Abstract
Background and Aims: Given the increased risk of post-transplant metabolic syndrome (PTMS; defined by hypertension, diabetes mellitus and hyperlipidemia), we aimed to identify the potential role of food addiction in the development of metabolic complications in the post-liver transplant population.
Methods: Inclusion criteria included adult liver transplant recipients followed at our institution between June 2016 and November 2016. Participants were administered a demographic survey as well as the Yale Food Assessment Scale 2.0, a 35-item questionnaire used to assess frequency of food addiction in accordance with the DSM-V guidelines of substance use disorders. Demographic and clinical data were collected.
Results: Our study included 236 liver transplant recipients (139 males, 97 females). The median (interquartile range [IQR]) BMI of participants was 26.8 kg/m2 (24.2, 30.4), and median (IQR) time since transplantation was 50.9 months (19.6, 119.8). The prevalence rates of hypertension, hypercholesterolemia and diabetes mellitus were 54.7%, 25.0% and 27.1%, respectively. Twelve participants (5.1%) were found to have a diagnosis of food addiction. A diagnosis of food misuse was made in 94 (39.8%) of the transplant recipients.
Conclusions: Our findings are consistent with prior data that indicate high prevalence of metabolic complications among liver transplant recipients. Food addiction was not predictive of metabolic complications within this population. Nevertheless, we found that this population was at high risk of demonstrating symptoms of food misuse, and they were not likely to appreciate the risks of pathologic patterns of eating. Given the increasing risk of cardiovascular morbidity and mortality in this population, efforts should be made to identify risk factors for the development of PTMS.
Keywords: Food addiction, Liver transplant, Metabolic complications
Introduction
As long-term survival among liver transplant recipients continues to increase, metabolic complications, including hypertension, diabetes, hypercholesterolemia and obesity, as well as cardiovascular disease, are becoming more prevalent. Metabolic syndrome is seen in approximately half of liver transplant recipients, appearing at least two times more often than observed rates in the general population,1 with up to 58% of liver transplant recipients meeting all criteria for metabolic syndrome as defined by NCEP-ATP III.1–3 Individual criteria for metabolic syndrome, such as hypertension, hyperglycemia and hyperlipidemia, also occur at higher rates in liver transplant recipients compared to the general population.2,4–7
Although post-transplant immunosuppression likely contributes to the development of post-transplant metabolic syndrome (PTMS) and post-transplant diabetes mellitus (PTDM), weight gain after liver transplantation has been found to be independent of commonly used immunosuppressive regiments.8 PTMS and PTDM have been associated with an increased prevalence of cardiovascular disease, which has become the leading cause of morbidity and mortality in long-term liver transplant survivors in many outcome studies.1 A meta-analysis reporting pooled estimates from population-based and nested case-control studies found that liver transplant recipients have an approximately 64% greater risk of cardiovascular events than the general population.9
Substance abuse disorders are defined by the Diagnostic and Statistical Manual of Mental Disorders V (DSM-V) as a pathologic set of behaviors related to use of that substance, which include impaired control, social impairment, risky use and pharmacologic indications, such as tolerance and withdrawal.10 The health consequences of substance use disorders, such as excessive alcohol use and cigarette smoking, are drastic and well documented.11 The similarities in neural activation on functional magnetic resonance imaging have been demonstrated in addictive-like eating behavior and substance dependence, with increased activation in reward circuitry in response to food cues and reduced activation in inhibitory regions in response to food intake.12
The advent of the Yale Food Addiction Scale (YFAS) and its successor, the YFAS 2.0, which link DSM-V criteria for substance use disorders to the consumption of food, have provided objective measures for defining food addiction that have been demonstrated to correlate with levels of obesity and pathologic eating.13 The YFAS 2.0 diagnostic criteria have provided evidence that food addiction is an identifiable clinical syndrome with psychiatric co-morbidities and a psycho-behavioral profile similar to conventional drug-abuse disorders.14
Given the increased risk of development of PTMS and other metabolic complications in the post-liver transplant population, and the threat of increasing morbidity and mortality secondary to cardiovascular disease, we sought to investigate the association between food addiction, as defined by the YFAS 2.0, and the development of obesity and its metabolic complications in this population. In addition to identifying the role of food addiction in the development of metabolic complications, we sought to identify whether “food misuse,” defined as meeting criteria for experiencing two symptoms of “food addiction” without meeting criteria for self-reported “clinical significance,” is associated with the development of metabolic complications. We hypothesized that food misuse and addiction in the post-liver transplant population are associated with the development of obesity, hypertension, diabetes mellitus and dyslipidemias.
Methods
Participants and procedures
Participants in this study were liver transplant recipients who were seen for follow-up at the University of California, Los Angeles Pfleger Liver Institute between June 2016 and November 2016. Surveys and informed consent were administered in both English and Spanish, and translation services were provided for patients whose native language was neither English nor Spanish. All eligible patients seen in the Pfleger Liver Institute were invited by investigators to participate in the study during their visit at the clinic.
Following a short verbal explanation of the study, participants were administered a demographic questionnaire and the YFAS 2.0 questionnaire (see below). Participation in the study was completely voluntary and there was no compensation offered. The University of California, Los Angeles Institutional Review Board approved the study. Prior medical records of all study participants were accessed in order to obtain information about the patients both prior to and after liver transplantation, including indication for liver transplantation, medications, date of transplantation, and laboratory test results.
Demographic questionnaire
Participants completed a demographic survey used to assess weight before and after transplantation. Other demographic data included age, sex, ethnicity, highest level of education, work status, socio-economic status and presence of co-morbidities, including hypertension, hypercholesterolemia and diabetes mellitus.
YFAS 2.0
The YFAS 2.0 is a 35-item questionnaire using a Likert scale to assess the frequency of food addiction.13 The purpose of the survey is to identify individuals who exhibit traits of food addiction in accordance with the DSM-V criteria for substance use disorders. Participants answered 35 questions based on a 0 to 6 scale, indicating frequency of which they experienced symptoms that correlated with food addiction. The frequency of experienced symptoms is stratified in the test according to the following numbers on the Likert scale: 0, less than once a month; 1, once a month; 2, 2–3 times a month; 3, once a week; 4, 2–3 times a week; 5, 4–6 times a week; and 6, every day.
The 35 questions used in the study were used to identify the 11 criteria of food addiction: substance taken in larger amount and for longer period of time than intended; persistent desire or repeated unsuccessful attempts to quit; much time/activity to obtain, use or recover; important social, occupational or recreational activities given up or reduced; use continues despite knowledge of adverse consequences; tolerance; characteristic withdrawal symptoms (substance taken to relieve withdrawal); continued use despite social or interpersonal problems; failure to fulfill major role obligation; use in physically hazardous situations; craving, or a strong desire or urge to use. Each question has a different threshold aimed at identifying how often symptoms are experienced. In order for one to qualify as having “food addiction,” they must meet the threshold for at least 2 symptoms, and must also meet the threshold for at least one of the two symptoms of “clinical significance,” defined as impairment as a result of their behaviors. If individuals meet at least two symptoms but do not meet criteria for clinical significance, they are not diagnosed with food addiction.
Participants were further stratified into one of four groups (no food addiction, mild, moderate or severe food addiction) based on the number of symptoms met. Mild food addiction was classified as meeting 2–3 symptoms, moderate food addiction was classified as meeting 4–5 symptoms, and severe food addiction was classified as meeting 6 or more symptoms. Higher scores on the YFAS 2.0 have been demonstrated to correlate with increased body mass index (BMI), more frequent binge eating, greater impulsivity and stronger cravings for fatty, processed foods.15 Higher scores have also been demonstrated to parallel patterns of neural response implicated in addiction.16 This scale has been demonstrated to have good internal consistency, as well as convergent, discriminant and incremental validity, with strong associations demonstrated between exceeding the food addiction threshold and obesity.13
Food misuse vs. food addiction
Common psychological substrates have been elaborated comparing unhealthy patterns of food consumption and substance abuse.17 There is increasing evidence to demonstrate that obese individuals and those who engage in pathological consumption of food, such as is seen in bulimia nervosa (BN) or binge eating disorder (BED), exhibit similar behavioral patterns to those with other addictive behaviors as defined by the DSM.18 However, the cause of obesity is multifactorial and some authors have argued that food “addiction” per se may at best be considered a “phenotype of obesity”19 and that the concept of “addiction” may not necessarily explain obesity.20 Moreover, it has been argued that only a small percentage of individuals would actually meet the criteria for food addiction as it is conceptualized.18
Food addiction, as defined based on the DSM-V addiction criteria, would require clinically significant distress or impairment ensuing from the maladaptive eating behaviors.17 However, individuals who do not meet these criteria may still be considered to have a subclinical presentation that correlates with their obesity and its metabolic complications. These pathological behaviors may be salient features of what we term “food misuse”. In our study, we defined food misuse as meeting at least two criteria of food addiction behaviors as defined by the YFAS 2.0, without meeting criteria for clinical significance. Gearhardt et al.15 have studied individuals who meet at least 2 symptoms of food addiction without meeting criteria for “clinical significance,” and this data has proved to have good internal consistency as well.
Operational definitions
In efforts to identify associations between food addiction in liver transplant patients and development of long-term sequelae, individual criteria constituting the definition of metabolic syndrome were studied, which include BMI, arterial hypertension, diabetes mellitus, hypercholesterolemia and hypertriglyceridemia.
We defined hypertension as a blood pressure value greater than 140/90 mmHg measured on two separate occasions, based on current Joint National Committee hypertensive guidelines, or as current use of anti-hypertensive medications.21 A diagnosis of diabetes mellitus was made if the patient met at least one of the following three criteria: a) fasting blood sugar equal to or greater than 126 mg/dL measured on two occasions; b) hemoglobin A1c level greater than or equal to 6.5%; and c) if the patient was currently taking medications for a prior diagnosis of diabetes mellitus.22 Hypercholesterolemia for liver transplant recipients was defined by an elevated low-density lipoprotein cholesterol (LDL-C) level greater than 100 mg/dL, as recommended by treatment guidelines by the American Association for the Study of Liver Diseases (AASLD), and/or individuals being treated with cholesterol-lowering medication.23 Hypertriglyceridemia was defined as a triglyceride levels greater than 200 mg/dL or the use of triglyceride-lowering medications.24 Obesity in the post-transplant population was defined using the World Health Organization definition BMI classification. BMI between 18.5–24.99 was classified as normal, 25–29.99 as overweight, 30–34.99 as class I obesity, 35–39.99 as class II obesity, and >40 as class III obesity.25 PTMS was defined in our study as meeting a diagnosis of diabetes, hypertension and hypertriglyceridemia as defined above.
Data analysis
Data were summarized as median with interquartile range (IQR) or number in group with percent of group. Wilcoxon rank sum test was used to test statistical significance in continuous variables and a Fisher’s exact test was used to test for statistical differences. A p-value below 0.05 was considered statistically significant and all statistical tests were two-sided. The R Statistical Computing Environment was used for analysis (R Core Team; Vienna, Austria).
Results
Demographics
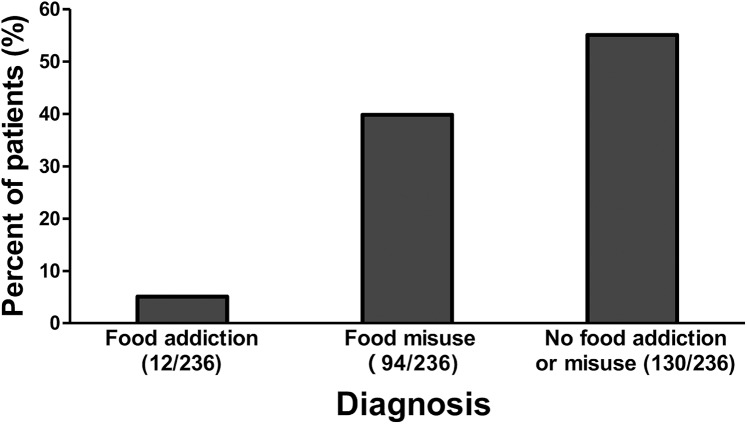
Overall, 12 participants (5.1%) in our study met a diagnosis of food addiction, while 94 participants (39.8%) met a diagnosis of “food misuse” (Fig. 1).
Fig. 1. Patients with food misuse compared to patients with food addiction.
Our study included 236 liver transplant recipients (139 males, 97 females), with a median age of 61 years old (median IQR, 53–67 years) and median time since liver transplantation of 50.9 months (median IQR, 19.6–119.8 months). Ethnicity of participants was 41.9% non-Hispanic white, 38.7% Hispanic, 11.0% Asian, 5.5% African American, 1.2% Native American, and 3.2% classified as “other”. The prevalence of food misuse in our study cohort based on reported ethnicity was 38.9% of non-Hispanic white participants, 39.1% of Hispanic, 25.0% of black, 28.0% percent of Asian, and 30% classified as “other”. No ethnicity was associated with food misuse or food addiction (p > 0.05). Other risk factors, including smoking status and sex, were not associated with the development of food misuse or food addiction.
The most common indication for liver transplantation was hepatitis C cirrhosis (53.0% of participants), followed by alcoholic cirrhosis (14.8%), non-alcoholic fatty liver disease (13.1%), hepatitis B cirrhosis (8.5%), autoimmune hepatitis (5.9%), and other causes. Among the liver transplant recipients, 14.4% also had a diagnosis of hepatocellular carcinoma prior to transplantation (Table 1). We noted a statistically significant association between hepatitis C as indication for transplantation and a diagnosis of food misuse, as 46.4% of those with hepatitis C had food misuse while only 32.4% of participants without hepatitis C were classified as having food misuse (p = 0.033). Other indications for liver transplantation were not associated with development of food misuse or food addiction.
Table 1. Patient demographic characteristics.
| Variable | Result |
| Median age (IQR), years | 61 (53, 67) |
| Sex, male/female | 139 (58.9)/97 (41.1) |
| Median time since liver transplant (IQR), months | 50.9 (19.6, 119.8) |
| Current immunosuppression medication | |
| Primary | |
| Tacrolimus | 190 (80.5) |
| Cyclosporine | 25 (10.6) |
| Sirolimus | 23 (9.7) |
| Adjunct | |
| Mycophenolate | 78 (33.1) |
| Prednisone | 39 (16.5) |
| Ethnicity | |
| Non-Hispanic white | 99 (41.9) |
| Hispanic white | 89 (38.7) |
| African American | 13 (5.5) |
| Asian | 26 (11.0) |
| Native American | 3 (1.2) |
| Other | 9 (3.8) |
| Indication for liver transplantation | |
| Hepatitis B | 20 (8.5) |
| Hepatitis C | 125 (53) |
| Alcoholic cirrhosis | 35 (14.8) |
| Autoimmune hepatitis | 14 (5.9) |
| Non-alcoholic fatty liver disease | 31 (13.1) |
| Other† | 37 (15.7) |
| Pre-transplant hepatocellular cancer | 34 (14.4) |
| History of smoking | 206 (87.3) |
| Pre-transplant | |
| Diabetes mellitus | 49 (20.8) |
| Hypertension | 90 (38.1) |
| High cholesterol | 40 (17.0) |
| High triglycerides | 49 (20.8) |
| Post-transplant | |
| Diabetes mellitus | 64 (27.1) |
| Hypertension | 129 (54.7) |
| High cholesterol | 59 (25) |
| High triglycerides | 24 (10.2) |
| Body mass index, median (IQR) | |
| Before transplant | 28 (24.4, 31.2) |
| After transplant, first clinic visit | 26 (23.2, 29.9) |
| Current | 26.8 (24.2, 30.4) |
| Education | |
| Less than high school | 9 (3.8) |
| High school | 123 (52.1) |
| College | 46 (19.5) |
| Graduate | 35 (14.8) |
| Other | 23 (9.7) |
| Estimated annual income | |
| <$50,000 | 114 (48.3) |
| $50,000–100,000 | 79 (33.5) |
| >$100,000 | 43 (18.2) |
| Employment status | |
| Employed | 82 (34.7) |
| Retired | 93 (39.4) |
| Other | 61 (25.8) |
| <35 hours/week | 18 (8.5) |
| >35 hours/week | 50 (23.6) |
Data are presented as n (%), unless otherwise indicated. IQR, interquartile range.
Other reasons for transplant: cryptogenic cirrhosis, Wilson’s disease, acute liver failure, primary biliary cirrhosis, hemochromatosis, benign tumor, polycystic liver disease, alpha-1-antitrypsin disease.
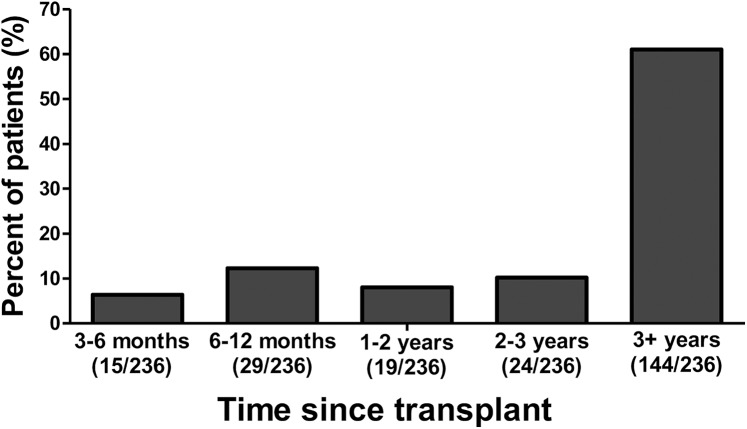
Of the participants in our study, 16.5% were currently on prednisone therapy, 10.6% were on cyclosporine, 9.7% were on sirolimus, 80.5% were on tacrolimus, and 33.1% were on mycophenolate mofetil (Table 1). Laboratory values obtained at the time of the survey are shown in Table 2. Most participants were transplanted at least 3 years before survey administration (Fig. 2). The use of cyclosporine was noted to have a statistically significant association with development of food misuse, as 16.0% of those on cyclosporine had food misuse, while 3.8% of those not on cyclosporine had food misuse (p = 0.027). Food misuse and food addiction were not associated with use of prednisone, sirolimus, tacrolimus or mycophenolate mofetil.
Table 2. Baseline laboratory data.
| Variable | Median (IQR) |
| AST in U/L | 15 (12, 23) |
| ALT in U/L | 13 (11, 21) |
| Total bilirubin in mg/dL | 1 (0.5, 1) |
| Creatinine in mg/dL | 1 (1, 1.3) |
| Glucose 1 in mmol/L | 121 (103.5, 124) |
| Glucose 2 in mmol/L | 116 (103, 124) |
| LDL-C in mmol/L | 100 (95, 103.5) |
| Triglyceride in mmol/L | 196 (165, 200) |
| Hemoglobin A1C as % | 6.1 (5.6, 6.7) |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; LDL-C, low-density lipoprotein cholesterol.
Fig. 2. Time since liver transplantation.
Hypertension
Self-reported prevalence of hypertension prior to transplantation was 38.1%. Prevalence of hypertension post-transplantation was 54.7% (Table 1). Neither food addiction (p = 0.139) nor food misuse (p = 0.262) was associated with the prevalence of post-transplant hypertension. De novo hypertension after transplantation was also not associated with either food addiction (p = 0.51) or food misuse (p = 0.188).
Hypercholesterolemia
Seventeen percent of our study cohort had a diagnosis of hypercholesterolemia before liver transplantation, and prevalence increased to 25.0% after liver transplantation (Table 1). Neither food misuse nor food addiction were associated with the development of de novo hypercholesterolemia post-transplantation (p = 0.888 and 0.233, respectively), although food misuse was associated with the prevalence of hypercholesterolemia after transplantation (p = 0.031).
Hypertriglyceridemia
Forty-nine participants (20.8%) in our study cohort reported having a diagnosis of hypertriglyceridemia prior to liver transplantation. After transplantation, 24 study participants (10.2%) had a diagnosis of hypertriglyceridemia (Table 1). Neither food misuse nor food addiction was associated with prevalence of hypertriglyceridemia at the time of our survey (p = 0.369 and 0.15, respectively). De novo hypertriglyceridemia after transplantation was also not associated with food misuse or food addiction (p = 0.429 and 0.223, respectively).
Diabetes mellitus
The prevalence of diabetes mellitus was 20.8% and 27.1% before and after liver transplantation, respectively (Table 1). Neither the prevalence of diabetes mellitus after transplantation nor de novo diabetes after transplantation was associated with food addiction (p = 0.907 and 0.717, respectively) or food misuse (p = 0.697 and 0.311, respectively).
Obesity
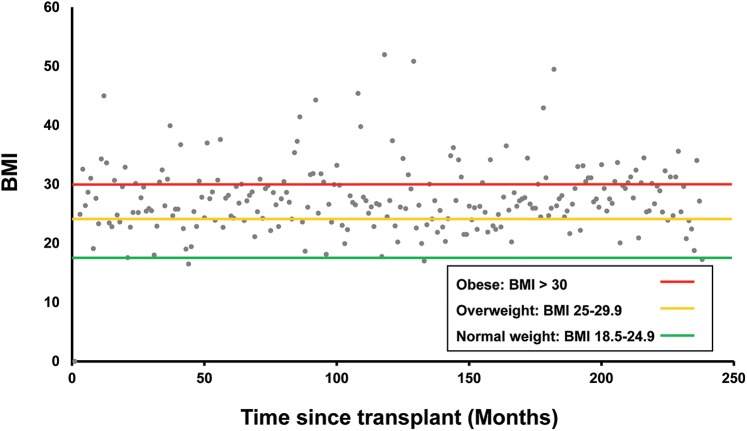
Between 6 to 12 months after transplantation, 80% of patients were classified as overweight or obese, at 12–24 months 66% were overweight or obese, at 24–36 months 78% were classified as overweight or obese and at 36 months or more the number of overweight or obese patients declined to 56% (Fig. 3). The median (IQR) BMI at the time of the first clinic visit after transplantation was 26.0 (23.2, 29.9) and at the time of our survey was 26.8 (24.2, 30.4) (Table 1). Seventy participants (30.0%) were noted to have more than a 10% increase in BMI since time of transplantation. An increase in BMI of or at least 10% was not associated with food addiction (p = 0.15) nor food misuse (p = 0.102) in our study.
Fig. 3. Body mass index since liver transplantation.
PTMS
Among those without food misuse or food addiction, 5.6% of participants in our study met a diagnosis of metabolic syndrome, while 3.7% of those with food misuse met a diagnosis of metabolic syndrome, although this was not statistically significant. There was no association between food misuse and PTMS.
Food addiction vs. food misuse
We aimed to study the individual symptoms of the YFAS 2.0 and assess whether each individual symptom was noted to have statistically significant association with either a diagnosis of food addiction or food misuse. We found that seven of the individual symptoms were associated with a diagnosis of food addiction, whereas the following four symptoms were not: “important social, occupational, or recreational activities given up or reduced,” (p = 0.193), “continued use despite social or interpersonal problems” (p = 0.193), “failure to fulfill major role obligation,” (p = 0.739), and “use in physically hazardous situations” (p = 0.146). Each of the 11 individual symptoms of the YFAS 2.0 was found to have a statistically significant association with a diagnosis of food misuse (p < 0.001 for each symptom) (Table 3).
Table 3. Association between diagnosis of food misuse and individual symptoms of food addiction.
| Variable | No food misuse, n = 142 | Food misuse, n = 94 | p |
| Substance taken in larger amount and for longer period than intended | <0.001 | ||
| No | 139 (97.9) | 70 (74.5) | |
| Yes | 3 (2.1) | 24 (25.5) | |
| Persistent desire or repeated unsuccessful attempts at quitting | <0.001 | ||
| No | 141 (99.3) | 69 (75) | |
| Yes | 1 (0.7) | 23 (25) | |
| Much time/activity to obtain, use, recover | <0.001 | ||
| No | 124 (87.3) | 47 (50.5) | |
| Yes | 18 (12.7) | 46 (49.5) | |
| Important social, occupational, or recreational activities given up or reduced | <0.001 | ||
| No | 128 (90.8) | 26 (28) | |
| Yes | 13 (9.2) | 67 (72) | |
| Use continues despite knowledge of adverse consequences | <0.001 | ||
| No | 142 (100) | 74 (78.7) | |
| Yes | 0 (0) | 20 (21.3) | |
| Tolerance | <0.001 | ||
| No | 140 (98.6) | 82 (87.2) | |
| Yes | 2 (1.4) | 12 (12.8) | |
| Characteristic withdrawal symptoms | <0.001 | ||
| No | 140 (99.3) | 66 (70.2) | |
| Yes | 1 (0.7%) | 28 (29.8) | |
| Continued use despite social or interpersonal problems | <0.001 | ||
| No | 138 (97.2) | 25 (27.2) | |
| Yes | 4 (2.8%) | 67 (72.8) | |
| Failure to fulfill major role obligation | <0.001 | ||
| No | 135 (95.1) | 37 (39.4) | |
| Yes | 7 (4.9%) | 57 (60.6) | |
| Use in physically hazardous situations | <0.001 | ||
| No | 138 (97.9) | 43 (46.7) | |
| Yes | 3 (2.1) | 49 (53.3) | |
| Craving, or a strong desire or urge to use | <0.001 | ||
| No | 142 (100) | 79 (84) | |
| Yes | 0 (0) | 15 (16) | |
| Use causes clinically significant impairment or distress | <0.001 | ||
| No | 140 (98.6) | 82 (87.2) | |
| Yes | 2 (1.4) | 12 (12.8) | |
Data are presented as n (%).
Discussion
Our results are consistent with prior data indicating that certain metabolic complications are at increased prevalence in the liver transplant population in comparison to the general population, and that most metabolic complications increased in prevalence after transplantation. For instance, the prevalence of hypertension was 54.7% in liver transplant recipients, similar to that described by others.6 In contrast, the prevalence of hypertension among the general population was 30.4%.26 The prevalence of hypercholesterolemia in our cohort was 25.0%, which is almost double that described in the general population.26 The prevalence of diabetes mellitus among participants of the NHANES III 2011 was 14.3%.26 Our study discovered a higher prevalence of diabetes mellitus among liver transplant recipients, over 27.1%. Our diabetes prevalence rates among liver transplant recipients is consistent with that described by others.1,3,4,27
It is important to highlight that among our study cohort an understanding of prevalence of metabolic syndrome, as defined by the NCEP-ATP III, was limited. Our data on each participant was limited to diagnoses of hypertension, hypertriglyceridemia and diabetes mellitus; we did not have data on waist circumference or high-density lipoprotein level in our population. Regardless, certain metabolic complications, as detailed in our results, remain higher in the liver transplant population in comparison to the general population. This highlights the fact that discrepancies exist between the definition of metabolic complications among liver transplant consensus guidelines and the NCEP-ATP III. For example, NCEP-ATPIII defines hypertriglyceridemia as a level greater than 150 mg/dL, although we define hypertriglyceridemia in our unique patient population as greater than 200 mg/dL, which is the level at which the AASLD guidelines for long-term management of liver transplant recipients recommend treatment.23,24,28 Similarly, the NCEP-ATP III defines hypertension as blood pressure greater than or equal to 130/85 mmHg, while guidelines recommend treatment for hypertension in post-liver transplant recipients to be initiated when blood pressure is greater than 130/80 mmHg. Given that liver transplant recipients represent such a unique population, it may be necessary to consider whether the definition of metabolic syndrome as defined by the NCEP-ATP III should be applicable to this group.
Our results also indicate that prevalence of food addiction in the post-liver transplant population occurs at a significantly lower rate than reported food addiction (19.9%) among a general population as studied by Gearhardt et al.15 Although very few in our study were classified as having food addiction according to the YFAS 2.0 criteria, a large cohort of patients (39.8%) met criteria for food misuse, defined in our study as having at least two symptoms of food addiction without meeting criteria for self-identified clinical significance. This represents a large disparity between these two populations among liver transplant recipients.
Identifying a large number of participants who possess harmful patterns of eating, but may not report these symptoms as distressing potentially places this particular population at risk for development of metabolic complications. This may underscore a critical issue to address in liver transplant recipients as rates of metabolic complications are higher in this population than in the general population, despite the lower prevalence of self-reported food addiction behaviors found in our study. Further research is thus required to identify liver transplant recipients who are at risk of developing long-term metabolic complications.
Two risk factors for food misuse have been identified in our study. We noted an association between hepatitis C infection as indication for liver transplantation and presence of food misuse, while food misuse was not associated with other indications for transplantation. The molecular pathways by which hepatitis C results in metabolic syndrome, such as by inducing insulin resistance, are well-documented.29 Data have also demonstrated that chronic hepatitis C has been associated with a significant increase in reported pleasure derived from eating.30 It is likely that there are mechanisms by which hepatitis C may result in maladaptive eating behaviors, and it would be beneficial to direct future research at understanding the mechanisms underlying this association.
We also noted that cyclosporine use was associated with food misuse. Prior data have demonstrated that cyclosporine is associated with an additional 2.3 kg weight gain in comparison to tacrolimus use in liver transplant recipients.31 Cyclosporine is also a well-documented risk factor for both hypertension and hypercholesterolemia in liver transplant recipients.27,31 It is necessary in the near future to identify whether cyclosporine use is associated with weight gain, hypertension and hypercholesterolemia due to our observation that this medication use is associated with food misuse.
Our study confirms prior data from Watt et al.24 that indicates most weight gain in liver transplant recipients occurs in the first 1–3 years after transplantation. It is important to note that weight gain and obesity can lead to many of the metabolic complications identified in our study, and prior studies have shown than an increase in BMI >10% has also been associated with a higher risk of developing non-alcoholic fatty liver disease.32 Given the increasing rates of obesity and metabolic complications in liver transplant recipients, it is crucial to identify those patients meeting the criteria for food addiction or food misuse early in the post-transplant course. As prevalence of obesity and greatest weight gain have been shown to occur within the first 1–3 years after transplantation, it may be optimal to assess patients for food addiction and food misuse even prior to transplantation, in an effort to identify behaviors which may be modified.
Neither food addiction nor food misuse was found to be associated with many of the metabolic complications evaluated in our study, although food misuse was noted to have a statistically significant association with increased prevalence of hypertension. Given the increased prevalence of many of these metabolic complications, further research is required to identify a screening tool designed for liver transplant recipients to identify risk factors that may be predictive of the development of these metabolic complications. As noted above, this particular population possesses many of the maladaptive symptoms of food addiction in the YFAS 2.0, although very few participants met the criteria for food addiction. Thus, it is especially important to screen for these risk factors as this population may be particularly susceptible to developing metabolic complications without possessing the clinically significant impairment that would prompt development of lifestyle modifications.
Metabolic complications in liver transplant recipients puts them at increased risk for cardiovascular complications. Thus, it is necessary to identify those patients at risk for development of these complications both before and soon after transplantation to prevent their occurrence. Our study revealed a lower prevalence of food addiction in liver transplant recipients, but a higher prevalence of food misuse than in the general population. Given the high prevalence of food misuse within the post-liver transplant population, further research is needed to identify screening tools that are predictive of an association between maladaptive eating patterns and development of future metabolic complications.
Abbreviations
- AASLD
American Association for the Study of Liver Diseases
- AST
aspartate aminotransferase
- ALT
alanine aminotransferase
- BED
binge eating disorder
- BMI
body mass index
- BN
bulimia nervosa
- DSM
diagnostic statistical manual
- IQR
interquartile range
- LDL-C
low-density lipoprotein cholesterol
- PTDM
post-transplant diabetes mellitus
- PTMS
post-transplant metabolic syndrome
- YFAS
Yale Food Addiction Scale
References
- 1.Bianchi G, Marchesini G, Marzocchi R, Pinna AD, Zoli M. Metabolic syndrome in liver transplantation: relation to etiology and immunosuppression. Liver Transpl. 2008;14:1648–1654. doi: 10.1002/lt.21588. 10.1002/lt.21588. [DOI] [PubMed] [Google Scholar]
- 2.Laish I, Braun M, Mor E, Sulkes J, Harif Y, Ben Ari Z. Metabolic syndrome in liver transplant recipients: prevalence, risk factors, and association with cardiovascular events. Liver Transpl. 2011;17:15–22. doi: 10.1002/lt.22198. 10.1002/lt.22198. [DOI] [PubMed] [Google Scholar]
- 3.Laryea M, Watt KD, Molinari M, Walsh MJ, McAlister VC, Marotta PJ, et al. Metabolic syndrome in liver transplant recipients: prevalence and association with major vascular events. Liver Transpl. 2007;13:1109–1114. doi: 10.1002/lt.21126. 10.1002/lt.21126. [DOI] [PubMed] [Google Scholar]
- 4.Tueche SG. Diabetes mellitus after liver transplant new etiologic clues and cornerstones for understanding. Transplant Proc. 2003;35:1466–1468. doi: 10.1016/s0041-1345(03)00528-1. 10.1016/S0041-1345(03)00528-1. [DOI] [PubMed] [Google Scholar]
- 5.Saab S, Cho D, Lassman RC, Gajjar NA, Ghobrial M, Busuttil RW. Recurrent non-alcoholic steatohepatitis in a living related liver transplant recipient. J Hepatol. 2005;42:148–149. doi: 10.1016/j.jhep.2004.07.032. 10.1016/j.jhep.2004.07.032. [DOI] [PubMed] [Google Scholar]
- 6.Gojowy D, Adamczak M, Dudzicz S, Gazda M, Karkoszka H, Wiecek A. High frequency of arterial hypertension in patients after liver transplantation. Transplant Proc. 2016;48:1721–1724. doi: 10.1016/j.transproceed.2015.11.043. 10.1016/j.transproceed.2015.11.043. [DOI] [PubMed] [Google Scholar]
- 7.Mells G, Neuberger J. Reducing the risks of cardiovascular disease in liver allograft recipients. Transplantation. 2007;83:1141–1150. doi: 10.1097/01.tp.0000262706.28513.6a. 10.1097/01.tp.0000262706.28513.6a. [DOI] [PubMed] [Google Scholar]
- 8.Richards J, Gunson B, Johnson J, Neuberger J. Weight gain and obesity after liver transplantation. Transpl Int. 2005;18:461–466. doi: 10.1111/j.1432-2277.2004.00067.x. 10.1111/j.1432-2277.2004.00067.x. [DOI] [PubMed] [Google Scholar]
- 9.Madhwal S, Atreja A, Albeldawi M, Lopez R, Post A, Costa MA. Is liver transplantation a risk factor for cardiovascular disease? A meta-analysis of observational studies. Liver Transpl. 2012;18:1140–1146. doi: 10.1002/lt.23508. 10.1002/lt.23508. [DOI] [PubMed] [Google Scholar]
- 10.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington: American Psychiatric Association; 2013. [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC) Alcohol-Related Disease Impact (ARDI). Available from: https://nccd.cdc.gov/DPH_ARDI/default/default.aspx .
- 12.Tang DW, Fellows LK, Small DM, Dagher A. Food and drug cues activate similar brain regions: a meta-analysis of functional MRI studies. Physiol Behav. 2012;106:317–324. doi: 10.1016/j.physbeh.2012.03.009. 10.1016/j.physbeh.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 13.Gearhardt AN, Corbin WR, Brownell KD. Development of the Yale Food Addiction Scale Version 2.0. Psychol Addict Behav. 2016;30:113–121. doi: 10.1037/adb0000136. 10.1037/adb0000136. [DOI] [PubMed] [Google Scholar]
- 14.Davis C, Loxton NJ, Levitan RD, Kaplan AS, Carter JC, Kennedy JL. ‘Food addiction’ and its association with a dopaminergic multilocus genetic profile. Physiol Behav. 2013;118:63–69. doi: 10.1016/j.physbeh.2013.05.014. 10.1016/j.physbeh.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 15.Gearhardt AN, Boswell RG, White MA. The association of “food addiction” with disordered eating and body mass index. Eat Behav. 2014;15:427–433. doi: 10.1016/j.eatbeh.2014.05.001. 10.1016/j.eatbeh.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gearhardt AN, Yokum S, Orr PT, Stice E, Corbin WR, Brownell KD. Neural correlates of food addiction. Arch Gen Psychiatry. 2011;68:808–816. doi: 10.1001/archgenpsychiatry.2011.32. 10.1001/archgenpsychiatry.2011.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moreno C, Tandon R. Should overeating and obesity be classified as an addictive disorder in DSM-5? Curr Pharm Des. 2011;17:1128–1131. doi: 10.2174/138161211795656701. 10.2174/138161211795656701. [DOI] [PubMed] [Google Scholar]
- 18.Meule A. How prevalent is “food addiction”? Front Psychiatry. 2011;2:61. doi: 10.3389/fpsyt.2011.00061. 10.3389/fpsyt.2011.00061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Corsica JA, Pelchat ML. Food addiction: true or false? Curr Opin Gastroenterol. 2010;26:165–169. doi: 10.1097/MOG.0b013e328336528d. 10.1097/MOG.0b013e328336528d. [DOI] [PubMed] [Google Scholar]
- 20.Wilson GT. Eating disorders, obesity and addiction. Eur Eat Disord Rev. 2010;18:341–351. doi: 10.1002/erv.1048. 10.1002/erv.1048. [DOI] [PubMed] [Google Scholar]
- 21.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 22.American Diabetes Association Strategies for improving care. Diabetes Care. 2016;39(Suppl 1):S6–12. doi: 10.2337/dc16-S004. 10.2337/dc16-S004. [DOI] [PubMed] [Google Scholar]
- 23.Lucey MR, Terrault N, Ojo L, Hay JE, Neuberger J, Blumberg E, et al. Long-term management of the successful adult liver transplant: 2012 practice guideline by AASLD and the American Society of Transplantation. Available from: https://www.aasld.org/sites/default/files/guideline_documents/managementadultltenhanced.pdf . [DOI] [PubMed]
- 24.Watt KD. Keys to long-term care of the liver transplant recipient. Nat Rev Gastroenterol Hepatol. 2015;12:639–648. doi: 10.1038/nrgastro.2015.172. 10.1038/nrgastro.2015.172. [DOI] [PubMed] [Google Scholar]
- 25.Obesity: preventing and managing the global epidemic Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii. 1–253. [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC) National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey. Available from: https://wwwn.cdc.gov/nchs/nhanes/search/nhanes11_12.aspx .
- 27.Gisbert C, Prieto M, Berenguer M, Bretó M, Carrasco D, de Juan M, et al. Hyperlipidemia in liver transplant recipients: prevalence and risk factors. Liver Transpl Surg. 1997;3:416–422. doi: 10.1002/lt.500030409. 10.1002/lt.500030409. [DOI] [PubMed] [Google Scholar]
- 28.Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 29.Sheikh MY, Choi J, Qadri I, Friedman JE, Sanyal AJ. Hepatitis C virus infection: molecular pathways to metabolic syndrome. Hepatology. 2008;47:2127–2133. doi: 10.1002/hep.22269. 10.1002/hep.22269. [DOI] [PubMed] [Google Scholar]
- 30.Musialik J, Suchecka W, Klimacka-Nawrot E, Petelenz M, Hartman M, Błońska-Fajfrowska B. Taste and appetite disorders of chronic hepatitis C patients. Eur J Gastroenterol Hepatol. 2012;24:1400–1405. doi: 10.1097/MEG.0b013e3283589f63. 10.1097/MEG.0b013e3283589f63. [DOI] [PubMed] [Google Scholar]
- 31.Canzanello VJ, Schwartz L, Taler SJ, Textor SC, Wiesner RH, Porayko MK, et al. Evolution of cardiovascular risk after liver transplantation: a comparison of cyclosporine A and tacrolimus (FK506) Liver Transpl Surg. 1997;3:1–9. doi: 10.1002/lt.500030101. 10.1002/lt.500030101. [DOI] [PubMed] [Google Scholar]
- 32.Contos MJ, Cales W, Sterling RK, Luketic VA, Shiffman ML, Mills AS, et al. Development of nonalcoholic fatty liver disease after orthotopic liver transplantation for cryptogenic cirrhosis. Liver Transpl. 2001;7:363–373. doi: 10.1053/jlts.2001.23011. 10.1053/jlts.2001.23011. [DOI] [PubMed] [Google Scholar]