Abstract
Purpose
Appearance-related stress may result from appearance-focused events such as seeing one’s reflection, seeing media images, and shopping for clothes. The purpose of this study was to examine the prospective association between momentary appearance-related stress and eating disorder (ED) behaviors (i.e., binge eating and vomiting) among women with anorexia nervosa (AN) using ecological momentary assessment (EMA). We hypothesized that appearance-related stress at Time 1 would predict binge eating and vomiting at Time 2, and that this prospective association would be mediated by momentary anxiety at Time 2 (controlling for anxiety at Time 1).
Methods
Women with AN completed a two-week EMA protocol involving repeated daily assessments of experiences and behaviors.
Results
Momentary appearance-related stress preceded binge eating and vomiting and momentary anxiety mediated the prospective association between appearance-related stress and ED behaviors.
Conclusions
Targeted momentary interventions delivered in the natural environments that address appearance-related stress may have utility in the treatment of ED behaviors.
Keywords: Anorexia nervosa, appearance, binge eating, purging, anxiety, ecological momentary assessment
The core diagnostic criteria for anorexia nervosa (AN) include maintenance of a low body weight and associated cognitive disturbances (e.g., fear of weight gain) [1]. However, individuals with AN may also engage binge eating and/or purging behaviors, which are maladaptive behaviors associated with marked psychosocial impairment [2]. For example, binge eating and purging are prospectively associated with disturbances in mood, interpersonal problems, and poor physical functioning [3–5]. Further, research has found that patients with AN who regularly engage in binge eating and/or purging have greater eating disorder severity, more co-occurring psychiatric disorders, and a worse overall prognosis compared to patients who do not regularly binge eat and/or purge [6,7].
Focus on appearance, often in the form of body weight and shape concerns, is a central symptom in AN [1]. For example, individuals with AN report more explicit beliefs regarding the importance of appearance compared to a control group [8]. Further, individuals with AN exhibit more negative body image, increased body checking, more anxiety about their body, and increased negativity toward their physical appearance compared to control groups [8–9]. With regard to the daily lives of individuals with eating disorders, appearance-related events (e.g., seeing oneself in the mirror, exposure to body-related media images, shopping for clothes) may occur throughout the day and could be associated with negative self-oriented mental states such as body dissatisfaction and aversive self-awareness--i.e., a negative view of oneself and concern over others’ appraisals of oneself. Appearance-related events may promote dissatisfaction with one’s appearance and body image and, additionally, may increase one’s self-discrepancy (i.e., difference between one’s perceived ideal self and perceived actual self). For instance, in a laboratory study in which individuals were exposed to their bodies by viewing a mirror for 40 minutes, individuals with eating disorders had greater negative emotional and cognitive responses compared to a control group [10]. Also, another study using a mirror exposure task found that women with AN reported greater negative thoughts about eating, weight, and shape than a non-dieting control group [11]. A large literature has also reported associations between viewing images in the media and body dissatisfaction and eating disorder behaviors [12]. Furthermore, studies show that disordered eating and body dissatisfaction are related to more negative experiences shopping for clothes [13–14]. Because appearance-related events often prompt negative self-oriented mental states, stress stemming from these events may also function as momentary risk factors for eating disorder behaviors.
Current Study
Appearance-related events, which are often experienced as stressful given the centrality of appearance concerns in AN, may be particularly important to investigate in relation to binge eating and purging. Furthermore, in research on women with bulimia nervosa, findings have suggested that it is the affective responses following stressful events that accounts for the association between those events and subsequent eating disorder behaviors [15]. Thus, affect may also be of importance in understanding the relationship between appearance-related events and binge eating and purging in AN. To date, we know little about temporal associations among appearance-related stress, associated affective states, and binge eating and purging in the natural environment. In the current study, momentary, naturalistic data collected through ecological momentary assessment (EMA) were used to examine (a) the prospective association between appearance-related stress and binge eating and vomiting among women with AN, and (b) momentary anxiety as a mediator of this association. Although previous naturalistic studies have demonstrated a pattern of increases in various aversive affective states preceding binge eating and vomiting across eating disorder samples [16–18] current study focused on anxiety, as this specific form of affect has been shown to be particularly important in relation to AN. For instance, anxiety and related temperamental constructs (e.g., harm avoidance) have been shown to be prospective risk factors for AN [19–20]. Elevated anxiety persists after recovery from AN and also may differentiate those who do and do not experience remission from AN [21–22]. Further, higher levels of anxiety have been shown to coincide with the occurrence of various eating disorder behaviors in AN [23], and data from several studies also indicate that appearance concerns are distinctly tied to anxiety symptomology [24–26]. Of note, the current data have been used to examine associations related to those investigated here, including between anxiety and binge/purge behaviors [23] and between media exposure and binge/purge behaviors [27] . However, previous papers have not investigated anxiety as a mediator between appearance-related stress (which includes media exposure as one example among several) and binge/purge. Consequently, we believe this paper offers a unique contribution to this literature.
Method
Participants
Women with AN (N = 118) were recruited at three sites in the Midwestern United States via eating disorder treatment facilities, online postings, and clinical, community, and campus advertising. The majority of the sample was Caucasian (96.6%). The mean age was 25.3 ± 8.4 years and the mean body mass index (BMI) was 17.2 ± 1.0 kg/m2. Eligibility criteria included: being female, at least 18 years of age, and meeting criteria for Diagnostic and Statistical Manual of Mental Disorders (4th Edition) [1] AN or subthreshold AN. Subthreshold AN criteria for the study were defined as meeting all of the DSM-IV criteria for AN except: (1) body mass index between 17.5 and 18.5; or (2) absence of amenorrhea or an absence of the cognitive features of AN. There were 73 women with AN-restricting subtype and 45 with AN-binge eating/purging subtype, and the sample was equally split between full-threshold and subthreshold AN.
Measures
Diagnostic interview
The Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-I/P) [28] was used to determine DSM-IV diagnostic criteria for AN and subthreshold AN. SCID interviews were recorded by trained assessors and a second independent assessor rated current eating disorder diagnoses in a random sample of 25% (n = 30) of these interviews. Interrater reliability for current AN diagnosis based upon a kappa coefficient was .929.
EMA measures
The current study used EMA data collected via three types of daily self-report methods using palmtop computers. Event-contingent reporting involved participants completing an assessment when a binge eating or vomiting episode occurred. Signal-contingent reporting required participants to complete an assessment at various times throughout the day in response to six semi-random signals distributed around six anchor points (i.e., 8:30 a.m., 11:10 a.m., 1:50 p.m., 4:30 p.m., 7:10 p.m., and 9:50 p.m.). Interval-contingent reporting involved participants completing an assessment each night before they went to sleep. Momentary appearance-related stress was measured with 3 items asking how stressed an individual felt when they “saw reflections of self,” “shopped for clothes,” and “saw media images about food, shape, or weight.” First, participants indicated “yes” or “no” as to whether the event occurred. If the participant answered “yes,” they were instructed to indicate how much stress they experienced on a scale from 1 (not at all) to 5 (very much). A score of 1 to 5 (i.e., the corresponding stress rating) was assigned to an item when a “yes” was endorsed for that item; a score of 0 was assigned when a “no” was endorsed for the item. . Scores for each item were summed, such that total scores for the 3-item scale could range from 0 to 15. To evaluate internal consistency of these items, we calculated summary scores of the three items for each person. The inter-correlations between the three items were .43, .63, and .64, suggesting consistency without excessive overlap. Appearance-related stress was measured only during random recordings.
Momentary anxiety was assessed using eight items (i.e., on edge, restless, tense, anxious, uneasy, shaky, panicky, and relaxed; α = .92) from the tension-anxiety scale of the Profile of Mood States (POMS-A) [29]. Participants rated each item in terms of their current mood on a 5-point scale ranging from 1 (not at all) to 5 (extremely). Anxiety was assessed at all recordings. For eating disorder behaviors, individuals were instructed to complete an EMA recording when they engaged in binge eating and vomiting. During random recordings, participants were able to report recent episodes of binge eating or vomiting that they had not yet recorded.
Procedure
Institutional review board approval for the study was obtained at each site. Potential participants were initially phone screened. Those who met initial study criteria were invited to attend an informational meeting to receive more information about the study and provide written informed consent if they wished to enroll in the study. Participants were then scheduled for two assessment visits to have a physical examination screening and laboratory tests to ensure medical stability. In addition, participants completed self-report questionnaires and structured interviews during this visit. Participants were trained on how to use the palmtop computers at the end of first assessment. During one of these initial assessment visits, a trained research staff member met with participants to discuss the objectives of the study, what to expect during participation, and how to address any questions that might arise from the signaling of the palmtop computer. Participants were instructed not to complete entries at any times when they felt unable to reply or if safety was a concern (e.g., when driving), but instead to delay responding until a later, more convenient time.
Participants carried the palmtop computer for two practice days. After these practice days, participants returned to the research center and provided the data recorded during their practice period; these data were not used in analyses. This practice period was used to help ensure that participants were familiar with the protocol and to minimize reactivity to the recording procedures. However, previous research suggests that reactivity to EMA monitoring is uncommon [30–31]. A research assistant reviewed practice data and gave feedback to participants regarding their compliance rates and answered any questions about the procedures. Participants were then given the palmtop computer to complete EMA recordings over the following two weeks. To maintain contact with the participants, minimize the loss of data, and proactively address any potential problems, attempts were made to schedule 2–3 visits for each participant during this two-week interval to obtain recorded data. Participants were given feedback at each visit regarding their compliance rates. Participants completed a study evaluation questionnaire at the end of the study and were compensated $100 per week for completing assessments. Additionally, they were offered a bonus of $50 for a compliance rate of at least 80% to random signals.
Data Analytic Plan
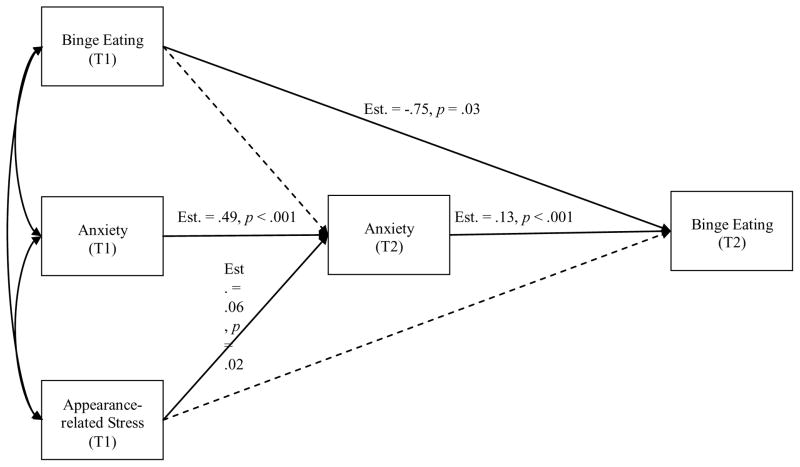
Descriptive statistics were calculated. Multilevel structural equation modeling (MSEM) [33] using Mplus version 7.3 [34] was used to test the proposed mediation model (see Figure 1). A 1-1-1 MSEM was used, which means the independent variable, mediating variable, and dependent variable were all used as Level 1 within-person variables. The independent variable was momentary appearance-related stress at Time 1, the mediating variable was momentary anxiety at Time 2, and binge eating and vomiting at Time 2 were the dependent variables. Time 2 reflects the time when a binge eating or vomiting episode occurred, while Time 1 represents the most proximal momentary rating preceding the binge eating or vomiting episode. Although the length of time between Time 1 and Time 2 varied, the average interval separating the two was 2 hours and 40 minutes. We first tested the direct effect of the independent variable (i.e., momentary appearance-related stress) on eating disorder behaviors. Then, we examined the model with the mediator (i.e., anxiety) added. We tested two separate models: one with binge eating as the outcome and another with vomiting as the outcome. In the mediation models, Time 1 levels of anxiety and binge eating or vomiting were included as covariates of Time 2 anxiety (the mediator), and Time 1 levels binge eating or vomiting were included as a covariate of Time 2 binge eating and vomiting. This allowed us to address whether increases in anxiety precede binge eating and vomiting. The between-subjects effects of appearance-related stress and anxiety were included as predictors of binge eating and vomiting as well.
Figure 1.
Fitted momentary mediation model for binge eating. Solid lines represent significant paths at p = .05; dashed lines represent nonsignificant paths.
Results
Compliance rates to random signals (defined as responding to signals within 45 minutes) averaged 87% across participants (range = 58–100%); 77% of all signals were responded to within 45 minutes. Compliance with end-of-day ratings averaged 89% (range = 24 100%). Across the two weeks of EMA, there were 2867 episodes of seeing one’s reflection, 154 episodes of shopping for clothes, and 686 episodes of seeing media images. The mean stress rating for seeing one’s reflection was 2.90 (SD = 1.30; Range = 1–5); the mean stress rating for shopping for clothes was 2.94 (SD = 1.50; Range = 1–5); and the mean stress rating for seeing media images was 2.82 (SD = 1.31; Range = 1–5). Shopping for clothes was associated with the highest percentage of high stress ratings (i.e., 4 or 5 on 5-point rating scales), followed by seeing one’s reflection and seeing media images (percentages were 38.9, 33.6, and 30.9, respectively).
The average level of appearance-related stress over the course of the EMA protocol was 0.77 (SD = 0.74; Range = 0–5) and the average level of anxiety over the course of the EMA protocol was 2.52 (SD = 0.79 Range = 1–5). Over the course of the EMA protocol, 42% of women (n = 49) reported at least one binge eating episode and 39% of women (n = 46) reported at least one vomiting episode. The mean number of binge eating episodes was 2.26 (SD = 4.45; Range = 0–29) and the mean number of vomiting episodes was 3.79 (SD = 7.92; Range = 0 37). An independent samples t-test revealed that compared to women who reported no binge eating over the EMA protocol, women who reported binge eating over the EMA protocol had a lower number of shopping events, t (116) = −2.94, p =.004. There were no differences in occurrence of seeing one’s reflection or seeing media images between women who reported binge eating versus not binge eating during the EMA protocol. There were no differences in occurrence of any appearance-related events between women who did and did not report vomiting during the EMA protocol.
Binge Eating Model
Time 1 appearance-related stress was first examined alone as a predictor of Time 2 binge eating. Time 1 appearance-related stress significantly predicted Time 2 binge eating (Estimate = .07, SE = .03, p = .03). The fitted mediation model is displayed in Figure 2 and direct and indirect paths estimates are displayed in Table 1. Time 1 appearance-related stress and Time 1 anxiety were entered as predictors of Time 2 anxiety, and Time 1 appearance-related stress and Time 2 anxiety were entered as predictors of binge eating. Time 1 appearance-related stress was significantly associated with Time 2 anxiety (Estimate = .06, SE = .03, p = .02) and not associated with Time 2 binge eating (Estimate = .05, SE = .03, p = .16). Time 1 anxiety was significantly associated with Time 2 anxiety (Estimate = .49, SE = .02, p < .001). Time 2 anxiety was significantly related to Time 2 binge eating (Estimate = .13, SE = .03, p < .001). The formal test of the indirect effect was significant (Estimate = .01, SE = .004, p = .03). Participants who reported greater momentary appearance-related stress at Time 1 had increased momentary anxiety at Time 2. In turn, greater momentary anxiety was associated with binge eating. Momentary anxiety fully mediated the association between momentary appearance-related stress and binge eating. Between-person anxiety was associated with more binge eating (Estimate = .10, SE = .02, p < .001) and between-person appearance-related stress was unrelated to binge eating (Estimate = .32, SE = .26, p = .21). Thus, women who report more anxiety in general engage in more binge eating, although the tendency to experience appearance-related events as stressful was not related to propensity for binge eating.
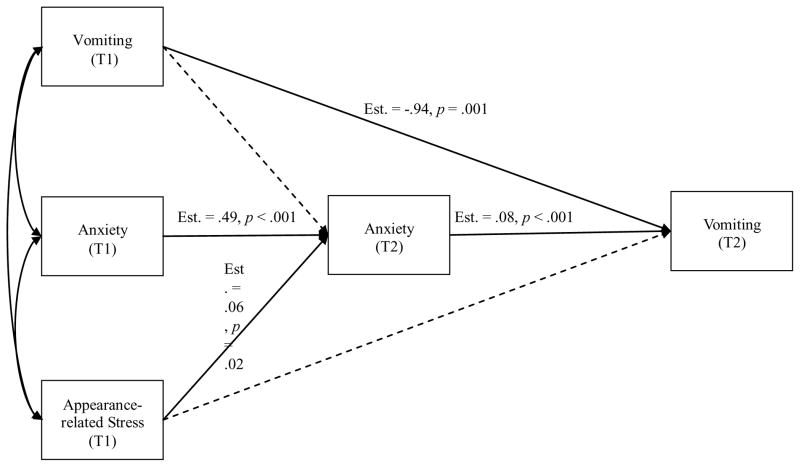
Figure 2.
Fitted momentary mediation model for vomiting. Solid lines represent significant paths at p = .05; dashed lines represent nonsignificant paths.
Vomiting Model
Time 1 appearance-related stress was first examined alone as a predictor of Time 2 vomiting. Time 1 appearance-related stress marginally predicted Time 2 vomiting (Estimate = .07, SE = .04, p = .06). The fitted mediation model is displayed in Figure 3 and direct and indirect paths estimates are displayed in Table 1. Time 1 appearance-related stress and Time 1 anxiety were entered as predictors of Time 2 anxiety and Time 1 appearance-related stress and Time 2 anxiety were entered as predictors of vomiting. Time 1 appearance-related stress was significantly associated with Time 2 anxiety (Estimate = .06, SE = .03, p = .02) and not associated with Time 2 vomiting (Estimate = .06, SE = .04, p = .13). Time 1 anxiety was significantly associated with Time 2 anxiety (Estimate = .49, SE = .02, p < .001). Time 2 anxiety was significantly related to Time 2 vomiting (Estimate = .08, SE = .02, p < .001). The formal test of the indirect effect was significant (Estimate = .01, SE = .002, p = .03). Participants who reported greater momentary appearance-related stress at Time 1 had increased momentary anxiety at Time 2. In turn, greater momentary anxiety was associated with vomiting. Momentary anxiety fully mediated the association between momentary appearance-related stress and vomiting. Neither between-person anxiety (Estimate = −.002, SE = .03, p = .93) nor between-person appearance-related stress (Estimate = −.26, SE = .38, p = .51) was related to vomiting.
Discussion
These findings indicate that appearance-focused events are associated with binge eating and self-induced vomiting. This is consistent with findings from the same data as the current study and found that stress related to media image exposure was prospectively associated with later binge eating and vomiting [27]. However, the present investigation expands upon these prior findings both by examining broader appearance-focused stress, and importantly, by considering the mechanisms underlying these prospective associations. Results demonstrated that momentary anxiety mediated the prospective association between appearance-related stress and eating disorder behaviors. Specifically, appearance-related stress predicted increased anxiety, which in turn, was associated with greater likelihood of engaging in binge eating and vomiting.
The present findings can be considered in light of certain theories of eating disorder psychopathology. For instance, consistent with escape theory of binge eating [35], appearance-related stress may lead to a state of aversive self-awareness, which prompts a negative emotional state that an individual seeks to escape through maladaptive strategies. Thus, when an individual with AN sees herself in the mirror, she may experience begin to feel more anxious due to negative self-judgments of her body shape/weight. This could prompt binge eating or vomiting as a method of coping with the anxiety. Further, consistent with the momentary maintenance model of Integrative Cognitive-Affective Therapy [36], appearance-related stressful events may function to highlight that an individual does not meet her appearance self-standard, resulting in self-discrepancy and appearance-focused stress and, potentially, appearance-focused self-criticism. Eating disorder behaviors such as vomiting may thus be prompted as a maladaptive attempt to reduce appearance-related self-discrepancies.
A notable strength of this study was the use of EMA methodology, which allowed for the examination of momentary mediational processes underlying the occurrence of eating disorder behaviors using temporally sequenced data collected in the natural environment. However, several limitations are important to consider. First, although participants were largely compliant with the EMA protocol, it is possible that not all binge eating and vomiting episodes were recorded. Second, we focused on binge eating and vomiting behaviors; future investigations should also examine the momentary impacts of appearance-related stress on other eating disorder behaviors (e.g., body checking, exercise). Also, while our model offers strong support for mediation, it is possible that third variables could be driving the mediational findings. Finally, our measure of appearance-related stress only included stress ratings from three possible appearance-based events; as such, other events associated with appearance-related stress may be important to assess in future research.
Clinical Implications
The current findings suggest that both appearance-related stress and anxiety may potentially be useful treatment targets, particularly among individuals with AN who binge and/or purge. Further, these results suggest that the inclusion of appearance-related stress in novel, naturalistic interventions — i.e., ecological momentary interventions (EMIs) — may be warranted. More specifically, EMIs are treatments that are delivered in the natural environment through the use of technology and are capable of intervening in real-time [37]. Given that momentary appearance-related stress is a precipitating factor of anxiety and binge eating and vomiting behaviors, EMIs may be particularly efficacious. For example, when individuals with AN experience appearance-related stress, EMIs may be used to intervene by providing psychoeducational material that focuses on reducing anxious reactions to stress as well as adaptively coping with stress. In addition, EMIs may provide clinical and psychoeducational material rooted in principles of self-compassion or emotion regulation [38–39]. Though the specific content may vary, the overarching goal of these EMI strategies is to prevent the occurrence of binge eating and vomiting.
With regard to traditionally delivered psychotherapeutic approaches, the finding that seeing one’s reflection was the most common appearance-related event suggests that targeting individuals’ reactions to their reflection may have clinical utility. Consistent with this concept, one study found that adding a mirror exposure component to inpatient treatment for AN produced less body dissatisfaction and increased reductions in body anxiety compared to treatment without mirror exposure [40]. Another study found evidence for the efficacy of a mirror exposure intervention in improving body image in women dissatisfied with their bodies [41]. In addition, given the increasing focus on emotion-based processes in the treatment of AN [42–43], prevention and intervention efforts may benefit from targeting the role of appearance-related stressors and associated emotional responses.
Conclusion
This study examined a momentary, mediational model of appearance-related stress, anxiety, and eating disorder behaviors (i.e., binge eating and vomiting). Findings revealed that momentary appearance-related stress was an important momentary antecedent to binge eating and vomiting, and importantly, that anxiety mediated the prospective association between momentary appearance-related stress and eating disorder behaviors. Appearance-related stress and associated anxiety may be useful clinical targets in the naturalistic environment. EMIs addressing appearance-related stress and related anxiety may have utility in the treatment of eating disorder behaviors among individuals with AN, and addressing adaptive responding to exposure to appearance-related stressors may be useful in psychotherapeutic approaches for treating AN.
Acknowledgments
Funding: This work was supported by grants R01MH059674 and T32MH082761 from the National Institute of Mental Health.
Footnotes
Conflict of Interest: The authors have no conflicts of interest to report.
Compliance with Ethical Standards: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®) Washington DC: Author; 2013. [Google Scholar]
- 2.Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mason TB, Heron KE. Do depressive symptoms explain associations between binge eating symptoms and later psychosocial adjustment in young adulthood? Eat Behav. 2016;23:126–130. doi: 10.1016/j.eatbeh.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 4.Solmi F, Sonneville KR, Easter A, Horton NJ, Crosby RD, Treasure J, Rodriguez A, Jarvelin MR, Field AE, Micali N. Prevalence of purging at age 16 and associations with negative outcomes among girls in three community-based cohorts. J Child Psychol Psychiatry. 2015;56:87–96. doi: 10.1111/jcpp.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stice E, Bearman SK. Body-image and eating disturbances prospectively predict increases in depressive symptoms in adolescent girls: A growth curve analysis. Dev Psychol. 2001;37:597–607. doi: 10.1037/0012-1649.37.5.597. [DOI] [PubMed] [Google Scholar]
- 6.DaCosta M, Halmi KA. Classifications of anorexia nervosa: Question of subtypes. Int J Eat Disord. 1992;11:305–313. doi: 10.1002/1098-108X(199205)11:4<305::AID-EAT2260110403>3.0.CO;2-2. [DOI] [Google Scholar]
- 7.Fouladi F, Mitchell JE, Crosby RD, Engel SG, Crow S, Hill L, Le Grange D, Powers P, Steffen KJ. Prevalence of alcohol and other substance use in patients with eating disorders. Eur Eat Disord Rev. 2015;23:531–536. doi: 10.1002/erv.2410. [DOI] [PubMed] [Google Scholar]
- 8.Hartmann AS, Thomas JJ, Greenberg JL, Elliott CM, Matheny NL, Wilhelm S. Anorexia nervosa and body dysmorphic disorder: A comparison of body image concerns and explicit and implicit attractiveness beliefs. Body Image. 2015;14:77–84. doi: 10.1016/j.bodyim.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 9.Bamford BH, Attoe C, Mountford VA, Morgan F, Sly R. Body checking and avoidance in low weight and weight restored individuals with anorexia nervosa and non-clinical females. Eat Behav. 2014;15:5–8. doi: 10.1016/j.eatbeh.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 10.Vocks S, Legenbauer T, Wächter A, Wucherer M, Kosfelder J. What happens in the course of body exposure? Emotional, cognitive, and physiological reactions to mirror confrontation in eating disorders. J Psychosom Res. 2007;62:231–239. doi: 10.1016/j.jpsychores.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 11.Cooper MJ, Fairburn CG. Thoughts about eating, weight and shape in anorexia nervosa and bulimia nervosa. Behav Res Ther. 1992;30:501–511. doi: 10.1016/0005-7967(92)90034-E. [DOI] [PubMed] [Google Scholar]
- 12.Spettigue W, Henderson KA. Eating disorders and the role of the media. Can Child Adolesc Psychiatr Rev. 2004;13:16–19. [PMC free article] [PubMed] [Google Scholar]
- 13.Tiggemann M, Lacey C. Shopping for clothes: Body satisfaction, appearance investment, and functions of clothing among female shoppers. Body Image. 2009;6:285–291. doi: 10.1016/j.bodyim.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 14.Trautmann J, Worthy SL, Lokken KL. Body dissatisfaction, bulimic symptoms, and clothing practices among college women. J Psychol. 2007;141:485–498. doi: 10.3200/JRLP.141.5.485-498. [DOI] [PubMed] [Google Scholar]
- 15.Goldschmidt AB, Wonderlich SA, Crosby RD, Engel SG, Lavender JM, Peterson CB, et al. Ecological momentary assessment of stressful events and negative affect in bulimia nervosa. J Consult Clin Psychol. 2014;82:30–39. doi: 10.1037/a0034974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berg KC, Crosby RD, Cao L, Crow SJ, Engel SG, Wonderlich SA, Peterson CB. Negative affect prior to and following overeating-only, loss of control eating-only, and binge eating episodes in obese adults. Int J Eat Disorder. 2015;48:641–53. doi: 10.1002/eat.22401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Engel SG, Wonderlich SA, Crosby RD, Mitchell JE, Crow S, Peterson CB, et al. The role of affect in the maintenance of anorexia nervosa: Evidence from a naturalistic assessment of momentary behaviors and emotion. J Abnor Psychol. 2013;122:709–719. doi: 10.1037/a0034010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. J Consult Clin Psychol. 2007;75:629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- 19.Deep AL, Nagy LM, Weltzin TE, Rao R, Kaye WH. Premorbid onset of psychopathology in long-term recovered anorexia nervosa. Int J Eat Disorder. 1995;17:291–297. doi: 10.1002/1098-108X(199504)17:3<291::AID-EAT2260170310>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 20.Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am J Psychiatry. 2004;161:2215–2221. doi: 10.1176/appi.ajp.161.12.2215. [DOI] [PubMed] [Google Scholar]
- 21.Holtkamp K, Müller B, Heussen N, Remschmidt H, Herpertz-Dahlmann B. Depression, anxiety, and obsessionality in long-term recovered patients with adolescent-onset anorexia nervosa. Eur Child Adolesc Psychiatry. 2005;14:106–110. doi: 10.1007/s00787-005-0431-5. [DOI] [PubMed] [Google Scholar]
- 22.Yackobovitch-Gavan M, Golan M, Valevski A, Kreitler S, Bachar E, Lieblich A, Mitrani E, Weizman A, Stein D. An integrative quantitative model of factors influencing the course of anorexia nervosa over time. Int J Eat Disorder. 2009;42:306–17. doi: 10.1002/eat.20624. [DOI] [PubMed] [Google Scholar]
- 23.Lavender JM, De Young KP, Wonderlich SA, Crosby RD, Engel SG, Mitchell JE, et al. Daily patterns of anxiety in anorexia nervosa: Associations with eating disorder behaviors in the natural environment. J Abnor Psychol. 2013;122:672–683. doi: 10.1037/a0031823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hart TA, Flora DB, Palyo SA, Fresco DM, Holle C, Heimberg RG. Development and examination of the social appearance anxiety scale. Assessment. 2008;15:48–59. doi: 10.1177/1073191107306673. [DOI] [PubMed] [Google Scholar]
- 25.Reed DL, Thompson JK, Brannick MT, Sacco WP. Development and validation of the physical appearance state and trait anxiety scale (PASTAS) J Anxiety Disord. 1991;5:323–332. doi: 10.1016/0887-6185(91)90032-O. [DOI] [Google Scholar]
- 26.Veale D, Eshkevari E, Kanakam N, Ellison N, Costa A, Werner T. The Appearance Anxiety Inventory: Validation of a process measure in the treatment of body dysmorphic disorder. Behav Cogn Psychother. 2014;42:605–616. doi: 10.1017/S1352465813000556. [DOI] [PubMed] [Google Scholar]
- 27.White EK, Warren CS, Cao L, Crosby RD, Engel SG, Wonderlich SA, Mitchell JE, Peterson CB, Crow SJ, Le Grange D. Media exposure and associated stress contribute to eating pathology in women with AN: Daily and momentary associations. Int J Eat Disorder. 2016;49:617–621. doi: 10.1002/eat.22490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM–IV Axis I Disorders: Patient Edition (SCIDI/P) New York: Biometrics; 1995. [Google Scholar]
- 29.Lorr M, McNair DM, Droppleman LF. Manual: Profile of Mood States. San Diego, CA: Educational and Industrial Testing Service; 1971. [Google Scholar]
- 31.Heron KE, Smyth JM. Is intensive measurement of body image reactive? A two-study evaluation using Ecological Momentary Assessment suggests not. Body Image. 2013;10:35–44. doi: 10.1016/j.bodyim.2012.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stein KF, Corte CM. Ecologic momentary assessment of eating-disordered behaviors. Int J Eat Disorder. 2003;34:349–360. doi: 10.1002/eat.10194. [DOI] [PubMed] [Google Scholar]
- 33.Preacher KJ, Zyphur MJ, Zhang Z. A general multilevel SEM framework for assessing multilevel mediation. Psychol Methods. 2010;15:209–233. doi: 10.1037/a0020141. [DOI] [PubMed] [Google Scholar]
- 34.Muthén K, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 2015. [Google Scholar]
- 35.Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychol Bull. 1991;110:86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- 36.Wonderlich SA, Peterson CB, Smith TL, Klein MH, Mitchell JE, Crow SJ. Integrative cognitive-affective therapy for bulimia nervosa: A treatment manual. Guilford Publication; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heron KE, Smyth JM. Ecological momentary interventions: Incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol. 2010;15:1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gale C, Gilbert P, Read N, Goss K. An evaluation of the impact of introducing compassion focused therapy to a standard treatment programme for people with eating disorders. Clin Psychol Psychother. 2014;21:1–12. doi: 10.1002/cpp.1806. [DOI] [PubMed] [Google Scholar]
- 39.Harrison A, Sullivan S, Tchanturia K, Treasure J. Emotion recognition and regulation in anorexia nervosa. Clin Psychol Psychother. 2009;16:348–356. doi: 10.1002/cpp.628. [DOI] [PubMed] [Google Scholar]
- 40.Key A, George CL, Beattie D, Stammers K, Lacey H, Waller G. Body image treatment within an inpatient program for anorexia nervosa: The role of mirror exposure in the desensitization process. Int J Eat Disorder. 2002;31:185–190. doi: 10.1002/eat.10027. [DOI] [PubMed] [Google Scholar]
- 41.Jansen A, Voorwinde V, Hoebink Y, Rekkers M, Martijn C, Mulkens S. Mirror exposure to increase body satisfaction: Should we guide the focus of attention towards positively or negatively evaluated body parts? J Behav Ther Exp Psychiatry. 2016;50:90–96. doi: 10.1016/j.jbtep.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 42.Sala M, Heard A, Black EA. Emotion-focused treatments for anorexia nervosa: a systematic review of the literature. Eat Weight Disord. 2016;21:147–64. doi: 10.1007/s40519-016-0257-9. [DOI] [PubMed] [Google Scholar]
- 43.Wildes JE, Marcus MD. Development of emotion acceptance behavior therapy for anorexia nervosa: A case series. Int J Eat Disorder. 2011;44:421–427. doi: 10.1002/eat.20826. [DOI] [PMC free article] [PubMed] [Google Scholar]