al., 2014; Miranda et al., 2003).
There is a paucity of literature regarding patients’ understanding of how antidepressants work, their side effects, or patients’ sources of information and education about antidepressants among any ethnic group. One study indicated that television, the Internet, print media, conversation, and radio broadcast comprise the major sources of mental health information identified by U.S. Latinos (Sorrell, 2014). In a non-Latino sample of English-speaking subjects or participants, patients most frequently reported receiving antidepressant information from pharmacists (58%), primary care physicians (50.6%), mental health specialists (40.7%), personal contacts (32.1%), and the Internet (18.5%); patients who received information from a greater number of sources were more adherent to antidepressant therapy (Sleath et al., 2003).
The current study followed up an existing research sample of depressed primary care patients, most of whom were low-income, uninsured, Spanish-speaking Latino immigrants, by recruiting those who had reported taking medication as part of their depression treatment. We targeted this sample to begin to learn more about this population of low-resources primary care patients’ knowledge about antidepressant medications, how information was obtained about their prescribed antidepressant medications, and about their recommendations for conveying and disseminating needed information about such medications at primary care clinics serving similar populations.
Study Background
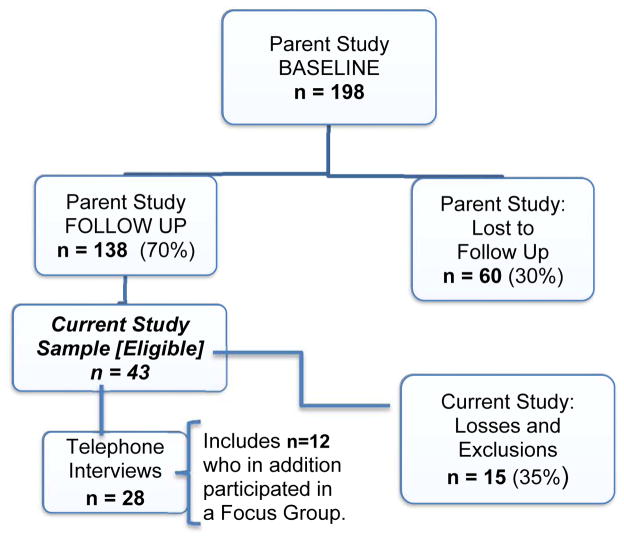
This investigation consisted of a follow-up of patients in a previous/parent study addressing the effectiveness of a collaborative care program (Kaltman, Watson, Campoli, Serrano, Kirkpatrick, Talisman, Mete, and Green, 2017, Evaluation of behavioral health services in primary care clinics serving low-income Latino immigrants, under review). The parent study was implemented in two clinics that are part of a network of primary care clinics providing care to low-income uninsured county residents in Maryland. In that study, we compared patients who met presumptive criteria for depression in a clinic with a formal collaborative care program to those in a clinic without this program. The latter clinic had a therapist on site. One hundred ninety-eight depressed patients were enrolled in the parent study, and 138 (70%) completed telephone follow-up. The current study comprised a mixed-methods investigation among those follow-up patients who took medication for their depression, to investigate their knowledge and attitudes about their antidepressant medication, including risks and benefits, how they actually received this information, and how they would prefer to learn about antidepressants. The study had two components: telephone interviews (Part 1), and focus groups (Part 2), the latter comprising a subset of Part 1 participants. Figure 1 depicts the Ns for the parent study and follow up, and for the current investigation. Methods and results are presented separately for each component; a general discussion follows. We obtained permission from the respective IRBs (Georgetown, clinic systems) to conduct this study.
Figure 1.
Relationship of the Current Study Sample (n=28) to the Prospective Parent Study Sample (n=198)
Part 1 – Telephone Interviews
Methods
Patients
Of the 138 depressed patients who completed follow-up interviews in the parent study, 47 reported at the parent study follow-up that they had taken medication for their depression (33%). Two patients had declined further research contact, and two patients were eliminated from the parent study because they had diagnoses of severe mental disorders (schizophrenia; bipolar disorder) in addition to depression. The remaining 43 participants comprised our target sample, and we attempted to contact each of these individuals. Twenty-eight patients completed interviews and qualified for inclusion; see Figure 1. Reasons for non-participation (n = 15) included inability to contact the individuals (4), person declining to be interviewed (4), not returning the consent form (5), insufficient information (1), and not remembering taking depression medication (1). All patients began the parent study having met or exceeded the cut-off criterion on the Patient Health Questionnaire 9 (PHQ9) for having major depression -- a score of ≥ 10.
Procedure
The interview was conducted via telephone in Spanish by a trained bilingual, Latina interviewer. She briefly described the study and asked if the patient was interested in participating; if so, the interviewer went over study details and reviewed the informed consent process. Consent forms were then mailed to interested participants, which they signed and returned. Patients were instructed to keep a copy of the consent form for themselves. Upon receipt of the consent, the interviewer called back and conducted the interview, also inviting the participants to join a later focus group if interested and convenient. The interview took approximately 30 minutes. Responses were recorded by hand on the interview form, and the additional questions were audio-recorded with participants’ permission. The interviewer then mailed a gift card for $15.00 to each participant, along with a self-stamped envelope and a receipt for the participants to sign and return by mail.
Measures
All study measures in the parent study were available in English and Spanish, as were the consent forms. All participants in this study chose to be interviewed in Spanish.
Existing data from parent study baseline
Demographics - age, gender, education, country of origin, time in US, language preference.
Depression was assessed with the Patient Health Questionnaire (PHQ-9; Spitzer et al., 1999; Spitzer and Williams, 1994). The validity of a Spanish version of the PHQ has been established (Diez-Quevedo et al., 2001; Wulsin et al., 2002). The Spanish translation used in the present study was the one used routinely in the clinics with the collaborative care program, within the system of care we studied. Study staff reviewed that translation for general issues and compatibility with Central and South American language styles before it was implemented. A PHQ9 cut-off of ≥ 10 was required for participation in the parent study.
Trauma exposure was assessed with five questions covering physical violence, sexual violence, witnessing violence, being controlled by a family member (emotional abuse), and a general question about any other extreme situation not already covered. Questions were modified from a trauma exposure measure used in the collaborative care clinic at intake (Kaltman et al., 2011).
PTSD was evaluated with the PTSD Checklist for DSM-IV (PCL; Weathers et al., 1993; Walker et al., 2002), among participants who endorsed at least one trauma exposure. The PCL has good reliability and validity with structured interviews for PTSD (Blanchard et al., 1996), and it has been used in studies of Latino immigrants (Eisenman et al., 2008; Fortuna et al., 2008; Kaltman et al., 2017, under review). Presumptive PTSD was defined by a score ≥ 30 (National Center for PTSD, 2014).
-
Medical Record (chart review) provided information about diagnoses, treatment for depression/other mental disorders, type of treatment, sessions, and medications taken, over a one-year time period preceding the parent study follow up interview.
At parent study follow up, depression was reassessed, and patients reported what types of treatment they were aware of receiving for their depression, and their satisfaction with treatment.
New data collected as part of this study (telephone interview survey - Part 1)
Current level of depression was re-assessed with the PHQ-9.
Knowledge about anti-depressants was collected via a measure used by Chandra et al. (2009), which included questions about benefits/effects, usage, and safety of antidepressants.
Additional questions
Patients were asked about their specific medications, as well as any side effects, how long they took the medication(s), and whether it was helpful. Patients were also asked how they learned about their medications’ purpose, risks, benefits, side effects, and what to do if they encountered problems. The questions were translated into Spanish and back-translated. Three bilingual Spanish-fluent Latino staff reviewed the translation.
Data Analysis
Descriptive analyses were conducted for demographic variables, and anti-depressant medication knowledge and use-related questions. Responses to the additional questions were either yes/no or short answers that were easily tallied. One study team member reviewed the interview tapes and tallied the responses onto a spreadsheet, and a second member reviewed the responses. An additional team member reviewed any unclear responses for final scoring. Details of follow-up responses informed the development of the focus group questions for the next part of the study. A repeated-measures ANOVA using SPSS, Version 22 for Windows (IBM, 2013) was used to compare PHQ scores for the current participants across the two parent-study data collection points and the current Part 1 telephone interview.
Results
All participating patients were Latinos, and 86% were women, with a mean age of 47.04 (SD = 11.52). Only about one third (36%) had completed high school, while 18% reported no formal education. They came from nine countries; most were from El Salvador (29%) or Guatemala (25%). A large proportion (86%) reported experiencing at least one traumatic event.
Final PHQ-9 depression scores for the parent study sample were significantly reduced from baseline (M = 14.79; SD = 3.84) to parent study follow-up (M = 6.59; SD = 5.70), with follow-up occurring an average of 8.2 months after baseline. Nearly two-thirds (64%) were below the clinical cutoff of 10 on the PHQ at follow-up. For the Part 1 study sample, initial PHQ scores averaged 16.96 (SD = 3.74), and the scores at the parent study follow-up averaged 7.82 (5.73). Both scores were slightly higher than for the sample as a whole. Among these 28 patients, 82% (23) met presumptive PTSD criteria at baseline.
The telephone interview component (Part 1) took place an average of 10.5 months after the parent study follow up. At that time, study participants had a PHQ-9 average of 8.36 (SD = 4.24) and 57% were still below the clinical cut-off of 10. This over-time change from parent study baseline, to parent study follow-up, to Part 1 follow-up, was significant (F [2, 81] = 31.70, p < .001), with most of the change occurring between baseline and parent study follow-up.
Patients typically were prescribed one (46%) or two (36%) antidepressant medications over the period we followed them, usually sequentially. The most common medications were citalopram (39% at some point), buproprion (21%), and sertraline (21%). At the time of the study interview, 37% of patients reported that they were still taking their medications as directed, with another 14% still taking medications but not fully as directed. Most (82%) of the sample reported taking medication for two months or more, yet only 54% reported taking the medications as recommended. A small minority reported only taking them PRN (14%). See Table 1 for responses to the Chandra questionnaire and to the added questions. Most patients agreed that antidepressants can help treat depression (68%), and that they are safe for most individuals (61%). However, they held the possibly contradictory views that medications must be taken daily for several weeks to ensure that they work (89%), but also that most people feel better within the first week (57%). Thirty-nine percent felt that these medications are addictive.
Table 1.
Medication Questions
| Chandra Scale Item (N = 28) | Agree (%) |
|---|---|
| Antidepressant medicines can help treat people’s depression by helping improve sleep, energy, and appetite | 68% |
| Antidepressant medicines are usually addictive | 39% |
| Antidepressant medications must be taken every day for several weeks to ensure they work | 89% |
| Most people feel better within a week of starting antidepressant medications | 57% |
| Antidepressant medications are safe for most individuals | 61% |
| Additional Questions | |
| Taking the medications went well | 68% |
| Medications made them feel better | 75% |
| Took medications for recommended amount of time | 57% |
| Took medications only when experiencing symptoms (PRN) | 14% |
Most patients reported that taking the medications “went well” (68%) and that the medications made them feel better (75%). Over half (54%) reported experiencing side effects, including sleepiness, insomnia, anxiety, and worsened depression. We asked those patients how they responded to negative side effects. Twelve percent reported that they switched medications, 24% changed medication dosage, and 12% adjusted their medication routine (e.g., took pills at a different time). Nineteen percent of the patients reported that they didn’t feel that the medications were helping. About half eventually discontinued their medications; 19% simply ran out of medications and did not refill their prescriptions. Of these, 31% felt better, and 38% felt worse. Only 50% of those discontinuing medication told their doctors.
Table 2 shows sources where patients reported receiving information about antidepressant medications and about their particular medication. Few patients reported receiving information about their medications verbally from their providers (23%). Most patients received some information from the clinic, including from other providers. While 60% of patients remembered getting written information, not all of it was in Spanish, their primary language. Only five patients did not report receiving information in some form/from some source (18%). Patients clearly sought out information on their own, including from pharmacists and the Internet.
Table 2.
Information received about Medications (N = 28)
| Received a verbal explanation | 23% |
| Received written materials | 61% |
| Spanish brochure | 28% |
| English brochure | 33% |
| Other depression information | 33% |
| Information received from | |
| Doctor | 16% |
| Mental health counselor | 11 % |
| Other clinic personnel | 26% |
| Pharmacy | 21% |
| Multiple sources | 21% |
| Sought other sources of information (e.g., Internet) | 33% |
Part 2 - Focus Groups
Methods
The purpose of Part 2 of the study was to follow up on the more closed ended and informational questions from the interview (e.g., Morgan, 1996), and to provide a comfortable environment for reviewing previously obtained critiques of current practices, as well as practical suggestions for new practices and formats that could be passed on to providers, and used to develop new materials.
Patients
Each of the 28 patients who participated in this study’s telephone interview (Part 1) was invited to attend a focus group. A total of 12 patients accepted our invitation and attended one of the groups. To best accommodate participants’ availability, we offered the option to attend a focus group at either clinic to have a choice of location, times, and dates. Some participants declined because they could not make the times offered (8), and one (1) had surgery scheduled. Others accepted the invitation, but we were not able to reach them to confirm (4), or they did not show up (3). We did not collect new demographic data at the focus groups, which were anonymous; however the target population from which the Focus Group participants were derived was described for Part 1.
Procedure
After the interviews were completed, the study team met to review the responses and to formulate the final questions for the focus groups, revising the originally proposed questions as needed. This review led us to include several questions about what information was NOT forthcoming, what information the patients would have liked to have received, and which professionals, from the patient perspective, should provide the information, in addition to our focus on best ways to convey needed information. The focus group guide was reviewed by study team members for clarity, completeness, and fit with the interview data. The topic areas for discussion can be found in Table 3.
Table 3.
Focus Group Questions and Themes: Information about Prescribed Antidepressants and Ways to Convey Information
| Questions | Themes |
|---|---|
| 1. When giving patients information about doctor-prescribed antidepressants… What information you think should be included? |
|
| 2. When you think back to the conversation you had when you received your antidepressant prescription…Were there pieces of information that you would have like to have had but didn’t get? |
|
| 3. Who do you think should provide this type of information to patients? |
|
|
4. What types/formats of information/materials would be helpful in having this discussion? [-Would you prefer written materials, or some other format?] [-Should information be in Spanish, English or both?] |
|
Patients were invited to participate in an anonymous focus group to further discuss their medication experiences and to make recommendations to the researchers about the best way to disseminate information about medication to patients. They were also asked to suggest types of materials that would be useful. The group was presented to them as a follow-up to the telephone interview, with the goal of eliciting ideas and opinions from the participants. Consent for the focus group had been included in the Part 1 consent; a separate consent to record the group discussion was obtained on site. Upon arrival, the purpose and procedures of the study were explained and participants were given the opportunity to ask questions. Following the focus group, participants received a $20 gift card for their participation. Three groups were held, two at the collaborative care clinic where two-thirds of the participants received their care, and one in the clinic with the therapist. Two bilingual, bicultural staff members with extensive experience in facilitating focus groups among diverse low-income populations conducted each group in Spanish.
Data analysis
One of the investigators conducting each focus group generated detailed notes in English, aided by the audiotape and following the formatted questions that structured the groups. The notes were then reviewed for completeness and accuracy, alongside each original audiotape. Direct quotes that illustrated certain points were transcribed verbatim into the notes. A fourth staff member summarized each group according to the focus group guide, and integrated the three reports into a summary document, making sure that each patient suggestion was incorporated, and that relevant quotes were reviewed and included. Another staff member compared the original notes per group to the summary document to insure that no information was missed. The summary document and quotes were used to describe the findings.
Results
The focus group questions are summarized in Table 3, along with the themes that came up in the discussion corresponding to each question. These themes are briefly described below, with selected patient quotes in italics. Note that while the themes usually came up in the segment of the focus group where the corresponding questions were asked, we organized the themes in the table, and in the results below, according to where they fit rather than when they were specifically raised in the group. For example, if someone brought up something they wish the provider had told them, but didn’t, when we were asking about materials and formats, it would still be listed under Question 1 rather than Question 4 in the table and this discussion.
Information that should be Included/Missing Information
Questions 1 and 2 are discussed together in the following section because they both were designed to get at similar information. Participating patients reported not receiving sufficient information about side effects such as memory loss, and appetite changes, about possible benefits or outcomes they should expect, for example, specific benefits of taking the medication (e.g., not just that the “medication would help them to feel better”), or about contraindications and drug/alcohol interactions. They also felt that there should be more verbal information about how the medication works, checking that patients understand the information.
“I didn’t read anything. I don’t speak English. If I asked my children they would help me, but I’ve never said anything to anyone. No one in my family knew I was taking antidepressant medication.”
As we learned from the Chandra scale in the interview study, a side effect that worried a number of patients was the possibility of becoming addicted to the medication, so patients wanted more information about that.
“I lived the experience of addiction to medication through my mother, so none of the information provided to me was enough to reduce my fear of becoming an addict.”
They suggested that providers should clarify risks, but also should clarify the tradeoffs to get better. For example, a patient looked up the prescribed antidepressant on the Internet, and it listed ‘hair loss’ as one of the side effects, so she decided not to take the medication.
“I wouldn’t mind losing weight but not my hair.”
Interestingly, although they were taking medications, many patients felt that they also wanted to know more about alternatives to medication, like yoga, exercise, and therapy.
“Sometimes you need to talk to someone and then you feel better. It would be helpful to have that along with the medicine.”
“Taking medication and feeling better is great… however, it is necessary … to be able to function without medication….”
Appropriate Providers of the Information about Medication (Question 3)
Some patients indicated that the primary care provider/”doctor” would be the most appropriate person to provide medication information, while others suggested that the psychiatrist and/or the mental health provider would be best because they understand the mental health condition.
“If I tell the [primary care] doctor how I’m feeling and he sends me to the psychologist, it shows me he is not prepared to deal with that type of problem... So, the best person to prescribe you and inform you is a mental health specialist.”
Other providers like nurse practitioners, health educators, and pharmacists were also mentioned for this role. Patients see that doctors have limited time, and suggested that a “counselor” could provide this information. (Note: in one of the clinics the therapist was involved in helping the patients understand the medication. It is not always clear to whom the patients were referring when they said “counselor.” Because this word came up almost exclusively in the clinic with the collaborative care program, participants may have been referring to the care manager).
Types of Materials that would be Helpful (Question 4)
Participants endorsed receiving information in multiple formats, including both verbal and written instructions and medication information, in Spanish, even though many patients don’t read well (hence the emphasis on verbal information); and they suggested that materials be in large font. They also recommended peer-group support like discussions with other antidepressant medication patients. Patients positively recommended videos, suggesting that these could cover more information, and would be a solution for those who cannot read (Spanish nor English). Videos could be combined with a book/brochure for reinforcement, using pictures for those who don’t read; and it was suggested that a peer discussion group could view a video together and then discuss it.
Discussion
This mixed-method exploratory study was designed to better understand low-income Latino primary care patients’ knowledge about depression and antidepressants, attitudes about taking them, needed information about how the medications work, and recommendations for how medication information would best be presented to patients. It followed up depressed patients taking medication from a previous prospective “parent” study, providing a beginning understanding of specific issues and concerns of the target patient population.
The parent sample from which the study sample was drawn presented with baseline levels of depression similar to those found in other studies of depressed Latino patients in primary care (e.g., Ishikawa et al., 2014). The current study sample experienced significant trauma exposure (86% reported at least one traumatic event), and a substantial percentage (82%) also met criteria for PTSD. This comorbidity increased the likelihood that the presentation of their mental health symptoms would be more complex, and could have complicated their depression treatment with either medication or therapy (Green et al., 2006). At baseline they were more depressed than the average in the parent study sample from which they were drawn, as might be expected from a subgroup of patients who were taking medication for their depression. Because the parent sample also had high rates of trauma (over 80%) and PTSD (64% and 68% respectively in the two clinics), we suggest that culturally similar depressed primary care populations may also have high trauma and PTSD rates that may go unexplored and treated.
Many of the medications for depression are also effective in treating PTSD (e.g., Friedman and Davidson, 2014), which may have contributed in part to the positive responses to the medications among the study sample. Over two-thirds of patients said that antidepressants can be helpful, that they are usually safe, that taking the medications went well, and that the medications made them feel better. They also reported good adherence, with over 80% of patients reporting taking medications for two months or more. However, less than 60% of patients said they took the medications for as long as recommended. Despite this inconsistency, their PHQ scores were significantly improved. We did find however, that 50% of the patients who discontinued their medication did not inform their providers. This finding suggests that it is important to emphasize continuous patient education on the part of the primary care providers regarding prescribed medications, not just when the prescription is provided, but over time. And patients can be reminded that discontinuing medications is an important step as well, and should be discussed with their providers.
The level of depression, and the high proportion of patients with PTSD, may have driven patients’ willingness to try medications (Aikens et al., 2008; Bauer et al., 2013; Fawzi et al., 2012) and resulted in the positive reported adherence rates. A few studies including Latino patients have shown better adherence to medications than to psychotherapy (Ishiwaka et al., 2014; Miranda et al., 2003), perhaps because of the time commitment required in psychotherapy, especially among individuals who may have unpredictable work schedules (Miranda and Green, 1999).
We did find a noteworthy minority of patients who were concerned about addiction. This concern has been raised in other studies, and it is associated with less willingness to take medications (Bauer et al., 2013; Fawzi et al., 2012; Vargas et al., 2015). Patients vary widely in their familiarity with any medications, psychotropic or otherwise. As a result, they may be understandably unclear on whether psychotropic medications could be addictive. This suggests an important aspect of education to be covered by providers in their discussions with patients.
In the focus groups, patients delineated areas where there were deficiencies of information, as well as what information they needed to know in order to feel prepared and comfortable taking the medications for their mental health condition. While some desired written information, many reported that they did not read well, even in their native language, and there is a paucity of simple language information in Spanish, another area for development. Patients also suggested the need for more detailed information about their specific medications, not just assurances that medications would be helpful. And they expressed the need to feel confident in their understanding of their prescribed medications, so they would not need to ask questions of family members and friends. These comments suggest that some providers may at times “talk down” to patients, or expect them to follow the provider’s recommendation without sufficient discussion and shared decision-making (Elwyn et al., 2012; Watson, 1996). While partnering with the patient to make decisions together is likely more difficult to achieve when providers and patients do not speak a common language, and when patients are not highly educated, the response of the patients suggests that the goal to be more specific is an important one.
Patients expected to receive information from their primary care providers, since these were usually the prescribers. However, some patients thought that mental health professionals should supply the information, since they were likely to know more about the medications, even though patients rarely see a mental health professional for medications. In the clinic with the on-site therapist (a master’s level social worker), the therapist herself sometimes helped to supply information about medications to patients who were also in therapy. Patients in the collaborative care program saying that the “counselor” supplied information about medications were most likely referring to a care manager.
At both study sites, the therapists and care managers were Latino, thus it is not surprising that the patients were reportedly more likely to get information from them in Spanish. Conveying appropriate information is a major concern in settings where the providers have a limited grasp of the primary language of their patients. Patients were not necessarily literate in reading their primary language, and most had less than a high school education. Patients were particularly pleased – and even anecdotally enthusiastic, about the idea of using videos to convey needed medication information. Videos do not require written comprehension to convey information, and could employ diagrams and other non-verbal media. As the patients pointed out, they could watch these alone, then talk with the provider later, or even watch them in groups, followed by a discussion. This pointed to a very important and relatively straightforward approach for developing and disseminating useful information in Spanish and other common languages of primary care patients: using simple language, pictures, and videos, with the possibility of having patients themselves help design the content and messages that can be more impactful. Based on responses from both components of the study, information on medications at primary care clinics for the underserved need to be more aligned in terms of language and literacy level, including language and educational level-appropriate written informational supplements.
Others have suggested the use of print fotonovelas (Cabassa et al., 2012), which are posed photos of individuals (or cartoons) with bubble texts containing educational messages and stories. Cabassa and colleagues (2012) developed a fotonovela for depression information for Latinos with limited English proficiency. Alternative materials like “fotonovela,” videos, and other illustrated materials can help low-literacy and limited English proficiency patients understand the need for seeking mental health care and adhering to prescribed treatment.
While information given to the patients by the prescribing providers was not ideal, patients did seek out and received information from a variety of sources, including other providers like nurses, care managers, pharmacists, community residents, and the Internet. This is important because of the lack of relevant and useful information available regarding medications, and the potential misinformation and misbeliefs in their community at large (Watson et al., 2013).
There are several study limitations. First, we had limited sample sizes and limited generalizability to other populations. It is not clear how the 28 participants in the final interview sample represented the original 43 targeted individuals, or how generalizable results would be to other settings. The individuals in the study were low-income patients from Central and South America, and the findings may not generalize to other Latino populations in the US. In an attempt to standardize the data collection for Part 1, only one interviewer was employed. This person was a trained and experienced Latina, who obviously facilitated participation. However, it is possible that the use of only one interviewer may have introduced response bias. The focus groups comprised an even smaller number of patients from the target population, so their specific suggestions may not be representative of what other patient groups may prefer.
Both study sites serve low-income, uninsured, and potentially undocumented or recent immigrant populations. These patient populations are characterized by having low education and literacy levels, some without written fluency in their primary language. Therefore, the results are specifically relevant to very selected patient groups. Nevertheless this study provides some beginning insights and recommendations that may be helpful to other depressed non-English speaking groups and potentially to other underserved/uninsured populations as well.
Although the results are modest in scope and the sample is small, It is important to continue addressing these issues in primary care settings, given that many people, especially minorities, prefer to receive mental health treatment in primary care (Alegria et al., 2002; Ault-Brutus and Alegria, 2016; Cabassa et al., 2006; Dobalian and Rivers, 2008; SAMHSA, 2015). It is even more critical when specialty care is less available, such as among those who do not have insurance. Many of the participants here were undocumented residents without access to insurance. Primary care providers are potentially able to address these medication needs, which can be provided free of charge in many cases, and it is appropriate for them to do so, especially as clinics develop resources and skills for non-English speaking patients.
Our study adds to the literature on attitudes about medications among Latinos with depression, primarily low-income and low education monolingual Spanish speaking immigrants. These individuals had depression, high levels of trauma exposure and PTSD, and were actually taking medications rather than commenting on them in general terms. Study participants were part of a longitudinal study over a relatively long follow up period; this study’s interview was their third contact with the investigation team. The focus groups allowed them to tell us about their experiences and their recommendations in this context, and in their own words.
Acknowledgments
Funding:
Improving Mental Health Services for Low-income Latinos in Primary Care. B.L. Green, PI, (NIMH; MH081809)
Knowledge Regarding Antidepressant Medication among Depressed Latino Patients in Primary Care. B.L. Green, PI. Supported by Georgetown University Center of Excellence in Regulatory Science and Innovation (CERSI; U01FD004319). This research does not necessarily reflect the views of the FDA
The effort and support of the following individuals is acknowledged: Mr. Steve Galen, Dr. Elise Riley, Dr. Susan Pankratz, Mr. Edwin Velis, Ms. Marlene Printz, Ms. Jennifer Pauk, Ms. Karen Orozco, and Ms. Maryen Vemuri, and the clinicians and staff at the two study clinics.
References
- Aikens JE, Nease DE, Kliinkman MS. Explaining patients’ beliefs about the necessity and harmfulness of antidepressants. Ann Family Med. 2008;6:23–29. doi: 10.1370/afm.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Ríos R, Vera M, Calderón J, Rusch D, Ortega AN. Mental health care for Latinos: Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino Whites. Psychiatr Serv. 2002;53:1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- Alexandre P, Martins S, Richard P. Disparities in adequate mental health care for past-year major depressive episodes among Caucasian and Hispanic youths. Psychiatr Serv. 2009;60:1365–1371. doi: 10.1176/ps.2009.60.10.1365. [DOI] [PubMed] [Google Scholar]
- Anastasia E, Bridges A. Understanding service utilization disparities and depression in Latinos: The role of fatalismo. J Immigr Minor Health. 2015;17:1758–1764. doi: 10.1007/s10903-015-0196-y. [DOI] [PubMed] [Google Scholar]
- Ault-Brutus A, Alegria M. Racial/ethnic differences in perceived need for mental health care and disparities in use of care among those with perceived need in 1990–1992 and 2001–2003. Ethnicity Health. 2016;21:1–16. doi: 10.1080/13557858.2016.1252834. [DOI] [PubMed] [Google Scholar]
- Bandiera FC, Pereira DB, Arif AA, Dodge B, Asal N. Race/ethnicity, income, chronic asthma, and mental health: A cross-sectional study using the behavioral risk factor surveillance system. Psychosom Med. 2008;70:77–84. doi: 10.1097/PSY.0b013e31815ff3ad. [DOI] [PubMed] [Google Scholar]
- Bauer A, Schillinger D, Parker M, Katon W, Adler N, Adams A, Moffit HH, Karter A. Health literacy and antidepressant medication adherence among adults with diabetes: The Diabetes Study of Northern California (DISTANCE) J Gen Intern Med. 2013;28:1181–1187. doi: 10.1007/s11606-013-2402-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazargan M, Chizobam O, Hindman D, Bazargan S, Baker S, Bell D, Rodriguez M. Correlates of complementary and alternative medicine utilization in depressed, underserved African American and Hispanic patients in primary care settings. Journal Altern Complem Med. 2008;14:537–544. doi: 10.1089/acm.2007.0821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: National health interview survey, 2012. Vital and Health Statistics Report Series. 2014;10 Retrieved from http://www.cdc.gov/nchs/data/series/sr_10/sr10_260.pdf. [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist. Behav Res Ther. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Cabassa LJ, Lester R, Zayas LH. “It’s like being in a labyrinth:” Hispanic immigrants’ perceptions of depression and attitudes toward treatments. J Immigr Health. 2007;9:1–16. doi: 10.1007/s10903-006-9010-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabassa LJ, Molina GB, Baron M. Development of a depression literacy tool for Latinos with limited English proficiency. Health Promot Prac. 2012;13:747–754. doi: 10.1177/1524839910367578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabassa LJ, Zayas LH, Hansen MC. Latino adults’ access to mental health care: A review of epidemiological studies. Adm Policy Ment Hlth. 2006;33:316–330. doi: 10.1007/s10488-006-0040-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra A, Scott MM, Jaycox LH, Meredith LS, Tanielian T, Burnam A. Racial/ethnic differences in teen and parent perspectives toward depression treatment. J Adolescent Health. 2009;44:546–553. doi: 10.1016/j.jadohealth.2008.10.137. [DOI] [PubMed] [Google Scholar]
- Clark C, Ryan L, Kawachi I, Canner MJ, Berkman L, Wright RJ. Witnessing community violence in residential neighborhoods: A mental health hazard for urban women. J Urban Health. 2008;85:22–38. doi: 10.1007/s11524-007-9229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez-Quevedo C, Trangil T, Sanchez-Planell L, Kroenke K, Spitzer RL. Validation and utility of the Patient Health Questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom Med. 2001;63:679–686. doi: 10.1097/00006842-200107000-00021. [DOI] [PubMed] [Google Scholar]
- Dobalian A, Rivers PA. Racial and ethnic disparities in the use of mental health services. J Behav Health Ser R. 2008;35:128–141. doi: 10.1007/s11414-007-9097-8. [DOI] [PubMed] [Google Scholar]
- Dwight-Johnson M, Sherbourne CD, Liao D, Wells KB. Treatment preferences among depressed primary care patients. J Gen Intern Med. 2000;15:527–534. doi: 10.1046/j.1525-1497.2000.08035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenman DP, Gelberg L, Liu H, Shapiro MF. Mental health and health-related quality of life among adult Latino primary care patients living in the United States with previous exposure to political violence. JAMA. 2003;290:627–634. doi: 10.1001/jama.290.5.627. [DOI] [PubMed] [Google Scholar]
- Eisenman DP, Meredith LS, Rhodes H, Green BL, Kaltman S, Cassells A, Tobin JN. PTSD in Latino patients: Illness beliefs, treatment preferences, and implications for care. J Gen Intern Med. 2008;23:1386–1392. doi: 10.1007/s11606-008-0677-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, Cording E, Tomson D, Dodd C, Rollnick S, Edwards A, Barry M. Shared decision making: A model for clinical practice. J Gen Intern Med. 2012;27:1361–1367. doi: 10.1007/s11606-012-2077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fawzi W, Abdel M, Yousry M, Hashem A, Moussa S, Coker E, Wilson K. Beliefs about medications predict adherence to antidepressants in older adults. Int Psychogeriatr. 2012;24:159–169. doi: 10.1017/S1041610211001049. [DOI] [PubMed] [Google Scholar]
- Fortuna LR, Proche MV, Alegria M. Political violence, psychosocial trauma, and the context of mental health services use among immigrant Latinos in the United States. Ethnic Health. 2008;13:435–463. doi: 10.1080/13557850701837286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman JJ, Davidson JRT. Pharmacotherapy for PTSD. In: Friedman MJ, Keane TM, Resick PA, editors. Handbook of PTSD: Science and practice. New York: The Guilford Press; 2014. pp. 482–501. [Google Scholar]
- Green BL, Krupnick JL, Chung J, Siddique J, Krause E, Revicki D, Frank L, Miranda J. Impact of PTSD co-morbidity on one-year outcomes in a depression trial. J Clinical Psychol. 2006;62:815–835. doi: 10.1002/jclp.20279. [DOI] [PubMed] [Google Scholar]
- Hirai M, Vernon L, Popan J, Clum G. Acculturation and enculturation, stigma toward psychological disorders, and treatment preferences in a Mexican American sample: the role of education in reducing stigma. J Latino/a Psychol. 2015;3:88–102. [Google Scholar]
- IBM Corporation. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp; 2013. [Google Scholar]
- Interian A, Ang A, Gara M, Rodriguez M, Vega W. The long-term trajectory of depression among Latinos in primary care and its relationship to depression care disparities. Gen Hosp Psychiatry. 2011;33:94–101. doi: 10.1016/j.genhosppsych.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Interian A, Martinez IE, Guarnaccia PJ, Vega WA, Escobar JI. A qualitative analysis of the perception of stigma among Latinos receiving antidepressants. Psychiatr Serv. 2007;58:1591–1594. doi: 10.1176/appi.ps.58.12.1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishikawa R, Cardemil E, Alegria M, Schuman C, Joseph R, Bauer A. Uptake of depression treatment recommendations among Latino primary care patients. Psycholol Serv. 2014;11:421–432. doi: 10.1037/a0035716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm AF. Mental health literacy: Empowering the community to take action for better mental health. Am Psychol. 2012;67:231–243. doi: 10.1037/a0025957. [DOI] [PubMed] [Google Scholar]
- Kaltman S, Hurtado de Mendoza A, Gonzales FA, Serrano A. Preferences for trauma-related mental health services among Latina immigrants from Central America, South America, and Mexico. Psychol Trauma: Theor Res, Prac Pol. 2014;6:83–91. [Google Scholar]
- Kaltman S, Hurtado de Mendoza A, Gonzales F, Serrano A, Guarnaccia PJ. Contextualizing the trauma experience of women immigrants from Central America, South America, and Mexico. J Trauma Stress. 2011;24:635–642. doi: 10.1002/jts.20698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaltman S, Hurtado de Mendoza A, Serrano A, Gonzales FA. A mental health intervention strategy for low-income, trauma-exposed Latina immigrants in primary care: A preliminary study. Am J Orthopsychiat. 2017;86:345–354. doi: 10.1037/ort0000157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Bruce ML, Koch JR, Laska EM, Leaf PJ, Manderscheid RW, Rosenheck RA, Walters EE, Wang PS. The prevalence and correlates of untreated serious mental illness. Health Serv Res. 2001;36:987–1007. [PMC free article] [PubMed] [Google Scholar]
- La Roche MJ. Psychotherapeutic considerations in treating Latinos. Harvard Rev Psychiatry. 2002;10:115–222. doi: 10.1080/10673220216214. [DOI] [PubMed] [Google Scholar]
- Lagomasino IT, Dwight-Johnson M, Miranda J, Zhang L, Liao D, Duan N, Wells KB. Disparities in depression treatment for Latinos and site of care. Psychiatr Serv. 2005;56:1517–1523. doi: 10.1176/appi.ps.56.12.1517. [DOI] [PubMed] [Google Scholar]
- Lanouette NM, Folsom DP, Sciolla A, Jeste DV. Psychotropic medication nonadherence among United States Latinos: A comprehensive literature review. Psychiatr Serv. 2009;60:157–174. doi: 10.1176/appi.ps.60.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda J, Chung J, Green B, Krupnick JL, Siddique J, Revicki D, Belin T. Treating depression in predominantly low-income young minority women: A randomized controlled trial. JAMA. 2003;290:57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- Miranda JM, Green BL. The need for mental health services research focusing on poor young women. J Ment Health Policy. 1999;2:73–80. doi: 10.1002/(sici)1099-176x(199906)2:2<73::aid-mhp40>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- Morgan DL. Focus groups. Ann Rev Sociol. 1996;22:129–152. [Google Scholar]
- National Center for PTSD, Veterans Affairs. Using the PTSD Checklist for DSM-IV (PCL) Boston, MA: VA National Center for PTSD; 2014. [Google Scholar]
- Olfson M, Marcus SC, Tedeschi M, Wan GJ. Continuity of antidepressant treatment for adults with depression in the United States. Am J Psychiatry. 2006;163:101–108. doi: 10.1176/appi.ajp.163.1.101. [DOI] [PubMed] [Google Scholar]
- Quinones A, Thielke S, Beaver K, Trivedi R, Williams E, Fan V. Racial and ethnic differences in receipt of antidepressants and psychotherapy by veterans with chronic depression. Psychiatr Serv. 2014;65:193–200. doi: 10.1176/appi.ps.201300057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubenstein LV, Jackson-Triche M, Unutzer J, Miranda J, Minnium K, Pearon ML, Wells KB. Evidence-based care for depression in managed primary care practices. Health Affair. 1999;18:89–105. doi: 10.1377/hlthaff.18.5.89. [DOI] [PubMed] [Google Scholar]
- Ruiz E, Aguirre R, Mitschke D. What leads non-U.S. born Latinos to access mental health care? Soc Work Health Care. 2013;52:1–19. doi: 10.1080/00981389.2012.733326. [DOI] [PubMed] [Google Scholar]
- Russell J, Kazantzis N. Medication beliefs and adherence to antidepressants in primary care. New Zeal Med J. 2008;121:14–20. [PubMed] [Google Scholar]
- Shattell MM, Hamilton D, Star SS, Jenkins CJ, Hinderliter NA. Mental health service needs of a Latino population: A community-based participatory research project. Iss Ment Health Nurs. 2008;29:351–370. doi: 10.1080/01612840801904316. [DOI] [PubMed] [Google Scholar]
- Sleath B, Wurst K, Lowery T. Drug information sources and antidepressant adherence. Community Ment Hlt J. 2003;39:359–68. doi: 10.1023/a:1024080410284. [DOI] [PubMed] [Google Scholar]
- Sorrell T. Mental health treatment preferences for persons of Mexican heritage. Dissert Abstr Intern: Section B – Sci Eng. 2014;74:08E. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of the PRIME-MD: The PHQ primary care study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW. DSM-III and the transformation of American psychiatry: A history. Am J Psychiatry. 1994;151:459–460. doi: 10.1176/ajp.151.3.459. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. SAMHSA. Racial/ethnic differences in mental health service use among adults. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015. (HHS Publication No. SMA-15-4906) [Google Scholar]
- Sue S. In search of cultural competence in psychotherapy and counseling. Am Psychol. 1998;53:440–448. doi: 10.1037//0003-066x.53.4.440. [DOI] [PubMed] [Google Scholar]
- Uebelacker LA, Marootian BA, Pirraglia PA, Primack J, Tigue PM, Haggarty R, Velazquez L, Bowdoin JJ, Kalibatseva Z, Miller IW. Barriers and facilitators of treatment for depression in a Latino community: A focus group study. Community Ment Hlt J. 2012;48:114–126. doi: 10.1007/s10597-011-9388-7. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Mental health: A report of the Surgeon General. Rockville, MD: United States Department of Health and Human Services; 1999. [Google Scholar]
- U.S. Department of Health and Human Services. Healthy people 2010: Understanding and improving health. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- U.S. Department of Health and Human Services. Mental health: Culture, race, and ethnicity--a supplement to mental health: a report of the Surgeon General. Rockville, MD: US Department of Health and Human Services; 2001. [Google Scholar]
- Vargas SM, Cabassa LJ, Nicasio A, De La Cruz AA, Jackson E, Rosario M, Guarnaccia R, Lewis-Fernandez R. Toward a cultural adaptation of pharmacotherapy: Latino views of depression and antidepressant therapy. Int J Env Res Pub He. 2015;52:244–273. doi: 10.1177/1363461515574159. [DOI] [PubMed] [Google Scholar]
- Walker EA, Newman E, Dobie DJ, Ciechanowski P, Katon W. Validation of the PTSD Checklist in an HMO sample of women. Gen Hosp Psychiatry. 2002;24:375–380. doi: 10.1016/s0163-8343(02)00203-7. [DOI] [PubMed] [Google Scholar]
- Watson MR. Diversity, dental public health practice, and the public’s health. J Public Health Dent. 1996;56:3–4. doi: 10.1111/j.1752-7325.1996.tb02386.x. [DOI] [PubMed] [Google Scholar]
- Watson MR, Kaltman S, Townsend TG, Goode T, Campoli M. A collaborative mental health research agenda in a community of poor and underserved Latinos. J Health Care Poor U. 2013;24:671–687. doi: 10.1353/hpu.2013.0079. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist: Reliability, validity, and diagnostic utility. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies; San Antonio, Texas. 1993. Oct, [Google Scholar]
- Woodward S, Berznicki B, Westbury J, Bereznicki L. The effect of knowledge and expectations on adherence to and persistence with antidepressants. J Patient Pref Adher. 2016;10:761–768. doi: 10.2147/PPA.S99803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wulsin L, Somoza E, Heck J. The feasibility of using the Spanish PHQ-9 to screen for depression in primary care in Honduras. Primary Care Comp J Clinical Psychiatry. 2002;4:191–195. doi: 10.4088/pcc.v04n0504. [DOI] [PMC free article] [PubMed] [Google Scholar]