Abstract
This paper describes a paradigm shift occurring in neonatal intensive care. Care teams are moving from a focus limited to healing the baby’s medical problems towards a focus that also requires effective partnerships with families. These partnerships encourage extensive participation of mothers and fathers in their baby’s care and ongoing bi-directional communication with the care team. The term Newborn Intensive Parenting Unit (NIPU) was derived to capture this concept. One component of the NIPU is family-integrated care, where parents are intimately involved in a baby’s care for as many hours a day as possible. We describe six areas of potentially better practices (PBPs) for the NIPU along with descriptions of NIPU physical characteristics, operations, and a relationship-based culture. Research indicates the PBPs should lead to improved outcomes for NIPU babies, better mental health outcomes for their parents, and enhanced well-being of staff.
Introduction
Neonatology has had few clinical breakthroughs in the past several decades, except for ‘niche’ treatments, such as total body cooling,1 that are targeted towards a small number of neonates, and genome-informed precision medicine, whose clinical promises have not yet been realized.2 Few new medicines have come onto the market since surfactant was first approved in 1990. Incremental changes in clinical care have produced corresponding incremental improvements in survival, especially among extremely preterm infants. Although increased survival initially led to larger numbers of infants with developmental impairments, in the last two decades neurodevelopmental outcomes among extremely preterm infants have improved. However, many still face a variety of sequelae from visual and hearing loss, to cognitive impairments and social challenges, to cerebral palsy.3 A recent review confirmed that even those born in the late preterm period are not immune to developmental disabilities, especially in the cognitive domain.4 Future clinical and technological innovations will certainly occur, but we propose that the next major advances in neonatology have already begun by focusing attention on a ‘natural resource’ that, historically, has been undervalued and underutilized, the family-infant relationship. Although babies can survive without their families, optimal physical, cognitive and emotional development occurs only within the context of loving, positive interactions with parents and/or emotionally involved primary caregivers.
Neonatal intensive care units (NICUs) are changing around the world.5, 6 The goals of neonatology are evolving to include optimizing the functioning of the family unit within the hospital to support improved infant as well as parent/infant outcomes. Broadening the focus of neonatal care to the family–infant relationship requires an emphasis on relationships in the unit, both relationships within the family and partnerships among staff and family. These partnerships are based on the premise that intensive parenting should begin as soon as possible and be interrupted only when absolutely necessary. The physical and emotional well-being of the family unit are the guiding concerns because it is known that ultimately, the well-being of the family affects the well-being of the baby.
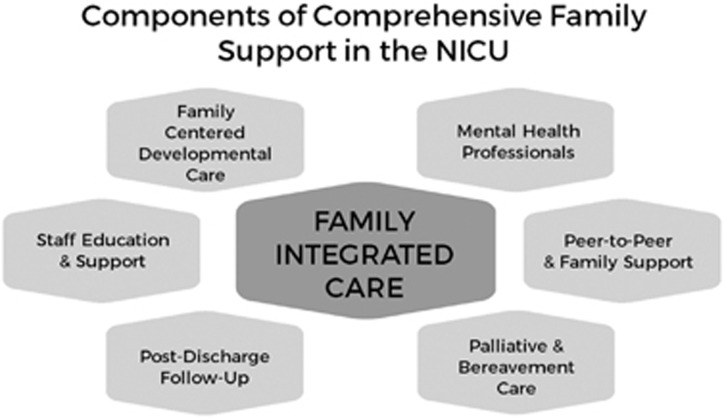
The term Newborn Intensive Parenting Unit (NIPU) was derived to capture this evolution in goals. This model, which began in the ‘We Are Family’ Homeroom of the Vermont Oxford Network (VON) and has been the topic of presentations at the VON Annual Quality Congress, is based on evolving concepts of family-centered7 and family-integrated care (FICare).5, 6 One component of the NIPU is FICare, a model of care where parents are intimately involved in their sick or premature baby’s care for as many hours a day as possible. While FICare serves as the foundation of the NIPU, a set of potentially better practices (PBPs) represent the building blocks surrounding and supporting both parents and staff. We describe six areas of PBPs, along with their empirical foundations, which are derived from the ‘Interdisciplinary Recommendations for the Psychosocial Support of NICU Parents’8 published by the National Perinatal Association in collaboration with many other professional and parent organizations. These include: (1) family-centered developmental care, (2) peer support, (3) mental health support, (4) palliative and bereavement care, (5) post-discharge support and (6) staff education and support.
For NICU staff to successfully carry out the mandate implicit in the enhanced environment envisioned in a NIPU, they will often need new tools as well as additional or expanded supports, many of which are described in the PBPs. Quality support for parenting within families is dependent on educational and emotional support for staff, from the leadership to environmental service providers, and across all disciplines. In the culture of the NIPU, everyone is concerned with the well-being of each other. We anticipate that the NIPU model of care will lead to improved developmental outcomes for babies, better mental health outcomes for their parents, and enhanced well-being of staff. Figure 1 illustrates the six content areas of the PBPs as integrated into FICare.
Figure 1.
Components of Comprehensive Family Support in the NIPU. NIPU, Newborn Intensive Parenting Unit.
Physical characteristics
What does a NIPU look like? The patient care space makes it not only possible, but also comfortable for parents to be present and involved at any time of their choosing, day and/or night (24 h a day and 7 days a week). The NIPU space provides a bed or a comfortable reclining chair for the parents in addition to the usual isolette or crib for the baby. Amenities are provided to support parents’ prolonged presence and active involvement in care. These may include the provision of meals, bathrooms and showers, laundry facilities, access to computers and Wi-Fi, kitchens where families can store and prepare meals, and lounge space where families can gather for peer-to-peer support and education sessions.
Single family rooms (SFRs) provide the privacy that enables families to share special moments together and for parents to grow into and claim their parental roles without the continual watchfulness of the NICU staff. SFRs were designed to optimally support and enhance infant neurobehavioral development through reduction of environmental stress and increased maternal involvement.9, 10 High maternal involvement, especially in a SFR NICU as contrasted with an open-bay design, is associated with improved neurodevelopmental outcome of infants at 18 months of age, and mothers in SFRs had more days of maternal involvement than those in open-bay NICUs.11 It has been suggested that infant development, particularly language development, may suffer in a SFR environment when parents are not able to be present for large periods of time.12 This undesirable outcome in a specific population should not serve as a deterrent to the use of SFRs, as the ultimate goal of a NIPU is to do everything possible to enable all parents to stay in the NIPU for extended periods, even if some may not be able to take advantage of this opportunity. Although SFRs could be considered the ideal arrangement for a NIPU, implementation of the FICare model cannot wait until all units have this patient care configuration. Indeed, the FICare model has already been shown to be successful in open-bay units.6
An essential element of a successful NIPU includes ongoing support of staff. The NIPU should allow for adequate space for staff to convene, for periods of relaxation while on their shifts, for collaborative interdisciplinary meetings and conferences, and for educational sessions.
Operational characteristics
The predominant operational feature of a NIPU is that the focus is on the family from the very first moment that a NIPU admission is anticipated. During antenatal consultations with high-risk mothers, during labor and delivery, or at the point of a baby’s referral to the NIPU from an outside hospital, the parents are engaged in their baby’s care by partnering with staff through fully transparent communication and shared decision-making.7 Parent–baby separation is minimized. Parental presence is always welcomed, including at shift change, on medical rounds,13 and during procedures if the parents desire.14 Parents and family are never considered ‘visitors’ or outsiders.
When members of the care team form equal partnerships with parents, roles evolve to enable shared decision-making. Although professionals have the clearest medical knowledge and the most clinical experience in deciding what is medically best for a baby; in the NIPU culture, staff transition from being ‘experts’ who alone can decide what is best for a baby, to becoming mentors, coaches and facilitators. Parents are expected to provide their own valued input to care plans. Partnerships are particularly relevant for the bedside nurse. Nursing education has not, historically, included the concept of sharing the care of these tiny patients with their parents. Nurses have sometimes been described by parents as ‘gatekeepers’ between them and their baby.15 Parents usually identify nurses as the primary source of information about their baby,16 making the nurse’s role critically important. Aagaard and Hall’s description of ‘facilitative’ nurses, who are ‘kind, helpful, patient, answering questions, and reassuring’ best fits the qualities of a NIPU nurse, rather than ‘inhibitive’ nurses who fail to identify and respect parents’ and infants’ needs and who consider infants to be ‘their’ babies to be safeguarded against inexperienced parents.15
In the NIPU, communication at the bedside goes beyond providing details of the baby’s condition to providing education about how parents (or primary caregivers) can be effectively involved in the baby’s care. Communication is frequent, attentive and respectful, interdisciplinary, and is delivered in a culturally effective manner, using terms the parents can understand. Mentoring includes anticipating and providing support for parents’ expected anxieties and emotional distress. Parents report that they want physicians to be direct, sensitive and empathic when talking with them, particularly when it is necessary to convey ‘bad news.’ Parents appreciate being given time to react and share their feelings.17 After being fully informed of choices, parents desire to be involved in shared decision-making about their baby’s care. Transparency is key and is facilitated by parents’ understanding of their baby’s condition through frequent communication and by providing access to the baby’s medical records. All forms of communication acknowledge that parents are the most important people in their baby’s life and provide reassurance that the NIPU staff is able and willing to support them in their parenting role.
Culture of a NIPU
The concept of a NIPU is based on the partnership that is forged between the medical team and the baby’s parents and family. The medical team takes the initiative in providing reassurance to the parents that their presence, opinions, and insights about their baby, as well as their active participation in their baby’s care, are essential to achieving the best possible outcomes.
Another fundamental characteristic of the NIPU is that interdisciplinary collaboration is valued, with caregivers operating as a team, not as individuals functioning within their own ‘silos’ of practice. Everyone on the team is aware of the emotional needs of parents so staff can be responsive to family concerns. The emotional needs of staff are also recognized and everyone on the team supports everyone else on the team. Due to the significant risks staff face for development of secondary traumatic stress syndrome, post-traumatic stress syndrome and/or burnout,18, 19, 20, 21 it is imperative that they are provided the support needed to make it possible for them to fully support the families in their care. Consistent and reliable support of staff, from both medical and nursing administration and from mental health professionals experienced in NICU-related stress issues, will enable their optimal functioning within the NIPU.
Continuous learning and continuous quality improvement are additional elements of a NIPU’s culture. Learning is both bi-directional and circular, with all disciplines sharing their expertise and all staff willing to learn from each other and from parents about ways to improve care of the baby and family. Quality improvement projects continually examine current practices to determine if they are providing the desired outcomes and are adjusted as needed.
Potentially better practices for the NIPU
Family-centered developmental care
The primary purpose of Family-Centered Developmental Care (FCDC) is to enhance the bonds of attachment between parents and their baby.22 In the past several decades, a growing body of research has documented that the quality of parent-infant attachment directly influences a child’s outcomes.23 Short-term effects of parental presence include improved physiologic stability and decreased stress, both of which are neuroprotective.24 Long-term effects of consistent parental presence include improved attachment and bonding, optimal brain development, and enhanced physical, cognitive and psychosocial development.25, 26
Provide family support, including antenatal consultation, whenever maternal or fetal conditions are identified that could lead to a NIPU stay.
- Provide families with a warm and culturally appropriate welcome upon admission to the NIPU, including:
- Welcoming signage with clear directions to the NIPU,
- Warm and supportive greeting from reception staff,
- Reconnection between parents and baby as a first priority,
- Review of NIPU routines and equipment in lay terms, free of medical jargon,
- Written description of resources for parents and families, and
- Assurance of 24/7 access to baby and information in the NIPU. 27
Treat parents as full partners in the NIPU caregiving team. 22
Teach all NIPU staff about the principles of FCDC. 28
Provide services of neonatal therapists including occupational therapy (OT), physical therapy (PT) and speech language pathologists (SLP) to mentor parents in neuroprotective developmental care. 29
Mentor parents in applying the principles of neuroprotective developmental care and in learning developmentally appropriate caregiving skills. 27, 30, 31
Coach parents in how to recognize and respond to the behavioral signs of stress, relaxation and the feeding cues of their baby. 27
Give parents written and verbal information about benefits of skin-to-skin contact with their baby and facilitate early, frequent and prolonged skin-to-skin contact throughout the NIPU stay. 27, 32
Teach parents swaddled bathing—in bed or tub as appropriate for their baby—to reduce stress, promote relaxation and support parent-infant bonding. 33
Incrementally increase parents’ engagement in all caregiving activities consistent with the clinical status of the baby and with the principles of FICare. 6, 27
Peer-to-peer and family support
Trained peer volunteers, who have, themselves, gone through the NIPU experience, are in the best position to understand what current NIPU parents are experiencing. Peer support creates a feeling of non-judgmental acceptance based on mutual respect.34 Parents may feel safer sharing some of their fears with peers than they would with the medical team, and peers can often help parents interpret difficult medical language.35, 36 Support can be provided in-person or by telephone,35 during group meetings,37 or through an Internet platform.38
Have a paid parent support coordinator.
Offer in-person peer support provided by volunteer NIPU graduate parents (‘veteran’ parents) to all current parents. 39
Provide peer support to parents beginning in the antepartum period when possible, through the NIPU and on to the transition to home.
Provide training to veteran parents who will provide peer support. 40
Include grandparents and siblings. 41
Forge ongoing collaboration between hospitals and veteran parents. 42
Mental health professionals
A spectrum of disciplines comprises the ‘mental health professional’ (MHP) domain, each discipline varying in specialty and training (depth and breadth). Disciplines include social workers, psychologists, psychiatrists and other para-professionally trained staff. There is a robust literature documenting both the psychosocial challenges families face when they have an infant in intensive care and the need for involving mental health professionals as critical members of the NIPU team.43, 44, 45 These challenges range from experiencing anxiety and depression to issues with bonding to managing the needs of healthy siblings. The MHPs are trained to address these needs and to educate other NIPU staff to provide basic psychosocial support.46 Additionally, mental health professionals in the NIPU, especially those with more specialized training, can play a role in ongoing research and quality improvement efforts, offer staff support and training, and administer and interpret screenings and other assessments.47
MHPs interact with all parents in the unit on a daily basis by providing support. 46
Provide both informal and formal mental health support to NIPU staff.
Screen all parents regularly to identify those in need of higher levels of care and make appropriate referrals. 48, 49
Train NIPU staff in symptom identification and counseling skills. 50, 51
Hold parent education groups with a therapeutic orientation. 46
Provide psychotherapy within the NIPU for those parents at highest risk. 52, 53
Establish telemedicine services for parents with travel difficulties if adequate information technology support is available. 47
Provide debriefing sessions with NIPU staff after critical events. 54
Palliative and bereavement care
Every NIPU provides comprehensive palliative and bereavement care. These care practices are founded on respect for the fetus’ and infant’s quality of life, dignity and integrity, as well as respect for the family as demonstrated by information sharing, parental involvement in decision-making, and collaboration with the medical team.55 Families need guidance—as do staff—especially when considering decisions to not initiate or to withdraw intensive life support from a baby, as the choices can be both ethically challenging and morally distressing.56
The adoption of palliative care practices recognizes that relief of pain and suffering is a viable treatment option for babies born at the edge of viability, those who are diagnosed with life-limiting conditions, or who become critically ill and are not responding to treatment. Hence, palliative care serves as an alternative to intensive care, continuing to provide quality care and grief support while honoring both the baby and the family.57
Bereavement care is relationship-based care that focuses on the grief process and provides interventions that support families with the goal of decreasing feelings of sorrow, psychosocial stress, and social isolation.58 Whether the death is anticipated or unexpected, family-centered interventions can make unbearable losses more bearable and acceptable.59
Provide consistent, reliable care that recognizes the family as the architect of the care plan.
Create protocols for the care and disposition of an infant’s body.
Respect and respond to the psychosocial needs of staff. 61
Build a continuum of support services for families across time and settings: hospital-based, community-based, faith-based and peer-facilitated.
Post-discharge follow-up
The importance of continuity of care for the NIPU baby and parents after discharge has long been recognized by hospitals and community health-care providers.29, 62 Parents may find the post-discharge period a stressful extension of their NIPU stay; to minimize anxiety, parental readiness for discharge can be achieved through participation in the infant’s care starting at NIPU admission. Family-centered care at discharge involves time-sensitive, two-way communication between parents and the multidisciplinary team with consideration for home visitation as an extension of the NIPU team. Part of the high stress that families experience after discharge includes costly medical bills, as well as non-medical expenses related to, for example, loss of work. Parents may also experience emotional distress while caring for premature infants after discharge due to concerns for their baby’s safety at home without continuous monitoring, complicated caregiving needs, or concerns for their ongoing development.63
Parents remain at increased risk for postpartum depression, post-traumatic stress disorder (PTSD), and anxiety disorders well after NIPU discharge, making it important for the NIPU to continue proactive and intentional work to address this critical transition period.44 Home visitation provided to all NIPU families after discharge can be done by a public health nurse, a NIPU nurse, or other trained person from a community support agency. Through their collaboration, NIPU OT, PT and SLP therapists offer important neurodevelopmental partnerships throughout the NIPU stay and post-discharge.29 Embracing the dynamics of team collaboration affords a parent-infant centric approach that ensures that each family receives state-of-the-art services in the NIPU and afterwards. Throughout the first years of life, parent mentoring and partnership are essential. PBPs cover medical follow-up, post-discharge parent mentoring and the roles of home visitors.
Assign a trained point person to every family to coordinate treatment plans and post-discharge referrals, and ensure that the family has necessary equipment.
Communicate with follow-up providers about the risk factors of parents/family, appointments, and medical records for baby.
Engage and empower parents to develop parenting skills and necessary care practices for their baby during the NIPU stay. 7
Provide individualized anticipatory guidance about psychosocial stresses families may face once baby is home. 64
- Home visitors: 65, 66
- Assess parents’ mental health symptoms and determine how these may affect care of and relationship with the baby,
- Identify and provide resources for each family as their needs change,
- Provide education to parents regarding infant health and how to provide responsive care to infant,
- Conduct infant developmental screens, and
Staff education and support
Burnout rates ranged from 7.5 to 54.4% among healthcare workers in 44 NICUs surveyed by Profit and colleagues.19 NICU and Labor and Delivery nurses are especially at risk for acute stress disorder, secondary traumatic syndrome, and PTSD related to their work.18, 20 Staff burnout and PTSD can have many adverse effects on patient care68, 69 and staff interactions19 as well as on their health and well-being.70, 71
- Staff support.
Summary
The NIPU is not a static system; it will be a dynamic, evolving place where new evidence-based PBPs continue to be introduced and tested to determine what works best. Importantly, long-term infant development and indices of parent and family well-being will need to be evaluated to determine if the NIPU model can deliver on its promise.
By necessity, the dynamic NIPU must focus on relationships that are ever changing. Three sets of relationships deserve attention. The first is parenting, a set of relationships within the family unit including parents, their baby, and other family members. The quality of these relationships will require continual monitoring, feedback, and support by caregivers in ways that are consistent in both content and continuity. A second set of relationships, those that occur between parents/family and staff, also require caregiver feedback and support. Staff must be given the education, communication techniques, coping tools and support by leadership to be effective in their roles as mentors, coaches and facilitators for parents and families. Staff education must emphasize that communication with parents is bi-directional with parents serving as equal partners in providing care. A third set of relationships to be nourished in the NIPU involves those among staff, from leadership to environmental service providers. The NIPU model requires mutual respect and coordinated efforts by the multidisciplinary teams. The emotional well-being of the staff must be monitored in a way that communicates awareness of the inherently stressful nature of the intensive care environment and ensures readily available supports. If there is one principle that permeates every aspect of the NIPU, it is that everyone is looking out for the physical, mental and emotional health and well-being of babies, families and each other.
Acknowledgments
We are grateful to the leadership of the Vermont Oxford Network. Many thanks also to the participants of the the National Perinatal Association Work group on Psychosocial Support for NICU Parents. We also appreciate the assistance of Lauren Leslie-Hynan.
Footnotes
The authors declare no conflict of interest.
References
- Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF et al. Whole body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med 2005; 353: 1574–1584. [DOI] [PubMed] [Google Scholar]
- Kingsmore SF, Petrikin J, Willig LK, Guest E. Emergency medical genomes: a breakthrough application of precision medicine. Genome Med 2015; 7: 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson-Costello D, Friedman H, Minich N, Siner B, Taylor G, Schluchter M et al. Improved neurodevelopmental outcomes for extremely low birth weight infants in 2000–2002. Pediatrics 2007; 119: 37–45. [DOI] [PubMed] [Google Scholar]
- Tripathi T, Dusing S. Long-term neurodevelopmental outcomes of infants born late preterm: a systematic review. Res Rep Neonatol 2015; 5: 91–111. [Google Scholar]
- Ortenstrand A, Westrup B, Brostrom E, Sarman I, Akerstrom S, Brune T et al. The Stockholm Neonatal Family Centered Care Study: effects on length of stay and infant morbidity. Pediatrics 2010; 125: e278–e285. [DOI] [PubMed] [Google Scholar]
- O’Brien K, Bracht M, Macdonell K, McBride T, Robson K, O’Leary L et al. A pilot cohort analytic study of Family Integrated Care in a Canadian neonatal intensive care unit. BMC Pregnancy Childbirth 2013; 13: S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Pediatrics, Committee on Hospital Care, Institute for Patient- and Family-Centered Care. Patient- and family-centered care and the pediatrician’s role. Pediatrics 2012; 129: 394–404. [DOI] [PubMed] [Google Scholar]
- Hall S, Hynan M. Interdisciplinary recommendations for the psychosocial support of NICU parents. J Perinatol 2015; 35: S1–S36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White R. Recommended standards for newborn ICU design. J Perinatol 2006; 26: S2–18. [DOI] [PubMed] [Google Scholar]
- Van Enk R, Steinberg F. Comparison of private room with multiple-bed ward neonatal intensive care unit. HERD 2011; 5: 52–63. [DOI] [PubMed] [Google Scholar]
- Lester B, Salisbury A, Hawes K, Dansereau L, Bigsby R, Laptook A et al. 18-month follow-up of infants cared for in a single-family room neonatal intensive care unit. J Pediatr 2016; 177: 84–89. [DOI] [PubMed] [Google Scholar]
- Pineda R, Neil J, Dierker D, Smyser C, Wallendorf M, Kidoro H et al. Alterations in brain structure and neurodevelopmental outcome in preterm infants hospitalized in different neonatal intensive care unit environments. J Pediatr 2014; 164: 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voos K, Ross G, Ward M, Yohay A, Osorio S, Perlman J. Effects of implementing family-centered rounds (FCR) in a neonatal intensive care unit (NICU). J Matern Fetal Neonatal Med 2012; 24: 1403–1406. [DOI] [PubMed] [Google Scholar]
- Jones M, Qzai M, Young K. Ethnic differences in parent preference to be present for painful medical procedures. Pediatrics 2005; 116: e191–e197. [DOI] [PubMed] [Google Scholar]
- Aagaard H, Hall E. Mothers’ experiences of having a preterm infant in the neonatal care unit: a meta-synthesis. J Pediatr Nurs 2008; 23: e26–e36. [DOI] [PubMed] [Google Scholar]
- Kowalski W, Leef K, Mackley A, Spear M, Paul D. Communicating with parents of premature infants: who is the informant? J Perinatol 2006; 26: 44–48. [DOI] [PubMed] [Google Scholar]
- Sharp M, Strauss R, Lorch S. Communicating medical bad news: parents’ experiences and preferences. J Pediatr 1992; 121: 539–546. [DOI] [PubMed] [Google Scholar]
- Beck C, Gable R. A mixed methods study of secondary traumatic stress in labor and delivery nurses. J Obstet Gynecol Neonatal Nurs 2012; 41: 747–760. [DOI] [PubMed] [Google Scholar]
- Profit J, Sharek P, Amspoker A, Kowalkowski M, Nisbet C, Thomas E et al. Burnout in the NICU setting and its relation to safety culture. BMJ Qual Saf 2014; 10: 806–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czaja A, Moss M, Mealer M. Symptoms of post-traumatic stress disorder among pediatric acute care nurses. J Pediatr Nurs 2012; 27: 357–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weintraub A, Geithner E, Stroustrup A, Waldman E. Compassion fatigue, burnout and compassion satisfaction in neonatologists in the US. J Perinatol 2016; 36: 1021–1026. [DOI] [PubMed] [Google Scholar]
- McGrath J, Samra H, Kenner C. Family-centered developmental care practices and research: what will the next century bring? J Perinat Neonatal Nurs 2011; 25: 165–170. [DOI] [PubMed] [Google Scholar]
- Schore AN. Effects of a secure attachment relationship on right brain development, affect regulation, and infant mental health. Infant Ment Health J 2001; 22: 7–66. [Google Scholar]
- Winberg J. Mother and newborn baby: mutual regulation of physiology and behavior—a selective review. Dev Psychobiol 2005; 47: 217–229. [DOI] [PubMed] [Google Scholar]
- Westrup B. Family-centered developmentally supportive care. NeoReviews 2014; 15: e325–e335. [Google Scholar]
- Als H, Gilkerson L. The role of relationship-based developmentally supportive newborn intensive care in strengthening outcomes of preterm infants. Semin Perinatol 1997; 21: 178–189. [DOI] [PubMed] [Google Scholar]
- Cleveland L. Parenting in the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs 2008; 37: 666–691. [DOI] [PubMed] [Google Scholar]
- Harrison T. Family-centered pediatric nursing care: state of the science. J Pediatr Nurs 2010; 25: 335–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbosa V. Teamwork in the neonatal intensive care unit. Phys Occup Ther Pediatr 2013; 33: 5–26. [DOI] [PubMed] [Google Scholar]
- Melnyk B, Feinstein N, Alpert-Gillis L, Fairbanks E, Crean H, Sinkin R et al. Reducing premature infants’ length of stay and improving parents' mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics 2006; 118: e1414–e1427. [DOI] [PubMed] [Google Scholar]
- Altimier L, Phillips R. The Neonatal Integrative Developmental Care Model: seven neuroprotective core measures for family-centered developmental care. Newborn Infant Nurs Rev 2013; 13: 9–22. [Google Scholar]
- Baley J. Committee on Fetus and Newborn. Skin-to-skin care for term and preterm infants in the neonatal ICU. Pediatrics 2015; 136: 596–599. [DOI] [PubMed] [Google Scholar]
- Edraki M, Paran M, Montaseri S, Nejad M, Montaseri Z. Comparing the effects of swaddled and conventional bathing methods on body temperature and crying duration in premature infants: a randomized clinical trial. J Caring Sci 2014; 3: 83–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preyde M, Ardal F. Effectiveness of a parent ‘buddy’ program for mothers of very preterm infants in a neonatal intensive care unit. CMAJ 2003; 168: 969–973. [PMC free article] [PubMed] [Google Scholar]
- Ainbinder J, Blanchard L, Singer G, Sullivan M, Powers L, Marquis J et al. A qualitative study of parent to parent support for parents of children with special needs. J Pediatr Psychol 1998; 23: 99–109. [DOI] [PubMed] [Google Scholar]
- Hurst I. One size does not fit all: parent’s evaluation of a support program in a newborn intensive care nursery. J Perinat Neonatal Nurs 2006; 20: 252–261. [DOI] [PubMed] [Google Scholar]
- Bracht M, Ardal F, Bot A. Initiation and maintenance of a hospital-based parent group for parents of premature infants: key factors for success. Neonatal Netw 1998; 17: 33–37. [PubMed] [Google Scholar]
- Scharer K. Internet social support for parents: the state of science. J Child Adolesc Psychiatr Nurs 2005; 18: 26–35. [DOI] [PubMed] [Google Scholar]
- Hall S, Ryan D, Beatty J, Grubbs L. Recommendations for peer-to-peer support for NICU parents. J Perinatol 2015; 35: S9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santelli B, Turnbull A, Marquis J, Lerner E. Parent to parent programs: a unique form of mutual support. Infant Young Child 1995; 8: 48–57. [Google Scholar]
- Kerr S, McIntosh J. Coping when a child has a disability: exploring the impact of parent-to-parent support. Child Care Health Dev 2000; 26: 309–322. [DOI] [PubMed] [Google Scholar]
- Boukydis C. Support services and peer support for parents of at-risk infants: an international perspective. Child Health Care 2000; 29: 129–145. [Google Scholar]
- Friedman S, Kessler A, Yang S, Parsons S, Friedman H, Martin R. Delivering perinatal psychiatric services in the neonatal intensive care unit. Acta Paediatr 2013; 102: e392–e397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holditch-Davis D, Santos H, Levy J, White-Traut R, O’Shea T, Geraldo V et al. Patterns of psychological distress in mothers of preterm infants. Inf Beh Devel 2015; 41: 154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw R, Bernard R, DeBlois T, Ikuta L, Ginzburg K, Koopman C. The relationship between acute stress disorder and posttraumatic stress disorder in the neonatal intensive care unit. Psychosomatics 2009; 50: 131–137. [DOI] [PubMed] [Google Scholar]
- Steinberg Z, Patterson C. Giving voice to the psychological in the NICU: a relational model. J Infant Child Adolesc Psych 2017; 16: 25–44. [Google Scholar]
- Hynan M, Steinberg Z, Baker L, Cicco R, Geller P, Lassen S et al. Recommendations for mental health professionals in the NICU. J Perinatol 2015; 35: S14–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hynan M, Mounts K, Vanderbilt D. Screening parents of high-risk infants for emotional distress: rationale and recommendations. J Perinatol 2013; 33: 748–753. [DOI] [PubMed] [Google Scholar]
- Kazak A. Pediatric psychosocial preventative health model (ppphm): research, practice, and collaboration in pediatric family systems medicine. Fam Syst Health 2006; 24: 381–395. [Google Scholar]
- Segre L, Stasik S, O’Hara M, Arndt S. Listening Visits: an evaluation of the effectiveness and acceptability of a home-based depression treatment. Psychother Res 2010; 20: 712–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segre L, Chuffo-Siewert R, Brock R, O’Hara M. Emotional distress in mothers of preterm hospitalized infants: a feasibility trial of nurse-delivered treatment. J Perinatol 2013; 33: 924–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jotzo M, Poets C. Helping parents cope with the trauma of premature birth: an evaluation of a trauma-preventive psychological intervention. Pediatrics 2005; 115: 915–919. [DOI] [PubMed] [Google Scholar]
- Shaw R, St. John N, Lilo E, Jo B, Benitez W, Stevenson D et al. Prevention of traumatic stress in mothers of preterm infants: a randomized controlled trial. Pediatrics 2013; 132: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keene E, Hutton N, Hall B, Rushton C. Bereavement debriefing sessions: an intervention to support health care professionals in managing their grief after the death of a patient. Pediatr Nurs 2010; 36: 185–189. [PubMed] [Google Scholar]
- Daboval T, Shidler S. Ethical framework for shared decision making in the neonatal intensive care unit: communicative ethics. Paediatr Child Health 2014; 19: 302–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter B, Leuthner S. Decision making in the NICU—strategies, statistics, and 'satisficing.'. Bioethics Forum [Internet] 2002; 18: 7–15. [PubMed] [Google Scholar]
- American Academy of Pediatrics Committee on Fetus and Newborn. Noninitiation or withdrawal of intensive care for high-risk newborns. Pediatrics 2007; 119: 401–403. [DOI] [PubMed] [Google Scholar]
- Forte A, Hill M, Pazder R, Feudtner C. Bereavement care interventions: a systematic review. BMC Palliat Care 2004; 3: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris L, Douma C. End-of-life care in the NICU: a family-centered approach. Neoreviews 2010; 11: e194–e199. [Google Scholar]
- National Association of Neonatal NursesPalliative and end-of-life care for newborns and infants. Position Statement #3063 [Internet]. National Association of Neonatal Nurses; 2015.
- Sanchez-Reilly S, Morrison S, Carey E, Bernacki R, O’Neil L, Kapo J et al. Caring for oneself to care for others: physicians and their selfcare. J Support Oncol 2013; 11: 75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith V, Hwang S, Dukhovny D, Young S, Pursley D. Neonatal intensive care unit discharge preparation, family readiness and infant outcomes: connecting the dots. J Perinatol 2013; 33: 415–421. [DOI] [PubMed] [Google Scholar]
- Melnyk B, Crean H, Feinstein N, Fairbanks E. Maternal anxiety and depression after a premature infant’s discharge from the neonatal intensive care unit: explanatory effects of the creating opportunities for parent empowerment program. Nurs Res 2008; 57: 383–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Placencia F, McCullough L. Biopsychosocial risks of parental care for high-risk neonates: implications for evidence-based parental counseling. J Perinatol 2012; 32: 381–386. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics and American College of Obstetricians and GynecologistsPerinatal Guidelines for Home Visitation. American Academy of Pediatrics and American College of Obstetricians and Gynecologists: Washington, DC, 2010. [Google Scholar]
- US Department of Health and Human Resources, Administration for Children and Families. Home Visiting Evidence of Effectiveness (HomeVee). 2015. Available at http://homvee.acf.hhs.gov [Accessed on 2 May 2017].
- Chuffo-Siewert R, Cline M, Segre L. Implementation of an innovative nurse-delivered depression intervention for mothers of NICU infants. Adv Neonatal Care 2015; 15: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cimiotti J, Aiken L, Sloan D, Wu E. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control [Internet] 2012; 40: 486–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken L, Clarke S, Sloane D, Sochalski J, Silber J. Hospital nurse staffing and patient mortality, nurse burnout and job dissatisfaction. JAMA 2002; 288: 1987–1993. [DOI] [PubMed] [Google Scholar]
- Braithwaite M. Nurse burnout and stress in the NICU. Adv Neonatal Care 2008; 8: 34–37. [DOI] [PubMed] [Google Scholar]
- Mealer M, Burnham E, Goode C, Rothbaum B, Moss M. The prevalence and impact of post- traumatic stress disorder and burnout syndrome in nurses. Depress Anxiety 2009; 26: 1118–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer L, Fulton S, Kirchner H, Eisengart S, Lewis B, Short E et al. Longitudinal predictors of maternal stress and coping after very low-birth-weight birth. Arch Pediatr Adolesc Med 2012; 164: 518–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer L, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA 1999; 281: 799–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wigert H, Dellenmark M, Bry K. Strengths and weaknesses of parent-staff communication in the NICU: a survey assessment. BMC Pediatr 2013; 13: 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Pediatric Workforce American Academy of Pediatrics. Culturally effective pediatric care: education and training issues. Pediatrics 1999; 103: 167–170. [DOI] [PubMed] [Google Scholar]
- Cortezzo D, Sanders M, Brownell E, Moss K. Neonatologists’ perspectives of palliative and end-of-life care in neonatal intensive care units. J Perinatol 2013; 33: 731–735. [DOI] [PubMed] [Google Scholar]
- National Association of Neonatal Nurses. The effect of staff nurses’ shift length and fatigue on patient safety. Position Statement #3054 [Internet]. National Association of Neonatal Nurses; 2011. Available from http://www.nann.org/uploads/files/The_Effect_of_Staff_Nurses_Shift_Length_and_Fatigue_on_Patient_Safety_2011.pdf. [DOI] [PubMed]
- Caldeira S, Hall J. Spiritual leadership and spiritual care in neonatology. J Nurs Manag 2012; 20: 1069–1075. [DOI] [PubMed] [Google Scholar]